Abstract
Drug overdose is now the leading cause of unintentional death nationwide, driven by increased prescription opioid overdoses. To better understand urban opioid overdose deaths, this paper examines geographic, demographic, and clinical differences between heroin-related decedents and prescription opioid decedents in San Francisco from 2010 to 2012. During this time period, 331 individuals died from accidental overdose caused by opioids (310 involving prescription opioids and 31 involving heroin). Deaths most commonly involved methadone (45.9 %), morphine (26.9 %), and oxycodone (21.8 %). Most deaths also involved other substances (74.9 %), most commonly cocaine (35.3 %), benzodiazepines (27.5 %), antidepressants (22.7 %), and alcohol (19.6 %). Deaths were concentrated in a small, high-poverty, central area of San Francisco and disproportionately affected African-American individuals. Decedents in high-poverty areas were significantly more likely to die from methadone and cocaine, whereas individuals from more affluent areas were more likely die from oxycodone and benzodiazepines. Heroin decedents were more likely to be within a younger age demographic, die in public spaces, and have illicit substances rather than other prescription opioids. Overall, heroin overdose death, previously common in San Francisco, is now rare. Prescription opioid overdose has emerged as a significant concern, particularly among individuals in high-poverty areas. Deaths in poor and affluent regions involve different causative opioids and co-occurring substances.
Electronic supplementary material
The online version of this article (doi:10.1007/s11524-015-9967-y) contains supplementary material, which is available to authorized users.
Keywords: Opiate overdose, Overdose, Prescription opiate, Opioid analgesic, Opioid, San Francisco, Naloxone, Opioid safety
Introduction
Drug poisoning is now the leading cause of unintentional death among American adults, surpassing motor vehicle accidents. In 2010, 38,000 people died from drug overdoses in the USA.1 Nationally, prescription opioid deaths increased nearly 400 % from 1999 to 20092,3 and now account for nearly half of all drug overdose deaths.4 Prescription opioid use leads to over three hundred thousand annual emergency department visits and billions in other associated health systems costs.5,6
Although there is a rich historical literature on the demographics and event-level characteristics of heroin overdose,7,8 our understanding of recent trends of opioid overdose is limited and largely based on health system and non-urban regional analyses.9–14 Prescription opioid overdose has been documented among rural and suburban non-Hispanic white men,9–15 middle-aged females,16,17 and those using psychotherapeutic drugs.2,18 Patients in safety net healthcare systems, including the Veterans Administration19 and Medicaid,20 are more likely to die of prescription opioid overdose compared to the general population. Case-level and broader health system studies suggest connections between prescription opioid use and subsequent heroin use.21,22 Investigators in New York City saw a distinct rise of prescription opioid overdose deaths in affluent, geographically distinct areas in the early 2000s and a subsequent transition to heroin overdose death in those same areas.23,24 The current characteristics of opioid overdose death in other urban regions in the USA are underexplored.
Studies of opioid overdose mortality in the 1990s in San Francisco documented almost exclusively heroin as the causative opioid, frequent co-occurrence of both other illicit and prescription substances, and a geographic concentration of deaths in and around single room occupancy (SRO) hotel units in high-poverty areas heavily affected by heroin use.25,27 Since 2000, the Office of the Chief Medical Examiner (OCME) of the City and County of San Francisco annual reports document an increase in prescription opioid overdose deaths alongside a substantial decline in heroin overdose deaths from a high of 183 in 1999.26, 27,28 In this study, we sought to characterize recent shifts in opioids causing death from 2010 to 2012 in San Francisco by comparing heroin and prescription opioid overdose deaths and by examining the differences between deaths observed in geographic areas above and below the poverty line.
Methods
Study Population
We analyzed an anonymous database of all opioid overdose decedents from 2010 to 2012 in the City and County of San Francisco. The University of California San Francisco Committee on Human Research determined that this study met the criteria for Human Subjects research exemption.
The database was developed by abstracting demographics, cause of death, death location, residence, and postmortem toxicology data for all opioid overdose deaths from the California Electronic Death Reporting System (CA-ERDS). CA-ERDS is a statewide electronic repository of all county-level death certificates with information on demographics, cause of death, and postmortem toxicology data as reported by county medical examiners and/or coroners. Cases were included if (a) death location was within the City and County of San Francisco; (b) cause of death included any illicit opiate (i.e., morphine-type alkaloid) or synthetic or semi-synthetic prescription opioid (e.g., methadone, oxycodone, fentanyl, hydrocodone, morphine, and others [specified in Supplemental Appendix 1]); and (c) death occurred between January 1, 2010 and December 31, 2012. In this paper, the term “opioids” refers to both morphine-type alkaloids and synthetic opioids. Cases were excluded if (a) the decedent was less than 18 years of age and (b) the primary cause of death did not include “acute intoxication” or was determined to be non-accidental (suicide or homicide with a medically appropriate cause of death listed). International Classification of Disease (ICD) codes were not used to select cases because they lacked appropriate sensitivity. Data were included only since 2010 because the cause of death in the CA-EDRS did not specify which drugs were involved prior to 2010. Data evaluation and coding were performed by AV and CB, and reviewed by NL and PC.
Opioid Overdose Classification
The San Francisco Office of the Chief Medical Examiner (OCME) takes jurisdiction and investigates via autopsy all suspected deaths involving sudden, unexpected, or violent circumstances. Specimens analyzed during autopsy include, but are not limited to, central/cardiac blood, peripheral blood, urine, vitreous humor, bile, and liver. The OCME’s Forensic Laboratory Division conducts several toxicologic evaluations including (a) duplicate screening and confirmation/quantitation of ethanol, methanol, acetone, isopropanol, and other related volatile compounds in peripheral blood by headspace gas chromatography with flame ionization detection, (b) screening in central blood and urine for amphetamines, barbiturates, benzodiazepines, cannabinoids, cocaine, fentanyl, methadone, phencyclidine, opioids, and tricyclic antidepressants by enzyme-linked immunosorbent assay, (c) screening in central blood and urine for over 100 drugs and metabolites by full-scan gas chromatography–mass spectrometry, and (d) confirmations and quantitations in peripheral blood and confirmations in urine by gas or liquid chromatography–tandem mass spectrometry as required. During our study time frame, not all known analytes for each drug class were included in every drug screen (e.g., buprenorphine and naloxone were screened for only if indicated in the decedent’s medical history, pharmacy records, or death investigation history). Drug screens were typically performed with the preferred central blood and urine, but also quantitations took place in peripheral blood. Supplemental Appendix Tables 1 and 2 note the ELISA blood and urine cut-off concentrations and the mass spectrometry blood limits of quantitation for opioid drugs at the OCME, respectively. Based on the drug screens and confirmations/quantitations performed, specific drugs were listed on the case postmortem toxicology report and included on the death certificate if they were considered as having caused the death or contributed to the death in the opinions of the board-certified forensic pathologist and forensic toxicologist in charge of each case. Heroin-related overdose was indicated in the postmortem toxicology for cases with the confirmed presence of the heroin metabolite 6-Monoacetylmorphine (6-MAM). Ten additional cases in which morphine and codeine were concurrently present were coded as prescription opioid cases given the absence of 6-MAM verification by gas or liquid chromatography–tandem mass spectrometry and then coded as heroin in a sensitivity analysis.
Statistical and Geospatial Analyses
We conducted descriptive analyses of all deaths, including mean, median, and 95 % confidence interval for continuous variables and number and percentage for categorical variables. We calculated the overdose death rate per 100,000 person years using the total and sex-specific population counts from the relevant year of the American Community Survey (ACS)29 and the National HIV Behavior Surveillance Survey for Injection Drug Users30 (see Supplemental Appendix 3 for methodology).
To examine the spatial variation and geographic disparities of opioid overdose deaths, we abstracted and geocoded CA-ERDS location of death data to overlying neighborhoods as described by the San Francisco Department of City Planning31 and census tracts as described by the 2010 ACS. Deaths were mapped according to the location of death, unless death occurred in hospital in which the case of death was mapped by residence if located within San Francisco. We used ArcGIS32 to geocode CA-ERDS death locations with a match criterion greater than 90 %. Unmatched addresses were reviewed and re-coded using GPS Visualizer.33 We derived economic and demographic characteristics of each census tract from the 2010 ACS. We visualized opioid decedent locations by creating a point vector map of each incident and through neighborhood-specific prescription opioid death counts. Visualizations were created using main thoroughfares and abstracted census tract lines to protect decedent anonymity.
We evaluated demographic and clinical differences between decedents who died within census tracts above and below the mean San Francisco 2010 ACS percentage of individuals in poverty. For this analysis, we excluded individuals who died in hospitals without prior residence in San Francisco (n = 10), since decedent location was not reflective of underlying local census tract demographic information. Additionally, we evaluated geographic, demographic, and clinical differences between decedents with heroin-related overdoses and those with only prescription opioids on postmortem toxicology. Between-group comparisons (above poverty line vs. below poverty line, prescription opioid vs. heroin-related) were evaluated using χ2 and Fischer’s exact test for categorical variables, if greater or less than five occurrences respectively, and Student’s t test and Wilcoxon rank sum for continuous variables.
We fitted a multivariable logistic regression model to evaluate the differences between heroin decedents and those without heroin on postmortem toxicology. For model building, predictors in the bivariate logistic regression analysis with a p value of 0.15 or lower were considered for inclusion in a larger, multivariable model. Starting with hypothesized confounders (age, gender, and race/ethnicity), we used a step-wise forward procedure using the most significant bivariate predictors. Likelihood ratio tests were used to verify that variables included made a statistically significant independent contribution to the larger model. A correction factor was incorporated into variables with no observations to prevent separation from occurring.34
Results
From January 1, 2010 to December 31, 2012, we identified 331 accidental opioid overdose deaths in the City and County of San Francisco, 310 (93.7 %) of which involved prescription opioids and 31 (9.4 %) of which involved heroin. Ten cases (3.0 %) involved both heroin and prescription opioids.
Sample Characteristics
Among all 331 opioid overdose decedents, median age at death was 50 years and 68.3 % were men; 71.0 % were non-Hispanic whites, and 19.9 % were African-American, compared to 54.3 and 6.1 % of San Francisco residents, respectively (Table 1).
TABLE 1.
All opioid overdoses in San Francisco from 2010 to 2012
| All observations | ||
|---|---|---|
| Count | ||
| n = 331 | % | |
| Age (years) | ||
| 18–24 | 20 | 6.0 % |
| 25–34 | 35 | 10.6 % |
| 35–44 | 65 | 19.6 % |
| 45–54 | 91 | 27.5 % |
| 55–64 | 102 | 30.8 % |
| >65 | 18 | 5.4 % |
| Mean (SD) | 48.2 | (12.5) |
| Median (IQR) | 50.0 | (40–58) |
| Sex | ||
| Female | 105 | 31.7 % |
| Male | 226 | 68.3 % |
| Race | ||
| Non-Hispanic White | 235 | 71.0 % |
| African-American | 66 | 19.9 % |
| Hispanic | 14 | 4.2 % |
| Asian | 7 | 2.1 % |
| Other | 9 | 2.7 % |
| San Francisco Residence | ||
| % of total | 285 | 86.1 % |
| Opioids present and considered causative of death | ||
| Methadone | 152 | 45.9 % |
| Morphine | 89 | 26.9 % |
| Oxycodone | 72 | 21.8 % |
| Hydrocodone | 54 | 16.3 % |
| Fentanyl | 18 | 5.4 % |
| Codeine | 18 | 5.4 % |
| Heroin (as 6-MAM) | 31 | 9.4 % |
| Other | 9 | 2.7 % |
| More than one opioid | 96 | 29.0 % |
| Morphine and codeine only opioids present | 4 | 1.2 % |
| Other substances present at death | ||
| No cocaine, amphetamines, alcohol, or benzodiazepines | 83 | 25.1 % |
| Alcohol | 65 | 19.6 % |
| Benzodiazepines | 91 | 27.5 % |
| Cocaine | 117 | 35.3 % |
| Amphetamines | 46 | 13.9 % |
| Antidepressant | 75 | 22.7 % |
| Antihistamine | 37 | 11.2 % |
| Antipsychotic | 11 | 3.3 % |
| Location of death | ||
| Hospital | 28 | 8.5 % |
| Public space | 23 | 6.9 % |
| Shelter/transitional housing | 5 | 1.5 % |
| Hotel, not SRO | 12 | 3.6 % |
| Private residence (All) | 263 | 79.5 % |
| Own SRO | 79 | 23.9 % |
| Own non-SRO residence | 138 | 41.7 % |
| Friend/other residence | 46 | 13.9 % |
| All SRO | 103 | 31.1 % |
Overdose Incidence Rate
The age-adjusted incidence rate per 100,000 person years for all-cause opioid overdose death in San Francisco was 15.6 overall,35 21.1 among males, 10.1 among females, 26.5 among non-Hispanic whites, 51.1 among African-Americans/Blacks, 1.0 among Asians, and 4.4 among Latinos.
Cause of Death
Among all deaths, the most common opioids present on postmortem toxicology and considered contributory to death were methadone (45.9 %), morphine (26.9 %), oxycodone (21.8 %), and hydrocodone (16.3 %). Heroin was present in 9.4 % of deaths. Twenty-nine percent had more than one opioid considered causative and 74.9 % had other substances believed to contribute to opioid overdose death, most frequently cocaine (35.3 %), benzodiazepines (27.5 %), or alcohol (19.6 %). Antidepressants were present in 22.7 % of all decedents. Excluding 43 decedents actively receiving methadone maintenance treatment at the time of death, methadone was present in 32.8 % of all decedents.
Location and Geographic Distribution
Most decedents (86.1 %) were San Francisco residents. Of the 263 deaths occurring in a private residence, 82.5 % were in the decedent’s own residence (30 % single room occupancy (SRO) hotel; 52.5 % other private residence) and 17.4 % occurred in a friend or acquaintance’s residence. Of the 69 deaths occurring in other spaces, 40.5 % were in a hospital and 34.7 % in a public location such as a street, car, or park.
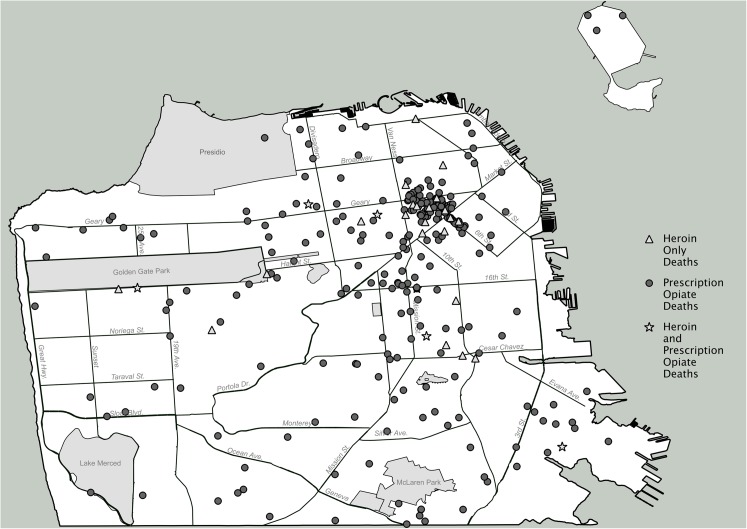
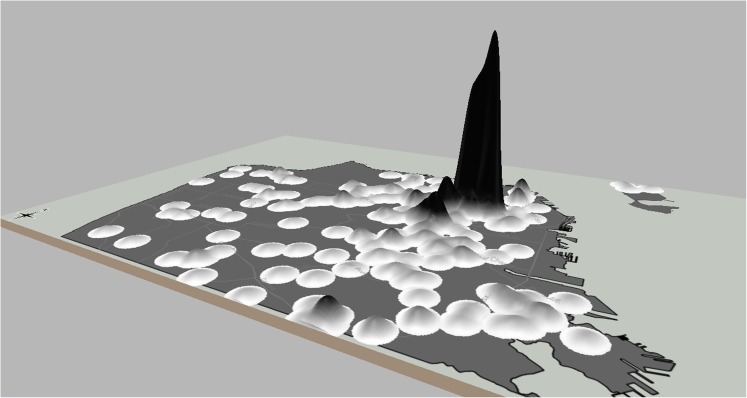
Deaths were clustered largely within the Tenderloin/Civic Center (32.5 %) and South of Market (12.4 %) neighborhoods, both of which have a high proportion of residents living in poverty, single room occupancy hotels, and opioid-related drug arrests.36–38 While 44.9 % of opioid-related deaths occurred in these two neighborhoods, remaining deaths were diffused throughout the city, with 35 of 37 neighborhoods recording at least one opioid overdose death (Appendix Table 1). The visualizations of opioid overdoses as points and elevation maps can be seen in Figs. 1 and 2.
FIG. 1.
Point visualization of prescription opioid deaths in San Francisco from 2010 to 2012.
FIG. 2.
Elevation visualization of opioid overdose deaths in San Francisco from 2010 to 2012.
Between-group differences for decedents with death locations in census tracts above and below the San Francisco poverty line are summarized in Table 2. While decedent age distribution was similar across areas, decedents within areas below the poverty line were more likely to be African-American (23.2 % compared to 11.9 %, p = 0.03). Deaths within areas below the poverty line were significantly more likely to involve methadone (53.2 vs. 25.0 %, p < 0.01) and cocaine (40.5 % compared to 20.2 % p < 0.01); in contrast, deaths within areas above the poverty line were more likely to involve oxycodone (31.0 % compared to 19.0 %, p = 0.02) and benzodiazepines (41.7 vs. 22.7 %, p < 0.01). Decedents in areas below the poverty line were more likely to have died in SRO rooms rather than private residences.
TABLE 2.
Comparison between Decedent Locations in Areas Above Versus Below Poverty line
| Decedents in areas above poverty line | Decedents in areas below poverty line | p value | |||
|---|---|---|---|---|---|
| Count | Count | ||||
| n = 84 | % | n = 237 | % | ||
| Age (years) | |||||
| 18–24 | 7 | 8.3 % | 11 | 4.6 % | 0.026 |
| 25–34 | 9 | 10.7 % | 25 | 10.5 % | 0.966 |
| 35–44 | 17 | 20.2 % | 45 | 19.0 % | 0.803 |
| 44–54 | 18 | 21.4 % | 69 | 29.1 % | 0.173 |
| 55–64 | 28 | 33.3 % | 74 | 31.2 % | 0.721 |
| >65 | 5 | 6.0 % | 13 | 5.5 % | 0.873 |
| Mean | 47.7 | (44.86–50.50) | 47.3 | (47.28–50.49) | 0.460 |
| Sex | |||||
| Male | 53 | 63.1 % | 167 | 70.5 % | 0.211 |
| Race | |||||
| Non-Hispanic White | 63 | 75.0 % | 164 | 69.2 % | 0.315 |
| African-American | 10 | 11.9 % | 55 | 23.2 % | 0.027 |
| Hispanic | 4 | 4.8 % | 9 | 3.8 % | 0.456 |
| Asian | 4 | 4.8 % | 3 | 1.3 % | 0.080 |
| Opioids present and considered causative of death | |||||
| Methadone | 21 | 25.0 % | 126 | 53.2 % | <0.001 |
| Morphine | 25 | 29.8 % | 60 | 25.3 % | 0.428 |
| Oxycodone | 26 | 31.0 % | 45 | 19.0 % | 0.023 |
| Hydrocodone | 19 | 22.6 % | 33 | 13.9 % | 0.063 |
| Fentanyl | 5 | 6.0 % | 12 | 5.1 % | 0.755 |
| Heroin (as 6-MAM) | 5 | 6.0 % | 26 | 11.0 % | 0.181 |
| More than one opioid | 24 | 28.6 % | 69 | 29.1 % | 0.925 |
| Other substances present at death | |||||
| No cocaine, amphetamines, alcohol or benzodiazepines | 22 | 26.2 % | 58 | 24.5 % | 0.754 |
| Cocaine | 17 | 20.2 % | 96 | 40.5 % | 0.001 |
| Alcohol | 16 | 19.0 % | 46 | 19.4 % | 0.942 |
| Antidepressant | 21 | 25.0 % | 53 | 22.4 % | 0.622 |
| Benzodiazepines | 35 | 41.7 % | 54 | 22.8 % | 0.001 |
| Amphetamines | 7 | 8.3 % | 38 | 16.0 % | 0.081 |
| Location of death | |||||
| Hospital | 6 | 7.1 % | 12 | 5.1 % | 0.477 |
| Public space | 5 | 6.0 % | 18 | 7.6 % | 0.616 |
| Shelter/transitional housing | 0 | 0.0 % | 5 | 2.1 % | 0.217 |
| Hotel, not SRO | 3 | 3.6 % | 9 | 3.8 % | 0.613 |
| Private residence (All) | 70 | 83.3 % | 193 | 81.4 % | 0.698 |
| Own SRO | 0 | 0.0 % | 79 | 33.3 % | <0.001 |
| Own non-SRO residence | 63 | 75.0 % | 75 | 31.6 % | <0.001 |
| Friend/other residence | 7 | 8.3 % | 39 | 16.5 % | 0.070 |
| All SRO | 0 | 0.0 % | 103 | 43.5 % | <0.001 |
Italicised data indicate significant variables or ratios with a p-value <0.05.
Heroin Decedents
Thirty-one deaths involved heroin (Table 3), ten of which also involved prescription opioids. Deaths were evenly distributed over the 3 years examined, with a heroin-involved overdose death rate of 49.1 to 76.8 per 100,000 person years among heroin injectors based on the estimated number of heroin injectors in San Francisco.30
TABLE 3.
Heroin involved deaths versus non-heroin opioid deaths comparison
| Heroin involved deaths | Non-heroin opioid deaths | p value | |||
|---|---|---|---|---|---|
| Count | Count | ||||
| n = 31 | % | n = 300 | % | ||
| Age (years) | |||||
| 18–24 | 6 | 18.8 % | 14 | 4.7 % | 0.001 |
| 25–34 | 2 | 6.3 % | 33 | 11.0 % | 0.433 |
| 35–44 | 6 | 18.8 % | 59 | 19.7 % | 0.967 |
| 44–54 | 5 | 15.6 % | 85 | 28.3 % | 0.137 |
| 55–64 | 11 | 34.4 % | 91 | 30.3 % | 0.554 |
| >65 | 1 | 3.1 % | 17 | 5.7 % | 0.546 |
| Mean (IQR) | 45.0 | (39.92–50.08) | 48.5 | (47.15–49.82) | 0.066 |
| Sex | |||||
| Male | 24 | 75.0 % | 202 | 67.3 % | 0.251 |
| Race | |||||
| Non-Hispanic White | 22 | 68.8 % | 213 | 71.0 % | 0.997 |
| African-American | 6 | 18.8 % | 60 | 20.0 % | 0.932 |
| Hispanic | 3 | 9.4 % | 11 | 3.7 % | 0.133 |
| Asian | 0 | 0.0 % | 7 | 2.3 % | 0.489 |
| Opioids Present at Death | |||||
| Methadone | 6 | 18.8 % | 146 | 48.7 % | 0.002 |
| Morphine | 0 | 0.0 % | 89 | 29.7 % | <0.001 |
| Oxycodone | 1 | 3.1 % | 71 | 23.7 % | 0.009 |
| Hydrocodone | 2 | 6.3 % | 52 | 17.3 % | 0.119 |
| Fentanyl | 1 | 3.1 % | 17 | 5.7 % | 0.568 |
| Heroin (as 6-MAM) | – | – | – | – | – |
| More than one opioid | 10 | 31.3 % | 86 | 28.7 % | 0.675 |
| Other substances present at death | |||||
| No cocaine, amphetamines, alcohol or benzodiazepines | 7 | 21.9 % | 76 | 25.3 % | 0.736 |
| Cocaine | 17 | 53.1 % | 100 | 33.3 % | 0.017 |
| Alcohol | 9 | 28.1 % | 56 | 18.7 % | 0.167 |
| Antidepressant | 2 | 6.3 % | 73 | 24.3 % | 0.024 |
| Benzodiazepines | 4 | 12.5 % | 87 | 29.0 % | 0.056 |
| Amphetamines | 6 | 18.8 % | 40 | 13.3 % | 0.356 |
| Location of death | |||||
| Hospital | 1 | 3.1 % | 27 | 9.0 % | 0.271 |
| Public space | 7 | 21.9 % | 16 | 5.3 % | <0.001 |
| Shelter/transitional housing | 0 | 0.0 % | 5 | 1.7 % | 0.600 |
| Hotel, not SRO | 2 | 6.3 % | 10 | 3.3 % | 0.325 |
| Private residence (All) | 21 | 65.6 % | 242 | 80.7 % | 0.090 |
| Own SRO | 6 | 18.8 % | 73 | 24.3 % | 0.536 |
| Own non-SRO residence | 9 | 28.1 % | 129 | 43.0 % | 0.133 |
| Friend/other residence | 6 | 18.8 % | 40 | 13.3 % | 0.356 |
| All SRO | 10 | 31.3 % | 93 | 31.0 % | 0.855 |
| San Francisco resident | 23 | 71.9 % | 262 | 87.6 % | 0.044 |
Italicised data indicate significant variables or ratios with a p-value <0.05.
On univariate analysis, heroin-involved deaths were more likely than non-heroin opioid deaths to be 18 to 24 years of age and to involve methadone, morphine, or oxycodone (p ≤ 0.01 for all cases), as well as cocaine (p = 0.01), but less likely to involve antidepressants (p = 0.024) or be San Francisco residents prior to death (p = 0.04) (Table 3). On multivariable logistic regression analysis, heroin deaths were more likely to involve cocaine and be found in a public space, but less likely to involve prescription opioids such as methadone, morphine, or oxycodone (Table 4).
TABLE 4.
Multivariate comparison of heroin involved deaths versus non-heroin opioid deaths
| Heroin involved deaths | 95 % CI | p value | ||
|---|---|---|---|---|
| Odds ratio | ||||
| Demographics | ||||
| Age | Age 25 and older | Referent | 0.92–15.73 | 0.063 |
| Age 18 to 24 | 3.82 | |||
| Gender | Female | Referent | 0.47–3.91 | 0.565 |
| Male | 1.36 | |||
| Ethnicity | Non-hispanic ethnicity | Referent | 0.28–16.92 | 0.453 |
| Latino/Hispanic | 2.19 | |||
| Opioids present at death | ||||
| Morphine | No | Referent | ||
| Yes | 0.04 | 0.00–0.28 | 0.002 | |
| Methadone | No | Referent | ||
| Yes | 0.08 | 0.03–0.25 | <0.001 | |
| Oxycodone | No | Referent | ||
| Yes | 0.05 | 0.06–0.37 | 0.004 | |
| Other substances present at death | ||||
| Cocaine | No | Referent | ||
| Yes | 3.80 | 1.49–9.66 | 0.005 | |
| Location of death | ||||
| Public space | No | Referent | 0.89–14.73 | 0.072 |
| Yes | 3.63 | |||
Italicised data indicate significant variables or ratios with a p-value <0.05.
Discussion
From 2010 to 2012, the opioid overdose death rate in the City and County of San Francisco was 2.23 times the national average,1 2.57 times the local rate of vehicular death, and 1.94 times the citywide homicide rate.28 Reflecting other national, state, and city level data,2,9,12 opioid overdose death in San Francisco largely affected middle-aged, non-Hispanic white males. Most deaths involved often high-potency prescription opioids including methadone and morphine, although oxycodone and hydrocodone were also substantial contributors. Most prescription opioid overdoses occurred with other illicit or sedating substances (e.g., cocaine, alcohol, and benzodiazepines). In contrast to other studies,36 African-Americans were disproportionately affected by opioid overdose relative to their population in San Francisco.
Compared to an analysis of opioid overdose death from 1997 to 2000,27 prescription opioids have replaced heroin as the primary cause of opioid overdose mortality in San Francisco. Heroin was involved in 9.4 % of all opioid overdose deaths and occurred in isolation without another opioid present in only 21 cases. This marks a dramatic reduction in heroin-related deaths from 183 in 1999.27 The reasons for this reduction may be related to both the introduction of “treatment-on-demand,” with improved access to opioid agonist maintenance therapy, and broad distribution of naloxone, the short-acting opioid antagonist, to heroin users.38 The Drug Overdose Prevention and Education Project distributed naloxone to over 4000 persons from 2003 to 2012 and documented 449 opioid overdose reversals from 2010 to 2012. Over 91 % of these reversed overdoses were due to heroin, suggesting that naloxone distribution, based largely on syringe exchange programs, reached heroin users rather than prescription opioid users.39 In the context of these and other data associating naloxone distribution with remarkable community-level reductions in opioid overdose mortality,40 expanding the prescription of naloxone to patients receiving prescription opioids and individuals in single-room occupancy hotels may help to reduce opioid overdose death in San Francisco.
Opioid overdose deaths remained concentrated in central San Francisco neighborhoods (Tenderloin/Civic Center and South of Market) with high poverty rates, high numbers of single room occupancy hotels, and high levels of opioid-related drug arrests.41–43 This geospatial distribution showed some overlap with heroin overdose deaths from 1997 to 2000;37 however, there were many more deaths in outlying neighborhoods, suggesting a more varied population affected by prescription opioids. We did not observe distinct geographic differences between prescription opioids and heroin deaths, as seen in New York City,15,24 but we did identify an association between high poverty areas with methadone-involved deaths and low poverty areas with oxycodone and benzodiazepine-involved deaths. Decedents in high poverty areas were more likely to have multiple illicit substances present, including cocaine and methamphetamine, compared to decedents in low poverty areas, where benzodiazepines were more frequent. The lack of clear geospatial differences in heroin compared to prescription opioid deaths may be due to the very low rate of heroin overdose death in San Francisco, the overlapping neighborhoods of San Francisco, or a different pattern of prescription opioid use and overdose in San Francisco compared to New York City. The broad dispersion of deaths compared to earlier analyses suggests that opioid safety interventions should be implemented throughout the city, including more affluent areas that may be prescribing opioids in conjunction with benzodiazepines or other central nervous system depressants. Additionally, sustained efforts to address overdose risk in SROs and the central neighborhoods of San Francisco, where opioid overdose deaths remain concentrated and social isolation is a major risk, are needed.
Our study has several limitations. Medical examiner data relies on the individual judgment of the investigating forensic pathologist in classifying deaths as accidental versus intentional overdose and in determining which substances found on toxicology are likely to have contributed to death, both of which may have led to misclassification of cases. Additionally, there are limitations stemming from variations in the collection of biological specimens at autopsy, the interval between death and specimen collection, the analytical limitations of the scope of drugs screened for, and the limits of detection and quantitation due to limitations in the current analytic equipment at the Office of the Chief Medical Examiner. Finally, we were unable to determine if opioids involved in deaths were prescribed to the decedents due to a prohibition on research use of prescription drug monitoring data in the authorizing California state law.
Conclusions
Opioid overdose death in San Francisco from 2010 to 2012 was almost exclusively due to prescription opioids, a major transition from the prior decade when heroin was the driver of such deaths. While opioid overdose still disproportionately affects persons in high-poverty areas and racial minorities, over this period, opioid overdose death became more dispersed throughout the city with different causal drugs in affluent versus high poverty neighborhoods. Interventions proven to reduce opioid overdose mortality include expanded access to agonist maintenance therapies and distribution of naloxone. Opioid stewardship interventions, intended to reduce misuse of prescription opioids, may also be of benefit. Ensuring sufficient forensic resources for comprehensive postmortem assessment of drug-involved cases and prompt communication of resultant data to public health providers may enhance the ability to implement and assess such opioid safety initiatives.
Electronic supplementary material
(XLSX 53 kb)
(JPEG 1025 kb)
(JPEG 1114 kb)
(PNG 256 kb)
Acknowledgments
The authors would like to thank the members of the University of California, San Francisco Drug Users Research Group for their insight on an earlier presentation of this research.
Disclaimer
The findings and conclusions in this paper are those of the authors and do not necessarily represent the views of the San Francisco Department of Public Health.
Funding
National Institute on Drug Abuse (R03DA038084).
References
- 1.Centers for Disease Control and Prevention. National Vital Statistics System. Multiple Cause of Death File. Hyattsville, MD: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2012.
- 2.Paulozzi LJ, J. C, Mack K, Rudd R, Centers for Disease Control and Pre- vention (CDC). Vital signs: overdoses of prescription opioid pain relievers---United States, 1999--2008. MMWR Morb Mortal Wkly Rep. 2011; 60(43), 1487–1492. [PubMed]
- 3.Jones CM, Mack KA, Paulozzi LJ. Pharmaceutical overdose deaths, United States, 2010. JAMA. 2013;309(7):657–9. doi: 10.1001/jama.2013.272. [DOI] [PubMed] [Google Scholar]
- 4.Jones CM. Frequency of prescription pain reliever nonmedical use: 2002–2003 and 2009–2010. Arch Intern Med. 2012;172(16):1265–7. doi: 10.1001/archinternmed.2012.2533. [DOI] [PubMed] [Google Scholar]
- 5.Hansen RN, Oster G, Edelsberg J, Woody GE, Sullivan SD. Economic costs of nonmedical use of prescription opioids. Clin J Pain. 2011;27(3):194–202. doi: 10.1097/AJP.0b013e3181ff04ca. [DOI] [PubMed] [Google Scholar]
- 6.Masson CL, Sorensen JL, Batki SL, Okin R, Delucchi KL, Perlman DC. Medical service use and financial charges among opioid users at a public hospital. Drug Alcohol Depend. 2002;66(1):45–50. doi: 10.1016/S0376-8716(01)00182-X. [DOI] [PubMed] [Google Scholar]
- 7.Coffin PO, Sullivan SD. Cost-effectiveness of distributing naloxone to heroin users for lay overdose reversal. Ann Intern Med. 2013;158(1):1–9. doi: 10.7326/0003-4819-158-1-201301010-00003. [DOI] [PubMed] [Google Scholar]
- 8.Coffin PO, Sullivan SD. Cost-effectiveness of distributing naloxone to heroin users for lay overdose reversal in Russian cities. J Med Econ. 2013;16(8):1051–60. doi: 10.3111/13696998.2013.811080. [DOI] [PubMed] [Google Scholar]
- 9.Paulozzi LJ, Xi Y. Recent changes in drug poisoning mortality in the United States by urban–rural status and by drug type. Pharmacoepidemiol Drug Saf. 2008;17(10):997–1005. doi: 10.1002/pds.1626. [DOI] [PubMed] [Google Scholar]
- 10.Paulozzi LJ, Logan JE, Hall AJ, McKinstry E, Kaplan JA, Crosby AE. A comparison of drug overdose deaths involving methadone and other prescription opiates in West Virginia. Addiction. 2009;104(9):1541–8. doi: 10.1111/j.1360-0443.2009.02650.x. [DOI] [PubMed] [Google Scholar]
- 11.Johnson EM, Lanier WA, Merrill RM, Crook J, Porucznik CA, Rolfs RT, et al. Unintentional prescription opioid-related overdose deaths: Description of decedents by next of kin or best contact, Utah, 2008–2009. J Gen Intern Med. 2013;28(4):522–9. doi: 10.1007/s11606-012-2225-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Piercefield E, Archer P, Kemp P, Mallonee S. Increase in unintentional medication overdose deaths: Oklahoma, 1994–2006. Am J Prev Med. 2010;39(4):357–63. doi: 10.1016/j.amepre.2010.05.016. [DOI] [PubMed] [Google Scholar]
- 13.Bohnert AS, Valenstein M, Bair MJ, Ganoczy D, McCarthy JF, Ilgen MA, et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305(13):1315–21. doi: 10.1001/jama.2011.370. [DOI] [PubMed] [Google Scholar]
- 14.Dunn KM, Saunders KW, Rutter CM, Banta-Green CJ, Merrill JO, Sullivan MD, et al. Opioid prescriptions for chronic pain and overdose: a cohort study. Ann Intern Med. 2010;152(2):85–92. doi: 10.7326/0003-4819-152-2-201001190-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cerda M, Ransome Y, Keyes KM, Koenen KC, Tracy M, Tardiff KJ et al. Prescription opioid mortality trends in New York City, 1990–2006: Examining the emergence of an epidemic. Drug Alcohol Depend. 2013. [DOI] [PMC free article] [PubMed]
- 16.Mack K, Jones C, Paulozzi L, CDC Vital signs: overdoses of prescription opioid pain relievers and other drugs among women–United States, 1999–2010. MMWR Morb Mortal Wkly Rep. 2013;62(26):537–42. [PMC free article] [PubMed] [Google Scholar]
- 17.Shah NG, Lathrop SL, Reichard RR, Landen MG. Unintentional drug overdose death trends in New Mexico, USA, 1990–2005: Combinations of heroin, cocaine, prescription opioids and alcohol. Addiction. 2008;103(1):126–36. doi: 10.1111/j.1360-0443.2007.02054.x. [DOI] [PubMed] [Google Scholar]
- 18.Martins SS, Fenton MC, Keyes KM, Blanco C, Zhu H, Storr CL. Mood and anxiety disorders and their association with non-medical prescription opioid use and prescription opioid-use disorder: Longitudinal evidence from the National Epidemiologic Study on Alcohol and Related Conditions. Psychol Med. 2012;42(6):1261–72. doi: 10.1017/S0033291711002145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bohnert AS, Valenstein M, Bair MJ, Ganoczy D, McCarthy JF, Ilgen MA, et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305(13):1315–21. doi: 10.1001/jama.2011.370. [DOI] [PubMed] [Google Scholar]
- 20.Coolen P, Best S, Lima A, Sabel J, Paulozz L. Overdose deaths involving prescription opioids among Medicaid enrollees—Washington, 2004–2007. MMWR Morb Mortal Wkly Rep. 2009;58(42):1171–5. [PubMed] [Google Scholar]
- 21.Peavy KM, Banta-Green CJ, Kingston S, Hanrahan M, Merrill JO, Coffin PO. “Hooked on” prescription-type opiates prior to using heroin: Results from a survey of syringe exchange clients. J Psychoactive Drugs. 2012;44(3):259–65. doi: 10.1080/02791072.2012.704591. [DOI] [PubMed] [Google Scholar]
- 22.Unick GJ, Rosenblum D, Mars S, Ciccarone D. Intertwined epidemics: National demographic trends in hospitalizations for heroin- and opioid-related overdoses, 1993–2009. PLoS ONE. 2013;8(2):e54496. doi: 10.1371/journal.pone.0054496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Galea S, Ahern J, Vlahov D, Coffin PO, Fuller C, Leon AC, et al. Income distribution and risk of fatal drug overdose in New York City neighborhoods. Drug Alcohol Depend. 2003;70(2):139–48. doi: 10.1016/S0376-8716(02)00342-3. [DOI] [PubMed] [Google Scholar]
- 24.Cerda M, Ransome Y, Keyes KM, Koenen KC, Tardiff K, Vlahov D, et al. Revisiting the role of the urban environment in substance use: the case of analgesic overdose fatalities. Am J Public Health. 2013;103(12):2252–60. doi: 10.2105/AJPH.2013.301347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Seal KH, Kral AH, Gee L, Moore LD, Bluthenthal RN, Lorvick J, et al. Predictors and prevention of nonfatal overdose among street-recruited injection heroin users in the San Francisco Bay Area, 1998–1999. Am J Public Health. 2001;91(11):1842–6. doi: 10.2105/AJPH.91.11.1842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Substance Abuse and Mental Health Services Administration (SAMHSA). Drug Abuse Warning Network, 2011 Emergency Department Excel Files, Metro Division, San Francisco. Rockville, MD: Office of Applied Studies, SAMHSA; 2011 URL:http://www.samhsa.gov/data/DAWN.aspx#San Francisco – SF Div. Accessed: 20 June 2014. (Archived by WebCite® at http://www.webcitation.org/6QTWSV2Aq).
- 27.Davidson PJ, McLean RL, Kral AH, Gleghorn AA, Edlin BR, Moss AR. Fatal heroin-related overdose in San Francisco, 1997–2000: a case for targeted intervention. J Urban Health. 2003;80(2):261–73. doi: 10.1093/jurban/jtg029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hart A. Office of the Chief Medical Examiner City and County of San Francisco. San Francisco, CA: Fiscal Year 2013–2014 Annual Report for FY 2010–2011; 2013.
- 29.United States Census Bureau, American FactFinder. DP03: HC01_VC171: Percentage of Families and People Whose Income in the Past 12 Months Is Below the Poverty Level – 18 years and over. 2009 – 2011 American Community Survey. US Census Bureau American Community Survey Office, 2011. URL: http://factfinder2.census.gov. Accessed: 20 June 2014. (Archived by WebCite® at http://www.webcitation.org/6QSvzoDqd).
- 30.H Fisher Raymond, from National HIV Behavior Surveillance Survey for Injection Drug Users. San Francisco, CA: Personal Communication; 2014.
- 31.City and County of San Francisco Department of City Planning. Neighborhood Groups Map. 2014. URL:http://sf-planning.org/index.aspx?page=1654. Accessed: 20 June 2014. (Archived by WebCite® at http://www.webcitation.org/6QStnXbQz).
- 32.ESRI . ArcGIS Desktop: release 10. Redlands, CA: Environmental Systems Research Institute; 2011. [Google Scholar]
- 33.Schneider A. GPS Visualizer. GPS Visualizer. 2013. URL:http://www.gpsvisualizer.com/. Accessed: 20 June 2014. (Archived by WebCite® at http://www.webcitation.org/6QSrTBinh).
- 34.Heinze G, Schemper M. A solution to the problem of separation in logistic regression. Stat Med. 2002;21(16):2409–19. doi: 10.1002/sim.1047. [DOI] [PubMed] [Google Scholar]
- 35.United States Census Bureau. Summary File. 2007 – 2011 American Community Survey. U.S. Census Bureau’s American Community Survey Office. 2013. URL: http://ftp2.census.gov. Accessed: 20 June 2014. (Archived by WebCite® at http://www.webcitation.org/6QSvzoDqd).
- 36.Green TC, Grau LE, Carver HW, Kinzly M, Heimer R. Epidemiologic trends and geographic patterns of fatal opioid intoxications in Connecticut, USA: 1997–2007. Drug Alcohol Depend. 2011;115(3):221–8. doi: 10.1016/j.drugalcdep.2010.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Davidson PJ, McLean RL, Kral AH, Gleghorn AA, Edlin BR, Moss AR. Fatal heroin-related overdose in San Francisco, 1997–2000: a case for targeted intervention. J Urban Health. 2003;80(2):261–73. doi: 10.1093/jurban/jtg029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Enteen L, Bauer J, McLean R, Wheeler E, Huriaux E, Kral AH, et al. Overdose prevention and naloxone prescription for opioid users in San Francisco. J Urban Health. 2010;87(6):931–41. doi: 10.1007/s11524-010-9495-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Eliza Wheeler, DOPE Project. Oakland, CA: Personal Communication; 2014.
- 40.Walley AY, Xuan Z, Hackman HH, Quinn E, Doe-Simkins M, Sorensen-Alawad A, et al. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: Interrupted time series analysis. BMJ. 2013;346:f174. doi: 10.1136/bmj.f174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.San Francisco Planning Commission . San Francisco Neighborhoods Socio-Economic Profiles. San Francisco, CA: American Community Survey 2005–2009; 2011. [Google Scholar]
- 42.Fribourg A. San Francisco’s Single-Room Occupancy (SRO) Hotels: A Strategic Assessment of Residents and Their Human Service Needs. A Study Conducted for the San Francisco Human Services Agency (SF-HSA), San Francisco, California. 2009. URL: http://www.sfdaas.org/asset/ReportsDataResources/CollectedSROReports.pdf. Accessed: 20 June 2014. (Archived by WebCite® at http://www.webcitation.org/6QSqk50kG).
- 43.San Francisco Policy Department. San Francisco Police Department Crime MAPS. 2014. URL:http://www.sf-police.org/index.aspx?page=1618. Accessed: 20 June 2014. (Archived by WebCite® at http://www.webcitation.org/6QSr6H1uK).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX 53 kb)
(JPEG 1025 kb)
(JPEG 1114 kb)
(PNG 256 kb)