Abstract
Background:
One of the most important problems after episiotomy is perineal pain which is more severe on the first day of postpartum period. The aim of this study was to compare the analgesic effects of indomethacin suppository and lidocaine cream in the management of post-episiotomy pain.
Materials and Methods:
In a randomized, controlled trial, 60 primiparous women who had mediolateral episiotomy received 50 mg indomethacin suppository (n = 30) or 2% lidocaine cream (n = 30) in the postpartum period in Hajar Hospital in Shahrekord (Iran). The mean severity of post-episiotomy pain was assessed with the first complaint and at 6, 12, and 24 h after the delivery, and compared in the two groups. The visual analog scale (VAS) was used for pain recording and data were analyzed with independent-samples t-test, χ2, and Fisher's exact tests, and significance was defined as P < 0.05.
Results:
With the first complaint of pain, the mean intensity of pain was 4.9 (1.9) in the indomethacin group and 4.9 (1.8) in the lidocaine group, and the difference was not significant (P = 0.25). Six hours after birth, it was 3.3 (1.3) in the indomethacin group and 3.2 (1.9) in the lidocaine group, and there was not a significant difference between the two groups (P = 0.90). No significant difference was found between the two groups at 12 h after birth [2.3 (1.7) vs 2.5 (1.7); P = 0.59]. Also, the difference was not significant at 24 h after birth [1.5 (1.3) vs 1.8 (1.3); P = 0.31].
Conclusions:
It was concluded from the study that indomethacin suppository and lidocaine cream have similar efficacy on episiotomy pain relief on the first day of postpartum period.
Keywords: Episiotomy pain, indomethacin suppository, lidocaine cream, primiparous
INTRODUCTION
Episiotomy or tearing of perineal tissues during childbirth is a common surgical procedure, despite little evidences supporting its routine use.[1,2] At least 65% of women in developed countries and 35-45% of women in undeveloped countries who give birth in a hospital setting experience an episiotomy.[3] However, the degree of perineal discomfort related to perineal trauma is often underestimated.[4] It interferes with basic daily activities and impacts on motherhood experiences.[3] An estimated 10% of women suffer pain in the 3 months after childbirth,[5,6] although this may be a significant underestimate of the size of the problem, with a recent Australian study reporting that 94% of women experienced one or more health problems up to 6 months after birth.[7] Factors that may influence the intensity of pain experienced include the mode of birth,[8] the degree of perineal trauma,[7] and the technique of perineal repair.[9,10]
For relieving the episiotomy pain, both non-pharmacological and pharmacological methods are tested. Application of heat or cold and sitz baths are examples of non-pharmacological methods of pain relief that are often inadequate. Acetaminophen with codeine is frequently used, but adverse effects, such as constipation, nausea, stomach pain, and dizziness, limit its appeal.[11] In the management of post-episiotomy pain, nonsteroidal anti-inflammatory drugs (NSAIDs) have been found to be effective, without related illness from adverse effects.[12] Pitangui et al. examined the effectiveness of high-frequency transcutaneous electrical nerve stimulation (TENS) on pain of primiparous puerpera who had experienced natural childbirth with an episiotomy, and reported that high-frequency TENS treatment (100 Hz frequency and 75 μs pulse for 60 min) significantly reduced pain intensity of episiotomy.[13] In the other study in 2012, Santos et al. examined the low-level laser therapy for pain relief after episiotomy and surveyed 115 women with right mediolateral episiotomy, and reported that low-level laser therapy cannot decrease perineal pain related to episiotomy.[14] Peter et al. compared ibuprofen (400 mg) versus acetaminophen (600 mg) with codeine (60 mg) in relieving perineal pain after childbirth, and reported that although both drugs have similar effect on patients’ pain, ibuprofen may be the preferred choice because it is less expensive and requires less nursing time to dispense.[11] In another study, in 2004, Dodd et al. examined the effect of rectal NSAID suppository on perineal pain after childbirth in Australia and reported that diclofenac suppository is a simple, effective, and safe drug for reducing the pain experienced by women following perineal trauma within the first 24 h after childbirth.[3]
In Hajar Hospital in Iran, there is no national protocol for postpartum pain management. Various analgesic drugs such as acetaminophen, ibuprofen, naproxen, etc., are used for postpartum pain treatment. Regarding the adverse effects of oral analgesic medications to relieve pain, such as gastrointestinal problems, nausea, and vomiting, and the limited evidences on comparing the efficacy and safety of rectal and local analgesia, this study was aimed to compare the effectiveness of indomethacin suppository and lidocaine cream on post-episiotomy pain.
MATERIALS AND METHODS
This study is a randomized, controlled trial conducted from February 2011 to December 2011 at the antenatal clinic and post-delivery ward in Hajar Hospital, a university hospital and referral center for obstetric care in Shahrekord, Iran. Permission was obtained for this study from the deputy of research and also from the ethics board of the Shahrekord University of Medical Sciences (Code of Ethics: 90-4-9). The clinical trial code of the study was obtained from Iranian Registry of Clinical Trials (IRCT201104253078N7). Primiparous women who have had normal vaginal delivery with mediolateral episiotomy and were experiencing perineal pain were recruited in the study. Exclusion criteria included women who had manual removal of placenta, severe asthma, gastric or duodenal ulcer, and preeclampsia. Women with a known sensitivity to NSAIDs, laceration of perineum, length of episiotomy larger than 5 cm, and adverse reaction to local anesthetics were also excluded. Participants received written and verbal information about the study at 37 weeks at the antenatal clinic and they were given the same information on admission to the postnatal ward by the ward midwife. All participants who agreed with the study procedures and voluntarily agreed to participate signed the free and informed consent form. The women were randomized by consecutively numbered sealed envelopes to one of the two study arms, that is, 2% lidocaine cream (n = 30) or 50 mg indomethacin suppository (n = 30). The study was not blinded to the women and investigators, but it was blinded for analyzer of data. The randomization schedules were prepared by a researcher not involved in patient care, using a computer-generated random number table, and the randomization was stratified for mode of birth (spontaneous vaginal birth vs instrumental vaginal birth).
After birth and at the time of post-delivery ward admission, the intensity of perineal pain was assessed with visual analog scale (VAS) by the ward midwife, with the first complaint of women and before the patients taking the first dose of medications in the two groups. Then 50 mg indomethacin rectal suppository was administered to patients in the first group and the patients in the second group received the 5 ml lidocaine cream 2% on the episiotomy line. Lidocaine topical cream was manufactured by Tehran Chemie Pharmaceutical Company (Tehran, Iran) and each 100 g of the cream contains lidocaine 2.5 g and prilocaine 2.5 g. Indomethacin suppository was manufactured by Caspian-Tamin Company (Rasht, Iran) and each suppository contains 50 mg indomethacin. Drugs were available in the hospital pharmacy. Socio-demographic information was obtained from the patient records. Women were asked to score their pain from 0 = no pain to 10 = worst possible pain in the VAS.[9] The primary outcomes were pain scores at 6, 12, and 24 h after birth with rest. The secondary outcomes relating to pain were the number of doses of medication, use of additional analgesia, time from birth to first analgesia, dosing intervals, and adverse effects of therapeutic medications. Data were analyzed by SPSS (version 16). Categorical variables were compared using χ2 and Fisher's exact tests and continuous variables were compared using independent samples t-test, and a P value of less than 0.05 was considered significant with confidence interval of 95%. The analysis was blinded to the treatment groups.
RESULTS
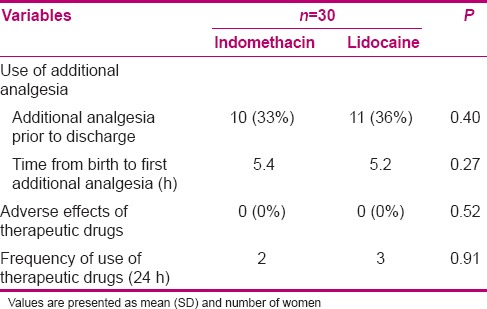
During the study period, a total of 420 women who gave birth at Hajar Hospital had perineal trauma requiring repairing during childbirth. A total of 280 gave written informed consent and 118 of them were potentially eligible for taking part in the trial. Of these, 58 women were excluded from the study as they were not experiencing perineal pain and 60 women met the inclusion criteria and were included in the study, with 30 randomized to receive indomethacin suppositories and the other 30 to receive lidocaine cream. The two groups were well matched for demographic characteristics at the trial entry and labor and birth outcomes [Table 1]. Study outcome data were available for 100% of women at 6, 12, and 24 h after birth. Comparison of the mean intensity of pain in the two groups is presented in Table 2, showing that there was no statistically significant difference in the intensity of pain with the first complaint of pain at rest between the two groups. Also, no significant differences were found in the intensity of pain at 6 h after childbirth between the two groups. Mean intensity of post-episiotomy pain showed no significant difference at 12 h after childbirth between the two groups. Also, the difference was not significant at 24 h after childbirth between the two groups. The incidence of use of medications during the 24 h after delivery and receiving the additional analgesic for pain relief of episiotomy showed no significant difference between the study groups. No adverse effects of medications were noted in the treatment groups [Table 3].
Table 1.
Maternal demographics and labor outcomes at trial entry
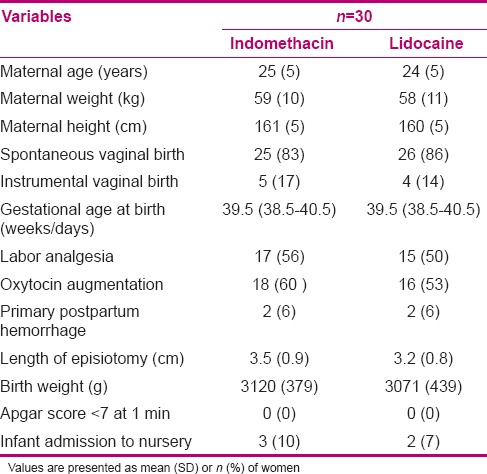
Table 2.
Primary outcomes measures
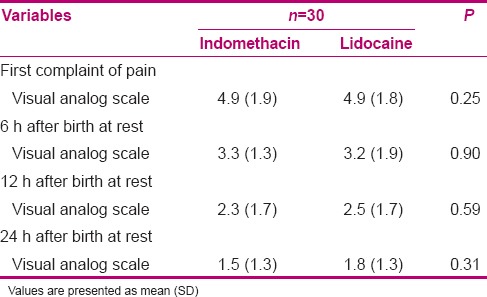
Table 3.
Secondary outcomes measures
DISCUSSION
The results of the present study showed that the indomethacin suppository and lidocaine cream have similar effects on pain relief post episiotomy. Few studies have compared the effectiveness of indomethacin and lidocaine cream on post-episiotomy pain relief. In this regard, one study reported that the lidocaine cream has reduced the pain intensity at 15 min after childbirth, but not at other times, and this study concluded that the analgesic effects of lidocaine cream are comparable to those of indomethacin suppository.[15] In other studies, the effects of indomethacin and lidocaine alone or in combination with other analgesic agents were assessed. In this regard, one study reported that the lidocaine jelly reduced the pain intensity in 6 and 12 h after administration.[16] Another study reported that there was not a significant difference between lidocaine jelly and placebo in reducing the pain intensity.[17] Another report indicated that lidocaine jelly and diclofenac suppository have similar effects on perineal pain during the first day after delivery.[18]
Women's perception of pain is subjective and the use of analgesia is influenced by many factors in addition to the level of pain experienced. These findings may reflect a policy of regular analgesia being offered and accepted on a routine basis to women in the postnatal period while in hospital.[3] Use of suppositories for the longer-term relief of pain and acceptability of rectal route of analgesia are less well reported. This study specifically addressed these questions. While rectal suppositories may be effective in reducing the perineal pain experienced after childbirth, drug effectiveness becomes a secondary consideration if women are not prepared to use a rectal route of administration. In detecting the acceptability of rectal analgesic suppositories, one study interviewed 400 surgical patients (both male and female), who were asked to choose between an intramuscular route of pain relief and rectal suppositories. Given a choice, only 18% of patients surveyed chose rectal suppositories as an acceptable method of pain relief.[19]
Indomethacin is almost completely protein bound, and as a result, minimal amounts of the drug are excreted in breast milk - an important consideration for women who are breast feeding.[20] One study reported that lidocaine jelly did not have any effect on women's consumption of oral analgesic.[10] No side effects of indomethacin suppository and lidocaine cream were found in the present study. Similar findings were reported in a study.[10] Although in the present study we did not find the side effects of analgesic agents, care should be maintained in prescribing these medications.[3] The strengths of our study include use of randomized design and measurement of the side effects of medications, and the study was limited by its small sample size and lack of follow-up of the participants at 48 h and in the first week of birth. In conclusion, our study demonstrated that the effectiveness of indomethacin rectal suppository and lidocaine cream was similar in post-episiotomy pain relief at 6, 12, and 24 h after birth.
CONCLUSION
The effectiveness of indomethacin rectal suppository and lidocaine cream was similar in post-episiotomy pain relief. Use of local and rectal analgesic agents is a simple, safe, and effective method for reducing the pain experienced by women following episiotomy within 6, 12, and 24 h after childbirth.
Footnotes
Source of Support: Granting Agency (grant NO.976): Faculty of Nursing and Midwifery, Shahrekord University of Medical Sciences, Shahrekord, Iran
Conflict of Interest: None declared.
REFERENCES
- 1.Hartmann K, Viswanathan M, Palmieri R, Gartlehner G, Thorp J, Jr, Lohr KN. Outcomes of routine episiotomy: A systematic review. JAMA. 2005;293:2141–8. doi: 10.1001/jama.293.17.2141. [DOI] [PubMed] [Google Scholar]
- 2.Nalbanski A, Nikolov A. Routine episiotomy-a five year practice at University Hospital “Majchin Dom. Akush Ginekol (Sofiia) 2009;48:11–4. [PubMed] [Google Scholar]
- 3.Dodd JM, Hedayati H, Pearce E, Hotham N, Crowther CA. Rectal analgesia for the relief of perineal pain after childbirth: A randomised controlled trial of diclofenac suppositories. BJOG. 2004;111:1059–64. doi: 10.1111/j.1471-0528.2004.00156.x. [DOI] [PubMed] [Google Scholar]
- 4.Steen M, Cooper K, Marchant P, Griffiths-Jones M, Walker J. A randomized controlled trial to compare the effectiveness of icepacks and Epifoam with cooling maternity gel pads at alleviating postnatal perineal trauma. Midwifery. 2000;16:48–55. doi: 10.1054/midw.1999.0188. [DOI] [PubMed] [Google Scholar]
- 5.Fauconnier A, Goltzene A, Issartel F, Janse-Marec J, Blondel B, Fritel X. Late post-partum dyspareunia: Does delivery play a role? Prog Urol. 2012;22:225–32. doi: 10.1016/j.purol.2012.01.008. [DOI] [PubMed] [Google Scholar]
- 6.Ejegård H, Ryding EL, Sjogren B. Sexuality after delivery with episiotomy: A long-term follow-up. Gynecol Obstet Invest. 2008;66:1–7. doi: 10.1159/000113464. [DOI] [PubMed] [Google Scholar]
- 7.Brown S, Lumley J. Maternal health after childbirth: Results of an Australian population based survey. Br J Obstet Gynaecol. 1998;105:156–61. doi: 10.1111/j.1471-0528.1998.tb10045.x. [DOI] [PubMed] [Google Scholar]
- 8.Buhling KJ, Schmidt S, Robinson JN, Klapp C, Siebert G, Dudenhausen JW. Rate of dyspareunia after delivery in primiparae according to mode of delivery. Eur J Obstet Gynecol Reprod Biol. 2006;124:42–6. doi: 10.1016/j.ejogrb.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 9.Kettle C, Johanson RB. Issue 4. Chichester, UK: Wiley; 2003. Continuous versus interrupted sutures for perineal repair [Cochrane review]. The Cochrane Library. [DOI] [PubMed] [Google Scholar]
- 10.Corkill A, Lavender T, Walkinshaw SA, Alfirevic Z. Reducing postnatal pain from perineal tears by using lignocaine gel: A double blindrandomised trial. Birth. 2001;28:22–7. doi: 10.1046/j.1523-536x.2001.00022.x. [DOI] [PubMed] [Google Scholar]
- 11.Peter EA, Janssen PA, Grange CS, Douglas MJ. Ibuprofen versus acetaminophen with codeine for the relief of perineal pain after childbirth: A randomized controlled trial. CMAJ. 2001;165:1203–9. [PMC free article] [PubMed] [Google Scholar]
- 12.Lim SS, Tan PC, Sockalingam JK, Omar SZ. Oral celecoxib versus oral diclofenac for post-perineal repair analgesia after spontaneous vaginal birth: A randomised trial. Aust N Z J Obstet Gynaecol. 2008;48:71–7. doi: 10.1111/j.1479-828X.2007.00808.x. [DOI] [PubMed] [Google Scholar]
- 13.Pitangui AC, de Sousa L, Gomes FA, Ferreira CH, Nakano AM. High-frequency TENS in post-episiotomy pain relief in primiparous puerpere: A randomized, controlled trial. J Obstet Gynaecol Res. 2012;38:980–7. doi: 10.1111/j.1447-0756.2011.01824.x. [DOI] [PubMed] [Google Scholar]
- 14.Santos Jde O, de Oliveira SM, da Silva FM, Nobre MR, Osava RH, Riesco ML. Low-level laser therapy for pain relief after episiotomy: A double-blind randomised clinical trial. J Clin Nurs. 2012;21:3513–22. doi: 10.1111/j.1365-2702.2011.04019.x. [DOI] [PubMed] [Google Scholar]
- 15.Seçkin B, Avşar F, Parlakyiğit E, Aksakal O. Effects of indomethacin suppository and lidocaine pomade for the relief of post-episiotomy pain. Int J Gynaecol Obstet. 2002;78:159–61. doi: 10.1016/s0020-7292(02)00103-0. [DOI] [PubMed] [Google Scholar]
- 16.Abedzadeh M, Sadat Z, SABERI F. Effect of lidocaine gel in pain relieving after episiotomy. Journal of Babol University of Medical Sciences. 2009;11:43–8. [Google Scholar]
- 17.Fardiazar Z, Zahery F, Sadegy Khamene S, Mohammad Alizade S, Kooshavar H. The Efficacy of 2% Lidocaine Gel in Healing the Episiotomy and Relieving Its Pain during Postpartum. J Ardabil Univ Med Sci. 2006;6:61–6. [Google Scholar]
- 18.Abedzadeh M, Sadat Z, Saberi F. The efficacy of 2% lidocaine gel versus diclofenac suppository in pain reliving after episiotomy. Koomesh. 2009;10:301–6. [Google Scholar]
- 19.Carroll M, Day F, Hennessy A, Buggy D, Cooney C. Patient attitudes to perioperative suppository administration for postoperative analgesia. Ir J Med Sci. 1996;165:286–8. doi: 10.1007/BF02943092. [DOI] [PubMed] [Google Scholar]
- 20.Lebedevs TH, Wojnar-Horton RE, Yapp P, Roberts MJ, Dusci LJ, Hackett LP, et al. Excretion of indomethacin in breast milk. Br J Clin Pharmacol. 2012;32:751–4. [PMC free article] [PubMed] [Google Scholar]


