Abstract
Introduction:
In developing countries, hemorrhage accounts for 30% of the maternal deaths. Postpartum hemorrhage has been defined as blood loss of around 500 ml or more, after completing the third phase of labor. Most cases of postpartum hemorrhage occur during the first hour after birth. The most common reason for bleeding in the early hours after childbirth is uterine atony. Bleeding during delivery is usually a visual estimate that is measured by the midwife. It has a high error rate. However, studies have shown that the use of a standard can improve the estimation. The aim of the research is to compare the estimation of postpartum hemorrhage using the weighting method and the National Guideline for postpartum hemorrhage estimation.
Materials and Methods:
This descriptive study was conducted on 112 females in the Omolbanin Maternity Department of Mashhad, for a six-month period, from November 2012 to May 2013. The accessible method was used for sampling. The data collection tools were case selection, observation and interview forms. For postpartum hemorrhage estimation, after the third section of labor was complete, the quantity of bleeding was estimated in the first and second hours after delivery, by the midwife in charge, using the National Guideline for vaginal delivery, provided by the Maternal Health Office. Also, after visual estimation by using the National Guideline, the sheets under parturient in first and second hours after delivery were exchanged and weighted. The data were analyzed using descriptive statistics and the t-test.
Results:
According to the results, a significant difference was found between the estimated blood loss based on the weighting methods and that using the National Guideline (weighting method 62.68 ± 16.858 cc vs. National Guideline 45.31 ± 13.484 cc in the first hour after delivery) (P = 0.000) and (weighting method 41.26 ± 10.518 vs. National Guideline 30.24 ± 8.439 in second hour after delivery) (P = 0.000).
Conclusions:
Natural child birth education by using the National Guideline can increase the accuracy of estimated blood loss. Therefore, training the personnel to use this guideline is recommended. However, It has less accuracy than 'sheet weighing’. Consequently, usage of symptoms and the weighing method is recommended in cases of postpartum bleeding.
Keywords: Gravimetric method, hemorrhage estimation, midwife, National Guideline, postpartum hemorrhage
INTRODUCTION
Postpartum hemorrhage is the major cause of maternal death, especially in developing countries.[1] Obstetric and delivery complications are responsible for around 536,000 maternal deaths across the world.[2]
Postpartum hemorrhage has been defined as a blood loss of around 500 ml or more after completing the third phase of labor.[3,4] It has been estimated that around 5% of the mothers who experience vaginal delivery, lose more than 1000 cc of blood. Therefore, if mother loses more than 500 ml, the physician must foresee severe hemorrhage.[4]
The Iranian Ministry of Health and Treatment reported maternal death as 25 out of 100,000 in 1385, the major cause of which was postpartum hemorrhage.[5]
Most of them were related to late diagnosis and late management of hemorrhage.[6,7] The late diagnosis could be related to less estimation of blood loss during labor.[8,9] The most common approach for estimating blood loss was the visual estimation method; however, several studies confirmed that it was not the correct method.[10,11,12]
Most specialists categorized hemorrhage based on visual estimation. The estimated blood loss was 100 – 150 cc less than the actual amount, and as a result, hemorrhage was estimated to be less than 500 ml in 30 – 50% of the cases.[10,11]
On the other hand, it seems applying the visual scale for estimating blood loss could be more helpful. For example, Wyatt et al., suggested a method for improving the accuracy of the visual scale during a menstrual period by a menstrual pictogram. Females used this pictogram to measure the quantity of their hemorrhage. Their estimation was largely in agreement with the laboratory diagnosis, with a specificity of 88% and a sensitivity of 88%. The total mean hemorrhage of the group with menstrual bleeding was 109 ml (15 – 836 ml).[13]
Bose et al. applied this method for preparing a similar pictogram, as an educational tool, for the Obstetrics Department. Low estimation was common in his study. Therefore, he concluded that the weak results of visual estimation confirmed the need for education.[14] Hence, it was necessary to use more effective methods for estimating postpartum hemorrhage.
One of the methods for blood loss is using the National Guidelines provided by the Maternal Health Office. It includes two general parts: The first part is related to providing healthcare services during normal delivery and the second is related to the manner in which care is provided. Estimating blood loss is discussed in the second part, including a picture that displays four bloody pads and the related amounts of blood loss for each one.[15]
The other method for estimating blood loss is the weighting method. The direct method (weighting) is one of the ancient methods for estimating the correct amount of bleeding. Lee et al., compared the gravimetric and laboratory methods of estimating the quantity of blood loss during operations in animals. Intraoperative blood loss was quantified by measuring the irrigation fluid and weighing the surgical sponges used for blood and fluid collection during surgery. The results of the gravimetric measurements were then correlated to the blood loss and quantified using the spectrophotometric analysis of hemoglobin (Hb) content. Homeostatic variables, including Buccal Mucosal Bleeding Time (BMBT), were measured before surgery and compared with the calculated amount of blood loss. They reported a high considerable correlation between the gravimetric and laboratory methods, which indicated that applying weight was the correct method for estimating blood loss.[16]
Application of weighting needs an accurate scale, which is time-consuming. On the other hand, the visual estimation method is one of the most common and ancient methods of measuring postpartum blood loss. Its accuracy can be increased by using a scale for estimating blood loss. This study aims to compare the estimation of postpartum hemorrhage using the weighting method and National Guideline with the postpartum hemorrhage estimation by midwives.
MATERIALS AND METHODS
This descriptive study was conducted on 112 females in the Omolbanin Maternity Department of Mashhad, for a six-month period, from November 2012 to May 2013. The accessible method was used for sampling. Inclusion criteria were, less than five deliveries, gestational age of 37 – 42 weeks, singleton pregnancy with cephalic presentation, neonatal weight of 2500 – 4000 g, dilation of 4 – 6 cm on admission, with regular uterine contractions lasting 30 – 90 seconds, and 2 – 5 contractions every 10 minutes, with no maternal risk factor (no midwifery or medical condition).
To begin with, the aim and method of the study were described to all the females. After taking informed consent, they were selected and selection forms were completed for them. Then they were interviewed for completing the demographic data and obstetrics data forms. When active labor was started, the labor progression form and pantographs were completed carefully based on researcher observation, and vital signs and contractions were also recorded.
The data collection tools were case selection, observation, and interview forms. The first checklist contained the case selection criteria. The second checklist contained two forms: Interview and observation forms.
The interview form included three sections: Demographic characteristics, history of previous pregnancies, and history of current pregnancy. The observation form included four sections: Information on the four stages of labor. Finally, there was a control form for vital signs and contractions from admission to discharge.
After complete discharge of the fetus, placenta, and membrane by the Brent maneuver, and pressing of the uterus for expelling the post placental clots, a rubber sheet and a carefully weighted sheet were spread under the parturient; then 10 units of oxytocin were injected intramuscularly (IM) into the gluteal muscles of all subjects. If the perineal area needed repair due to episiotomy or rupture, all the applied gauzes were weighted before, during, and after the repair and tampon process of the cervix. They were then recorded in the observation forms.
In the fourth phase of labor, the quantity of bleeding was estimated by the midwife in charge, using the National Guideline, and then the sheets under the parturient were exchanged and weighted by researcher in the first and second hours after delivery. The sheets were weighed by using the Bellini scale (error: 0.1 in 2 kg), for blood loss estimation.
On the basis of the National Guideline provided by the Maternal Health Office:
“Scant hemorrhage is blood and Lochia around 10 ml or less or a bloody pad less than 5 cm
“Light hemorrhage is blood and Lochia of 10 – 25 ml or a bloody pad less than 10 cm
“Moderate hemorrhage is blood and Lochia to 25 – 50 ml or bloody pad less than 15 cm
“Heavy/Profuse hemorrhage is blood and Lochia of 50 – 80 ml or one pad that becomes bloody in two hours
“Excessive hemorrhage is when one pad becomes bloody in 15 minutes or blood accumulates under the parturient. Clots larger than a lemon or a large amount of blood suddenly are indicators of excessive bleeding.
In the present study, midwives were asked to mark the following picture based on the hemorrhage in the first and second hours after delivery [Figure 1]. These data were recorded in the forms and the blood quantity and hemorrhage severity were also estimated.
Figure 1.
Picture of National Guideline for estimating postpartum hemorrhage. (Source: It is extracted from Reference 15. Country guide for Manual labor and presenting the drugs and non-drug methods for reducing labor pain)
The lactation period and neonatal sucking were recorded for all groups. When there was no problem, the parturient was transferred to the Gynecology/Maternity Department. Data were analyzed using descriptive statistics and the t- test. The significance level was considered as P < 0.05.
It should be noted that if a parturient had a hemorrhage of more than 500 ml and experienced no uterine contraction interventions, such as, manual massage, additional oxytocin prescription or Methergine, were implemented, then they were excluded from the study. These cases were referred to an obstetrician.
Ethical considerations
This study was approved by regional ethics committee of research of research chancellery of Mashhad University of Medical Sciences. All of the included subjects, after brief explanation of the study protocol, signed the informed consent. They were free to leave the study whenever unsatisfied during the study period.
RESULTS
The subjects were aged 25.24 ± 4.77 years. Most of them (33%) had a high school diploma and were housekeepers (97.3%); 49% of them were primipara, 29.5% had two, and 21.5% had three and more pregnancies; 51.8% of them had experienced no normal delivery before, 32.1% had one, 14.2% had two, and 1.9% had three or more normal deliveries; 7.1% had previous curettage and 92.9% reported no history of curettage. No one reported a history of Amniotic fluid infection or placental adhesion. The mean of the gestational age was 39.35 ± 1.761 years. The mean of the pregnancy interval (present with previous) was 4.74 ± 2.674 years.
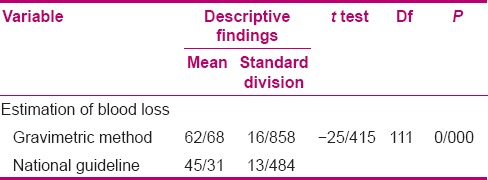
According to the results, a significant difference was found between the estimated blood loss based on the weighting methods and after using the National Guideline in the first hour after delivery (weighting 62.68 ± 16.858 cc vs. National Guideline 45.31 ± 13.484 cc) (P = 0.000) [Table 1].
Table 1.
Comparing estimation of postpartum hemorrhage using the weighting method and National Guideline postpartum hemorrhage in the first hour after delivery
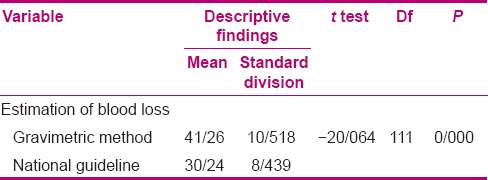
There was also a significant difference between the estimated blood loss based on the weighting method and using National Guideline, in the second hour (weighting method 41.26 ± 10.518 cc vs. National Guideline 30.24 ± 8.439 cc) (P = 0.000) [Table 2].
Table 2.
Comparing the estimation of postpartum hemorrhage using the weighting method and National Guideline postpartum hemorrhage in the second hour after delivery
DISCUSSION
A significant difference was found between blood loss estimation based on the weighting method and by using the National Guideline (P = 0.000).
In the mentioned studies, visual estimation was based on previous experience, and error in uneducated people was more than in the educated ones.[10] Education by simulation techniques could improve the abilities of the healthcare provider for estimating a predetermined quantity of blood in medical scenarios, however, these estimations are still incorrect, especially as the present study showed that although in voluminous hemorrhages,[10,17,18] the estimation of blood loss was improved by the picture guideline, it was still lower than the weighting method.
Prata et al., suggested an exclusive method for estimating blood loss by traditional birth attendants (TBAs), in Kigoma, Tanzania. ‘Kanga’ was a standard cut of cloth, such as a skirt or a scarf, which was used for carrying neonates. Traditionally old ‘kangas’ were used as towels for postpartum hemorrhage. After several measurements, it was concluded that two kangas absorb more than 500 ml of blood, therefore, the TBAs were educated and told that if a parturient had two kangas of hemorrhage, she was diagnosed as postpartum hemorrhage, and should be transferred. The TBAs should start their interventions at this point.[19] In this study, it was attempted to provide a more accurate estimation for postpartum hemorrhage, using a visual scale.
The direct measurement of blood is probably the most ancient method for reporting hemorrhage. Edhi et al., in their research to study the reasons for bleeding and correct bleeding control after delivery, concluded that assessment of the risk factor and estimation of blood loss are necessary to prevent this fatal condition. The following protocols are also important for improving the outcome of patients with massive bleeding.[20] Al kadri et al., has showed that the visual estimate of blood loss is 30% less than the weighting method, and the estimator (physician or nurse) plays no role in this estimation.[21] The present study confirms this finding.
According to the other studies, the methods that can be implemented with the least equipment and education, revolve around direct measurement and weighing.[11,12,21] The weighting method needs just a container and a scale and it can be considered for its advantages, however, some disadvantages have been noticed, for example, the need for a scale, the time consumed, need for weighing before and after by using pads, and some of the staff do not like this procedure, as they believe it may be infectious.
Some limitations could be considered, such as, false result due to collection of other fluids such as, urine with blood, which was inevitable. In the present study, the bladder was empty and this issue was controlled. The other limitation was that the study was done just on normal hemorrhage after delivery. It was recommended to study other voluminous hemorrhage after delivery. On the other hand, the picture presented in National Guideline should be applied cautiously because four pads, regardless of their quality, such as, difference in absorption or applied instruments, were used. It should be noted that in voluminous hemorrhage these pictures could be used less, because the vital signs should be paid more attention to. To sum up, although using a scale could improve an individual's estimation of blood loss, it was still different from the weighting method. It seemed that lack of clinical skills of the midwives for estimation of blood loss was one of the sources of errors on visual estimation. Thus, visual estimation using a scale could be helpful, but practical revision for applying this scale was recommended.
CONCLUSION
As the most common estimation method for blood loss is visual estimation, the National Guideline could be helpful, but it should be taught to the healthcare providers. However, it is of lower efficiency in comparison with the weighting method, for blood loss estimation. Thus, as management of postpartum hemorrhage is very important and the weighting method is simple and feasible for blood loss estimation in Maternity Departments, it is recommended to run workshops and educational programs for practical measurement of hemorrhage, using bloody pads.
ACKNOWLEDGMENT
This study is a result of Mashhad University of Medical Sciences (MUMS) approved research, proposed (approval code 910175). The authors appreciate the Vice Presidency of MUMS for the research, the Ethics Committee, authorities, and the special midwives of the Mashhad Omolbanin Hospital, for their kind cooperation.
Footnotes
Source of Support: Mashhad University of Medical Sciences.
Conflict of Interest: None declared.
REFERENCES
- 1.Shane B, Burns M, Dahlquist K. Preventing postpartum Hemorrhage: Managing the third stage of labor. Am Fam Physician. 2006;73:1025–8. [PubMed] [Google Scholar]
- 2.Khan KS, Wojdyla D, Say L, Gulmezoglu AM, Van Look PF. WHO analysis of causes of maternal death: A systematic review. Lancet. 2006;367:1066–74. doi: 10.1016/S0140-6736(06)68397-9. [DOI] [PubMed] [Google Scholar]
- 3.Geneva: World Health Organization; 2003. World Health Organization Managing Complications in Pregnancy and Childbirth: A guide for midwives and doctors. Department of Reproductive Health and Research. [Google Scholar]
- 4.Cunningham FG, Leveno KJ, Bloom SL, Hauth JC, Rouse DJ. New York: Mc Graw- Hill; 2010. Williams Obsetrics. [Google Scholar]
- 5.Abbaspoor Z, Vaziri I, Emam J. Sensitivity and specificity collector bag for the measurement of post-partum hemorrhage. J Guilan Univ Med Sci. 2012;83:58–64. [Google Scholar]
- 6.Mander R, Smith GD. Saving Mothers’ Lives (Formerly Why Mothers Die): Reviewing Maternal Deaths To Make Motherhood Safer 2003- 2005. Midwifery. 2008;24:8–12. doi: 10.1016/j.midw.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 7.Berg CJ, Harper MA, Atkinson SM, Bell EA, Brown HL, Hage ML, et al. Preventability of Pregnancy-Related Deaths: Results of A State-Wide Review. Obstet Gynecol. 2005;106:1228–34. doi: 10.1097/01.AOG.0000187894.71913.e8. [DOI] [PubMed] [Google Scholar]
- 8.Dildy III GA, Paine AR, George NC, Velasco C. Estimating Blood Loss: Can Teaching Significantly Improve Visual Estimation? Obstet Gynecol. 2004;104:601–7. doi: 10.1097/01.AOG.0000137873.07820.34. [DOI] [PubMed] [Google Scholar]
- 9.Stafford I, Dildy GA, Clark SL, Belfort MA. Visually Estimated and Calculated Blood Loss in Vaginal and Cesarean Delivery. Am J Obstet Gynecol. 2008;199:519–26. doi: 10.1016/j.ajog.2008.04.049. [DOI] [PubMed] [Google Scholar]
- 10.Glover P. Blood loss at delivery: How accurate is your estimation? Aust J Midwifery. 2003;16:21–4. doi: 10.1016/s1031-170x(03)80005-3. [DOI] [PubMed] [Google Scholar]
- 11.Patel A, Goudar SS, Geller SE, Kodkany BS, Edlavitch SA, Wagh K, et al. Drape estimation vs. visual assessment for estimating postpartum hemorrhage. Int J Gynaecol Obstet. 2006;93:220–4. doi: 10.1016/j.ijgo.2006.02.014. [DOI] [PubMed] [Google Scholar]
- 12.Schorn MN. Measurement of blood loss: Review of the literature. J Midwifery Womens Health. 2010;55:20–7. doi: 10.1016/j.jmwh.2009.02.014. [DOI] [PubMed] [Google Scholar]
- 13.Wyatt KM, Dimmock PW, Walker TJ, O’Brien PM. Determination of total menstrual blood loss. Fertil Steril. 2001;76:125–31. doi: 10.1016/s0015-0282(01)01847-7. [DOI] [PubMed] [Google Scholar]
- 14.Bose P, Regan F, Paterson-Brown S. Improving the accuracy of estimated blood loss at obstetric haemorrhage using clinical reconstructions. BJOG. 2006;113:119–24. doi: 10.1111/j.1471-0528.2006.01018.x. [DOI] [PubMed] [Google Scholar]
- 15.Emami Afshar N, Jafari N, Jalilvand P, Changizi N, Hejazi S, Radpoyan L, et al. [Last accessed on 2014 May 10]. Available from: http://www.sbmu.ac.ir/uploads/Guide_to_Natural_Childbirth.pdf .
- 16.Lee MH, Ingvertsen BT, Kirpensteign J, Jensen AL, Kristensen AT. Quantification of surgical blood loss. Vet Surg. 2006;35:388–93. doi: 10.1111/j.1532-950X.2006.00162.x. [DOI] [PubMed] [Google Scholar]
- 17.Sukprasert M, Choktanasiri W, Ayudhya NI, Promsonthi P, O-Prasertsawat P. Increase accuracy of visual estimation of blood loss from education programme. J Med Assoc Thai. 2006;89:S54–9. [PubMed] [Google Scholar]
- 18.Maslovitz S, Barkai G, Lessing JB, Ziv A, Many A. Improved accuaracy of postpartum blood loss estimation as assessed by simulation. Acta Obstet Gynecol. 2008;87:929–34. doi: 10.1080/00016340802317794. [DOI] [PubMed] [Google Scholar]
- 19.Prata N, Mbaruku G, Campbell M. Using the kanga to measure postpartum blood loss. Int J Gynaecol Obstet. 2005;89:49–50. doi: 10.1016/j.ijgo.2005.01.019. [DOI] [PubMed] [Google Scholar]
- 20.Edhi MM, Aslam HM, Naqvi Z, Hashmi H. Post partum hemorrhage: Causes and management. BMC Res Notes. 2013;6:236. doi: 10.1186/1756-0500-6-236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Al Kadri HM, Al Anazi BK, Tamim HM. Visual estimation versus gravimetric measurement of postpartum blood loss: A prospective cohort study. Arch Gynecol Obstet. 2011;283:1207–13. doi: 10.1007/s00404-010-1522-1. [DOI] [PubMed] [Google Scholar]


