Abstract
Data from surveys on knowledge, attitudes and practice (KAP) on tuberculosis (TB) conducted under the Axshya project at two time points (baseline 2010–2011 and mid-line 2012–2013) were analysed for changes in coverage and equity of TB awareness after project interventions. Overall coverage increased from 84% at baseline to 88% at midline (5% increase, P < 0.05). In comparison to baseline results, coverage at the midline survey had significantly increased, from 81% to 87% among the rural population, from 81% to 86% among women, from 73% to 85% in the ⩾55 years age group, from 71% to 80% among illiterates and from 73% to 81% in the south zone (P < 0.05). The equity gap among the different study groups (settlement, sex, age, education and zones) decreased from 6–23% at baseline to 3–11% during the midline survey. The maximum decline was observed for type of settlement (rural vs. urban), from 10% to 3% (P < 0.05). This community-driven TB control project has achieved high and equitable coverage of TB awareness, offering valuable lessons for the global community.
Keywords: KAP surveys, ACSM, assessment, general population
Abstract
Des données émanant d’enquêtes « connaissances, attitudes, pratiques » (KAP) en matière de tuberculose (TB) réalisées dans le cadre du projet « Axshya » à deux périodes (de 2010 à 2011 au départ et de 2012 à 2013 à mi-parcours) ont été analysées à la recherche de modifications dans la couverture et l’équité en matière de connaissances de la TB à la suite des interventions du projet. La couverture d’ensemble a augmenté de 84% au départ à 88% à mi-parcours (augmentation de 5% ; P < 0,05). En comparaison au point de départ, la couverture de l’enquête à mi-parcours a augmenté significativement de 81% à 87% dans la population rurale, de 81% à 86% chez les femmes, de 73% à 85% dans la tranche d’âge ⩾55 ans, de 71% à 80% chez les personnes illettrées et de 73% à 81% dans la zone sud (P < 0,05). La différence en termes d’équité parmi les divers groupes d’étude (lieu, sexe, âge, instruction et zones) a diminué de 6% à 23% au départ jusqu’à 3% à 11% lors de l’enquête à mi-parcours. Le déclin maximal a été observé pour la localisation (rurale contre urbaine), de 10% à 3% (P < 0,05). Le projet à base communautaire de lutte contre la TB a abouti à une couverture élevée et équitable des connaissances en matière de TB, ce qui offre des leçons à portée universelle.
Abstract
Se llevó a cabo un análisis de la evolución de la cobertura y la equidad en la sensibilización a la tuberculosis (TB) después de las intervenciones realizadas en el marco del Proyecto Axshya, a partir de los resultados de las encuestas del proyecto sobre los conocimientos, las actitudes y las prácticas en materia de TB que se realizaron al comienzo entre el 2010 y el 2011 y a medio término de la intervención, del 2012 al 2013. La cobertura global aumentó de 84% al comienzo del proyecto a 88% a medio término (aumento de un 5% ; P < 0,05). En comparación con los datos iniciales, en la encuesta de mitad del período, la cobertura observada aumentó de manera considerable en la población rural de 81% a 87%, en las mujeres de 81% a 86%, en el grupo de ⩾55 años de 73% a 85%, en la población analfabeta de 71% a 80% y en la región del sur aumentó de 73% a 81% (P < 0,05). La amplitud de la brecha de equidad en los diferentes grupos del estudio (en función del asentamiento, el sexo, la edad, la educación y las zonas) disminuyó de 6% a 23% al comienzo hasta 3% a 11% en la encuesta de medio término. La máxima disminución se observó con respecto al asentamiento (rural contra urbano), de 10% a 3% (P < 0,05). Este proyecto de control de la TB dirigido por la comunidad ha logrado una alta cobertura y gran equidad en la sensibilización sobre la TB y ofrece enseñanzas valiosas a otros entornos similares en todo el mundo.
‘Axshya’, meaning free from tuberculosis (TB), is a Global Fund-supported advocacy, communication and social mobilisation (ACSM) TB project covering 374 districts across 21 states of India to increase awareness of TB and improve access to diagnostic and treatment services through increased community engagement.1,2 Through a network of around 1200 non-governmental organisations (NGOs), 3000 community-based organisations (CBOs) and 15 000 community volunteers, awareness about TB (symptoms, diagnosis, treatment and availability of free services) is being increased through community meetings with village health sanitation and nutrition committees, community groups (including self-help groups, youth groups, networks of people living with the human immunodeficiency virus, etc.) and through mid-media (wall painting, street plays, etc.) and mass media activities. Marginalised and vulnerable areas, both rural and urban, with limited access to TB services are prioritised.
Very few studies, mainly at the subdistrict level, have been conducted in the past to assess knowledge, attitudes and practices (KAP) about TB.3,4 This is the first time that large serial surveys have been conducted, one in 2010–2011 (baseline survey), before the initiation of the project activities, and another in 2012–2013 (midline survey), in 30 districts (Figure) across the country to monitor changes in KAP and provide evidence-based guidance in implementing ACSM activities.1,2 The project has been commended by the Revised National Tuberculosis Control Programme (RNTCP) for its contribution.5
FIGURE.

Geographic distribution of 30 districts across four zones in India where baseline (2010–2011) and midline (2012–2013) KAP surveys were conducted. KAP = knowledge, attitudes and practices.
ACSM for TB control has been viewed with concern by TB experts, primarily due to the lack of impact assessment tools. The present study attempts to assess the contribution of the ACSM interventions under Axshya by measuring the changes in coverage and equity of TB awareness among the general population before and during project implementation.
METHODS
This retrospective study was conducted using data from the KAP surveys conducted in 2010–2011 (baseline survey) and 2012–2013 (midline survey) as part of an assessment of changes in KAP.1,2 Thirty of India’s 374 districts were selected across four zones (north, south, east and west) using three-stage stratified cluster sampling.1,2 The 374 districts were first stratified into four zones. Of these, 30 representative districts were selected based on population proportion to size (PPS) sampling. Second, 10 rural and urban primary sampling units (PSUs) were selected in each district using PPS. Third, in each PSU, house listing and individual listing (age >18 years) was carried out and 15 individual respondents were selected based on the systematic sampling method. The sample size in both surveys was calculated using the same method.
The surveys, conducted by an independent research agency, included the administration of a structured questionnaire by trained field workers aimed at assessing TB KAP among the general population, TB patients, health care providers, opinion leaders and NGOs. Given the wider scope of the surveys, the study assessed changes between the two surveys in coverage and equity of awareness about TB as an illness among the general population and subgroups.
TB awareness was measured as ‘heard of TB as an illness’. Coverage was defined as the percentage of survey population who had ‘heard of TB as an illness’ stratified by age, sex, type of settlement (urban, rural), education (illiterate, literate) and zones (north, south, east and west). High, moderate and low coverage were defined as respectively ⩾80%, 50–79% and <50%. Equity referred to similarities in coverage between and among subgroups of the survey population or reduced gaps in TB awareness among subgroups of the survey population, as used by the World Health Organization/European Commission health care services.6,7 The comparison of proportions was analysed using the χ2 test. P ⩽ 0.05 was considered statistically significant.
The Ethics Advisory Group of the International Union Against Tuberculosis and Lung Disease (The Union), Paris, France, approved the study. Local ethics approval was obtained from the independent ethics committee of partner NGO REACH (Resource Group for Education and Advocacy for Community Health), Chennai, India.
RESULTS
The total number of respondents from the general population in the baseline and midline surveys was respectively 4562 and 4804. All those interviewed in both surveys responded on the question ‘heard of TB as an illness’. Overall coverage among the respondents during the baseline survey was 84% (3823/4562), which increased to 88% (4211/4804) during the midline survey (5% increase, P < 0.001) (Table). During the baseline survey, coverage, irrespective of sex, type of settlement, age (except for the ⩾55 years age group, 73%), education (except illiterate, 71%) and zone (except south, 73%) (P < 0.05), was high (>80%). In the midline survey, coverage in all subgroups, including the ⩾55 years age group (85%), the illiterate (80%) and the south zone (81%) (P < 0.05), increased significantly.
TABLE.
Baseline and midline coverage and equity of TB awareness in the Axshya project among marginalised and vulnerable populations and subgroups in India between 2010–2011 (baseline) and 2012–2013 (midline)
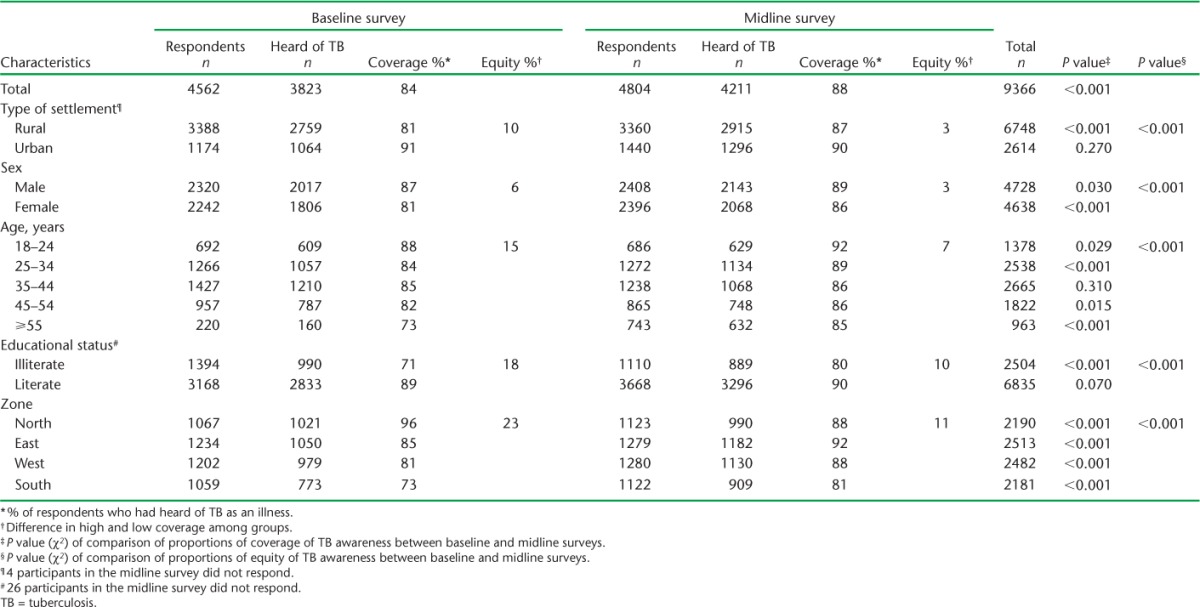
Equity (coverage gap) ranged from 6% (male, 87%; female 81%) to 23% (south, 71%; north, 96%) in the baseline survey, which was narrowed down from 3% (male, 89% vs. female, 86% and rural, 87% vs. urban, 90%) to 11% (south, 81%; east, 92%) in the midline survey (P < 0.05) (Table 1). The maximum decline in equity gap was observed for type of settlement, which fell from 10% (rural, 81%; urban, 91%) to 3% (rural, 87%; urban, 90%) (P < 0.05).
DISCUSSION
Of the estimated 3 million TB cases missed globally every year, 1 million are thought to be in India.7,8 The primary reasons for missed cases are 1) limited access to health care due to poor awareness about TB and TB services, stigma and discrimination, little community engagement; 2) lack of diagnosis despite having access; and 3) lack of notification even when diagnosed.9 Through a network of around 1200 NGOs, 3000 CBOs and 15 000 community volunteers, the Axshya project is raising awareness about TB and identifying presumptive TB patients (PTBP) by symptom screening (⩾2 weeks of cough) and linking them to the diagnostic and treatment services available under India’s RNTCP. The PTBPs identified are given the choice to be referred or to have their sputum collected and transported to the nearest microscopy centre for sputum examination.
The study has revealed a significant increase in TB awareness coverage among the different subgroups of the survey population over a period of 2 years. Coverage was high among the rural population, at either end of the age spectrum, among the illiterate, and in the south and east zones. A significant decline in north zone coverage, from 96% at baseline to 88% at midline, was noted. This could be attributed to the delay in the initiation of project activities in north zone districts. Ensuring equitable coverage is a major challenge under any TB programme. However, the project was equitable among the subgroups of the survey population at midline. The considerable coverage gap was significantly reduced among male vs. female, rural vs. urban, younger vs. older age groups, literate vs. illiterate and the different zones. In China, an ACSM project has also raised awareness and improved health-seeking behaviour.10 Interestingly, according to the RNTCP annual report, the number of PTBPs examined in the 374 project districts increased from 9 907 457 (2010–2011) to 10 257 051 (2012–2013), a 4% change.5,11 However, this increase may not be entirely attributable to project activities, but associated with other factors, including economic growth, rise in education levels, the efforts of other ongoing projects and the impact of audiovisual media. This requires further research.
The gain in coverage could be due to the focused project interventions undertaken by trained community volunteers delivering key messages on various aspects of TB, including symptoms, diagnosis, treatment and the availability of free services. The project has also trained and engaged non-qualified health care providers to serve as the first point of contact for the majority of the rural and urban poor, community groups and associations, village heads, opinion leaders and district forums. This may also have indirectly raised awareness among the population. The project targeted women, children and rural populations in all zones, and this may have helped to reduce the equity gap. Challenges in implementing project interventions include the vast coverage area; socio-culturally diverse populations; standardisation of messages; varied capacity of the local NGOs, CBOs and volunteers; and matching demand with quality-assured TB services.
There are some limitations to the study: 1) respondents in the two surveys were different, 2) the study is powered at the zonal level, and 3) increase in awareness could also be related to the increase in the education and economic level of the respondents interviewed at midline and other TB interventions in the survey areas. Further research is needed to understand the contribution of the project in enhancing access to TB services disaggregated by age group, sex and other socio-economic factors.
In conclusion, this study has shown that community-driven ACSM projects can enhance TB awareness despite numerous challenges, and that this is associated with an increased number of people accessing TB diagnostic services. This offers a valuable lesson for similar settings in other parts of the world.
Footnotes
Conflicts of interest: none declared.
References
- 1.International Union Against Tuberculosis and Lung Disease South-East Asia Office. KAP study of tuberculosis in India. New Delhi, India: The Union SouthEast Asia Office; 2011. http://www.axshya-theunion.org/images/documents/kap-survey.pdf Accessed February 2015. [Google Scholar]
- 2.International Union Against Tuberculosis and Lung Disease South-East Asia Office. KAP study of tuberculosis in India. New Delhi, India: The Union South-East Asia Office; 2014. http://www.axshya-theunion.org/images/documents/kap-midline.pdf Accessed February 2015. [Google Scholar]
- 3.Chinnakali P, Ramakrishnan J, Vasudevan K , Gurumurthy J, Upadhyay R P, Panigrahi K C. Level of awareness about tuberculosis in urban slums: implications for advocacy and communication strategy planning in the national program. Lung India. 2013;30:139–142. doi: 10.4103/0970-2113.110422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kar M, Logaraj M. Awareness, attitude and treatment seeking behaviour regarding tuberculosis in a rural area of Tamil Nadu. Indian J Tuberc. 2010;57:226. [PubMed] [Google Scholar]
- 5.Central TB Division, Directorate General of Health Services, Ministry of Health and Family Welfare. TB India 2014, Revised National Tuberculosis Control Programme Annual Status Report. New Delhi, India: Revised National Tuberculosis Control Programme, India; 2014. http://www.tbcindia.nic.in/pdfs/TB%20INDIA%202014.pdf Accessed February 2015. [Google Scholar]
- 6.Thapa S. High and equitable coverage of Vitamin A supplementation program in Nepal. J Community Med Health Educ. 2014;4:1. [Google Scholar]
- 7.Directorate-General for Employment, Social Affairs and Equal Opportunities, European Commission. Quality in and equality of access to healthcare services. Brussels, Belgium: European Commission; 2008. http://www.euro.centre.org/data/1237457784_41597.pdf. Accessed February 2015. [Google Scholar]
- 8.World Health Organization. Global TB report 2014. Geneva, Switzerland: WHO; 2014. WHO/HTM/TB/2014.08. http://apps.who.int/iris/bitstream/10665/137094/1/9789241564809_eng.pdf?ua=1 Accessed February 2015. [Google Scholar]
- 9.World Health Organization. World TB Day brochure 2014. Geneva, Switzerland: WHO; 2014. chnhttp://www.stoptb.org/assets/documents/resources/publications/acsm/WORLD_TB_DAY_BROCHURE_14March.pdf. Accessed February 2015. [Google Scholar]
- 10.Zhang T, Tang S, Jun G, Whitehead M. Persistent problems of access to appropriate, affordable TB services in rural China: experiences of different socio-economic Groups. BMC Public Health. 2007;7:19. doi: 10.1186/1471-2458-7-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Central TB Division, Directorate General of Health Services, Ministry of Health and Family Welfare. TB India 2012, Revised National Tuberculosis Control Programme Annual Status Report. New Delhi, India: Revised National Tuberculosis Control Programme; 2012. http://tbcindia.nic.in/pdfs/TB%20India%202012-%20Annual%20Report.pdf Accessed February 2015. [Google Scholar]


