Abstract
As discoveries regarding the genetic contribution to disease have grown rapidly, health care professionals are expected to incorporate genetic and genomic perspectives into health education and practice. Genetic competencies common to all health professionals have been identified by the US National Coalition for Health Professional Education in Genetics (NCHPEG), which defined the knowledge, skills, and attitudes required to achieve these competencies. The aim of this study is to analyze genetic competencies of primary health care professionals in Brazil. It is a descriptive survey study, whereby doctors, nurses, and dentists were invited to participate by answering a questionnaire including 11 issues based on competencies established by the NCHPEG. Data were presented as percentages. Differences between groups of participants were assessed by the Fisher exact test, with the level of significance set at p < 0.05. Results showed that concerning knowledge, about 80 % of the participants recognized basic genetics terminology, but practitioners had difficulty in identifying patterns of inheritance. Regarding clinical skills, practitioners were able to recognize facial dysmorphias and identify situations where referral of patients to specialists was necessary. Nevertheless, there were challenges in the process of valuing and gathering information about family history. Regarding attitudes, 68.9 % of the participants thought about the comprehensiveness of care but faced challenges in counselling parents. The results of this study may contribute to developing an ongoing education program for primary health care professionals, leading to a strategy to overcome the challenges of including genetics in the Brazilian Unified Health System.
Keywords: Brazil, Unified Health System, Primary health care, Medical genetics, Clinical competence, Continuous professional development
Introduction
The Unified Health System (Sistema Único de Saúde, SUS) was created in 1988 in Brazil, and since then has undergone many developments with the aim of providing equitable access to comprehensive preventive and curative health care through region-based decentralized management and provision of services. The objective is also to promote community participation at all administrative and deliberative levels (Paim et al. 2011).
Expansion and qualification of Primary Healthcare (PHC) is seen as a fundamental policy to structure and strengthen the SUS and has been supported by the Ministry of Health over the last 20 years. Various financial and organizational strategies have been used to address this challenge, notably the Family Health Strategy (FHS). The FHS consolidates a model of community-oriented primary care run by a team of nurses, general practitioners, and community health workers. It includes comprehensive care, cultural competence, and social accountability, focusing on local family and community-based health care (Pinto et al. 2012). The FHS prioritizes coverage of vulnerable low-income populations and now reaches about 65 % of Brazilian citizens (more than 125 million people in August 2014).1
In January 2014, the Ministry of Health in Brazil established the National Policy on Comprehensive Care for People with Rare Diseases in the SUS. As 80 % of rare diseases have a genetic aetiology, this has created an opportunity to include genetics in the SUS. This policy assumes that health care should be integrated into a region-based context, structured both by primary and specialized health care services. PHC should be responsible for coordinating health care and carrying out long-term health care for the population that is registered under its responsibility, as well as being the principal point of access and point of care of genetic patients in the SUS network. PHC was also established by the policy as being responsible for nine initiatives and specific actions to promote health, early diagnosis, monitoring, patient follow-up, appropriate specialist referral, and care coordination, including at the family level. Specialized health care should consist of outpatient and hospital services that support and complement primary care services (Brasil 2014).
It is estimated that there are no more than 250 medical geneticists throughout the country, and undoubtedly, this small number of specialists is an obstacle and a challenge for a generalized implementation of specialized services in genetics (Horovitz et al. 2013; Melo and Sequeiros 2012; Novoa and Burnham 2011). In October 2014, the Brazilian Society of Medical Genetics registered 173 genetics specialist members: 157 (90.7 %) physicians, 10 (5.8 %) biologists, five (2.9 %) biomedical professionals, and one (0.6 %) biochemist. In addition to the small number of professionals, there is also a great disparity in their national distribution, as 94 (54.3 %) live in the Southeast, 36 (20.8 %) in the South, 18 (10.4 %) in the Midwest, 16 (9.3 %) in the Northeast region, and only nine (5.2 %) in the Northern region.2 The geographical distribution of genetics professionals and services relates to the population density and human development index, although in the more remote, poorer, and less densely populated areas (particularly in the North and Northeast), there is a greater shortage of professionals.
Reflecting the distribution of professionals, most centers and care genetic services are located in the South and Southeast regions of the country. These services are usually integrated into university and reference hospitals and provide medical care to thousands of individuals and families annually. Furthermore, they are considered as a point of reference at regional or national level. Some genetic services can also be found in hospitals that specialize in specific conditions such as diseases and disorders of the locomotive system and craniofacial anomalies. Several of these institutions have laboratory infrastructures and can also offer tests such as cytogenetic examinations and molecular biology techniques (Horovitz et al. 2013). Access to these services, however, is limited and inequitable, as the services are not organized in a network and are not linked with PHC.
Regarding training human resource personnel in medical genetics, there are only 11 Medical Genetics residency programs in the country, offering 22 new positions every year. At present, there are still no specific training courses for genetic counsellors. The Brazilian Coordination for the Improvement of Higher Education Personnel (CAPES, Coordenação de Aperfeiçoamento de Pessoal de Nível Superior) recognizes 43 graduate courses in Genetics: 20 Doctoral, 22 Master’s, and one professional Master’s program.3 Many of these courses have research trajectories related to human and/or medical genetics and are responsible for training professionals, both in the area of health and biological sciences. It is estimated that there are about 20 nurses working in the area, and most of them hold PhDs. At the moment, these nurses are attempting to set up a society for nurses in Genetics.4
Therefore, there is a shortage of specialists to organize specialized care, on the one hand, while on the other, primary care professionals are not trained sufficiently to deal with clinical situations involving rare genetic diseases. Primary care practitioners need to become “genetically literate” to deal with this issue. This is particularly important given the inclusion of genetics in primary health care, and particularly in the Family Health Strategy, is one of the key strategies linked to the National Policy on Comprehensive Care for People with Rare Diseases in the SUS.
Education to develop genetic care competence is crucial in translating the benefits of medical genetics and genomics to patients and their families. Competencies common to all health professionals have been identified by the US National Coalition for Health Professional Education in Genetics (NCHPEG), since 2007. They recommend that at a minimum, every health care professional should be able (1) to examine a patient’s competence of practice on a regular basis, identifying areas of strength and areas where professional development related to genetics and genomics would be beneficial; (2) to understand that health-related genetic information can have important social and psychological implications for individuals and families; and (3) to know how and when to make a referral to a genetics professional. The NCHPEG has also defined knowledge, skills, and attitudes (Table 1) required to achieve these competencies (NCHPEG 2007).
Table 1.
NCHPEG’s core competencies in genetics
| 1. Knowledge |
| 1.1. basic human genetics terminology |
| 1.2. basic patterns of biological inheritance and variation, both within families and within populations |
| 1.3. how identification of disease-associated genetic variations facilitates development of prevention, diagnosis, and treatment options |
| 1.4. the importance of family history (minimum three generations) in assessing predisposition to disease |
| 1.5. the interaction of genetic, environmental, and behavioural factors in predisposition to disease, onset of disease, response to treatment, and maintenance of health |
| 1.6. the difference between clinical diagnosis of disease and identification of genetic predisposition to disease (genetic variation is not strictly correlated with disease manifestation) |
| 1.7. the various factors that influence the client’s ability to use genetic information and services, for example, ethnicity, culture, related health beliefs, ability to pay, and health literacy |
| 1.8. the potential physical and/or psychosocial benefits, limitations, and risks of genetic information for individuals, family members, and communities |
| 1.9. the resources available to assist clients seeking genetic information or services, including the types of genetics professionals available and their diverse responsibilities |
| 1.10. the ethical, legal and social issues related to genetic testing and recording of genetic information (e.g., privacy, the potential for genetic discrimination in health insurance and employment) |
| 1.11. professional role in the referral to or provision of genetics services, and in follow-up for those services |
| 2. Skills |
| 2.1. gather genetic family history information, including at minimum a three-generation history |
| 2.2. identify and refer clients who might benefit from genetic services or from consultation with other professionals for management of issues related to a genetic diagnosis |
| 2.3. explain effectively the reasons for and benefits of genetic services |
| 2.4. use information technology to obtain credible, current information about genetics |
| 2.5. assure that the informed-consent process for genetic testing includes appropriate information about the potential risks, benefits and limitations of the test in question |
| 3. Attitudes |
| 2.6. appreciate the sensitivity of genetic information and the need for privacy and confidentiality |
| 2.7. seek coordination and collaboration with an interdisciplinary team of health professionals |
The aim of this study is to analyze genetic care competencies of primary care health professionals in Brazil. Our initial hypothesis was that these particular professionals have insufficient genetic care competencies in order to support the implementation of the National Policy on Comprehensive Care for People with Rare Diseases in the SUS.
Materials and methods
Setting
The study was conducted in São Carlos, a city located in the São Paulo State’s geographical center, in southeast Brazil. There are approximately 220,000 inhabitants, and the birth rate is approximately 2700 births/year (Brasil IBGE 2010). In 2010, its human development index was 0.805, and therefore, it was considered the 28th most developed city in the country (PNUD 2013). Its gross domestic product per capita is R$ 20,519.065 (Brasil IBGE 2010). São Carlos is an important regional center; the economy of which is based both on industrial and agricultural activities. There are also many shops and services (including health services), which are largely used by the small neighboring towns. There are two important public universities (the Federal University of São Carlos, UFSCar, and the University of São Paulo, USP) and a Brazilian Corporation of Agricultural Research (Empresa Brasileira de Pesquisa Agropecuária, EMBRAPA), reinforcing the condition of a regional center for scientific and technological development.
Over the last 4 years, São Carlos has had an average of 8.57 deaths per 1000 births, 41 % lower than São Paulo State’s average, the rate of which was 12.15 deaths per 1000 births in the same period (São Paulo 2014).
São Carlos Primary Care is based on Basic Health Centres (BHC) from the clinical-centered Primary Care model and Family Health Centres (FHC), which include the FHS community-oriented primary care model. Nowadays, there are 12 BHCs, its staff generally consisting of medical doctors, pediatricians, gynecologists, and obstetricians, nurses, and dentists; and 15 FHSs, which include family doctors (general practitioners), nurses, dentists, dental technicians, and lay community health workers.
The only public clinical genetics service in the city is an outreach activity at the Federal University, established in 2006. This Medical Genetics Outpatient Care is located in the local Speciality Health Centre and meets the demand of the SUS for this speciality in the city, as well as for other cities in the nearby region.
Characteristics of participants
The study included 45 health practitioners (21 doctors, 16 nurses, and 8 dentists), accounting for approximately 30 % of higher-education professionals working in the city’s primary health care. Most participants (77.8 %) had attended state schools, 60 % were female, and the average time since they had left school was 18.5 years; 31.1 % of the participants worked in the FHCs and thus, with the support of the FHS; the remainder 68.9 % worked in the BHCs. A profile of the sample can be seen in Table 2.
Table 2.
Profile of the study sample (n = 45)
| Characterization | n | % |
|---|---|---|
| Doctors | 21 | 46.7 |
| Nurses | 16 | 35.6 |
| Dentists | 8 | 17.7 |
| Work at basic health center | 31 | 68.9 |
| Work at family health center | 14 | 31.1 |
| Female | 27 | 60.0 |
| Male | 18 | 40.0 |
| Finished federal state school | 18 | 40.0 |
| Finished state school | 14 | 31.1 |
| Finished local state school | 3 | 6.7 |
| Finished private school | 10 | 22.2 |
| Time since having finished (years) | 18.5 (SD ± 8.6) | |
Design of the study
The study is a descriptive survey study in which doctors, nurses, and dentists were invited to answer a questionnaire including demographic information and 11 structured genetics-oriented questions developed by the authors, based on competencies established by the US National Coalition for Health Professional Education in Genetics (NCHPEG 2007). Questionnaires addressing this subject have not been developed and validated previously; the authors (experts on genetics and/or primary care) developed initial evidence on this questionnaire validation using content validation only (expert and semantic analyses). Structural validity was not performed.
The first question consisted of five statements (true or false) regarding basic human genetics terminology.
The second question included a clinical vignette case of Down syndrome, with five different options of how to clinically address this situation. It was a multiple choice question intended to assess knowledge regarding the importance of pedigrees, plus the ability to gather information about family genetic history and refer the patient to specialized evaluation. Two aspects concerning attitudes were included as alternatives, both related to the sensitivity of perceiving the importance and consequences of genetic information: the possibility of seeing that patient without sharing the diagnostic risk with the mother, and the possibility of being directive in genetic counselling, advising mothers older than 40 years old not to become pregnant again.
The third question was also a multiple-choice one and made reference to the same Down syndrome case. It assessed knowledge about professional resources and services available for treatment and attitudes when the information was given, analyzing whether the participants considered integral care, as well as the social and educational context of the patients and their family.
Questions 4 and 5 assessed the ability to give guidance to a woman in order to prevent birth defects. They allowed for knowledge assumptions about the interaction of genetic, environmental, and behavioral factors, since it analyzed the importance of using folic acid in preconception (question 4) and the recognition of major teratogens (question 5). There was also one aspect concerning attitudes in question 4: the possibility of the professional advising, in a reproachable way, about habits and addictions that might influence fetal development.
Question 6 consisted of eight true or false sentences. It assessed the ability to conduct a positive neonatal screening and knowledge about the role of health professionals when managing patients positive for hypothyroidism, sickle cell anemia, and phenylketonuria.
Questions 7 and 11 had photos of patients with Down and Crouzon syndromes, to evaluate their ability to recognize facial dysmorphic features in both cases.
The eighth question included another clinical vignette of a woman who told the doctor she had a family history of breast cancer, during a gynecological examination. It was a multiple-choice question with five options. It aimed to assess knowledge about the importance of pedigrees and the ability to collect information about the family genetic history in that situation, regarding not just breast, but all different kinds of cancer.
Question 9 addressed craniofacial defects and consisted of five true or false statements. The purpose was to assess knowledge regarding the importance of pedigrees and dentists’ roles in similar situations and investigate the knowledge about resources and specialized health services available in the region.
Question 10 was multiple-choice and included a pedigree of a family with an autosomal dominant disease. The objective was to evaluate knowledge about classical inheritance patterns.
The procedure to complete the questionnaire was made clear, and doubts were clarified.
Ethical aspects
The project was approved by the Human Research Ethics Committee at the Federal University of São Carlos (process 162,280). All participants provided a written informed consent at the beginning of the questionnaire and all questionnaires were anonymized.
Data analysis
The answers were analyzed and grouped into three categories: knowledge, skills, and attitudes. Descriptive statistics were made using Microsoft Excel® and results presented as percentages. Differences between three groups (doctors, nurses, and dentists) were assessed by the Fisher exact test, using Graphpad prism 6®. The level of significance was set at p < 0.05.
Results
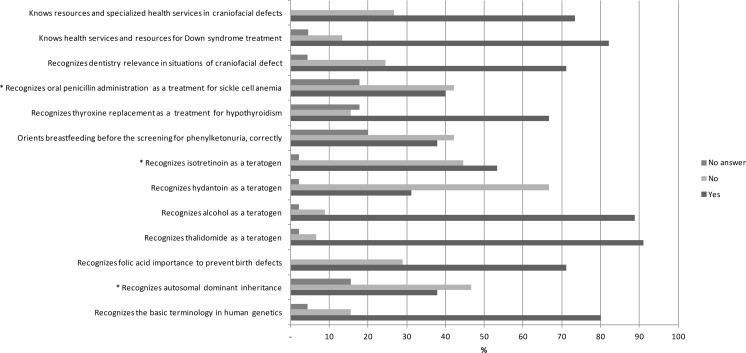
The results (Fig. 1) showed that approximately 80 % of the participants recognized the basic terminology in genetics, but, in general, practitioners found it challenging to identify patterns of inheritance: only 37.8 % of the participants recognized an autosomal dominant pattern of inheritance. On the other hand, approximately 71 % recommended intake of folic acid to prevent birth defects. Thalidomide and alcohol were recognized as a teratogen by 91 and 88.9 % of participants. Significant differences were observed regarding the recognition of the autosomal dominant inheritance between doctors (57.1 %) and dentists (12.5 %) (p = 0.03); recognition of isotretinoin as a teratogen between doctors (76.2 %) and nurses (26.7 %) (p = 0.006); and recognition of oral penicillin as a treatment for sickle cell anemia between doctors (71.4 %) and nurses (18.7 %) (p = 0.003) and between doctors and dentists (0 %) (p = 0.003).
Fig. 1.
Results regarding the knowledge investigated (asterisk indicates knowledge where there was a statistically significant difference between distinct groups of professionals)
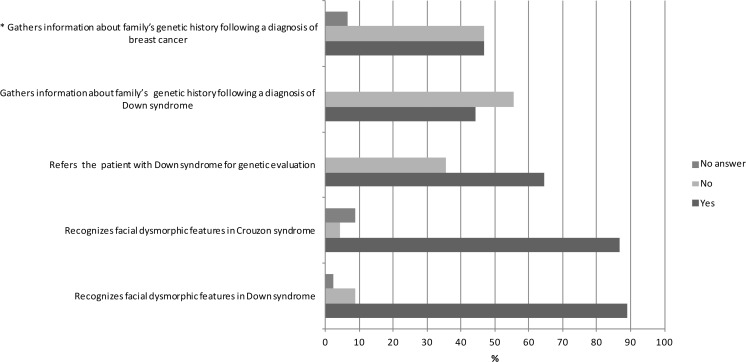
As for clinical skills (Fig. 2), most practitioners were able to recognize facial dysmorphias and the need to refer the patient to specialist evaluation. Nevertheless, there were challenges in the process of valuing and gathering information about family history: 46.7 % neglected asking about other kinds of cancer in a family with breast cancer history. Moreover, concerning care for Down syndrome, 55.5 % would not register any family history and pedigree. A significant difference was observed regarding the skill of collecting family history in the case of breast cancer between dentists (62.5 %) and nurses (31.2 %) (p = 0.012).
Fig. 2.
Results regarding the skills investigated (asterisk indicates the skill in which there was a statistically significant difference between distinct groups of professionals)
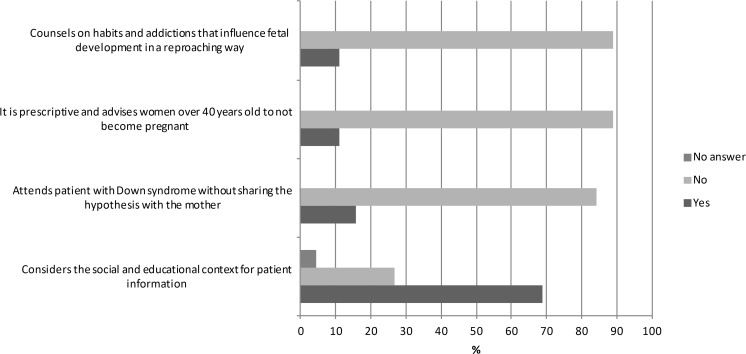
From the point of view of attitudes (Fig. 3), 68.9 % of participants thought about the comprehensiveness of care, considering the social and educational context of the patient and family; however, 15.5 % agreed to attend a child with a clinical suspicion of Down syndrome, without sharing the diagnostic uncertainty with the mother, and 11.1 % were prescriptive, advising women over 40 years not to become pregnant. Significant differences regarding attitudes between the three professional categories were not observed.
Fig. 3.
Results regarding the attitudes investigated
Discussion
We confirmed the hypothesis that primary care professionals still have insufficient genetic care competencies to support the implementation of the National Policy on Comprehensive Care for People with Rare Diseases in the SUS. Insufficiencies included identifying simple patterns of inheritance, valuing and collecting family history, and counselling parents properly. These are all key competencies in providing adequate care for people with rare diseases and must be addressed in future educational actions to mitigate this barrier to the implementation of this policy.
A systematic review examining provision of genetic services by primary care physicians involving 18 studies in the USA (9), UK (6), Scotland (1), Netherlands (1), and Switzerland (1) reported a similar scenario. Major barriers identified were (1) inadequate knowledge of basic genetics; (2) lack of complete or updated family history; (3) lack of physicians’ confidence; and (4) lack of referral guidelines (Suther and Goodson 2003).
Genetics integration in Brazilian primary healthcare (PHC) is a public health Policy implementation requirement, both because the SUS is organized as a network, and as a result of the limited number of specialists. Internationally speaking, changes are already taking place in the provision of genetic services and redefinition of professional roles, with a strong tendency favoring the integration of genetic medicine and other speciality competencies (Korf 2013) into primary care (Emery and Hayflick 2001; Starfield et al. 2002; Robins and Metcalfe 2004; Qureshi et al. 2004; Elwyn et al. 2005; Drury et al. 2007; Cheng et al. 2008; Martin et al. 2009). As a matter of fact, plans for restructuring genetic services have been developed in the UK, some USA states, some Canadian provinces, and a few other countries in Europe (Grosse et al. 2009; Battista et al. 2012).
SUS, as other primary care-centered health care systems, has characteristics that can be explored to maximize recognition of potential genetic problems and to coordinate care services. Primary care settings are the most equitable, as almost everyone will have better access to them compared with access to specialized care. For many conditions, general practitioners may be the main link the population has to health care. Considering this, primary health care professionals must be aware of common clinical presentations of various genetic conditions and recognize when there is a need for referral to a genetic specialist. The long-term person-focused nature of primary care is more conducive to an expanded medical record of patients, in the context of their families and communities. Therefore, primary health care professionals are more likely to ascertain familial diseases than other specialists and health professionals. Coordinating care provided within a primary care setting is also an important aspect of PHC. In rare diseases, ongoing care from a wide range of professionals is required, and effective and efficient mechanisms to transfer information need to be established between primary and specialized care, and vice versa. Other specialists need information not only about diagnosis, but also about the family and cultural context. Primary health care professionals, in turn, require information not only about the problem, but also about possible alternative interventions, in order to help patients choose the best options for themselves and their families. There is a need for continuing communication between primary and specialized health care (Starfield et al. 2002).
In addition to NCHPEG (2007), many groups have worked on creating core educational guidelines and competencies. These included the American Society of Human Genetics (ASHG 1995), the Association of Professors of Human and Medical Genetics (Friedman et al. 1998), the American Association of Family Practitioners (AAFP 1999), the American Academy of Nursing (Lea 2002), the Internal Medicine Residency Training Program Genetics Curriculum Committee (Riegert-Johnson et al. 2004), and the International Society of Nurses in Genetics (ISNG 2007); in 2008, the European Society of Human Genetics (ESHG) adopted the Core Competences in Genetics for Health Professionals developed by EuroGentest and has recommended that national societies use them as a basis for curricula and initiatives in professional education.
Core Competences in Genetics for Health Professionals in Europe are specific for physicians and nurses, and also for medical generalists and nongenetic specialists.6 The theoretical NCHPEG framework, adopted in this work, points to a minimum set of competences common to all health professionals, aiming to converge their performances regarding medical genetics, although professionals specificities have been dealt with in this study. Our results showed that physicians, more used to dealing with drug prescriptions, recognized better the importance of penicillin in the management of sickle cell anemia and isotretinoin as a teratogen.
It is of concern that almost 50 % of the professionals in this study did not recognize the autosomal dominant inheritance and have difficulty in collecting family history. This is a risk factor for many chronic diseases, including cancer, cardiovascular disease, and diabetes. The advantages of family history include lower costs and greater acceptability than other genetic tools and reflect the interaction between genetic and environmental factors (Valdez et al. 2010); however, the usefulness of family history in public health has been poorly investigated. There is a statement from the NIH State-of-the-Science Conference that current evidence on the effectiveness of family history to determine and manage risks for common chronic diseases is weak (Berg et al. 2009), which has encouraged efforts to rigorously assess the validity and usefulness of family history in public health settings (Orlando et al. 2011, 2013).
Undoubtedly, one of the main competences in genetics required in PHC is related to taking, recording, and interpreting family history. Considering this, as well as the recognition of common patterns of inheritance, skills in genetic risk assessment and communication are required for nondirective counselling (Emery and Hayflick 2001).
The integration of genetic medicine into primary care requires basic knowledge about common genetic disorders and patterns of inheritance, genetic testing, and foreseeable therapeutic innovations should be incorporated into both undergraduate and postgraduate training and in continuous education.
In Brazil, a training experience reported by a resident in Family and Community Medicine suggests that graduates could qualify for family history collection, identification, and monitoring of at risk situations, patient care coordination with genetic disease, and information about available resources (Melo and Gomes 2009).
Another study, in which 43 PHC professionals took part (doctors, nurses, and dentists) of a medium-sized municipality of Rio de Janeiro State, showed that, although the collection of family data is used in clinical practice, about a quarter of the professionals do not consider it relevant to identify and monitor families at risk for genetic diseases. These results point to the need to extend continuing education in genetics for primary care professionals (Vieira et al. 2013a).
An experiment was carried out in 2009 and 2012, an educational program in medical genetics aimed at PHC, developed by the Medical Genetics Service of Hospital de Clínicas de Porto Alegre (SGM/HCPA). This pilot project, involving 43 professionals from three Basic Health Units, was helpful for approaching medical genetics and PHC and showed the need for continuing education strategies and ongoing support to PHC (Vieira et al. 2013b).
Genetic specialists should be responsible for developing mechanisms for continuing education of family physicians and other health care professionals. Clinical practice can be improved by involving practitioners in planning and carrying out clinical research, in reviewing and developing guidelines. Computerized protocols developed jointly by genetic specialists and primary care practitioners could potentially provide a method not only to advise on indications for referral, but also on which tests should be done prior to referral and which are not indicated.
In October 2013, Brazil set up the program “More Doctors” (Programa Mais Médicos), with the aim of developing medical resources for the SUS and the following objectives: to reduce the shortage of doctors in priority regions to reduce regional inequalities; to strengthen provision of primary health care services; to improve medical education and provide more medical practice during training; to expand the inclusion of trainees in the SUS, as a way to develop their knowledge about the Brazilian health situation; to strengthen continuing education with integration of higher education institutions in the academic supervision of clinical activities; to promote exchange of knowledge and experiences between Brazilian and foreign health professionals; to improve doctors’ work in public health policy and the SUS organization and functioning, and to stimulate the research applied to SUS. According to the “More Doctors Programme,” the first year of a Residency Program in General Family Medicine and Community will be required, by the end of 2018, for admission in Medical Residency Programs for Internal Medicine, Paediatrics, Obstetrics and Gynaecology, General Surgery, Psychiatry, and Social and Preventive Medicine (Brasil 2013). This might be a key opportunity for competency-based education and skills training in genetics.
In addition, we believe that the National Policy of Permanent Education in Health (Brasil 2009) could support national genetics education for professionals of the SUS, qualifying those already working in health care. This policy was established by the Ministry of Health in 2009 with the aim of transforming health practices and strengthening the SUS through education strategies focused on the work process. In other words, this policy foresees that practical situations, experienced by PHC professionals, can provide a path to learning, by reflexive analysis of practical problems and appreciation of the work process in its intrinsic context. From this perspective, it is important that Community Family Health Teams identify the genetic problems in their community-based health care, as a starting point for education programs.
Moreover, organizing genetics services in the SUS, such as those provided by the National Policy on Comprehensive Care for People with Rare Diseases, may be an incentive for new physicians to become experts in this area. It can also contribute to setting up more Medical Genetics residency programs and accrediting nurse specialists in genetics, as well as recognizing genetic counsellors.
Genetic counsellors are health professionals with specialized training, typically covering medical/scientific and counselling areas, including clinical genetics, population genetics, cyto and molecular genetics, as well as psychosocial principles, ethics and counselling techniques. Counselling techniques are part of the training program for physicians specializing in genetics, but the Brazilian Society of Medical Genetics did not yet recognize genetic counsellor professionals. The National Policy on Comprehensive Care for People with Rare Diseases recognizes genetic counselling as a specific health procedure to be performed in Reference Centres for Rare Disease (Brasil 2014), but it is not clear what professionals should deliver it. Regulating the profession of genetic counselling in Brazil is urgent and will enable the definition of specific professional attributes and the establishment of minimum qualifications for their specific training.
Limitations
This is a preliminary study, and the results reflect the effect of a nonstatistical sample in a restricted context. The participants compose a heterogeneous sample and probably gained different knowledge about genetics in their BSc studies, as this is not defined in the curriculum guidelines of the Ministry of Education. Research conducted in 2003 with 57 Brazilian medical schools showed that genetics in curricula varied in the topics presented and the depth of study (Porciúncula 2004). Furthermore, data were collected using a novel questionnaire, which has not yet fully been validated. Further studies should address this issue. On the other hand, this is the first Brazilian study using a questionnaire based on competency-based international guidelines and may warrant further studies and public policies.
Final considerations
Universal genetic care access has the potential of reducing disparity and inequity in populations’ health needs, mainly in developing countries. As new genetic knowledge may lead to improved health outcomes, technology must be accessible to everyone, provided by well-trained professionals prepared to deal with it on different health care levels, especially in primary care, as this is an ideal scenario for long-term patient-centered care in the context of the family and community.
It will be a challenge to implement the National Policy on Comprehensive Care for People with Rare Diseases in Brazil, and one of the greatest difficulties will be to design a feasible and affordable training program for health professionals already working in primary health care.
The results of this study may contribute to the development of an effective educational program in genetics based on primary health care, as a key strategy to overcome the challenges of including genetics in the SUS policies.
Acknowledgments
We would like to thank the research participants who willingly provided data for this investigation.
Conflict of interest
The authors have no conflicts of interest to declare.
Compliance with ethical standards
This survey was supported by CAPES (Coordination for the Improvement of Higher Education Personnel) through the Young Talents for Science Project. The research was approved by the Human Research Ethics Committee at the Federal University of São Carlos (process 162,280). All participants provided a written informed consent.
Footnotes
Trends in Family Health Strategy national coverage—Department of Primary Care of the Ministry of Health—available at http://dab.saude.gov.br/portaldab/historico_cobertura_sf.php (accessed on October 16th, 2014).
Brazilian Society of Medical Genetics (SBGM)—available at http://www.sbgm.org.br/ (accessed on 18 October 2014).
Coordination for the Improvement of Higher Education Personnel (CAPES)—available at http://www.capes.gov.br/ (accessed on 19 October 2014).
These data were obtained through personal communications
Equivalent to US$ 6,333.04 on 16 March 2015
European Society of Human Genetics (ESHG)—available at https://www.eshg.org/139.0.html (accessed on 18 October 2014).
This article is part of the special issue on “Genetics and Ethics in Latin America”
Pamela Karen de Paula and Stephania de Araujo Rodrigues contributed equally to this work.
References
- AAFP, American Academy of Family Physicians Core Educational Guidelines - Medical genetics: Recommended core educational guidelines for family practice residents. Am Fam Physician. 1999;60:305–307. [Google Scholar]
- ASHG, American Society of Human Genetics Report from the ASHG Information and Education Committee: medical school core curriculum in genetics. Am J Hum Genet. 1995;56(2):535–537. [PMC free article] [PubMed] [Google Scholar]
- Battista RN, Blancquaert I, Laberge AM, van Schendel N, Leduc N. Genetics in health care: an overview of current and emerging models. Public Health Genom. 2012;15:34–45. doi: 10.1159/000328846. [DOI] [PubMed] [Google Scholar]
- Berg AO, Baird MA, Botkin JR, Driscoll DA, Fishman PA, Guarino PD, Hiatt RA, Jarvik GP, Millon-Underwood S, Morgan TM, Mulvihill JJ, Pollin TI, Schimmel SR, Stefanek ME, Vollmer WM, Williams JK. National Institutes of Health State-of-the-Science Conference Statement: Family History and Improving Health: August 24-26, 2009. NIH Consens State Sci Statements. 2009;26:1–19. [PubMed] [Google Scholar]
- Brasil (2009) Ministério da Saúde, Secretaria de Gestão do Trabalho e da Educação na Saúde, Departamento de Gestão da Educação em Saúde (2009) Política Nacional de Educação Permanente em Saúde. Ministério da Saúde, Brasília. Available at: http://bvsms.saude.gov.br/bvs/publicacoes/politica_nacional_educacao_permanente_saude.pdf accessed 1 Feb 2015
- Brasil (2013) Presidência da República, Casa Civil. Lei n° 12.871, de 22 outubro 2013. Institui o Programa Mais Médicos, altera as Leis no 8.745, de 9 dezembro 1993, e no 6.932, de 7 julho 1981, e dá outras providências
- Brasil (2014) Ministério da Saúde, Gabinete do Ministro. Portaria no 199, de 30 janeiro 2014. Institui a Política Nacional de Atenção Integral às Pessoas com Doenças Raras, aprova as Diretrizes para Atenção Integral às Pessoas com Doenças Raras no âmbito do Sistema Único de Saúde (SUS) e institui incentivos financeiros de custeio. Available at: http://bvsms.saude.gov.br/bvs/saudelegis/gm/2014/prt0199_30_01_2014.html accessed 18 Oct 2014
- Brasil IBGE, Instituto Brasileiro de Geografia e Estatística (2010) Censo Demográfico 2010. Available at http://www.cidades.ibge.gov.br/; accessed on 18 Oct 2014
- Cheng TL, Cohn RD, Dover GJ. The genetics revolution and primary care pediatrics. JAMA. 2008;299:451–453. doi: 10.1001/jama.299.4.451. [DOI] [PubMed] [Google Scholar]
- Drury N, Bethea J, Guilbert P, Qureshi N. Genetics support to primary care practitioners - a demonstration project. J Genet Couns. 2007;16:583–591. doi: 10.1007/s10897-007-9096-1. [DOI] [PubMed] [Google Scholar]
- Elwyn G, Edwards A, Iredale R, Davies P, Gray J. Identifying future models for delivering genetic services: a nominal group study in primary care. BMC Fam Pract. 2005;6:1–6. doi: 10.1186/1471-2296-6-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emery J, Hayflick S. The challenge of integrating genetic medicine into primary care. BMJ. 2001;322:1027–1030. doi: 10.1136/bmj.322.7293.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman JM, Blitzer M, Elsas LJ, 2nd, Francke U, Willard HF. Clinical objectives in medical genetics for undergraduate medical students. Association of Professors of Human Genetics, Clinical Objectives Task Force. Genet Med. 1998;1:54–55. doi: 10.1097/00125817-199811000-00011. [DOI] [PubMed] [Google Scholar]
- Grosse SD, Schechter MS, Kulkarni R, Lloyd-Puryear MA, Strickland B, Trevathan E. Models of comprehensive multidisciplinary care for individuals in the United States with genetic disorders. Pediatrics. 2009;123:407–412. doi: 10.1542/peds.2007-2875. [DOI] [PubMed] [Google Scholar]
- Horovitz DD, de Faria Ferraz VE, Dain S, Marques-de-Faria AP. Genetic services and testing in Brazil. J Community Genet. 2013;4:355–375. doi: 10.1007/s12687-012-0096-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ISNG, International Society of Nurses in Genetics (2007) Genetics and Genomics Nursing: Scope and Standards of Practice. American Nursing Association, Washington, D.C. Available at: http://www.nursingworld.org/MainMenuCategories/EthicsStandards/Genetics-1/Genetics-and-Genomics-Nursing-Scope-and-Standards.pdf accessed 18 Oct 2014
- Korf BR. Integration of genomics into medical practice. Discov Med. 2013;16:241–248. [PubMed] [Google Scholar]
- Lea DH (2002) Position statement: integrating genetics competencies into baccalaureate and advanced nursing education. Nurs Outlook 50(4):167–168 [DOI] [PubMed]
- Martin G, Currie G, Finn R. Bringing genetics into primary care: findings from a national evaluation of pilots in England. J Health Serv Res Policy. 2009;14:204–211. doi: 10.1258/jhsrp.2009.008158. [DOI] [PubMed] [Google Scholar]
- Melo DG, Gomes TLCS (2009) Capacitação em Genética Médica para residentes em Medicina de Família e Comunidade: relato de experiência. Revista de APS 12:83–87
- Melo DG, Sequeiros J. The challenges of incorporating genetic testing in the unified national health system in Brazil. Genet Test Mol Biomark. 2012;16:651–655. doi: 10.1089/gtmb.2011.0286. [DOI] [PubMed] [Google Scholar]
- NCHPEG, National Coalition for Health Professional Education in Genetics (2007) Core Competencies in Genetics for Health Professionals. Available at: www.nchpeg.org/index.php?option=com_content&view=article&id=237&Itemid=84 accessed 18 Oct 2014
- Novoa MC, Burnham TF. Challenges for the universalization of clinical genetics: the Brazilian case. Rev Panama Salud Publ. 2011;29:61–68. doi: 10.1590/S1020-49892011000100010. [DOI] [PubMed] [Google Scholar]
- Orlando LA, Hauser ER, Christianson C, Powell KP, Buchanan AH, Chesnut B, Agbaje AB, Henrich VC, Ginsburg G. Protocol for implementation of family health history collection and decision support into primary care using a computerized family health history system. BMC Health Serv Res. 2011;11:1–7. doi: 10.1186/1472-6963-11-264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orlando LA, Buchanan AH, Hahn SE, Christianson CA, Powell KP, Skinner CS, Chesnut B, Blach C, Due B, Ginsburg GS, Henrich VC. Development and validation of a primary care-based family health history and decision support program (MeTree) N C Med J. 2013;74:287–296. [PMC free article] [PubMed] [Google Scholar]
- Paim J, Travassos C, Almeida C, Bahia L, Macinko J. The Brazilian health system: history, advances, and challenges. Lancet. 2011;377:1778–1797. doi: 10.1016/S0140-6736(11)60054-8. [DOI] [PubMed] [Google Scholar]
- Pinto RM, Wall M, Yu G, Penido C, Schmidt C. Primary care and public health services integration in Brazil's unified health system. Am J Public Health. 2012;102:e69–e76. doi: 10.2105/AJPH.2012.300972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PNUD, Programa das Nações Unidas para o Desenvolvimento do Brasil (2013). Atlas do Desenvolvimento Humano no Brasil 2013. Available at: www.pnud.org.br accessed 18 Oct 2014
- Porciúncula CGG (2004) Avaliação do ensino de genética médica nos cursos de medicina do Brasil. Dissertation, University of Campinas, Brazil
- Qureshi N, Modell B, Modell M. Timeline: raising the profile of genetics in primary care. Nat Rev Genet. 2004;5:783–790. doi: 10.1038/nrg1453. [DOI] [PubMed] [Google Scholar]
- Riegert-Johnson DL, Korf BR, Alford RL, Broder MI, Keats BJ, Ormond KE, Pyeritz RE, Watson MS. Outline of a medical genetics curriculum for internal medicine residency training programs. Genet Med. 2004;6:543–547. doi: 10.1097/01.GIM.0000144561.77590.85. [DOI] [PubMed] [Google Scholar]
- Robins R, Metcalfe S. Integrating genetics as practices of primary care. Soc Sci Med. 2004;59:223–233. doi: 10.1016/j.socscimed.2003.10.025. [DOI] [PubMed] [Google Scholar]
- São Paulo. SEADE, Sistema Estadual de Análise de Dados (2014) População e Estatíticas Vitais. Available at http://www.seade.gov.br/ accessed 18 Oct 2014
- Starfield B, Holtzman NA, Roland MO, Sibbald B, Harris R, Harris H. Primary care and genetic services. Health care in evolution. Eur J Public Health. 2002;12:51–56. doi: 10.1093/eurpub/12.1.51. [DOI] [PubMed] [Google Scholar]
- Suther S, Goodson P. Barriers to the provision of genetic services by primary care physicians: a systematic review of the literature. Genet Med. 2003;5:70–76. doi: 10.1097/01.GIM.0000055201.16487.61. [DOI] [PubMed] [Google Scholar]
- Valdez R, Yoon PW, Qureshi N, Green RF, Khoury MJ. Family history in public health practice: a genomic tool for disease prevention and health promotion. Annu Rev Public Health. 2010;31:69–87. doi: 10.1146/annurev.publhealth.012809.103621. [DOI] [PubMed] [Google Scholar]
- Vieira DKR, Attianezi M, Horovitz DD, Llerena JC., Jr Atenção em genética médica no SUS: a experiência de um município de médio porte. Physis. 2013;23:243–261. doi: 10.1590/S0103-73312013000100014. [DOI] [Google Scholar]
- Vieira TA, Giugliani C, da Silva LP, Faccini LS, Loguercio Leite JC, Artigalás OA, Medeiros Lenz ML, Muñoz-Rojas MV, Giugliani R. Inclusion of medical genetics in primary health care: report of a pilot project in Brazil. J Community Genet. 2013;4:137–145. doi: 10.1007/s12687-012-0110-4. [DOI] [PMC free article] [PubMed] [Google Scholar]