Abstract
Setting: The Black Lion Referral Hospital, Addis Ababa, Ethiopia.
Objective: To document indications for admission, complications and outcomes of patients with diabetes mellitus (DM) admitted between 2010 and 2013.
Design: A descriptive retrospective study using medical files.
Results: Of 8048 admissions, 523 (6.5%) had DM; of these, 418 medical records were retrieved: 301 (72%) patients had type 2 and 104 (28%) type 1 disease, with male sex (62%) and older age (median age 60 years) being features of type 2 disease. Main admission diagnoses for type 2 disease were diabetic foot ulcer (39%) and cardiovascular disease (21%); for type 1 disease, it was diabetic ketoacidosis (62%). Hypertension, neuropathy, nephropathy, retinopathy and diabetic foot accounted for 85% of the 756 existing complications. Overall in-patient mortality was 21%. Of the 89 deaths, 77 occurred among patients with type 2 disease; the main indications for admission were diabetic foot ulcer/gangrene and cardiovascular disease.
Conclusion: DM, especially type 2 DM, is an important cause of admission to Ethiopia’s largest referral hospital. Many patients had already developed disease-related complications at admission, and mortality was high. There is a need to improve awareness about and care for DM in Ethiopia.
Keywords: diabetes mellitus, Ethiopia, mortality, operational research, SORT IT
Abstract
Contexte : Hôpital de référence du Black Lion, Addis Ababa, Ethiopie.
Objectif : Documenter les indications d’admission, les complications et le devenir des patients atteints de diabète (DM) admis à l’hôpital entre 2010 et 2013.
Schéma : Etude descriptive rétrospective sur dossiers médicaux.
Résultats : Sur 8048 admissions, 523 (6,5%) avaient un DM et parmi eux, 418 dossiers médicaux ont été retrouvés : 301 (72%) patients avaient un DM de type 2 et 104 (28%) avaient un DM de type 1 ; les hommes (62%) et les personnes âgées (âge médian 60 ans) étaient caractéristiques du type 2. Les diagnostics d’admission les plus fréquents du type 2 étaient l’ulcère diabétique du pied (39%) et les problèmes cardiovasculaires (21%), et celui du type 1, l’acidocétose diabétique (62%). L’hypertension, les neuropathies, les néphropathies, la rétinopathie et le pied diabétique représentaient 85% des 756 complications existantes. La mortalité totale des patients admis a été de 21%. Sur ces 89 décès, 77 patients étaient de type 2 avec comme indications principales d’admission l’ulcère diabétique du pied/la gangrène et les problèmes cardiovasculaires.
Conclusion : Le DM, surtout de type 2, est une cause importante d’admission dans le plus grand hôpital de référence du pays. De nombreux patients avaient déjà développé des complications liées au DM lors de l’admission, et la mortalité a été élevée. Il est nécessaire d’améliorer la connaissance et les soins relatifs au DM en Ethiopie.
Abstract
Marco de referencia: El hospital de referencia Black Lion de Addis Abeba en Etiopía.
Objetivo: Documentar las indicaciones de hospitalización, las complicaciones y los desenlaces clínicos de los pacientes con diabetes (DM) hospitalizados entre el 2010 y el 2013.
Métodos: Fue este un estudio descriptivo retrospectivo realizado a partir de las historias clínicas.
Resultados: En las 8048 hospitalizaciones hubo 523 casos de DM (6,5%); se consultaron 418 historias clínicas. En 301 pacientes el diagnóstico fue DM de tipo 2 (72%) y en 104 casos fue DM de tipo 1 (28%); los pacientes con DM de tipo 2 eran predominantemente de sexo masculino (62%) y de edad avanzada (mediana de la edad 60 años). El principal motivo de hospitalización en el grupo de DM de tipo 2 fue la úlcera diabética del pie (39%) y la enfermedad cardiovascular (21%) y en el grupo con DM de tipo 1 fue el estado de cetoacidosis (62%). De las 756 complicaciones existentes, el 85% consistieron en hipertensión neuropatía, retinopatía y pie diabético. La mortalidad intrahospitalaria global fue 21%; de las 89 defunciones, 77 correspondieron a pacientes con DM de tipo 2, hospitalizados por pie diabético o gangrena y enfermedad cardiovascular.
Conclusión: La DM de tipo 2 representa una causa importante de hospitalización en el principal hospital de referencia del país. Muchos pacientes presentaban complicaciones relacionadas con la enfermedad en el momento de la hospitalización y la mortalidad fue alta. Es necesario consolidar la sensibilización con respecto a la DM y a la atención de estos pacientes en Etiopía.
Chronic non-communicable diseases have emerged as the next twenty-first century global epidemic and have already become the leading causes of death and disability worldwide.1 Among these, the global burden of diabetes mellitus (DM) is immense. In 2013, an estimated 382 million people were living globally with DM, with numbers expected to rise to 592 million by 2030.2 Most of these persons have type 2 DM, and given the association between DM and unhealthy lifestyles, such as poor diet and physical inactivity, there are more people with DM in urban than in rural areas; this divide is estimated to reach 314 million and 143 million, respectively, in 2030. In 2013, DM-related complications were a major cause of disability and reduced quality of life, and an estimated 5 million people aged 20–79 years worldwide died prematurely from the disease.2
Although Asia is the epicentre of the DM pandemic, there is an increasing burden of disease in sub-Saharan African countries.3 A systematic review of studies in Ethiopia from 1970 to 2011 suggested that DM prevalence in the country was about 2%, rising to >5% in persons aged ⩾40 years in certain settings.4 A more recent nationwide World Health Organization (WHO) STEPS survey among 2153 persons in Ethiopia found the DM prevalence to be 6.5%.5 It is therefore important to monitor and anticipate the growing burden of DM and related complications, together with treatment outcomes, for the purpose of resource planning (i.e., the human and material resources needed to diagnose, treat and manage this disease) and to inform future control and management strategies.
A previous study in two specialised hospitals in Addis Ababa documented the trend in DM admissions between 2005 and 2009, noting that admissions increased from 51 per annum to 245 over this period.6 Up-to-date information on the indications for hospital admission, the types of DM, existing complications and hospital outcomes is important, as this will help policy makers and health care staff better understand the DM burden and associated comorbidities. In Ethiopia, where there are no community-level studies on the burden of DM, hospital data serve as a useful proxy.
The aim of the present study was therefore to document indications for admission, complications and hospital outcomes of patients with DM admitted to the largest referral hospital (in Addis Ababa, Ethiopia), and compare findings between patients with type 1 and type 2 DM. Specific objectives for patients stratified by type of DM were to describe 1) demographic characteristics and indications for hospital admission, 2) existing complications and comorbidities, and 3) hospital outcomes.
METHODS
Study design
This was a retrospective descriptive study using medical files.
Setting
General setting
Ethiopia, located in the Horn of Africa, is the third most populated country in sub-Saharan Africa, with 80 million inhabitants, of whom >80% live in rural areas. The country has around 80 different ethnic groups. Addis Ababa is the capital city of Ethiopia, with a population of over 3 million, according to the 2007 population census, and an annual estimated growth rate of 3.8%.7 The country is poor, with a gross national income per capita of US$1110 in 2012.8 Infectious and communicable diseases account for about 60–80% of the health problems in the country, although non-communicable diseases are thought to be rapidly increasing.9
Study site
The Black Lion Hospital (Tikur Anbessa in Amharic) is Ethiopia’s largest specialised and referral public hospital. In 1998, the hospital was handed over to Addis Ababa University by the Ministry of Health so that it could also function as a teaching hospital. The hospital has more than 800 beds and offers diagnosis and treatment for approximately 400 000 in-patients and out-patients a year. The hospital receives patients who are referred from across the country, as well as spatients from Addis Ababa.
DM management
Patients with DM are mainly classified as type 1 and type 2, with specific forms of DM and gestational diabetes making up the remainder. Type 1 DM is managed with insulin, while type 2 is managed by lifestyle and dietary advice, oral medications (mainly sulphonylureas and metformin) and short-, medium- and long-acting insulin. Patients are usually managed on an out-patient basis in a specialised diabetes clinic, but are admitted if they develop acute (hypoglycaemia or ketoacidosis) or more chronic complications (cardiovascular disease, stroke, foot disease).
Patient population
All patients with DM (previously known or diagnosed on the current admission) who were admitted to the wards of the Department of Internal Medicine at the Black Lion Hospital, between January 2010 and December 2013 were included in the study.
Data variables, data collection and sources of data
Data variables collected in relation to the study objectives included the number of medical admissions each year and the number with a hospital in-patient admission diagnosis of DM collected from the hospital health information system logbooks; age; sex; residence; type of DM; indications for hospital admission; existing complications and hospital discharge outcomes collected from patient medical charts. A data abstraction sheet was prepared into which the relevant data were entered. The data were collected in August 2014 by identifying the medical record number from the Health Management Information System log book, which was then used to trace and access individual patient medical charts. The principal investigator led the abstraction process, aided by local co-investigators.
Analysis and statistics
Data were single-entered from the paper-based abstraction sheet into an electronic EpiData file (version 3.1, EpiData Association, Odense, Denmark). A descriptive analysis with frequencies and proportions was carried out. Baseline characteristics and hospital outcomes were compared between patients with type 1 and type 2 DM using the χ2 test, with levels of significance set at 5%.
Ethics
Permission for the study was obtained from the Research and Ethics Committee of the School of Public Health and the Department of Internal Medicine, School of Medicine, Addis Ababa University. The study met the Médecins Sans Frontières (MSF) Ethics Review Board (Geneva, Switzerland) approved criteria for studies of routinely collected data, and was approved by the Ethics Advisory Group of the International Union Against Tuberculosis and Lung Disease, Paris, France. Names were not used in collecting the data from the medical files, and confidentiality was maintained by keeping the data collection forms locked in a secure cabinet; the electronic data file was kept securely in a password protected computer.
RESULTS
Between 2010 and 2013, there were 8048 hospital admissions to the Department of Internal Medicine, of which 523 (6.5%) were recorded as DM. The numbers and proportions of patients admitted with DM each year are as follows: 138 (8%) in 2010, 118 (7%) in 2011, 159 (7%) in 2012 and 108 (4%) in 2013.
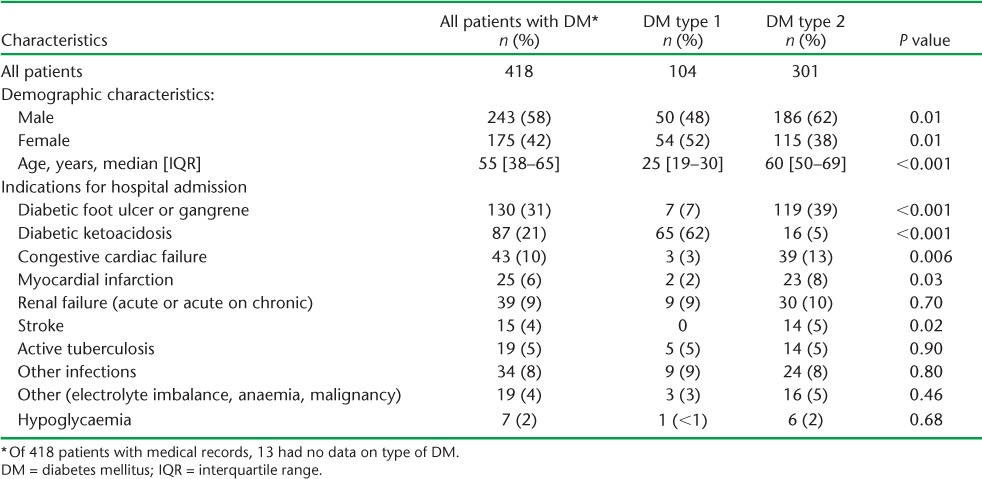
Of the 523 logbook entries, 418 medical records were retrieved: 50 records were from patients who did not in fact have DM, and 55 records could not be found. Of the patients with medical records, 306 (73%) lived in Addis Ababa; the remainder had been referred. Demographic characteristics and indications for hospital admission for all patients and for those with type 1 and type 2 DM are shown in Table 1. Type 2 DM accounted for nearly three quarters of all admissions; this group had a higher proportion of males and a higher median age (60 years) than the group with type 1 DM. Nearly one third of the patients were admitted with diabetic foot ulcer/gangrene, about 20% with diabetic ketoacidosis or cardiovascular disease/stroke and nearly 10% with renal failure. Infections were responsible for 13% of admissions, with active tuberculosis (TB) accounting for 5% of these. In those with type 2 DM there was a significantly higher burden of diabetic foot ulcer, congestive cardiac failure, myocardial infarction and stroke, and a significantly lower frequency of diabetic ketoacidiosis compared with the group with type 1 DM.
TABLE 1.
Demographic characteristics and indications for hospital admission in patients with DM admitted to the Black Lion Hospital, Addis Ababa, Ethiopia, 2010–2013
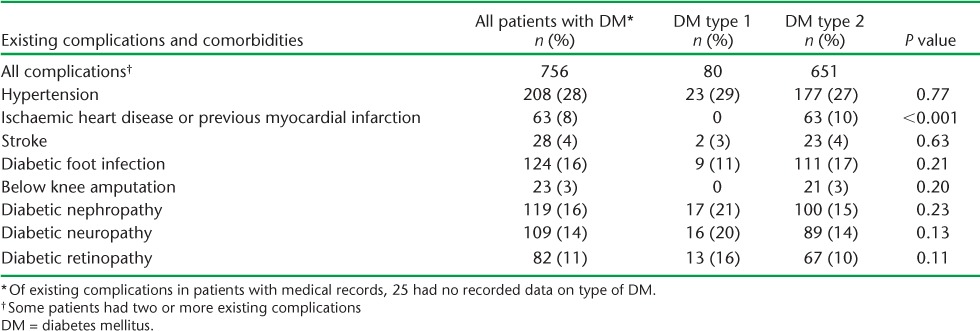
A large number of patients had existing complications (Table 2). Hypertension, chronic complications of DM such as neuropathy, nephropathy and retinopathy, and previous diabetic foot infections accounted for 85% of these. The only significant difference between patients with type 1 and those with type 2 DM was that the existing complication of ischaemic heart disease and/or previous myocardial infarction was only observed in those with type 2 DM.
TABLE 2.
Existing complications and comorbidities in patients with diabetes admitted to the Black Lion Hospital, Addis Ababa, Ethiopia, stratified by type 1 and type 2 DM, 2010–2013
The median period of hospitalisation for all patients was 12 days (interquartile range [IQR] 6–23); for those with type 1 DM it was 8 days (IQR 5–16) and for type 2 DM it was 14 days (IQR 7–25). Hospital outcomes for all patients and for those with type 1 DM and type 2 DM are shown in Table 3. The in-hospital mortality rate among all DM patients was high (21%), and 26% more common for type 2 DM patients than in those with type 1 DM. In patients who died, the indications for hospital admission in relation to type of DM are shown in Table 4. Although there were no significant differences due to the small numbers, diabetic foot ulcer/gangrene, cardiovascular disease, stroke and renal disease were the most common reasons for admission among those with type 2 DM. A significant difference in mortality was found in those with diabetic ketoacidosis due to type 1 DM compared to type 2 DM.
TABLE 3.
Hospital outcomes among patients with diabetes admitted to the Black Lion Hospital, Addis Ababa, Ethiopia, stratified by type 1 and type 2 DM, 2010–2013
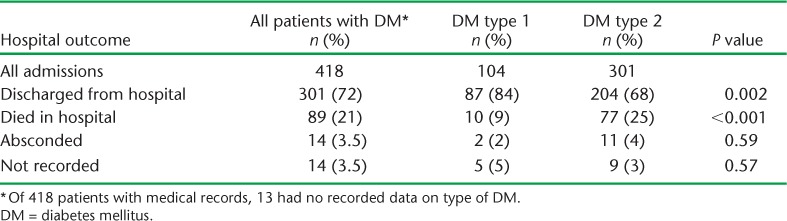
TABLE 4.
Indications for admission in patients with type 1 and type 2 DM who died in the Black Lion Hospital, Addis Ababa, Ethiopia, 2010–2013

DISCUSSION
This study shows that patients with DM constituted >5% of all medical admissions to the largest referral hospital in Ethiopia, with the disease burden remaining roughly the same between 2010 and 2013. The majority had type 2 DM; patients were generally male, with a median age of 60 years. In this group, diabetic foot ulcer and non-communicable disease constituted the most common reasons for hospital admission. About one quarter of the patients with type 1 DM were young, and ketoacidosis was the most common cause of admission in this group. The proportion of patients admitted with type 1 DM was higher than normally observed in other African settings; this may be related to malnutrition-related disease, which is known to be common in Ethiopia.10 The prevalence of infection and active TB was similar for both types of DM, with TB being the cause of hospital admission in one in 20 patients. Recent systematic reviews have found that DM patients are two to three times more likely to develop TB than others,11,12 and the last few years have seen a global increase in this dual disease burden.13
The majority of patients admitted with DM already had existing complications and comorbidities requiring ongoing care both in hospital and in the community once the patent has been discharged. The existing complications, added to the indications for hospital admission, were probably responsible for the high in-hospital mortality observed overall, and particularly those with type 2 DM, in whom diabetic foot ulcer and cardiovascular disease were the main admission indications that eventually lead to death.
The strengths of this study were that it included all DM patients admitted to this large referral hospital during a 4-year period, and there was no need for any sampling framework. The study report also followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.14 Limitations included the operational nature of the study and the use of data already collected from patient files, which might have been inaccurate. Moreover, in nearly 10% of the patients registered as having DM in the health information log books, this information was incorrect, and in another 10% the patients’ medical charts could not be found.
The findings of this study support the belief that DM is a large and growing global public health problem, especially in low- and middle-income countries and in sub-Saharan Africa.2,15 The main indication for admission was diabetic foot ulcer/gangrene, especially in patients with type 2 DM, in line with other reports in Africa.16 Although we have no evidence, this may be related to poor glycaemic control prior to hospital admission, which in turn may be related to difficult access to medication or poor adherence to medication guidance, as has been observed elsewhere in Ethiopia.17 The proportion of patients who died in this study was higher than reported previously.6 However, high rates of hospital mortality have been associated elsewhere with diabetic foot ulcer and cardiovascular disease,18,19 and these were the most common indications for hospital admission in the present study. Associated hypertension is also known to increase the risk of cardiovascular disease and mortality.18
There are several implications of our study. First, better awareness about and community mobilisation for the prevention and care of DM is needed in the community and among health care staff, and this includes health decision makers who need to consider capacity development and appropriate resources. This in turn can be supported by early screening of people attending health facilities, including those over a certain age, such as 40–50 years, those at risk of non-communicable diseases and pregnant women, as in other countries.20 Second, discussion and advocacy for free medication is needed for those living in low- and middle-income countries to support what is in effect life-long treatment. Third, special attention should be given to those who are admitted with diabetic foot ulcer or cardiovascular complications, as these are leading causes of death; good blood pressure control should also be emphasised. The high rates of in-hospital mortality need to be reduced, and earlier detection and better case management of those at risk of death may contribute to this reduction. Fourth, as DM patients are two to three times more likely to develop TB than other patients,11,12 consideration should be given to routine screening of DM admissions for symptoms and signs of TB. Evidence suggests that it is worthwhile screening persons with DM for TB in countries such as Ethiopia, where TB case notification rates exceed 100 per 100 000 population. This approach has also been endorsed by WHO and the International Union Against Tuberculosis and Lung Disease.21,22 Finally, the hospital needs to improve on its health information systems and storage of medical records.
In conclusion, DM constituted an important cause of admission to the medical wards of the largest referral hospital in Ethiopia. Type 2 DM predominated, with diabetic foot ulcer and associated non-communicable diseases being important causes of existing comorbidity and admission. These in turn were associated with high in-patient mortality. There is a need to improve awareness and care in the management of DM in Ethiopia.
Acknowledgments
This research was conducted through the Structured Operational Research and Training Initiative (SORT IT), a global partnership led by the Special Programme for Research and Training in Tropical Diseases at the World Health Organization (WHO/TDR, Geneva, Switzerland). The model is based on a course developed jointly by the International Union Against Tuberculosis and Lung Disease (The Union, Paris, France) and Medécins Sans Frontières (MSF, Brussels Operational Centre, Luxembourg). The specific SORT IT programme which resulted in this publication was jointly developed and implemented by: the Operational Research Unit (LUXOR), MSF Brussels Operational Center; the Centre for Operational Research, The Union; the Centre for International health, University of Bergen, Bergen, Norway; the Institute of Tropical Medicine, Antwerp, Belgium; The University of Nairobi, Nairobi, Kenya and the University of Chester, Chester, United Kingdom. The programme was funded by The Union, MSF, the Department for International Development (DFID, London, UK) and WHO. We also thank the School of Public Health, Addis Ababa University, Addis Ababa, Ethiopia, for financial support. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
In accordance with WHO’s open-access publication policy for all work funded by WHO or authored/co-authored by WHO staff members, the WHO retains the copyright of this publication through a Creative Commons Attribution intergovernmental organisation licence (http://creativecommons.org/licenses/by/3.0/igo/legalcode) which permits unrestricted use, distribution and reproduction in any medium provided the original work is properly cited.
Footnotes
Conflict of interest: none declared.
References
- 1.Lozano R M, Naghavi M, Foreman K et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study. Lancet. 2012;380:2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.International Diabetes Federation. IDF Diabetes Atlas. 6th ed. Brussels, Belgium: IDF; 2013. http://www.idf.org/diabetesatlas Accessed January 2015. [Google Scholar]
- 3.Mbanya J C, Motala A A, Sobngwi E, Assah F K, Enoru S T. Diabetes in sub-Saharan Africa. Lancet. 2010;375:2254–2266. doi: 10.1016/S0140-6736(10)60550-8. [DOI] [PubMed] [Google Scholar]
- 4.Nigatu T. Epidemiology, complications and management of diabetes in Ethiopia: a systematic review. J Diabetes. 2012;4:174–180. doi: 10.1111/j.1753-0407.2011.00181.x. [DOI] [PubMed] [Google Scholar]
- 5.Nshisso L D, Reese A, Gelaye B, Lemma S, Berhane Y, Williams M A. Prevalence of hypertension and diabetes among Ethiopian adults. Diabetes Metab Syndr. 2012;6:36–41. doi: 10.1016/j.dsx.2012.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adem A, Demis T, Seleke Y. Trend of diabetic admissions in TikurAnbessa and St Paul’s University Teaching Hospital from January 2005 to December 2009, Addis Ababa, Ethiopia. Ethiop Med J. 2011;49:231–238. [PubMed] [Google Scholar]
- 7.Central Statistical Authority. 2007 Population and Housing Census of Ethiopia: Administrative Report 2012. Addis Ababa, Ethiopia: CSA; 2007. http://www.csa.gov.et Accessed January 2015. [Google Scholar]
- 8.World Health Organization. World health statistics, 2014. Geneva, Switzerland: WHO; 2014. [Google Scholar]
- 9.Federal Ministry of Health. Health and health-related indicators: 2008/2009. Addis Ababa, Ethiopia: FMoH; 2010. [Google Scholar]
- 10.Gill G, English P, Price C, Dedicoat M, Tesfaye S. The variable African diabetic phenotype: tales from the north and the south. African J Diab Med. 2010;18:12–14. [Google Scholar]
- 11.Stevenson C R, Critchley J A, Forouhi N G et al. Diabetes and the risk of tuberculosis: a neglected threat to public health. Chronic Illness. 2007;3:228–245. doi: 10.1177/1742395307081502. [DOI] [PubMed] [Google Scholar]
- 12.Jeon C Y, Murray M B. Diabetes mellitus increases the risk of active tuberculosis: a systematic review of 13 observational studies. PLOS MED. 2008;5:e152. doi: 10.1371/journal.pmed.0050152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lönnroth K, Roglic R, Harries A D. Improving tuberculosis prevention and care through addressing the global diabetes epidemic: from evidence to policy and practice. Lancet Diabetes Endocrinol. 2014;2:730–739. doi: 10.1016/S2213-8587(14)70109-3. [DOI] [PubMed] [Google Scholar]
- 14.Von Elm E, Altman D G, Egger M. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Bull World Health Organ. 2007;85:867–872. doi: 10.2471/BLT.07.045120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization. Diabetes. Geneva, Switzerland: WHO; 2015. http://www.who.int/topics/diabetes_mellitus/fr/ Accessed January 2015. [Google Scholar]
- 16.Ajayi E A, Ajayi A O. Pattern and outcome of diabetic admissions at a federal medical center: a 5-year review. Ann Afr Med. 2009;8:271–275. doi: 10.4103/1596-3519.59584. [DOI] [PubMed] [Google Scholar]
- 17.Solomon M, Yemane B, Alemayehu W. Barriers to diabetes medication adherence in North West Ethiopia. Springerplus. 2014;3:195. doi: 10.1186/2193-1801-3-195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ryden L, Grant P J, Anker S D et al. ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: the Task Force on diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and developed in collaboration with the European Association for the Study of Diabetes (EASD) Eur Heart J. 2013;34:3035–3087. doi: 10.1093/eurheartj/eht108. [DOI] [PubMed] [Google Scholar]
- 19.Martins-Mendes D, Monteiro-Soares M, Boyko E J et al. Independent contribution of diabetic foot ulcer on lower extremity amputation and mortality risk. J Diabetes Complications. 2014;28:632–638. doi: 10.1016/j.jdiacomp.2014.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Khader A, Farajallah L, Shahin Y et al. Cohort monitoring of persons with diabetes mellitus in a primary health care clinic for Palestine refugees in Jordan. Trop Med Int Health. 2012;17:1108–1116. doi: 10.1111/j.1365-3156.2012.03097.x. [DOI] [PubMed] [Google Scholar]
- 21.Jeon C Y, Harries A D, Baker M A et al. Bi-directional screening for tuberculosis and diabetes: a systematic review. Trop Med Int Health. 2010;15:1300–1314. doi: 10.1111/j.1365-3156.2010.02632.x. [DOI] [PubMed] [Google Scholar]
- 22.World Health Organization & The International Union Against Tuberculosis and Lung Disease. Collaborative framework for care and control of tuberculosis and diabetes. Geneva, Switzerland: WHO; 2011. WHO/HTM/TB/2011.15. [PubMed] [Google Scholar]


