Abstract
Interventional cardiovascular magnetic resonance (iCMR) promises to enable radiation-free catheterization procedures and to enhance contemporary image guidance for structural heart and electrophysiological interventions. However, clinical translation of exciting pre-clinical interventions has been limited by availability of devices that are safe to use in the magnetic resonance (MR) environment. We discuss challenges and solutions for clinical translation, including MR-conditional and MR-safe device design, and how to configure an interventional suite. We review the recent advances that have already enabled diagnostic MR right heart catheterization and simple electrophysiologic ablation to be performed in humans and explore future clinical applications.
Keywords: Interventional cardiovascular MRI, Structural heart disease, MRI catheterization, Cardiac electrophysiology, Electrophysiology mapping and ablation, Cardiovascular catheterization, Real-time MRI
Introduction
Minimally invasive transcatheter therapies are targeting increasingly complex pathologies, but X-ray fluoroscopic guidance alone is insufficient. Through necessity, the twenty-first century interventional cardiologist has embraced multimodality imaging, for example intravascular ultrasound or optical coherence tomography to guide coronary stent deployment or transesophageal echocardiography for transcatheter aortic valve replacement or mitral valve repair.
Soft tissues only appear as shadows on X-ray fluoroscopy. The operator relies on knowledge of anatomy and experience of how a catheter should move to navigate through the vasculature. Contrast lumenography is the only way to actually “see” vessels and cardiac chambers. Ultrasound is limited by field of view, contrast, and available imaging windows and so is not useful to navigate through the vasculature or to monitor for remote complications. Though the spatial resolution and tissue characterization of CT are excellent, ionizing radiation doses for a lengthy cardiovascular intervention are currently prohibitive. In contrast, real-time magnetic resonance (MR) imaging combines the advantages of excellent soft tissue characterization, unconstrained imaging planes, and good image contrast—all without ionizing radiation.
In this review, we explore past pre-clinical and present-day clinical interventional cardiovascular MR (“iCMR”) applications. We review how to configure an iCMR suite and discuss the technical challenges and solutions to future translation of more complex procedures.
X-Ray Fused with MRI or “XFM”
As an interim step to performing cardiovascular interventions from start to finish in the MRI scanner, pre-acquired MR images can be “fused” with X-ray fluoroscopy. External fiduciary markers [1] or internal anatomic structures [2] are used to co-register MR overlays of chosen 3D structures onto the fluoroscopic images. In the field of electrophysiology, co-registration of CT or MRI images with electroanatomic maps to improve catheter navigation in three dimensions has been applied for many years. The major advantage of MRI over CT for this type of fusion imaging is the ability to incorporate cardiac and respiratory motion, rather than static overlays [3]. Software moves the overlays automatically as the X-ray image intensifier is moved around the patient to maintain correct orientation at all times. Specific targets can be highlighted, eliminating the need for repeated angiograms (Fig. 1). Early experience suggests that XFM can reduce procedure time, iodinated contrast use, and ionizing radiation dose [4]. Importantly, aside from additional software, which is currently investigational, no new hardware is required. This means that XFM can be used in any cardiac catheterization laboratory using images pre-acquired on any diagnostic MRI scanner. However, by definition, XFM overlays are obtained from data acquired before the intervention so cannot accommodate for anatomical distortion caused by devices (e.g., stiff guidewires) or by the intervention itself.
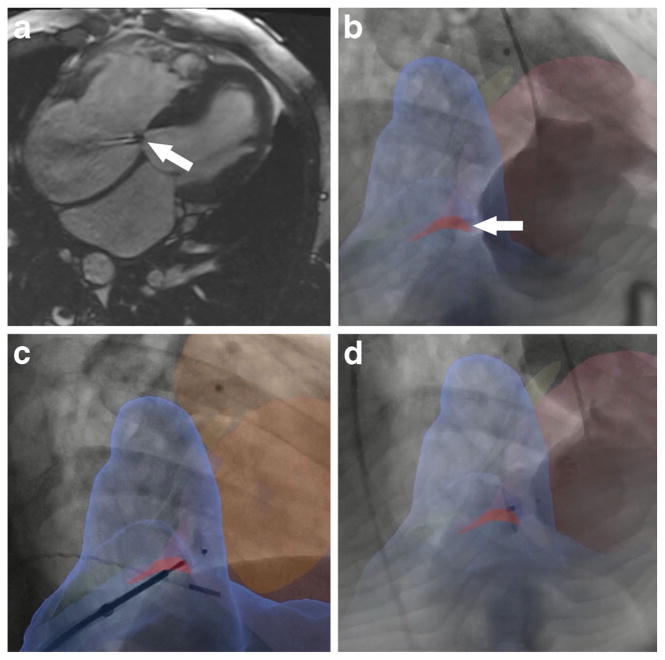
Fig. 1.
Clinical X-ray fused with MRI (XFM)-guided closure of ventricular-atrial (Gerbode) defect. a Four-chamber cine MRI showing defect between left ventricle and right atrium (arrow). Left-to-right flow is clearly seen. b XFM image in which the defect appears as a red overlay on the fluoroscopy (arrow). c Nitinol closure device on its delivery cable positioned across the defect. Both discs have been deployed. d Closure device after release. (Courtesy of Kanishka Ratnayaka (2014), Department of Cardiology, Children’s National Hospital Center, Washington DC, USA)
Why Should I Do iCMR?
Because It Can Improve Existing Interventions
Neurosurgery guided by intra-operative MRI increases the likelihood of complete tumor resection [5]. Performing cardiac catheterization using MR guidance requires comparable procedure time to traditional X-ray guidance [6•], avoids iodinated contrast, and can provide incremental physiological information [7]. Pre-clinical studies suggest that MR-guided electrophysiology studies may provide more accurate disease localization and be less likely to miss small but important abnormalities compared with present-day electroanatomic mapping [8]. Challenging catheter maneuvers become simple because the operator can actually see the anatomical structures. Real-time MRI using workhorse steady-state free precession pulse sequences can support imaging frame rates of between 5–10 images per second with acceptable spatial resolution and contrast [9]. Image acquisition can be accelerated with parallel acquisition schemes such as SENSE [10, 11] or GRAPPA [12], and although it still has lower frame rate than X-ray, real-time MRI is comparably information-rich.
Because It Is Radiation Free
Cumulative radiation exposure is potentially harmful in certain populations, particularly children with congenital heart disease in whom serial X-ray procedures may be required over many years [13]. MRI is already accepted as the best noninvasive imaging modality for patients with complex congenital heart disease [14], and MR-guided catheterization could significantly reduce cumulative radiation dose. Moreover, awareness of the potential adverse effects of radiation exposure on operators and catheterization laboratory staff is growing [15, 16]. Switching from X-ray to MR guidance for complex and lengthy procedures could significantly reduce staff radiation exposure.
Because It Can Enable Novel Procedures
We believe that the soft tissue visualization afforded by MRI can facilitate novel procedures that cannot be performed using X-ray fluoroscopy, in particular interventions that violate vascular boundaries. These novel interventions mandate visualization of the interaction between the device and each tissue traversed to avoid important structures and to monitor for complications. Pre-clinical examples include direct closed chest beating-heart transthoracic access to the right and left ventricles to deliver large devices [17, 18], transcatheter extra-anatomic “bidirectional cavopulmonary” shunt (Ratnayaka et al. 2015, under review), and closed chest transthoracic VSD repair [19].
Pre-Clinical Applications and Challenges to Clinical Translation
The following MR-guided interventions have been performed in animals: aortic coarctation, aneurysm, and dissection repairs [20–22]; atrial septal defect, ventricular septal defect, and patent foramen ovale closures [23, 24, 19]; atrial trans-septal puncture and balloon septostomy [25]; inferior vena cava filter deployment and retrieval [26, 27]; iliac, renal, and carotid artery stenting [28–30]; renal and hepatic embolization [31, 32]; and transcatheter pulmonary artery and aortic valve implantation [33, 34]. Although coronary catheterization and intervention have been described in animals [35, 36], the spatial resolution of MRI compares unfavorably with X-ray fluoroscopy and MR-guided coronary intervention appears unrealistic at present.
Most diagnostic and guiding X-ray catheters and device delivery systems contain steel braiding to impart torquability and kink resistance. Although the most commonly used 316L steel is not strongly attracted by magnetic fields, it causes severe MR imaging artifacts. Simply removing the braiding is not a solution because this usually destroys the mechanical properties of the catheters or devices and has the unfortunate side effect of rendering them MRI invisible. It is therefore necessary to replace the steel parts with other materials, for example metals such as nitinol or titanium, or alternatively polymers. The issue of MR visibility can be resolved through “passive” or “active” tracking. “Passive” tracking relies on intrinsic material properties under MRI. Markers on the device create a dark signal void (e.g., iron oxide paint) [37]. Although simple, this approach is limited because signals can be confused with anatomic structures and rely on markers being in the selected imaging plane. “Active” tracking by incorporating coils or antennae into devices is our preferred approach [38–41]. Devices are connected to the scanner hardware through appropriate circuitry and appear as color overlays on the real-time MR images. Conductive wires can resonate and heat during radiofrequency excitation for MRI [42], which is a potential challenge for both passive and active devices and is determined by the total length of the conductive wire, the inserted length within the body, and the position within the scanner bore [43]. Strategies to prevent device heating include incorporating coaxial chokes or transformers into the transmission line or using wireless resonators that do not require transmission lines [44–46].
An alternative approach is to limit heating by limiting the energy delivered by the imaging pulse sequence [47]. The excitation flip angle relates to heating quadratically, and lengthening the repetition time reduces heating proportionally [48]. Radial sampling, spiral sampling, and echo planar imaging use fewer excitation pulses and longer repetition times, and variable flip angle sequences [49] or parallel imaging can reduce the energy deposited per image. Each of these methods can reduce the heating with only a small penalty in image quality. Methods being developed to reduce SAR at high fields, such as adapted parallel transmission, may also be applicable to reduce heating in MRI-guided interventions [50].
Complexity of device engineering has limited their commercial availability and remains the chief hurdle to widespread adoption of iCMR and to clinical translation of more complex interventions. Nonetheless, some existing interventional devices such as angioplasty balloons and non-braided vascular introducer sheaths are inherently MR-safe and could be used safely if a suitable guidewire was available. Several teams have therefore sought to develop MR-conditional or intrinsically MR-safe guidewires as a means of facilitating procedures. Early attempts to develop a polymer guidewire were abandoned because of the difficulty of reproducing the necessary strength and torquability of a metal guidewire [51]. Other designs are currently being evaluated. Active conductive guidewires have been tested in humans, but early prototypes did not have a clearly conspicuous tip and probably heated [52]. Although it is possible to estimate heating patterns, it is important to ensure that these predictions are born out in vivo. To monitor for significant heating, we embedded a fiber-optic temperature probe into a 0.035-in. active guidewire with similar mechanical properties to commercial X-ray guidewires [53]. Heating was negligible in vivo under normal operating conditions. The whole shaft is active, and the tip has a distinct signal which is critical when navigating the vasculature [54]. We plan to test this guidewire in human subjects once US regulatory approval is received.
iCMR Applications Today
The engineering challenge of designing devices that are safe for use in the MR environment has delayed clinical translation of many promising pre-clinical interventions. However, there have been some notable advances made in recent years. MR-conditional electroanatomic mapping and ablation systems are now in clinical testing, and clinicians have worked around the constraints of operating in the MRI environment by using non-ferromagnetic inherently MR-safe catheters to perform simple procedures.
Diagnostic MRI Catheterization
Several institutions have adopted invasive cardiac catheterization under MR guidance [55, 56, 6•]. Since we published our experience at NIH in 2012, we have performed nearly 100 procedures and MRI catheterization has been reclassified as a standard procedure in our hospital. To perform MRI-guided right heart catheterization, we fill the balloon at the tip of a commercial non-braided balloon wedge end-hole catheter (Cook, Medtronic, Vascor, or Arrow) with 1 % dilute gadolinium. The balloon then appears as a white ball on the image and can then be navigated through the chambers of the heart with standard catheter maneuvers using real-time MR imaging (Fig. 2). Using saturation pre-pulses, the white ball can be visualized in thick-slab images easily should it move out of the selected thin plane. Pre-specified anatomical views are saved as “roadmaps” that can be called up as the catheter is manipulated from one chamber to another (e.g., bi-caval, tricuspid valve, pulmonary artery bifurcation). Hemodynamic parameters, such as pulmonary vascular resistance or pulmonary artery compliance, calculated from invasive pressures and MRI flow measurements are more accurate than traditional methods using thermodilution or the Fick principle to measure cardiac output [57•, 58]. Provocative testing with exercise or IV fluid challenge can be useful to unmask latent symptoms and pathologic findings [59]. By streamlining scanning protocols, we perform repeated invasive and MRI measurements under three different physiologic conditions in approximately 1 h. Additional MRI sequences to screen for specific pathologies can be incorporated into the protocol—e.g., pulmonary perfusion to assess for chronic thromboembolic disease [60] or late gadolinium enhancement to identify myocardial scar or fibrosis.
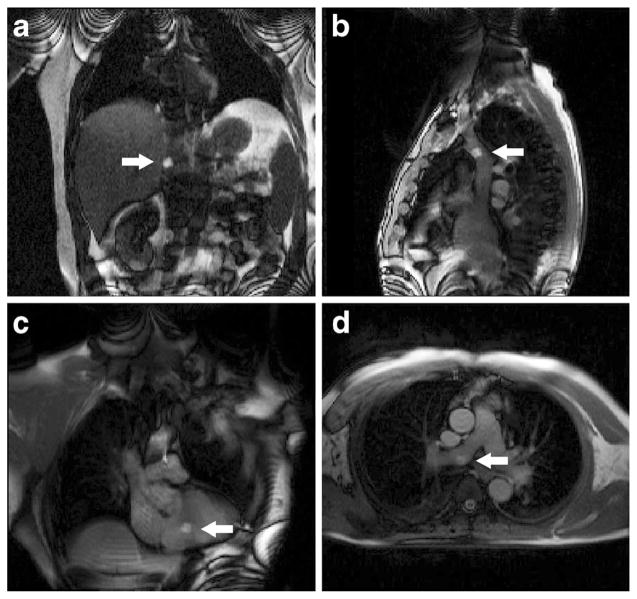
Fig. 2.
Clinical MRI right heart catheterization. The gadolinium-filled balloon at the tip of the catheter is visible as a white ball (arrows) in the inferior vena cava (a), superior vena cava (b), right ventricle (c), and right pulmonary artery (d)
Electroanatomic Mapping and Ablation
X-ray fluoroscopic guidance cannot visualize important anatomic landmarks or precisely locate catheters in three dimensions. Neither does X-ray permit visualization of infarcted regions of the myocardium or ablation lesions. These limitations currently result in long electrophysiology procedure times, excess fluoroscopy exposure, and a high rate of arrhythmia recurrence. The ability to accurately position catheters in three dimensions is particularly attractive for complex electrophysiology interventions. Currently, maps of the endocardial surface are generated through electroanatomic mapping, which can be time consuming. Co-registration of pre-acquired volumes from CT or MRI with these maps may reduce fluoroscopy and procedure time. Volumes incorporating additional functional information such as infarct distribution from late gadolinium enhancement (LGE) MRI provide incremental information. Procedural success defined by arrhythmia termination remains relatively low for atrial fibrillation and ventricular tachycardia ablation, almost certainly because of incomplete ablation. The need for better ablation imaging has been recognized in current guidelines [61]. MRI can enable visualization of ablation lesions with T2-weighted, T1 intrinsic contrast, or LGE sequences [62–66]. If gaps in ablation lines can be visualized, then they can be ablated [67, 68]. There is evidence that the extent of LGE post-ablation correlates with procedural success defined by rate of arrhythmia recurrence [69].
Electroanatomic mapping and ablation systems for use inside the MRI scanner are now available for clinical investigation (Imricor, MRI Interventions). Using these systems, pre-clinical feasibility of electroanatomic mapping and ablation of the left ventricle [8], pulmonary veins and cavo-tricuspid isthmus [70, 71], and MR-guided cannulation of the coronary sinus [72] have been described. In recent years, electroanatomic mapping and ablation of atrial arrhythmias in humans have been reported [73–75], which represents an important milestone in the clinical translation of iCMR (Fig. 3).
Fig. 3.
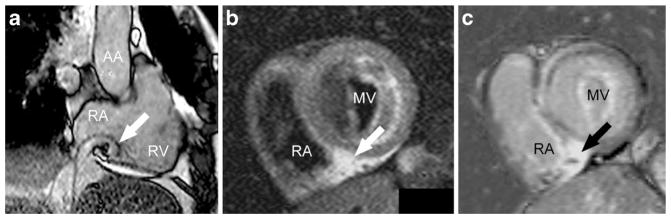
Clinical MR-guided electroanatomic mapping and ablation. a Real-time MR imaging of the electroanatomic mapping and ablation catheter. The passively tracked tip (arrow) is positioned above the cavo-tricuspid isthmus. Post-ablation T2-weighted (b) and late gadolinium enhancement (c) images of the cavo-tricuspid isthmus showing the ablation lesion (arrows). AA ascending aorta, MV mitral valve, RA right atrium, RV right ventricle. (Courtesy of M. Gutberlet, M. Grothoff and G. Hindricks (2014), University of Leipzig, Germany)
Structural Interventions
Some structural iCMR procedures have already been performed in humans, including aortic co-arctation angioplasty [76], femoral and popliteal artery angio-plasty [77], and pulmonary valvuloplasty [51]. But widespread clinical adoption has been delayed by the unavailability of commercial guidewires, catheters, and devices for use in the MR environment. In the interim, peri-procedural MR could be used for advanced hemodynamic assessment of X-ray-guided structural interventions, for example to measure pulmonary regurgitant fraction and right ventricular stroke volume after percutaneous pulmonary valve implantation in patients with congenital right ventricular outflow tract obstruction [78].
How Can I Do iCMR?
How to Build an iCMR Suite
To date, most existing iCMR suites have been built alongside X-ray fluoroscopy labs to permit “bailout” should complications arise in MRI. Options for construction include single room [79], moveable [80], or separate room localized systems. Placing MRI and X-ray in separate rooms allows both to be used independently and maximize usage. However, as experience grows and complications are shown to be rare and manageable within—or just outside—the MRI room, we anticipate this co-localization to become unnecessary. This means that any MRI room can be converted into an interventional suite. Analogy can be drawn with the first percutaneous coronary interventions, for which cardiothoracic surgical teams and operating rooms were kept on standby. Today, coronary interventions are performed in hospitals around the world without cardiothoracic surgery on site.
Incremental physical hardware requirements are surprisingly few. All major MR system manufacturers offer real-time imaging capability with interactive slice prescription during continuous scanning. At NIH, we built a dedicated platform with specialist iCMR functions including active device color overlays [81], but similar programs are available (Interventional Front End, Siemens; RTHawk, HeartVista; Cleartrace, MRI Intervention; iSuite, Philips). A noise-cancelling communication system is needed so that operators and nursing staff within the MRI room can communicate with the team outside and with the patient in the bore while scanning. Such systems are now commercially available from several manufacturers (Optoacoustics, Innovere). LCD monitors or projectors are required within the MRI room to display images and hemodynamics to the operator. These are also available commercially in the form of MR-conditional LCD monitors or radiofrequency-shielded boxes for LCD projectors (Gaven Industries). MR-conditional hemodynamic monitoring systems are available (Invivo, GE, Medrad) and are sufficient for basic monitoring. However, there are currently no commercial high-fidelity hemodynamic recording systems. Custom systems can be built for research purposes using filters to correct for interference from the scanner and fiber-optic cables or wireless systems to transmit signals out of the room, and using research acquisition hardware (National Instruments, ADInstruments, Biopac), but a commercial system—preferably integrated into conventional catheterization laboratory hemodynamic analysis systems (e.g., Siemens Sensis, GE Mac-Lab)—remains under development (Pinmed). It is possible to manage intubated and ventilated patients, because MR-conditional anesthesia machines and infusion pumps are commercially available.
In addition to a standard catheterization laboratory team of physician operators, nurses, and technologists, iCMR requires one extra staff member—the MR technologist—to drive the scanner during procedures.
Safety Considerations
It is critical to ensure that no ferromagnetic objects that could become projectiles be accidentally moved from X-ray into the MRI room during patient transfer. At NIH, we require two independent staff members to perform a visual inspection of the operative field and table before transfer. Completing a safety checklist to ensure all ferromagnetic tools are clear before transfer is also advised. Hemodynamic monitoring should be continuous during transfer—or only suspended briefly—while transferring from one monitoring system to another.
It is also important to plan for emergencies. Code team members arriving from other parts of the hospital should be diverted away from the MRI room until the patient is safely transferred back to an adjacent “safe” room by the primary team. In our lab, this is the X-ray laboratory but could easily be a patient recovery area. Currently, available defibrillators are not safe for use in the MRI environment. If ventricular tachycardia or fibrillation occurs, then the patient must be evacuated from the magnetic field to an adjacent room for defibrillation. At NIH, we drill evacuations quarterly and can consistently evacuate a patient from the scanner and defibrillate a patient within less than 1 min. In the future, MR-conditional defibrillators should enable defibrillation inside the MRI scanner.
Future Applications
All of the interventions performed in pre-clinical experiments to date are theoretically possible in humans. The limiting factor remains availability of commercially available guidewires, catheters, and devices. A number of institutions and commercial entities are now working on passive or active devices, which would represent a major leap forwards to facilitate increasingly complex interventions. In the future, we anticipate growing interest in iCMR electrophysiology studies and ablation, because the potential to reduce procedure time, ionizing radiation exposure, and arrhythmia recurrence is compelling.
A specific example of an intervention to which iCMR could add real value is endomyocardial biopsy, which has fallen out of favor in recent years, mostly because of low diagnostic yield [82]. This is almost certainly in part because many cardiomyopathies affect the myocardium in a heterogeneous pattern. Nonetheless, biopsy remains a key tool in the investigation of unexplained heart failure [83]. LGE MRI is widely accepted as the best imaging modality to assess for fibrosis and infiltration [84], and we hypothesize that MRI-guided targeted biopsy could greatly enhance the diagnostic yield. Several groups are working to develop MR-conditional bioptomes for this purpose.
Conclusions
iCMR is finally transitioning from research interest to clinical tool. We do not advocate MRI guidance for all cardiovascular procedures but rather for select structural heart and electro-physiology interventions where the additional functional and anatomic information afforded by MRI, including real-time visualization of soft tissues and three-dimensional structures, is important. We recommend that new centers considering iCMR should first start with simple procedures such as MRI right heart catheterization to gain experience of working in the MR environment. We anticipate that as guidewires, catheters, electroanatomic mapping system, and interventional devices become commercially available, more complex and innovative interventions will be possible.
Acknowledgments
This work was supported by the Division of Intramural Research, National Heart Lung and Blood Institute, National Institutes of Health (Z01-HL005062).
We thank Kanishka Ratnayaka for thoughtful comments and Anthony Faranesh, Michael Hansen, and Adrienne Campbell-Washburn for their help with technical aspects of iCMR.
Footnotes
Conflict of Interest Toby Rogers and Robert J. Lederman are full-time employees of NHLBI, NIH.
Robert J. Lederman is a co-inventor on patents, assigned to NIH, for catheter devices to be used under MR guidance.
Compliance with Ethics Guidelines
Human and Animal Rights and Informed Consent All human subjects provided informed consent. This article does not contain any studies with animal subjects.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
- 1.de Silva R, Gutierrez LF, Raval AN, McVeigh ER, Ozturk C, Lederman RJ. X-ray fused with magnetic resonance imaging (XFM) to target endomyocardial injections: validation in a swine model of myocardial infarction. Circulation. 2006;114(22):2342–50. doi: 10.1161/CIRCULATIONAHA.105.598524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dori Y, Sarmiento M, Glatz AC, Gillespie MJ, Jones VM, Harris MA, et al. X-ray magnetic resonance fusion to internal markers and utility in congenital heart disease catheterization. Circ: Cardiovascular Imaging. 2011;4(4):415–24. doi: 10.1161/circimaging.111.963868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Faranesh AZ, Kellman P, Ratnayaka K, Lederman RJ. Integration of cardiac and respiratory motion into MRI roadmaps fused with x-ray. Med Phys. 2013;40(3):032302. doi: 10.1118/1.4789919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abu Hazeem AA, Dori Y, Whitehead KK, Harris MA, Fogel MA, Gillespie MJ, et al. X-ray magnetic resonance fusion modality may reduce radiation exposure and contrast dose in diagnostic cardiac catheterization of congenital heart disease. Catheter Cardiovasc Interv. 2014 doi: 10.1002/ccd.25473. [DOI] [PubMed] [Google Scholar]
- 5.Avula S, Mallucci CL, Pizer B, Garlick D, Crooks D, Abernethy LJ. Intraoperative 3-Tesla MRI in the management of paediatric cranial tumours–initial experience. Pediatr Radiol. 2012;42(2):158–67. doi: 10.1007/s00247-011-2261-6. [DOI] [PubMed] [Google Scholar]
- 6•.Ratnayaka K, Faranesh AZ, Hansen MS, Stine AM, Halabi M, Barbash IM, et al. Real-time MRI-guided right heart catheterization in adults using passive catheters. Eur Heart J. 2013;34(5):380–9. doi: 10.1093/eurheartj/ehs189. This paper shows that MRI right heart catheterization can be implemented into a clinically-realistic workflow for standard clinical practice. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rogers T, Ratnayaka K, Lederman RJ. MRI catheterization in car-diopulmonary disease. Chest. 2014;145(1):30–6. doi: 10.1378/chest.13-1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dukkipati SR, Mallozzi R, Schmidt EJ, Holmvang G, d’Avila A, Guhde R, et al. Electroanatomic mapping of the left ventricle in a porcine model of chronic myocardial infarction with magnetic resonance-based catheter tracking. Circulation. 2008;118(8):853–62. doi: 10.1161/CIRCULATIONAHA.107.738229. [DOI] [PubMed] [Google Scholar]
- 9.Yutzy SR, Duerk JL. Pulse sequences and system interfaces for interventional and real-time MRI. J Magn Resonance Imaging: JMRI. 2008;27(2):267–75. doi: 10.1002/jmri.21268. [DOI] [PubMed] [Google Scholar]
- 10.Pruessmann KP, Weiger M, Scheidegger MB, Boesiger P. SENSE: sensitivity encoding for fast MRI. Magn Resonance Med: Off J Soc Magn Resonance Med/Soc Magn Resonance Med. 1999;42(5):952–62. [PubMed] [Google Scholar]
- 11.Kellman P, Epstein FH, McVeigh ER. Adaptive sensitivity encoding incorporating temporal filtering (TSENSE) Magn Resonance Med: Off J Soc Magn Resonance Med/Soc Magn Resonance Med. 2001;45(5):846–52. doi: 10.1002/mrm.1113. [DOI] [PubMed] [Google Scholar]
- 12.Griswold MA, Jakob PM, Heidemann RM, Nittka M, Jellus V, Wang J, et al. Generalized autocalibrating partially parallel acquisitions (GRAPPA) Magn Resonance Med: Off J Soc Magn Resonance Med/Soc Magn Resonance Med. 2002;47(6):1202–10. doi: 10.1002/mrm.10171. [DOI] [PubMed] [Google Scholar]
- 13.Johnson JN, Hornik CP, Li JS, Benjamin DK, Jr, Yoshizumi TT, Reiman RE, et al. Cumulative radiation exposure and cancer risk estimation in children with heart disease. Circulation. 2014;130(2):161–7. doi: 10.1161/CIRCULATIONAHA.113.005425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fratz S, Chung T, Greil G, Samyn M, Taylor A, Valsangiacomo Buechel E, et al. Guidelines and protocols for cardiovascular magnetic resonance in children and adults with congenital heart disease: SCMR expert consensus group on congenital heart disease. J Cardiovasc Magn Reson. 2013;15(1):51. doi: 10.1186/1532-429X-15-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Venneri L, Rossi F, Botto N, Andreassi MG, Salcone N, Emad A, et al. Cancer risk from professional exposure in staff working in cardiac catheterization laboratory: insights from the National Research Council’s Biological Effects of Ionizing Radiation VII Report. Am Heart J. 2009;157(1):118–24. doi: 10.1016/j.ahj.2008.08.009. [DOI] [PubMed] [Google Scholar]
- 16.Chambers CE, Fetterly KA, Holzer R, Lin PJ, Blankenship JC, Balter S, et al. Radiation safety program for the cardiac catheterization laboratory. Catheterization Cardiovascular Interv: Off J Soc Cardiac Angiography Interv. 2011;77(4):546–56. doi: 10.1002/ccd.22867. [DOI] [PubMed] [Google Scholar]
- 17.Barbash IM, Saikus CE, Faranesh AZ, Ratnayaka K, Kocaturk O, Chen MY, et al. Direct percutaneous left ventricular access and port closure: pre-clinical feasibility. J Am Coll Cardiol Intv. 2011;4(12):1318–25. doi: 10.1016/j.jcin.2011.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Halabi M, Ratnayaka K, Faranesh AZ, Hansen MS, Barbash IM, Eckhaus MA, et al. Transthoracic delivery of large devices into the left ventricle through the right ventricle and interventricular septum: preclinical feasibility. J Cardiovascular Magn Resonance: Off J Soc Cardiovascular Magn Resonance. 2013;15(1):10. doi: 10.1186/1532-429X-15-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ratnayaka K, Saikus CE, Faranesh AZ, Bell JA, Barbash IM, Kocaturk O, et al. Closed-chest transthoracic magnetic resonance imaging-guided ventricular septal defect closure in swine. J Am Coll Cardiol Intv. 2011;4(12):1326–34. doi: 10.1016/j.jcin.2011.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Raval AN, Telep JD, Guttman MA, Ozturk C, Jones M, Thompson RB, et al. Real-time magnetic resonance imaging-guided stenting of aortic coarctation with commercially available catheter devices in swine. Circulation. 2005;112(5):699–706. doi: 10.1161/CIRCULATIONAHA.105.542647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Raman VK, Karmarkar PV, Guttman MA, Dick AJ, Peters DC, Ozturk C, et al. Real-time magnetic resonance-guided endovascular repair of experimental abdominal aortic aneurysm in swine. J Am Coll Cardiol. 2005;45(12):2069–77. doi: 10.1016/j.jacc.2005.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eggebrecht H, Kuhl H, Kaiser GM, Aker S, Zenge MO, Stock F, et al. Feasibility of real-time magnetic resonance-guided stent-graft placement in a swine model of descending aortic dissection. Eur Heart J. 2006;27(5):613–20. doi: 10.1093/eurheartj/ehi732. [DOI] [PubMed] [Google Scholar]
- 23.Buecker A, Spuentrup E, Grabitz R, Freudenthal F, Muehler E, Schaeffter T, et al. Magnetic resonance-guided placement of atrial septal closure device in animal model of patent foramen ovale. Circulation. 2002;106:511–5. doi: 10.1161/01.cir.0000023621.88708.62. [DOI] [PubMed] [Google Scholar]
- 24.Rickers C, Jerosch-Herold M, Hu X, Murthy N, Wang X, Kong H, et al. Magnetic resonance image-guided transcatheter closure of atrial septal defects. Circulation. 2003;107(1):132–8. doi: 10.1161/01.cir.0000039343.95540.cf. [DOI] [PubMed] [Google Scholar]
- 25.Raval AN, Karmarkar PV, Guttman MA, Ozturk C, Desilva R, Aviles RJ, et al. Real-time MRI guided atrial septal puncture and balloon septostomy in swine. Catheterization Cardiovascular Interv: Off J Soc Cardiac Angiography Interv. 2006;67(4):637–43. doi: 10.1002/ccd.20579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bucker A, Neuerburg JM, Adam GB, Glowinski A, Schaeffter T, Rasche V, et al. Real-time MR guidance for inferior vena cava filter placement in an animal model. J Vascular Interv Radiol: JVIR. 2001;12(6):753–6. doi: 10.1016/s1051-0443(07)61448-1. [DOI] [PubMed] [Google Scholar]
- 27.Shih MC, Rogers WJ, Bonatti H, Hagspiel KD. Real-time MR-guided retrieval of inferior vena cava filters: an in vitro and animal model study. J Vascular Interv Radiol: JVIR. 2011;22(6):843–50. doi: 10.1016/j.jvir.2011.01.428. [DOI] [PubMed] [Google Scholar]
- 28.Buecker A, Neuerburg JM, Adam GB, Glowinski A, Schaeffter T, Rasche V, et al. Real-time MR fluoroscopy for MR-guided iliac artery stent placement. J Magn Resonance Imaging: JMRI. 2000;12(4):616–22. doi: 10.1002/1522-2586(200010)12:4<616::aid-jmri15>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 29.Feng L, Dumoulin CL, Dashnaw S, Darrow RD, Delapaz RL, Bishop PL, et al. Feasibility of stent placement in carotid arteries with real-time MR imaging guidance in pigs. Radiology. 2005;234(2):558–62. doi: 10.1148/radiol.2341031950. [DOI] [PubMed] [Google Scholar]
- 30.Elgort DR, Hillenbrand CM, Zhang S, Wong EY, Rafie S, Lewin JS, et al. Image-guided and -monitored renal artery stenting using only MRI. J Magn Resonance Imaging: JMRI. 2006;23(5):619–27. doi: 10.1002/jmri.20554. [DOI] [PubMed] [Google Scholar]
- 31.Fink C, Bock M, Umathum R, Volz S, Zuehlsdorff S, Grobholz R, et al. Renal embolization: feasibility of magnetic resonance-guidance using active catheter tracking and intraarterial magnetic resonance angiography. Investig Radiol. 2004;39(2):111–9. doi: 10.1097/01.rli.0000110744.70512.df. [DOI] [PubMed] [Google Scholar]
- 32.Seppenwoolde JH, Bartels LW, van der Weide R, Nijsen JF, van het Schip AD, Bakker CJ. Fully MR-guided hepatic artery catheterization for selective drug delivery: a feasibility study in pigs. J Magn Resonance Imaging: JMRI. 2006;23(2):123–9. doi: 10.1002/jmri.20479. [DOI] [PubMed] [Google Scholar]
- 33.Kuehne T, Saeed M, Higgins CB, Gleason K, Krombach GA, Weber OM, et al. Endovascular stents in pulmonary valve and artery in swine: feasibility study of MR imaging-guided deployment and postinterventional assessment. Radiology. 2003;226(2):475–81. doi: 10.1148/radiol.2262011639. [DOI] [PubMed] [Google Scholar]
- 34.Kahlert P, Parohl N, Albert J, Schafer L, Reinhardt R, Kaiser GM, et al. Real-time magnetic resonance imaging-guided transarterial aortic valve implantation: in vivo evaluation in swine. J Am Coll Cardiol. 2012;59(2):192–3. doi: 10.1016/j.jacc.2011.09.046. [DOI] [PubMed] [Google Scholar]
- 35.Spuentrup E, Ruebben A, Schaeffter T, Manning WJ, Gunther RW, Buecker A. Magnetic resonance–guided coronary artery stent placement in a swine model. Circulation. 2002;105(7):874–9. doi: 10.1161/hc0702.104165. [DOI] [PubMed] [Google Scholar]
- 36.Omary RA, Green JD, Schirf BE, Li Y, Finn JP, Li D. Real-time magnetic resonance imaging-guided coronary catheterization in swine. Circulation. 2003;107(21):2656–9. doi: 10.1161/01.CIR.0000074776.88681.F5. [DOI] [PubMed] [Google Scholar]
- 37.Unal O, Li J, Cheng W, Yu H, Strother CM. MR-visible coatings for endovascular device visualization. J Magn Resonance Imaging: JMRI. 2006;23(5):763–9. doi: 10.1002/jmri.20555. [DOI] [PubMed] [Google Scholar]
- 38.Dumoulin CL, Souza SP, Darrow RD. Real-time position monitoring of invasive devices using magnetic resonance. Magn Resonance Med: Off J Soc Magn Resonance Med/Soc Magn Resonance Med. 1993;29(3):411–5. doi: 10.1002/mrm.1910290322. [DOI] [PubMed] [Google Scholar]
- 39.Ladd ME, Zimmermann GG, Quick HH, Debatin JF, Boesiger P, von Schulthess GK, et al. Active MR visualization of a vascular guidewire in vivo. J Magn Resonance Imaging: JMRI. 1998;8(1):220–5. doi: 10.1002/jmri.1880080137. [DOI] [PubMed] [Google Scholar]
- 40.McKinnon GC, Debatin JF, Leung DA, Wildermuth S, Holtz DJ, von Schulthess GK. Towards active guidewire visualization in interventional magnetic resonance imaging. Magma. 1996;4(1):13–8. doi: 10.1007/BF01759775. [DOI] [PubMed] [Google Scholar]
- 41.Ocali O, Atalar E. Intravascular magnetic resonance imaging using a loopless catheter antenna. Magn Resonance Med: Off J Soc Magn Resonance Med/Soc Magn Resonance Med. 1997;37(1):112–8. doi: 10.1002/mrm.1910370116. [DOI] [PubMed] [Google Scholar]
- 42.Nitz W, Oppelt A, Renz W, Manke C, Lenhart M, Link J. On the heating of linear conductive structures as guide wires and catheters in interventional MRI. J Magn Resonance Imaging: JMRI. 2001;13:105–14. doi: 10.1002/1522-2586(200101)13:1<105::aid-jmri1016>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 43.Nordbeck P, Fidler F, Weiss I, Warmuth M, Friedrich MT, Ehses P, et al. Spatial distribution of RF-induced E-fields and implant heating in MRI. Magn Resonance Med: Off J Soc Magn Resonance Med/Soc Magn Resonance Med. 2008;60(2):312–9. doi: 10.1002/mrm.21475. [DOI] [PubMed] [Google Scholar]
- 44.Ladd ME, Quick HH. Reduction of resonant RF heating in intra-vascular catheters using coaxial chokes. Magn Resonance Med: Off J Soc Magn Resonance Med/Soc Magn Resonance Med. 2000;43(4):615–9. doi: 10.1002/(sici)1522-2594(200004)43:4<615::aid-mrm19>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 45.Weiss S, Vernickel P, Schaeffter T, Schulz V, Gleich B. Transmission line for improved RF safety of interventional devices. Magn Resonance Med: Off J Soc Magn Resonance Med/Soc Magn Resonance Med. 2005;54:182–9. doi: 10.1002/mrm.20543. [DOI] [PubMed] [Google Scholar]
- 46.Quick HH, Kuehl H, Kaiser G, Bosk S, Debatin JF, Ladd ME. Inductively coupled stent antennas in MRI. Magn Resonance Med: Off J Soc Magn Resonance Med/Soc Magn Resonance Med. 2002;48(5):781–90. doi: 10.1002/mrm.10269. [DOI] [PubMed] [Google Scholar]
- 47.Yeung C, Susil R, Atalar E. RF safety of wires in interventional MRI: using a safety index. Magn Resonance Med: Off J Soc Magn Resonance Med/Soc Magn Resonance Med. 2002;47:187–93. doi: 10.1002/mrm.10037. [DOI] [PubMed] [Google Scholar]
- 48.Armenean C, Perrin E, Armenean M, Beuf O, Pilleul F, Saint-Jalmes H. RF-induced temperature elevation along metallic wires in clinical magnetic resonance imaging: influence of diameter and length. Magn Resonance Med: Off J Soc Magn Resonance Med/Soc Magn Resonance Med. 2004;52(5):1200–6. doi: 10.1002/mrm.20246. [DOI] [PubMed] [Google Scholar]
- 49.Srinivasan S, Ennis DB. Variable flip angle balanced steady-state free precession for lower SAR or higher contrast cardiac cine imaging. Magn Resonance Med: Off J Soc Magn Resonance Med/Soc Magn Resonance Med. 2013 doi: 10.1002/mrm.24764. [DOI] [PubMed] [Google Scholar]
- 50.Wu X, Akgun C, Vaughan JT, Andersen P, Strupp J, Ugurbil K, et al. Adapted RF pulse design for SAR reduction in parallel excitation with experimental verification at 9.4 T. J Magn Reson. 2010;205(1):161–70. [PMC free article] [PubMed] [Google Scholar]
- 51.Tzifa A, Krombach GA, Kramer N, Kruger S, Schutte A, von Walter M, et al. Magnetic resonance-guided cardiac interventions using magnetic resonance-compatible devices: a preclinical study and first-in-man congenital interventions. Circ Cardiovasc Interv. 2010;3(6):585–92. doi: 10.1161/CIRCINTERVENTIONS.110.957209. [DOI] [PubMed] [Google Scholar]
- 52.Dick AJ, Raman VK, Raval AN, Guttman MA, Thompson RB, Ozturk C, et al. Invasive human magnetic resonance imaging during angioplasty: feasibility in a combined XMR suite. Catheterization Cardiovascular Interv: Off J Soc Cardiac Angiography Interv. 2005;64(3):265–74. doi: 10.1002/ccd.20302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sonmez M, Saikus CE, Bell JA, Franson DN, Halabi M, Faranesh AZ, et al. MRI active guidewire with an embedded temperature probe and providing a distinct tip signal to enhance clinical safety. J Cardiovascular Magn Resonance: Off J Soc Cardiovascular Magn Resonance. 2012;14:38. doi: 10.1186/1532-429X-14-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kocaturk O, Kim AH, Saikus CE, Guttman MA, Faranesh AZ, Ozturk C, et al. Active two-channel 0.035″ guidewire for interventional cardiovascular MRI. J Magn Resonance Imaging: JMRI. 2009;30(2):461–5. doi: 10.1002/jmri.21844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Razavi R, Hill DL, Keevil SF, Miquel ME, Muthurangu V, Hegde S, et al. Cardiac catheterisation guided by MRI in children and adults with congenital heart disease. Lancet. 2003;362(9399):1877–82. doi: 10.1016/S0140-6736(03)14956-2. [DOI] [PubMed] [Google Scholar]
- 56.Kuehne T, Yilmaz S, Schulze-Neick I, Wellnhofer E, Ewert P, Nagel E, et al. Magnetic resonance imaging guided catheterisation for assessment of pulmonary vascular resistance: in vivo validation and clinical application in patients with pulmonary hypertension. Heart. 2005;91(8):1064–9. doi: 10.1136/hrt.2004.038265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57•.Muthurangu V, Taylor A, Andriantsimiavona R, Hegde S, Miquel ME, Tulloh R, et al. Novel method of quantifying pulmonary vascular resistance by use of simultaneous invasive pressure monitoring and phase-contrast magnetic resonance flow. Circulation. 2004;110(7):826–34. doi: 10.1161/01.CIR.0000138741.72946.84. This is a seminal demonstration of the enhanced accuracy of MRI catheterization over conventional indicator-dilution techniques for measuring blood flow required to determine pulmonary vascular resistance. [DOI] [PubMed] [Google Scholar]
- 58.Muthurangu V, Atkinson D, Sermesant M, Miquel ME, Hegde S, Johnson R, et al. Measurement of total pulmonary arterial compliance using invasive pressure monitoring and MR flow quantification during MR-guided cardiac catheterization. Am J Phys Heart Circ Phys. 2005;289(3):H1301–6. doi: 10.1152/ajpheart.00957.2004. [DOI] [PubMed] [Google Scholar]
- 59.Nishimura RA, Carabello BA. Hemodynamics in the cardiac catheterization laboratory of the 21st century. Circulation. 2012;125(17):2138–50. doi: 10.1161/CIRCULATIONAHA.111.060319. [DOI] [PubMed] [Google Scholar]
- 60.Ohno Y, Hatabu H, Murase K, Higashino T, Nogami M, Yoshikawa T, et al. Primary pulmonary hypertension: 3D dynamic perfusion MRI for quantitative analysis of regional pulmonary perfusion. AJR Am J Roentgenol. 2007;188(1):48–56. doi: 10.2214/AJR.05.0135. [DOI] [PubMed] [Google Scholar]
- 61.Blomström Lundqvist C, Auricchio A, Brugada J, Boriani G, Bremerich J, Cabrera JA, et al. The use of imaging for electrophys-iological and devices procedures: a report from the first European Heart Rhythm Association Policy Conference, jointly organized with the European Association of Cardiovascular Imaging (EACVI), the Council of Cardiovascular Imaging and the European Society of Cardiac Radiology. Europace: European pacing, arrhythmias, and cardiac electrophysiology: journal of the working groups on cardiac pacing, arrhythmias, and cardiac cellular electrophysiology of the European Society of Cardiology. 2013;15(7):927–36. doi: 10.1093/europace/eut084. [DOI] [PubMed] [Google Scholar]
- 62.Lardo AC, McVeigh ER, Jumrussirikul P, Berger RD, Calkins H, Lima J, et al. Visualization and temporal/spatial characterization of cardiac radiofrequency ablation lesions using magnetic resonance imaging. Circulation. 2000;102(6):698–705. doi: 10.1161/01.cir.102.6.698. [DOI] [PubMed] [Google Scholar]
- 63.Dickfeld T, Kato R, Zviman M, Lai S, Meininger G, Lardo AC, et al. Characterization of radiofrequency ablation lesions with gadolinium-enhanced cardiovascular magnetic resonance imaging. J Am Coll Cardiol. 2006;47(2):370–8. doi: 10.1016/j.jacc.2005.07.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Arujuna A, Karim R, Caulfield D, Knowles B, Rhode K, Schaeffter T, et al. Acute pulmonary vein isolation is achieved by a combination of reversible and irreversible atrial injury after catheter ablation: evidence from magnetic resonance imaging. Circ: Arrhythmia Electrophysiol. 2012;5(4):691–700. doi: 10.1161/circep.111.966523. [DOI] [PubMed] [Google Scholar]
- 65.Harrison JL, Jensen HK, Peel SA, Chiribiri A, Grøndal AK, Bloch LØ, et al. Cardiac magnetic resonance and electroanatomical mapping of acute and chronic atrial ablation injury: a histological validation study. Eur Heart J. 2014 doi: 10.1093/eurheartj/eht560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Celik H, Ramanan V, Barry J, Ghate S, Leber V, Oduneye S, et al. Intrinsic contrast for characterization of acute radiofrequency ablation lesions. Circ Arrhythmia Electrophysiol. 2014 doi: 10.1161/CIRCEP.113.001163. [DOI] [PubMed] [Google Scholar]
- 67.Ranjan R, Kato R, Zviman MM, Dickfeld TM, Roguin A, Berger RD, et al. Gaps in the ablation line as a potential cause of recovery from electrical isolation and their visualization using MRI. Circ Arrhythmia Electrophysiol. 2011;4(3):279–86. doi: 10.1161/CIRCEP.110.960567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ranjan R, Kholmovski EG, Blauer J, Vijayakumar S, Volland NA, Salama ME, et al. Identification and acute targeting of gaps in atrial ablation lesion sets using a real-time magnetic resonance imaging system. Circ Arrhythmia Electrophysiol. 2012;5(6):1130–5. doi: 10.1161/CIRCEP.112.973164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Peters DC, Wylie JV, Hauser TH, Nezafat R, Han Y, Woo JJ, et al. Recurrence of atrial fibrillation correlates with the extent of post-procedural late gadolinium enhancement: a pilot study. J Am Coll Cardiol Img. 2009;2(3):308–16. doi: 10.1016/j.jcmg.2008.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hoffmann BA, Koops A, Rostock T, Mullerleile K, Steven D, Karst R, et al. Interactive real-time mapping and catheter ablation of the cavotricuspid isthmus guided by magnetic resonance imaging in a porcine model. Eur Heart J. 2010;31(4):450–6. doi: 10.1093/eurheartj/ehp460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ganesan AN, Selvanayagam JB, Mahajan R, Grover S, Nayyar S, Brooks AG, et al. Mapping and ablation of the pulmonary veins and cavo-tricuspid isthmus with a magnetic resonance imaging-compatible externally irrigated ablation catheter and integrated elec-trophysiology system. Circ Arrhythmia Electrophysiol. 2012;5(6):1136–42. doi: 10.1161/CIRCEP.112.974436. [DOI] [PubMed] [Google Scholar]
- 72.Neizel M, Kramer N, Schutte A, Schnackenburg B, Kruger S, Kelm M, et al. Magnetic resonance imaging of the cardiac venous system and magnetic resonance-guided intubation of the coronary sinus in swine: a feasibility study. Investig Radiol. 2010;45(8):502–6. doi: 10.1097/RLI.0b013e3181e45578. [DOI] [PubMed] [Google Scholar]
- 73.Nazarian S, Kolandaivelu A, Zviman MM, Meininger GR, Kato R, Susil RC, et al. Feasibility of real-time magnetic resonance imaging for catheter guidance in electrophysiology studies. Circulation. 2008;118(3):223–9. doi: 10.1161/CIRCULATIONAHA.107.742452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Eitel C, Piorkowski C, Hindricks G, Gutberlet M. Electrophysiology study guided by real-time magnetic resonance imaging. Eur Heart J. 2012;33(15):1975. doi: 10.1093/eurheartj/ehr414. [DOI] [PubMed] [Google Scholar]
- 75.Grothoff M, Piorkowski C, Eitel C, Gaspar T, Lehmkuhl L, Lucke C, et al. MR imaging-guided electrophysiological ablation studies in humans with passive catheter tracking: initial results. Radiology. 2014;271(3):695–702. doi: 10.1148/radiol.13122671. [DOI] [PubMed] [Google Scholar]
- 76.Krueger JJ, Ewert P, Yilmaz S, Gelernter D, Peters B, Pietzner K, et al. Magnetic resonance imaging-guided balloon angioplasty of coarctation of the aorta: a pilot study. Circulation. 2006;113(8):1093–100. doi: 10.1161/CIRCULATIONAHA.105.578112. [DOI] [PubMed] [Google Scholar]
- 77.Paetzel C, Zorger N, Bachthaler M, Hamer OW, Stehr A, Feuerbach S, et al. Magnetic resonance-guided percutaneous angioplasty of femoral and popliteal artery stenoses using real-time imaging and intra-arterial contrast-enhanced magnetic resonance angiography. Investig Radiol. 2005;40(5):257–62. doi: 10.1097/01.rli.0000159876.09033.2e. [DOI] [PubMed] [Google Scholar]
- 78.Lurz P, Nordmeyer J, Muthurangu V, Khambadkone S, Derrick G, Yates R, et al. Comparison of bare metal stenting and percutaneous pulmonary valve implantation for treatment of right ventricular outflow tract obstruction: use of an x-ray/magnetic resonance hybrid laboratory for acute physiological assessment. Circulation. 2009;119(23):2995–3001. doi: 10.1161/CIRCULATIONAHA.108.836312. [DOI] [PubMed] [Google Scholar]
- 79.White MJ, Thornton JS, Hawkes DJ, Hill DL, Kitchen N, Mancini L, et al. Design, operation, and safety of single-room interventional MRI suites: practical experience from two centers. J Magn Resonance Imaging: JMRI. 2014 doi: 10.1002/jmri.24577. [DOI] [PubMed] [Google Scholar]
- 80.Hoult DI, Saunders JK, Sutherland GR, Sharp J, Gervin M, Kolansky HG, et al. The engineering of an interventional MRI with a movable 1.5 Tesla magnet. J Magn Resonance Imaging: JMRI. 2001;13(1):78–86. doi: 10.1002/1522-2586(200101)13:1<78::AID-JMRI1012>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 81.Guttman MA, Ozturk C, Raval AN, Raman VK, Dick AJ, DeSilva R, et al. Interventional cardiovascular procedures guided by real-time MR imaging: an interactive interface using multiple slices, adaptive projection modes and live 3D renderings. J Magn Resonance Imaging: JMRI. 2007;26(6):1429–35. doi: 10.1002/jmri.21199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Bennett MK, Gilotra NA, Harrington C, Rao S, Dunn JM, Freitag TB, et al. Evaluation of the role of endomyocardial biopsy in 851 patients with unexplained heart failure from 2000–2009. Circ: Heart Failure. 2013;6(4):676–84. doi: 10.1161/circheartfailure.112.000087. [DOI] [PubMed] [Google Scholar]
- 83.Leone O, Veinot JP, Angelini A, Baandrup UT, Basso C, Berry G, et al. 2011 consensus statement on endomyocardial biopsy from the Association for European Cardiovascular Pathology and the Society for Cardiovascular Pathology. Cardiovascular Pathol: Off J Soc Cardiovascular Pathol. 2012;21(4):245–74. doi: 10.1016/j.carpath.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 84.Hundley WG, Bluemke DA, Finn JP, Flamm SD, Fogel MA, Friedrich MG, et al. ACCF/ACR/AHA/NASCI/SCMR 2010 expert consensus document on cardiovascular magnetic resonance: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents. J Am Coll Cardiol. 2010;55(23):2614–62. doi: 10.1016/j.jacc.2009.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]