Abstract
Background:
Sexuality is a basic and important factor in human experiences, which varies among different types of cancers. This study was carried out with the aim of defining the relationship between sexual dysfunction and related factors in genital and breast cancers.
Materials and Methods:
This cross-sectional study was conducted on 150 women with genital and breast cancers admitted to two specialized hospitals in Isfahan and by using a two-stage sampling method. Participants completed demographic/disease questionnaire and sexual function questionnaire. Collected data were analyzed by using SPSS software version 14 and statistical tests of correlation coefficient, Student's t-test and one-way analysis of variance (ANOVA).
Results:
The obtained results showed that 47% of women had sexual dysfunction with the mean (SD) age of 47 (7.7) years (with the range of 25–65 years). There was a significant correlation between sexual functioning and age, occupation, educational level, and treatment duration (P < 0.05). There was also a significant correlation between the stage of disease, primary disorder (0.003), and recent disorder (0.028). Meanwhile, Chi-square test showed no significant relationship between cancer type and primary disorder (0.403) and recent disorder (0.416).
Conclusions:
Breast and genital cancers may result in significant difficulties with sexual functioning and sexual life. Addressing these problems is essential to improve the quality of life in women with cancer and further investigations should be conducted for prevention and treatment of disorders by the health authorities.
Keywords: Cancer, factors, sexual functioning, Iran
INTRODUCTION
The concept of sexual dysfunction involves disorder in sexuality and mental–social changes. This disorder affects the sexual response cycle and creates stresses and interpersonal problems including lack of sexual desire, hatred of sex, sexual arousal disorder, and orgasmic disorder.[1] In Iran, according to a national survey conducted in 2005, 31.15% of women had sexual dysfunction.[2] There are a lot of contributing factors on the sexual response, including age, duration, quality of relationship, individual psychological factors with roots in childhood relations with parents, previous failures, methods of coping with emotions, using drugs such as alcohol and unauthorized drugs, disease, and treatment.[1,3,4] Disease could be an important factor in creating sexual problems due to reasons such as body dementia, reduced ability to perform daily activities, hospitalization of the patient, and finally depression.[5] The prevalence of sexual dysfunction is approximately 40% in women, while this rate reaches 80% in women with gynecologic cancer.[6] According to the latest reports, almost 13% of women in the world and 11% of women in the United States of America are affected by different types of gynecologic cancers.[7] Among the most important and influential diseases, cancers can be cited, especially cancers of women. Each of them affects the sexual cycle depending on the organ involved.[8] Genital cancer and its treatment can have a substantial effect on the sexual activities in all phases of the sexual response cycle and the body image.[8,9] Cancer diagnosis and its associated stresses may have a profound effect on the emotional state of the woman and her partner. Therefore, the diagnosis of cancer can have a detrimental effect on sexual activity.[10] On the other hand, after the diagnosis of cancer, women are generally tolerant to the treatment process and, sometimes, surgery.[11] In women with gynecologic and breast cancers, sexual dysfunction can lead to the maximum stress at the time of diagnosis and also throughout the follow-up period.[12,13] Studies have reported that women with progressive cervical, recurrent, or chronic cancers experience problems in connection with the marital relationship.[14,15] Vulvar cancer is rare and happens in women over 60 years of age. Therefore, it is necessary to pay more attention to the impact of vulvar cancer on sexual functioning.[16] Studies conducted on women with ovarian cancer have shown that the items related to sexual activities included young age, not receiving treatment, body image and good confidence.[17,18] In relation with breast cancer, the most important predictors of sexual health include lack of vaginal dryness, having a sense of well-being, positive body image, better quality of relationship, and lack of sexual problems in the partner.[19,20] Studies have shown that there are many key factors for sexual dysfunction, such as types of cancer, type of treatment, personal characteristics, and sexual dysfunction disease.[21,22,23] Considering the importance of sexual matters in maintaining physical–mental health and family and also the issue that sexual health is one of the components of general health, and keeping in mind the impact of sexual problems in the relationship of couples, it seems that despite conducting numerous studies in the field of diagnosis and treatment of sexual disorders, it is necessary to conduct further researches on the underlying problems and sexual disruptions following cancers for providing more detailed information to the health care providers about sexual problems in these cancers. However, it requires strengthening the communication with women about the sexual consequences. It is an essential requirement at the start of diagnosis, throughout the period of treatment, and also in the follow-up period. In addition to the listed items, women's sexual functioning is influenced by various other factors, and this functioning is different in different societies, cultures, values, and religions. Therefore, this study was conducted with the aim of determining the relationship of sexual dysfunction and its associated factors in women with genital and breast cancers, who were admitted to Isfahan specialized cancer hospitals in 2010–2011.
MATERIALS AND METHODS
This research was a cross-sectional study performed on 150 patients with genital and breast cancers, who were admitted to Milad and Sayed-Al-Shohada hospitals in Isfahan. After visiting the desired hospitals, the researchers obtained the patients’ consents and explained the purpose of the study for them. The inclusion criteria were: Married women with genital and breast cancers; passing of a minimum of 1 year after treatment; being under the coverage of Milad and Sayed-Al-Shohada hospitals, admitted for examination, testing, diagnostic and therapeutic procedures; lack of sexual disorders before cancer diagnosis; not using drugs interfering with sexual functioning (such as antihypertensive drugs, antipsychotics, thiazide diuretics, antihistamines, and barbiturates); lack of illnesses interfering with sexual functioning (including multiple sclerosis, Alzheimer's, or any disturbance in the central nervous system); not suffering from severe depression, mental retardation, vasculitis, hypo- or hyperthyroidism, or genital trauma; having no sexual dysfunction before cancer; and patient willing to participate in the study. Then, the questionnaires were completed. Sample size was calculated based on a pilot study conducted on 10 patients with genital and breast cancers by using the correlation coefficient formula (Z value for confidence interval of 95% =1.96, P = 0.5, and D with an accuracy equal to 0.08). Based on the formula  , the sample size was calculated to be at least 150 people. The sampling method was convenient and accessible. Data gathering tools in this study included demographic/disease questionnaire and also sexual dysfunction questionnaire with 44 questions. This questionnaire was adapted from two questionnaires of female sexual function index and sexual function–vaginal changes with the following four categories: Lack of sexual desire, sexual arousal disorder, orgasmic disorders, sexual pain disorders and sexual aversion. This questionnaire assessed sexual dysfunction related to two stages of life (first year of marriage and recent occurrence). In the present study, content validity was used and for determining the scientific validity of the questionnaire, most recent books and articles regarding personal/disease characteristics and sexual dysfunction were studied. Then, they were given to a few experts and professors for evaluation. In order to confirm the scientific reliability of the study, test–retest method was used (with an interval of 2 weeks). Thus, the researcher conducted the test for 10 patients at the beginning of the study and then 1 week later. Reliability of both questionnaires was confirmed with a correlation coefficient of r = 0.86, P= 0.021 (for personal/disease questionnaire) and r = 0.89, P= 0.013 (for sexual dysfunction questionnaire). After collecting the data, statistical tests including Student's t-test, Mann–Whitney, one-way analysis of variance (ANOVA), Chi-square and Pearson correlation coefficient.
, the sample size was calculated to be at least 150 people. The sampling method was convenient and accessible. Data gathering tools in this study included demographic/disease questionnaire and also sexual dysfunction questionnaire with 44 questions. This questionnaire was adapted from two questionnaires of female sexual function index and sexual function–vaginal changes with the following four categories: Lack of sexual desire, sexual arousal disorder, orgasmic disorders, sexual pain disorders and sexual aversion. This questionnaire assessed sexual dysfunction related to two stages of life (first year of marriage and recent occurrence). In the present study, content validity was used and for determining the scientific validity of the questionnaire, most recent books and articles regarding personal/disease characteristics and sexual dysfunction were studied. Then, they were given to a few experts and professors for evaluation. In order to confirm the scientific reliability of the study, test–retest method was used (with an interval of 2 weeks). Thus, the researcher conducted the test for 10 patients at the beginning of the study and then 1 week later. Reliability of both questionnaires was confirmed with a correlation coefficient of r = 0.86, P= 0.021 (for personal/disease questionnaire) and r = 0.89, P= 0.013 (for sexual dysfunction questionnaire). After collecting the data, statistical tests including Student's t-test, Mann–Whitney, one-way analysis of variance (ANOVA), Chi-square and Pearson correlation coefficient.
Ethical considerations
Permission for this study was through the ethics committee of MUI. Other ethical issues in this study involved the assurance of confidentiality and anonymity of the participants. All participants were informed about the purpose and design of this research, and that their participation was voluntary. Participants signed a written informed consent for their participation.
RESULTS
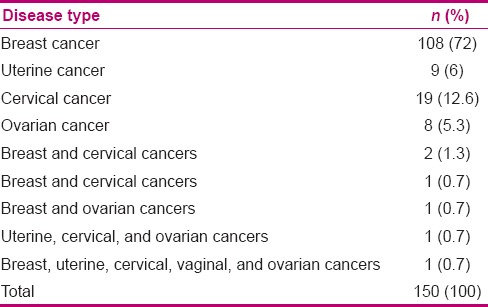
The mean (SD) of some of the demographic characteristics are given in Table 1. Fifty-four (36%) patients had university degrees and 94 (62.7%) subjects were housewives. Frequency distribution of the type of cancer is given in Table 2.
Table 1.
Statistical indicators related to quantitative demographic variables in women with genital and breast cancers
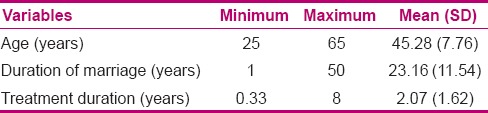
Table 2.
Frequency distribution of subjects depending on the type of cancer
29.3% of patients were in the second stage of disease, 16.7% in the third, 10.7% in the fourth, and 7.3% were in the first stage of disease. In addition, 47.3% were being treated with radiotherapy and chemotherapy, and 31.7% with radiotherapy, chemotherapy, and surgery. McNemar test showed that recent sexual disorder frequency in all areas had been significantly higher than the primary disorder [Table 3].
Table 3.
Frequency distribution of sexual dysfunction in women with genital and breast cancers depending on the type of disorder
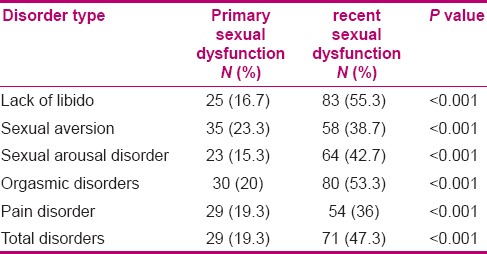
Independent t-test showed that patient age and duration of treatment had a relationship with primary sexual dysfunction. Mann–Whitney test showed that there was a significant relationship between educational level of the patient and primary disorder (P = 0.006) and recent disorder (P = 0.003). Based on Chi-square test, there was a significant relationship between the occupation of the patient and primary disorder (P = 0.03) and recent disorder (P = 0.01). Chi-square test also showed that there was a significant relationship between the stage of the disease and primary disorder (P = 0.003) and recent disorder (P = 0.028). Chi-square test showed that there was no significant relationship between the type of cancer and primary disorder (P = 0.403) and recent disorder (P = 0.416).
DISCUSSION
The results of the present study show that the most primary and recent disorders in sexual functioning were related to the areas of sexual disgust and lack of libido, respectively. The results of Zeighami et al.'s study in Babolsar showed the most common sexual dysfunctions in women with breast cancer were of sexu ality, stimulation, or sexual arousal.[24] In the study of Hendren and colleagues, women with rectal cancer were found to have impaired sexual functioning as follows: 41% decrease in desire, 29% decrease in stimulation, 56% decrease in vaginal lubrication, 35% decrease in orgasm, and 46% decrease in dyspareunia.[25] The differences in the findings of the present study compared to the other mentioned studies might be related to the difference in body areas with cancer. The study results of Schover showed that the most common sexual problems in women with breast cancer are due to loss of interest in sexual activity and dyspareunia. According to Anderson's study, surgical operations due to cancer in female patients (such as hysterectomy, mastectomy, or removal of ovaries) have considerably decreased the sexual desire, decreased the sexual simulate, increased dyspareunia, and cause difficulty in reaching orgasm.[26] Among the other findings of this study, the relationship of sexual dysfunction with age, level of education, occupation, and stage of disease has been mentioned. In line with the results of this study, the results of Chen et al.'s study in Taiwan showed that there was a significant relationship between sexual satisfaction in women and national status, age, duration of treatment, and type of treatment.[27] In addition, women who had been treated throughout the past year had less sexual satisfaction. Binney observed in North Carolina that there was no statistically significant relationship between the sexual functioning of women with breast cancer and the type of treatment (chemotherapy, radiotherapy, and surgery).[28] The study of Ferreira et al. in Brazil on 28 women with vulvar cancer with a mean age of 66 years indicated that only 21% of patients had been sexually active. In addition, the findings showed the relationship of age and women's sexual functioning.[17] Therefore, with increasing age, sexual dysfunction in women also increased, which is consistent with the results of the present study. However, the mean age (45 years) in the present study was much less than in that study. The study results of Sbitti et al. on 125 women with breast cancer in Morocco indicated that there was no statistical relationship between sexual dysfunction and age, level of education, disease stage, and type of treatment.[29] Perhaps, one reason for our results not being in line with the results of the above-mentioned studies is its larger sample size and considering only one type of cancer. In addition, individual, cultural, and racial differences could also be the other possible reasons. According to various studies, Asian women reported more sexual dysfunction compared to women in Western countries.[30,31]
CONCLUSION
Finally, given the high rates of sexual dysfunction in genital and breast cancers, and its relevance with some demographic variables and disease in these patients in this study, it is necessary to focus on performing reviews and preventing and treating this disorder by health care providers to solve these problems. According to the obtained results from this study, awareness about sexual functioning and related factors in women with cancer can help the health professionals to identify appropriate care for improving marital relationships, problems, and specific needs. Therefore, understanding and awareness in the context of changes in sexual dysfunction is necessary and important in the diagnosis and treatment of patients with cancer.
ACKNOWLEDGMENTS
This study is extracted from a proposal approved in 2010 (research number 289237) at Isfahan University of Medical Sciences (in Iran), which is sponsored by the research deputy. We greatly appreciate the support of nursing and midwifery care research center in Isfahan University of Medical Sciences and the cooperation of the authorities of the selected hospitals and all the participating women.
Footnotes
Source of Support: Isfahan University of Medical Sciences.
Conflict of Interest: None declared.
REFERENCES
- 1.Pinto AC. Sexuality and breast cancer: Prime time for young patients. J Thorac Dis. 2013;5(Suppl 1):S8–61. doi: 10.3978/j.issn.2072-1439.2013.05.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hopkinson JB, Fenlon DR, Okamoto I, Wright DN, Scott I, Addington-Hall JM, et al. The deliverability, acceptability, and perceived effect of the Macmillan approach to weight loss and eating difficulties: A phase II, cluster-randomized, exploratory trial of a psychosocial intervention for weight-and eating-related distress in people with advanced cancer. J Pain Symptom Manage. 2010;40:684–95. doi: 10.1016/j.jpainsymman.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 3.Ismail KM. Psychological challenges in obstetrics and gynecology. Obstet Gynaecol. 2008;10:206. [Google Scholar]
- 4.Anderson JL. Acknowledging Female Sexual Dysfunction in women with Cancer. Clin J Oncol Nurs. 2013;17:233–5. doi: 10.1188/13.CJON.233-235. [DOI] [PubMed] [Google Scholar]
- 5.Rodin G, Olmsted MP, Rydall AC, Maharaj SI, Colton PA, Jones JM, et al. Eating disorders in young women with type 1 diabetes mellitus. J Psychosom Res. 2002;53:943–9. doi: 10.1016/s0022-3999(02)00305-7. [DOI] [PubMed] [Google Scholar]
- 6.Matulonis U, Kornblith A, Lee H, Bryan J, Gibson C, Wells C, et al. Long-term adjustment of early-stage ovarian cancer survivors. Int J Gynecol Cancer. 2008;18:1183–93. doi: 10.1111/j.1525-1438.2007.01167.x. [DOI] [PubMed] [Google Scholar]
- 7.Jemal A, Siegel R, Xu J, Ward E. Cancer statistics. CA Cancer J Clin. 2010;60:277–300. doi: 10.3322/caac.20073. [DOI] [PubMed] [Google Scholar]
- 8.Carter J, Huang H, Chase DM, Walker JL, Cella D, Wenzel L. Sexual function of patients with endometrial cancer enrolled in the Gynecologic Oncology Group LAP2 Study. Int J Gynecol Cancer. 2012;22:1624–33. doi: 10.1097/IGC.0b013e31827277fa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Collins JJ, Baase CM, Sharda CE, Ozminkowski RJ, Nicholson S, Billotti GM, et al. The assessment of chronic health conditions on work performance, absence, and total economic impact for employers. J Occup Environ Med. 2005;47:547–57. doi: 10.1097/01.jom.0000166864.58664.29. [DOI] [PubMed] [Google Scholar]
- 10.Goedhard RG, Goedhard WJ, editors. Elsevier: International Congress Series; 2005. Work ability and perceived work stress. [Google Scholar]
- 11.Plotti F, Nelaj E, Sansone M, Antonelli E, Altavilla T, Angioli R, et al. Sexual Function after Modified Radical Hysterectomy (Piver II/Type B) vs. Classic Radical Hysterectomy (Piver III/Type C2) for Early Stage Cervical Cancer. A Prospective Study. J Sex Med. 2012;9:909–17. doi: 10.1111/j.1743-6109.2011.02581.x. [DOI] [PubMed] [Google Scholar]
- 12.Emilee G, Ussher J, Perz J. Sexuality after breast cancer: A review. Maturitas. 2010;66:397–407. doi: 10.1016/j.maturitas.2010.03.027. [DOI] [PubMed] [Google Scholar]
- 13.Sbitti Y, Kadiri H, Essaidi I, Fadoukhair Z, Kharmoun S, Slimani K, et al. Breast cancer treatment and sexual dysfunction: Moroccan women's perception. BMC Women's Health. 2011;11:29. doi: 10.1186/1472-6874-11-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brotto LA, Yule M, Breckon E. Psychological interventions for the sexual sequelae of cancer: A review of the literature. J Cancer Surviv. 2010;4:346–60. doi: 10.1007/s11764-010-0132-z. [DOI] [PubMed] [Google Scholar]
- 15.Frumovitz M, Sun CC, Schover LR, Munsell MF, Jhingran A, Wharton JT, et al. Quality of life and sexual functioning in cervical cancer survivors. J Clin Oncol. 2005;23:7428–36. doi: 10.1200/JCO.2004.00.3996. [DOI] [PubMed] [Google Scholar]
- 16.Bergmark K, ÅVall-Lundqvist E, Dickman PW, Henningsohn L, Steineck G. Patient-rating of distressful symptoms after treatment for early cervical cancer. Acta Obstet Gynecol Scand. 2002;81:443–50. doi: 10.1034/j.1600-0412.2002.810512.x. [DOI] [PubMed] [Google Scholar]
- 17.de Melo Ferreira AP, de Figueiredo EM, Lima RA, Cândido EB, de Castro Monteiro MV, de Figueiredo Franco TM, et al. Quality of life in women with vulvar cancer submitted to surgical treatment: A comparative study. Eur J Obstet Gynecol Reprod Biol. 2012;165:91–5. doi: 10.1016/j.ejogrb.2012.06.027. [DOI] [PubMed] [Google Scholar]
- 18.Gershenson DM, Miller AM, Champion VL, Monahan PO, Zhao Q, Cella D, et al. Reproductive and sexual function after platinum-based chemotherapy in long-term ovarian germ cell tumor survivors: A Gynecologic Oncology Group Study. J Clin Oncol. 2007;25:2792–7. doi: 10.1200/JCO.2006.08.4590. [DOI] [PubMed] [Google Scholar]
- 19.Panjari M, Bell RJ, Davis SR. Sexual function after breast cancer. J Sex Med. 2011;8:294–302. doi: 10.1111/j.1743-6109.2010.02034.x. [DOI] [PubMed] [Google Scholar]
- 20.Forgione A, Leroy J, Cahill RA, Bailey C, Simone M, Mutter D, et al. Prospective evaluation of functional outcome after laparoscopic sigmoid colectomy. Ann Surg. 2009;249:218–24. doi: 10.1097/SLA.0b013e318195c5fc. [DOI] [PubMed] [Google Scholar]
- 21.Brotto LA, Erskine Y, Carey M, Ehlen T, Finlayson S, Heywood M, et al. A brief mindfulness-based cognitive behavioral intervention improves sexual functioning versus wait-list control in women treated for gynecologic cancer. Gynecol Oncol. 2012;125:320–5. doi: 10.1016/j.ygyno.2012.01.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Akkuzu G, Ayhan A. Sexual Functions of Turkish Women with Gynecologic Cancer during the Chemotherapy Process. Asian Pac J Cancer Prev. 2013;14:3561–4. doi: 10.7314/apjcp.2013.14.6.3561. [DOI] [PubMed] [Google Scholar]
- 23.Olsson C, Athlin E, Sandin-Bojö AK, Larsson M. Sexuality is not a priority when disease and treatment side effects are severe: Conceptions of patients with malignant blood diseases. J Clin Nurs. 2013;22:3503–12. doi: 10.1111/jocn.12333. [DOI] [PubMed] [Google Scholar]
- 24.Zeighami Mohammadi S, Fatemeh G. Sexual Dysfunction and Its Correlation with Quality of Life among Women Affected with Cancer. Iranian J Obstet Gynecol Infertil. 2009;12:39–46. [Google Scholar]
- 25.Hendren SK, O’Connor BI, Liu M, Asano T, Cohen Z, Swallow CJ, et al. Prevalence of male and female sexual dysfunction is high following surgery for rectal cancer. Ann Surg. 2005;242:212. doi: 10.1097/01.sla.0000171299.43954.ce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schover LR. Sexuality and body image in younger women with breast cancer. J Natl Cancer Inst Monogr. 1994;16:177–82. [PubMed] [Google Scholar]
- 27.Chen C, Huang K, Wan G, Tu L, Lee J. Sexual satisfaction and related factors in women previously treated for gynecological cancer. Hu liza zhi J Nurs. 2013;60:61–70. doi: 10.6224/JN.60.2.61. [DOI] [PubMed] [Google Scholar]
- 28.Binney GL. Sexual Satisfaction Among Young Breast Cancer Survivors. 2011 [Google Scholar]
- 29.Sbitti Y, Kadiri H, Essaidi I, Fadoukhair Z, Kharmoun S, Slimani K. Breast cancer treatment and sexual dysfunction: Moroccan women's perception. BMC Womens Health. 2011;11:2–5. doi: 10.1186/1472-6874-11-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Laumann EO, Nicolosi A, Glasser DB, Paik A, Gingell C, Moreira E, et al. Sexual problems among women and men aged 40–80 y: Prevalence and correlates identified in the Global Study of Sexual Attitudes and Behaviors. Int J Impot Res. 2004;17:39–57. doi: 10.1038/sj.ijir.3901250. [DOI] [PubMed] [Google Scholar]
- 31.Moreira E, Brock G, Glasser D, Nicolosi A, Laumann E, Paik A, et al. Help-seeking behavior for sexual problems: The Global Study of Sexual Attitudes and Behaviors. Int J Clin Pract. 2005;59:6–16. doi: 10.1111/j.1742-1241.2005.00382.x. [DOI] [PubMed] [Google Scholar]


