Abstract
Background: The lack of published information about children with multidrug-resistant tuberculosis (MDR-TB) is an obstacle to efforts to advocate for better diagnostics and treatment.
Objective: To describe the lack of recognition in the published literature of MDR-TB and extensively drug-resistant TB (XDR-TB) in children.
Design: We conducted a systematic search of the literature published in countries that reported any MDR- or XDR-TB case by 2012 to identify MDR- or XDR-TB cases in adults and in children.
Results: Of 184 countries and territories that reported any case of MDR-TB during 2005–2012, we identified adult MDR-TB cases in the published literature in 143 (78%) countries and pediatric MDR-TB cases in 78 (42%) countries. Of the 92 countries that reported any case of XDR-TB, we identified adult XDR-TB cases in the published literature in 55 (60%) countries and pediatric XDR-TB cases for 9 (10%) countries.
Conclusion: The absence of publications documenting child MDR- and XDR-TB cases in settings where MDR- and XDR-TB in adults have been reported indicates both exclusion of childhood disease from the public discourse on drug-resistant TB and likely underdetection of sick children. Our results highlight a large-scale lack of awareness about children with MDR- and XDR-TB.
Keywords: tuberculosis, multidrug-resistant, extensively drug-resistant tuberculosis, pediatric
Abstract
Cadre : La pénurie d’informations publiées sur la tuberculose multirésistante (TB-MDR) de l’enfant entrave les efforts visant à en améliorer le diagnostic et le traitement.
Objectif : Décrire le manque de reconnaissance de la TB-MDR et de la TB ultra-résistante (TB-XDR) de l’enfant dans la littérature publiée.
Schéma : Nous avons réalisé une recherche systématique de la littérature publiée dans les pays qui ont déclaré au moins un cas de TB-MDR ou -XDR avant 2012 afin d’identifier des cas de TB-MDR ou -XDR chez des adultes et des enfants.
Résultats : Sur les 184 pays et territoires qui ont déclaré des cas de TB-MDR entre 2005 et 2012, nous avons identifié des cas de TB-MDR de l’adulte dans la littérature dans 143 (78%) pays et des cas de TB-MDR pédiatrique dans 78 (42%) pays. Sur les pays qui ont déclaré des cas de TB-XDR, nous avons identifié des cas adultes dans la littérature dans 55 (60%) pays et des cas pédiatriques dans 9 (10%) pays.
Conclusion : L’absence de publications documentant les cas de TB-MDR et -XDR chez l’enfant dans des régions où la TB-MDR et la TB-XDR ont été déclarées chez les adultes témoigne à la fois d’une exclusion de la maladie de l’enfant du discours public sur la TB pharmacorésistante et probablement d’une sous-détection des enfants malades. Nos résultats mettent en évidence un manque de connaissance à grande échelle de la TB-MDR et de la TB-XDR de l’enfant.
Abstract
Marco de referencia: La falta de información publicada sobre los niños con tuberculosis multidrogo-resistente (TB-MDR) es un obstáculo a los esfuerzos para abogar por mejores diagnósticos y tratamientos.
Objetivos: Describir la falta de reconocimiento en la literatura publicada de la TB-MDR y la TB extremadamente resistente (TB-XDR) en los niños.
Métodos: Para los países que hasta 2012 habían informado de algún caso de TB-MDR o TB-XDR, realizamos una búsqueda sistemática de la literatura publicada para identificar casos de TB-MDR o TB-XDR en adultos y en niños.
Resultados: De los 184 países y territorios que informaron algún caso de TB-MDR durante 2005–2012, encontramos reportes de casos de TB-MDR en adultos en la literatura publicada para 143 (78%) países, y reportes de casos de TB-MDR pediátricos para 78 (42%) países. De los 92 países que informaron algún caso de TB-XDR, encontramos reportes de casos de TB-XDR en adultos en la literatura publicada para 55 (60%) países y reportes de casos de TB-XDR pediátricos para 9 (10%) países.
Conclusión: La ausencia de publicaciones que documentan casos de TB-MDR y TB-XDR pediátricos en lugares donde casos de TB-MDR y TB-XDR en adultos han sido reportados indica tanto la exclusión de enfermedad infantil del discurso público sobre la TB drogo-resistente y la probable sub-detección de niños enfermos. Nuestros resultados recalcan la falta de reconocimiento a gran escala de los niños con TB-MDR y TB-XDR.
Multidrug-resistant tuberculosis (MDR-TB, defined as TB resistant to at least both isoniazid and rifampin), among children is an unrecognized epidemic. Like drug-susceptible TB, MDR-TB is curable, but treatment requires the use of longer regimens with more toxic drugs, few of which are available in child-friendly formulations.1 Although an estimated 32 000 children fall sick each year with MDR-TB,2 few of these are diagnosed and treated. An analysis of age-disaggregated surveillance data collected in 85 countries during 1994–2011 found that 50 (59%) of these countries reported no child MDR-TB cases,3 although many of them did report cases of MDR-TB, presumably in adults, during this period.4 The microbiological diagnosis of drug-resistant TB in children is complicated by insensitive diagnostic tests, limited diagnostic capacity in many countries with high TB burdens5 and the inability of young children to expectorate sputum.6 These diagnostic challenges, as well as historic misperceptions that children are not likely to be important contributors to or victims of the global TB epidemic,7 have contributed to the invisibility of the MDR-TB epidemic among children.8
The lack of published evidence documenting numbers of children treated for MDR-TB, as well as treatment practices and outcomes, is an obstacle to efforts to advocate for better diagnostics, treatments, and policies for children with MDR-TB. As publicly available data on numbers of MDR-TB cases reported by different countries are not disaggregated by age,4 it is impossible to determine how many children are diagnosed with MDR-TB each year. A systematic review of studies reporting outcomes among children treated for MDR-TB found only eight studies, comprising a total of 315 children.9 With such sparse published evidence on both the magnitude of the problem and its potential solutions, it is difficult to convince companies to invest in new diagnostics for drug-resistant disease in children, investigators to include children in clinical trials of second-line regimens and governments to reform policies that limit access to effective treatment for children with MDR-TB.
As global TB policies tend to focus on adults, there is a profound lack of awareness about the MDR-TB epidemic among children. In the present study, we sought to describe the current state of awareness about children with MDR-TB by comparing documentation of child and adult MDR-TB cases in the published literature.
METHODS
The numbers of MDR-TB cases reported each year by governments of individual countries and territories (referred to from here on as ‘countries’) are publicly available through the World Health Organization (WHO).4 Based on these data, we compiled a list of countries that reported at least one notified MDR-TB case during 2005–2012.4 We then used a systematic search of the published literature to identify child and adult MDR-TB cases in each country. We repeated this process to identify child and adult cases of extensively drug-resistant TB (XDR-TB), the subset of MDR-TB strains with additional resistance to fluoroquinolones and second-line injectable agents.
For each country, we attempted to identify a publication documenting at least one MDR-TB case in a child aged ⩽14 years, and one documenting at least one MDR-TB case in an adult aged >14 years (Figure 1). In our search for pediatric MDR-TB cases, we first referred to two publications documenting country-specific reports of MDR-TB in children: one based on WHO surveillance data3 and the other a systematic review.2 For countries in which no pediatric MDR-TB cases were indicated in either of these publications, we systematically searched for publications published through 1 July 2014 in PubMed, EMBASE, LILACS, Web of Science, BIOSIS and WHO regional databases. Together, these databases include citations for a variety of published literature, including research publications, case reports, editorials and conference abstracts.
FIGURE 1.
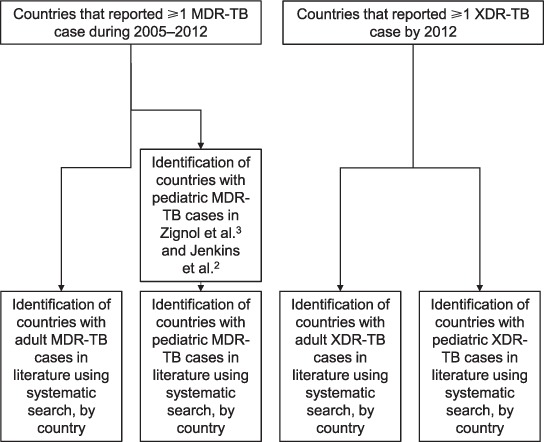
Search strategy for identifying publications, by country, for adult and pediatric MDR- and XDR-TB cases among countries that reported MDR- and XDR-TB cases. MDR-TB = multidrug-resistant tuberculosis; XDR-TB = extensively drug-resistant TB.
No reviews or surveillance summaries explicitly focused on adults with MDR-TB. We referred to the aforementioned systematic review of MDR-TB in children,2 which also documented adult cases in some countries. For the remaining countries, we systematically searched the published literature for publications documenting adult MDR-TB cases. We used an analogous process to search for XDR-TB cases in both adults and children in all countries that had reported at least one XDR-TB case by 2012.10
We used search terms that included combinations intended to capture publications documenting MDR- and XDR-TB cases (e.g., ‘multidrug resistant tuberculosis,’ ‘MDR-TB,’ ‘drug-resistant TB’) and country names. In our search for child cases, we also included terms intended to capture children (e.g., ‘child*,’ ‘pediatric’). The complete search strategy is documented in Appendix Table A.1. We did not restrict publications on the basis of language. For publications in English and Spanish, we contacted authors by e-mail for additional information if the publication identified MDR- or XDR-TB cases but we were unable to determine the age of subjects.
For each of the four categories of cases (child MDR-TB, adult MDR-TB, child XDR-TB, adult XDR-TB), we considered a single publication sufficient to document the presence of that type of case in a given country. If our search yielded multiple published reports for a country, we recorded only the most recent English-language report, or the most recent report in any language if no English-language report was found.
No ethics approval was required for this study, as the data used were publicly available and contained no personal identifying information.
RESULTS
Of the 216 national and territorial governments that reported TB case data, 184 (85%) reported at least one case of MDR-TB during 2005–2012.4 Through our literature searches, we found publications documenting adult MDR-TB cases in 143 (78%) of the 184 countries (Table and Appendix Table A.2). By contrast, we found publications documenting pediatric MDR-TB cases in 78 (42%) of these countries. We were thus unable to identify any pediatric MDR-TB cases for 45% of the countries for which we were able to identify adult MDR-TB cases through our systematic literature search. There were no countries with publications documenting MDR-TB cases in children but not in adults.
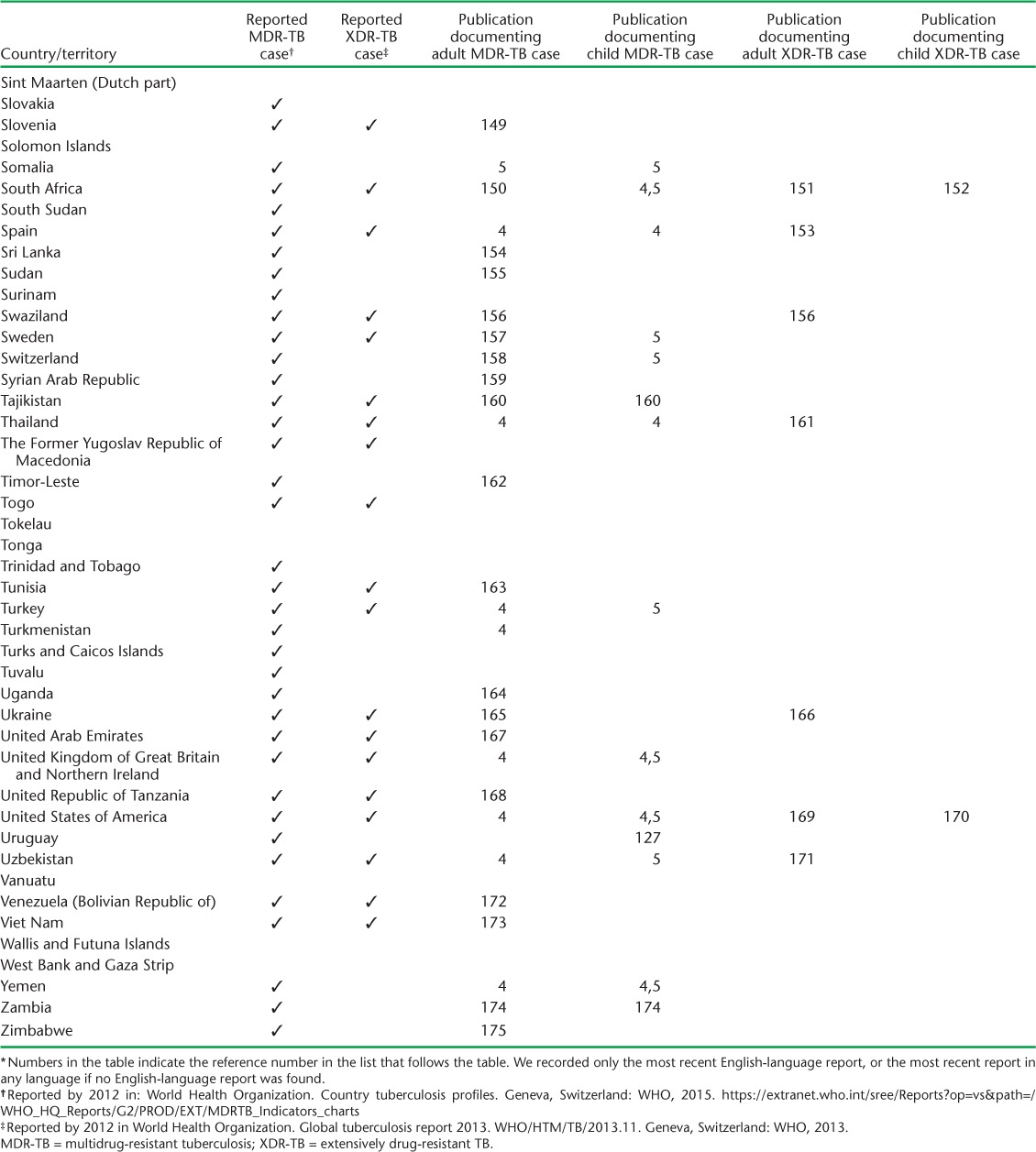
TABLE.
Countries and territories with publications documenting MDR-TB cases in adults and children *
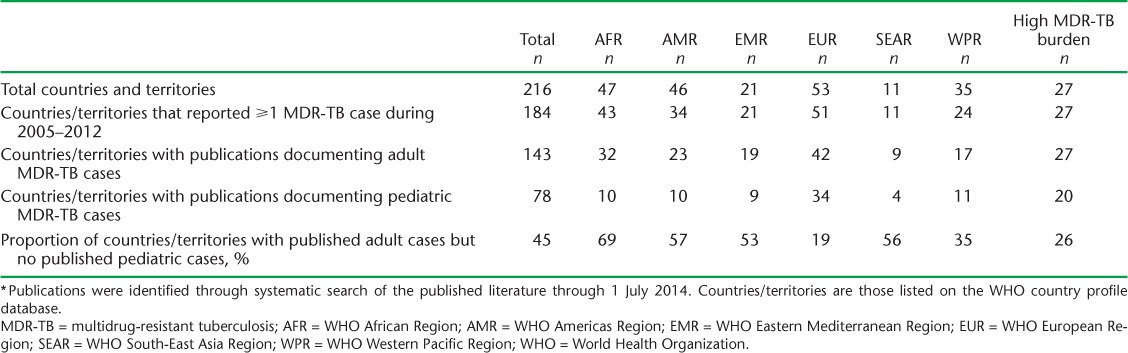
Figure 2 shows the countries categorized according to whether any MDR-TB case was reported during 2005–2012, whether we identified any adult MDR-TB case through our literature search and whether we identified any pediatric MDR-TB case through our literature search. The proportion of countries for which we were able to find publications documenting adult MDR-TB cases but not pediatric MDR-TB cases was highest for the WHO African Region (69%) and lowest for the European region (19%) (Table). We found publications documenting adult MDR-TB cases for all of the 27 countries classified as having a high MDR-TB burden,10 but found no publications documenting pediatric MDR-TB cases for 7 (26%) of these countries.
FIGURE 2.
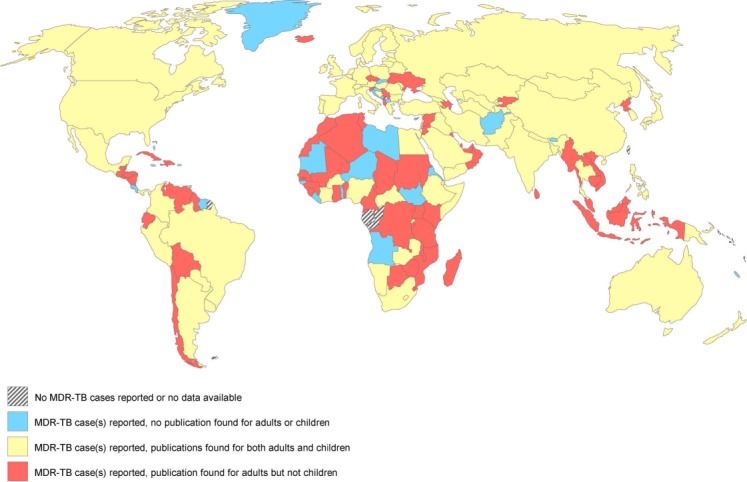
Adult vs. child MDR-TB cases in the published literature: documentation of adult vs. child MDR-TB cases in the published literature among countries reporting ⩾1 case of MDR-TB during 2005–2012. Note that some smaller countries and territories are not depicted. MDR-TB = multidrug-resistant tuberculosis.
By 2012, XDR-TB cases had been reported in 92 countries.10 We identified publications documenting adult XDR-TB cases for 55 (60%) of these countries, and publications documenting pediatric XDR-TB cases for 9 (10%) countries. We found no pediatric XDR-TB cases for 84% of the countries for which we identified adult XDR-TB cases through our literature search. Figure 3 shows the countries categorized according to whether any case of XDR-TB was reported by 2012, whether we identified any adult XDR-TB case through our literature search and whether we identified any pediatric XDR-TB case through our literature search.
FIGURE 3.
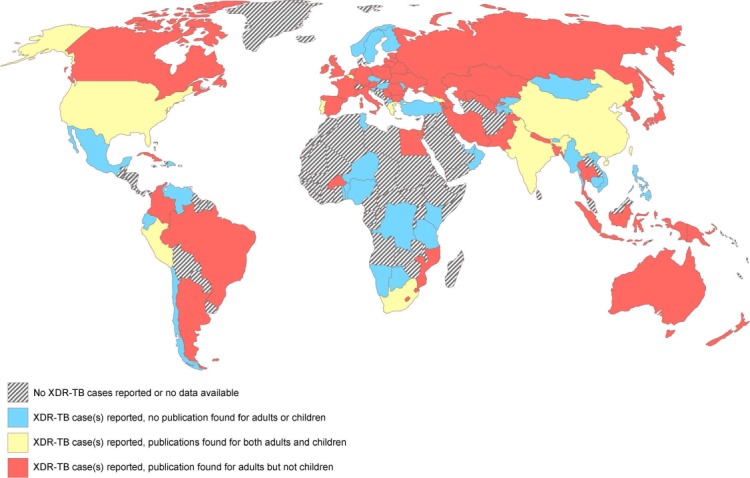
Adult vs. child XDR-TB cases in the published literature: documentation of adult vs. child XDR-TB cases in the published literature among countries reporting ⩾1 case of XDR-TB by 2012. Note that some smaller countries and territories are not depicted. XDR-TB = extensively drug-resistant tuberculosis.
DISCUSSION
In almost every household where an adult has TB, children, who are even more susceptible than adults to developing TB disease,11 are exposed. However, although we found documentation of MDR-TB cases in adults for over three quarters of the countries whose governments reported any case of MDR-TB by 2012 through systematic searches of published literature, we were unable to find published reports of MDR-TB in children for over half of these countries. We were unable even to find published reports of MDR-TB cases in children for a quarter of the countries with a high MDR-TB burden. The size of the discrepancy varied by geographic region, and was even greater in our search for XDR-TB cases. Our results are consistent with large-scale deficient disease awareness of children with MDR- and XDR-TB. This deficiency has major implications for national and global TB policies, as children (age ⩽14 years) make up approximately 25% of the global population and may comprise 20–40% of persons with TB in high TB incidence settings.12
The pronounced absence of childhood MDR-TB cases in the literature is worrying, as the published literature is an important forum for the dissemination of information, the discussion of public health policy, and the testing of new ideas. In a time when MDR- and XDR-TB are gaining worldwide attention, the absence of child cases in the published literature can only perpetuate the invisibility of children already suffering from these forms of TB. Of course, there may be reasons for this absence: research publications often exclude children, and publications are generally not a priority for resource-limited TB programs struggling to provide treatment. However, as programs strive to improve the diagnosis and treatment of children with MDR- and XDR-TB, the lack of published evidence in these areas may prove an obstacle.
While the absence of cases in the published literature may not indicate an actual absence of diagnosed cases, the magnitude of the discrepancy between published accounts of adult cases and published accounts of child cases raises strong suspicions about underdetection. Given the large number of adults worldwide with untreated or inadequately treated MDR-TB,13 transmission to children in their households is inevitable, and child MDR-TB cases are to be expected wherever adult MDR-TB cases are reported.8 Recent estimates have suggested that each year 600 000 children worldwide require evaluation for household exposure to MDR-TB,8 and that 30 000–50 000 require treatment for MDR-TB.2,8 However, many of these children are likely going undiagnosed. Although global data on children diagnosed with MDR- and XDR-TB are lacking, widespread underdetection of child MDR-TB cases is suggested by the finding that 59% of the countries from which age-disaggregated surveillance data on MDR-TB were available reported no child MDR-TB cases,3 although many of these countries did report MDR-TB cases, presumably in adults.4
The major limitation of the present analysis is that a review of published literature is unable to distinguish between the effect of underdetection of MDR- and XDR-TB in children and the effect of any publication disparities that may exist. Many factors could contribute to a publication bias against reports that include children with drug-resistant TB. For example, research studies often exclude children; analyses of routinely collected data on patients are frequently limited to patients with bacteriologically confirmed disease, which reduces the likelihood of children being included; and children are commonly excluded from drug resistance and prevalence surveys. In addition, countries with high TB burdens (and likely higher relative burdens of childhood TB cases12) are often poorly represented in the published literature; the ratio of TB publications to TB cases is orders of magnitude higher for Western Europe, the United States and Canada, than for Asia, Eastern Europe, Africa and Latin America.14 Many countries for which we found no publications documenting any MDR-TB case were countries for which few TB publications existed. However, true underdetection of MDR-TB in children is also likely in many of these countries given the limitations in the current diagnostic capacities of their TB programs. Public availability of age-group-specific data on reported MDR- and XDR-TB cases would allow a more careful assessment of the relative contributions of underdetection and publication bias to our findings.
Another limitation is that our analysis only included publications that were indexed in a systematically searchable format; although available databases cover a variety of publications, including conference abstracts, bulletins and perspective pieces, some types of publications, such as advocacy materials and national tuberculosis program reports, are generally not included. While information on children with MDR- and XDR-TB may appear in these other types of publications, we had no way of systematically searching them. A recent advocacy effort to collect information about the experiences of children with drug-resistant TB found stories of children with MDR-TB from 10 of the countries for which we could not find any publications in our search.15
However, despite the limitations inherent in using published literature as an indicator of case detection, our results add weight to the suspicion of underdetection of MDR- and XDR-TB in children. Reasons for this underdetection are varied, but multiple steps can be taken to overcome existing obstacles to the recognition of child cases of drug-resistant disease. First, providers require more training to recognize the manifestations of TB disease in children, which can be diverse and non-specific.16 In addition, as children frequently have paucibacillary disease and cannot produce sputum, programs should employ child-focused methods of specimen collection and diagnostic technologies that are more sensitive than smear microscopy.16 Even with these methods, however, cultured isolates for drug susceptibility testing (DST) will be unavailable for the majority of sick children.6 Both individual providers and TB programs should therefore presumptively treat sick children who meet clinical criteria for TB disease and drug resistance in the absence of bacteriologic confirmation.6,17 Finally, household contact investigations of adult MDR- and XDR-TB patients should be carried out to promptly identify and treat children with drug-resistant TB.8
Underdetection of childhood drug-resistant TB cases should be an indicator of weaknesses in TB programs, such as the failure to perform contact investigations or the underutilization of sensitive diagnostic techniques. To rigorously quantify underdetection, accurate counting of children with MDR- and XDR-TB will be necessary. If programs count and report only bacteriologically confirmed cases of drug-resistant TB, a substantial proportion of children with MDR- and XDR-TB will not be included, as the majority of children with TB will not have a bacterial culture available for DST.6 Surveillance systems should therefore allow for the reporting of probable MDR-TB cases in children, with diagnosis based on clinical evidence of disease and exposure to an MDR- or XDR-TB case.18 Furthermore, universal reporting of MDR- and XDR-TB cases by age group19 and public accessibility of these surveillance data are necessary to broaden our understanding of the magnitude of the drug-resistant TB epidemic in children.
CONCLUSION
The absence of information about child MDR- and XDR-TB cases in countries where adult cases have been reported has major implications for national and global TB policies. Recognition of this large-scale deficiency in awareness should spur more systematic work to improve surveillance for and estimates of TB cases in children, which are necessary to allow programs to project unmet needs and allocate resources. In addition, it should serve as a warning that children with drug-resistant TB in these countries are going undiagnosed. Clinical awareness, aggressive methods of specimen collection, use of sensitive diagnostics and active case finding through contact investigation are all needed to ensure that children with TB—including those with MDR- and XDR-TB—are promptly recognized and treated.20 Finally, policy makers, providers, investigators and advocates should all be aware that the discourse about how to end the toll of drug-resistant TB must include children to ensure that this vulnerable population is not neglected.
Acknowledgments
This work was supported by funding from Janssen (Beerse, Belgium). The funder had no role in the study design, collection of data, analysis or interpretation of data, writing of the report, or decision to submit the paper for publication.
The authors would like to thank C GawneMark and B Liebenow for their help with data collection and P A Bain, Countway Library of Medicine, Harvard Medical School, Boston, MA, USA, for his help to develop the literature search strategy. We would also like to thank N Candia, H Cox, D Falzon, M Joloba, C Martinaud, J Millet, D L Molina, N Rastogi, L Nelson, R Noor, V Ritacco, P W Smit, E Talbot, A Trébucq, A Van Deun, T Vremera, and I Živanović for kindly providing additional unpublished data in response to our requests.
APPENDIX
TABLE A.1.
Terms used in systematic searches of published literature
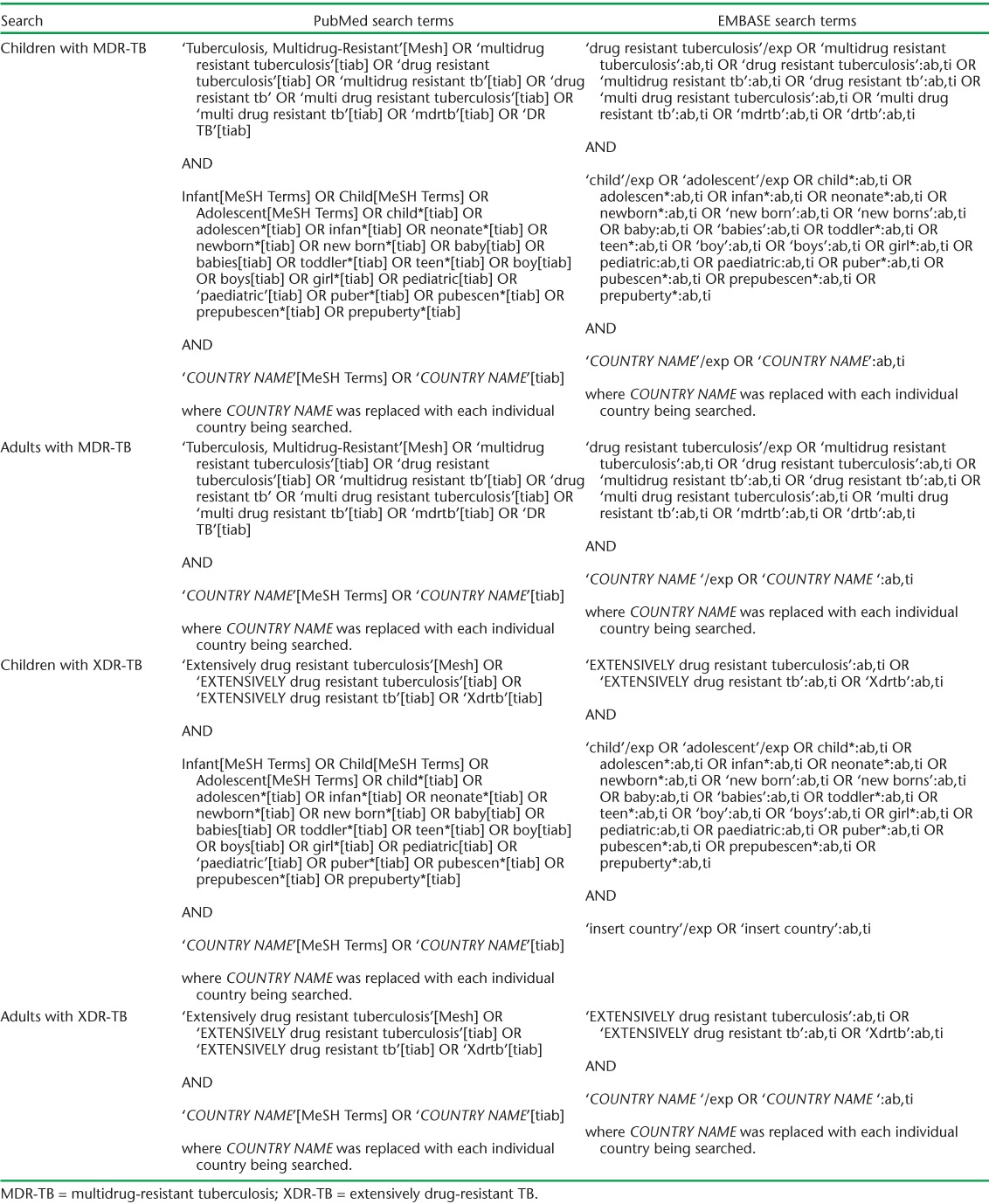
TABLE A.2.
Table of identified references by country *
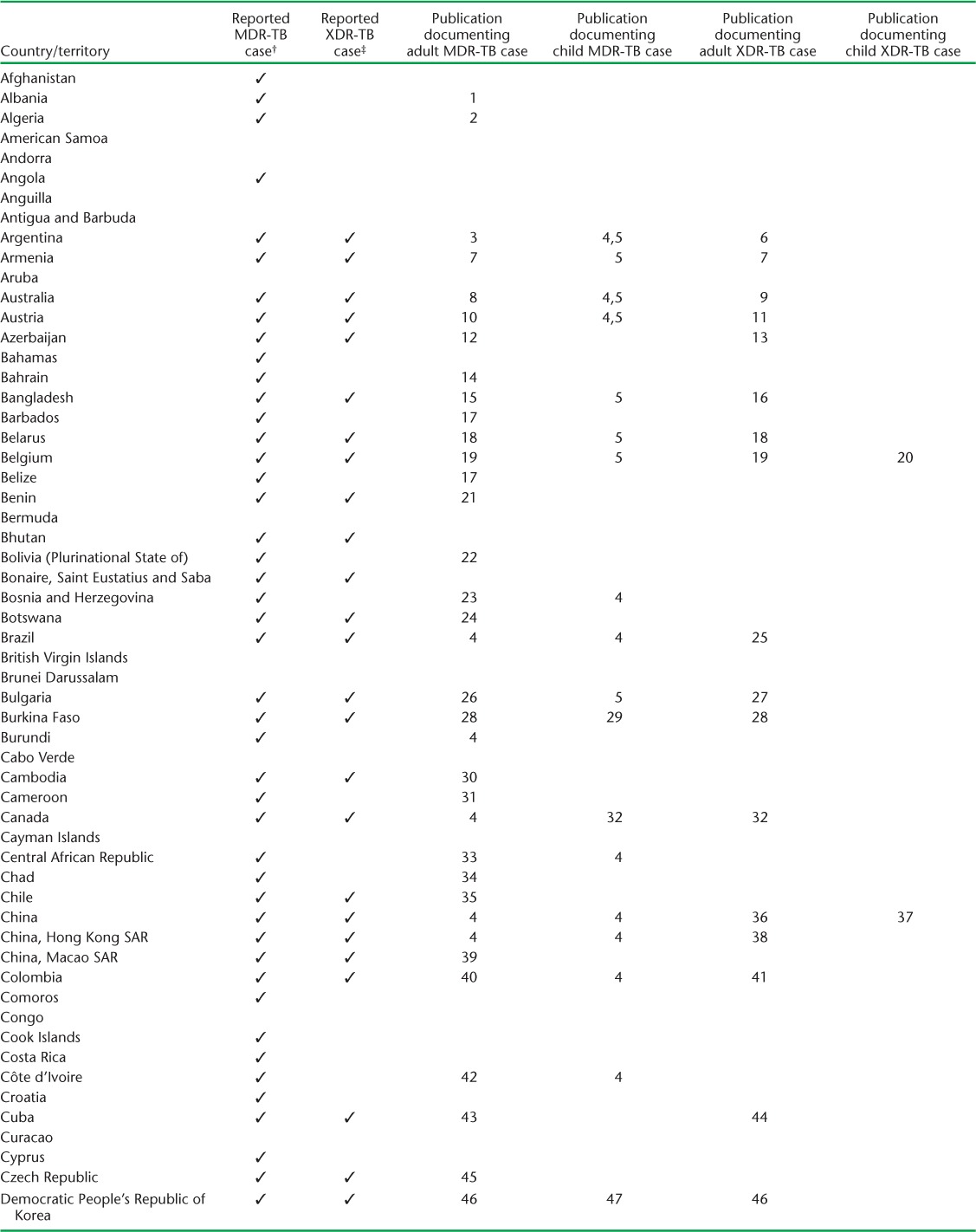
TABLE A.2.
(continued)
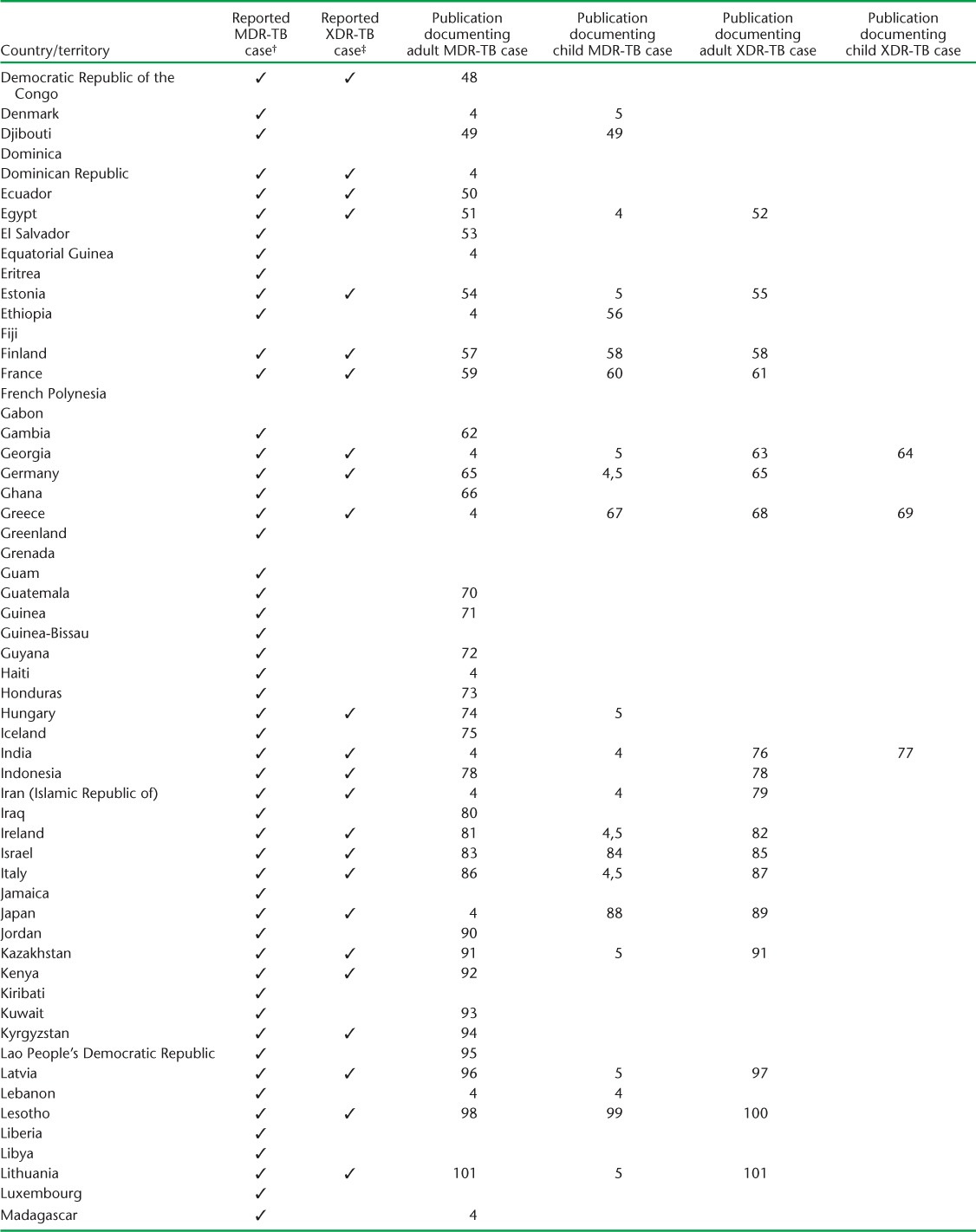
TABLE A.2.
(continued)
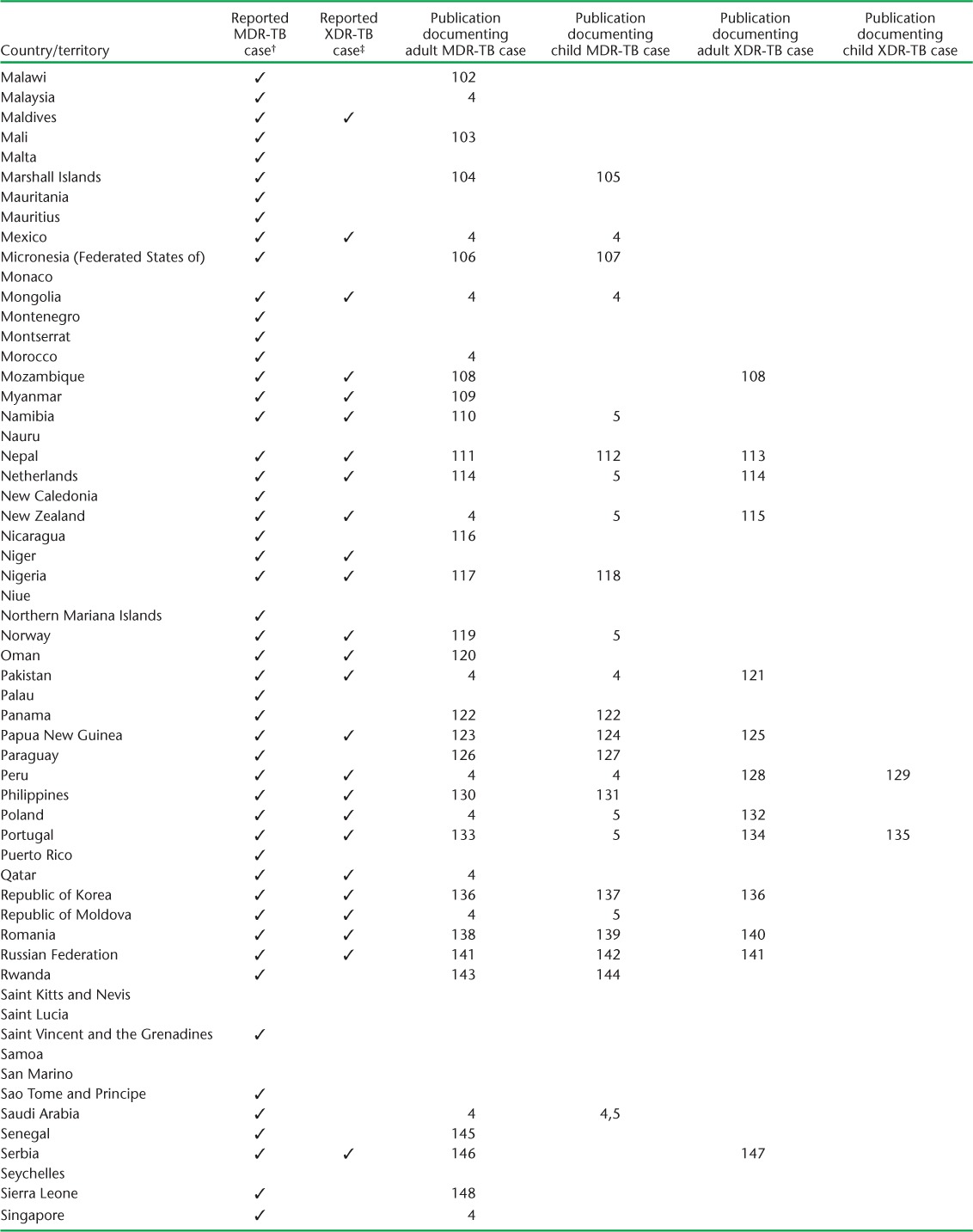
TABLE A.2.
(continued)
References
- 1.Tafaj S, Zhang J, Hauck Y et al. First insight into genetic diversity of the Mycobacterium tuberculosis complex in Albania obtained by multilocus variable-number tandem-repeat analysis and spoligotyping reveals the presence of beijing multidrug-resistant isolates. J Clin Microbiol. 2009;47:1581–1584. doi: 10.1128/JCM.02284-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ifticene M, Gacem F Z, Yala D, Boulahbal F. Mycobacterium tuberculosis genotype Beijing: about 15 strains and their part in MDR-TB outbreaks in Algeria. Int J Mycobacteriol. 2012;1:196–200. doi: 10.1016/j.ijmyco.2012.10.006. [DOI] [PubMed] [Google Scholar]
- 3.Reniero A, Beltran M, de Kantor I N, Ritacco V. AIDS patient’s long-term battle with multiply recurrent tuberculosis: reinfection or reactivation? Rev Argent Microbiol. 2010;42:271–273. doi: 10.1590/S0325-75412010000400006. [DOI] [PubMed] [Google Scholar]
- 4.Jenkins H E, Tolman A W, Yuen C M et al. Incidence of multidrug-resistant tuberculosis disease in children: systematic review and global estimates. Lancet. 2014;383:1572–1579. doi: 10.1016/S0140-6736(14)60195-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zignol M, Sismanidis C, Falzon D, Glaziou P, Dara M, Floyd K. Multidrug-resistant tuberculosis in children: evidence from global surveillance. Eur Respir J. 2013;42:701–707. doi: 10.1183/09031936.00175812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abbate E, Vescovo M, Natiello M et al. Successful alternative treatment of extensively drug-resistant tuberculosis in Argentina with a combination of linezolid, moxifloxacin and thioridazine. J Antimicrob Chemother. 2012;67:473–477. doi: 10.1093/jac/dkr500. [DOI] [PubMed] [Google Scholar]
- 7.Sanchez E. Treatment outcome of a cohort of drug-resistant tuberculosis patients in Yerevan (Armenia) Trop Med Int Health. 2009;14:41. [Google Scholar]
- 8.Francis J R, Blyth C C, Colby S, Fagan J M, Waring J. Multidrug-resistant tuberculosis in Western Australia, 1998–2012. Med J Aust. 2014;200:328–332. doi: 10.5694/mja13.11342. [DOI] [PubMed] [Google Scholar]
- 9.Lumb R, Bastian I, Carter R, Jelfs P, Keehner T, Sievers A. Tuberculosis in Australia: bacteriologically confirmed cases and drug resistance, 2010. A report of the Australian Mycobacterium Reference Laboratory Network. Commun Dis Intell Q Rep. 2013;37:E40–E46. [PubMed] [Google Scholar]
- 10.Schmid D, Fretz R, Kuo H W et al. An outbreak of multidrug-resistant tuberculosis among refugees in Austria, 2005–2006. Int J Tuberc Lung Dis. 2008;12:1190–1195. [PubMed] [Google Scholar]
- 11.Indra A, Rowhani M, Rumetshofer R et al. Extensively drug-resistant tuberculosis: first report of a case in Austria, May 2008. Euro Surveill. 2008;13:18940. [PubMed] [Google Scholar]
- 12.Pfyffer G E, Strassle A, van Gorkum T et al. Multidrug-resistant tuberculosis in prison inmates, Azerbaijan. Emerg Infect Dis. 2001;7:855–861. doi: 10.3201/eid0705.017514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gkaravela L, Foka A, Athanassiou M et al. The genetic diversity of Mycobacterium tuberculosis complex in Azerbaijan by 24 MIRU-VNTR loci genotyping in association with susceptibility testing by conventional and molecular methods. Clin Microbiol Infect. 2012;18:829. [Google Scholar]
- 14.Elhassan M, Saeed S, Elmekki M, Al-Jarie A, Hamid M. Detection of multi-drug-resistant tuberculosis using PCR compared to the conventional proportional method. Bahrain Med Bull. 2012;34:11–15. [Google Scholar]
- 15.Flora M S, Amin M N, Karim M R et al. Risk factors of multidrug-resistant tuberculosis in Bangladeshi population: a case control study. Bangladesh Med Res Counc Bull. 2013;39:34–41. doi: 10.3329/bmrcb.v39i1.15808. [DOI] [PubMed] [Google Scholar]
- 16.Noor R, Akhter S, Rahman F, Munshi S, Kamal S M M, Feroz F. Frequency of extensively drug-resistant tuberculosis (XDR-TB) among re-treatment cases in NIDCH, Dhaka, Bangladesh. J Infect Chemother. 2013;19:243–248. doi: 10.1007/s10156-012-0490-8. [DOI] [PubMed] [Google Scholar]
- 17.Millet J, Baboolal S, Streit E, Akpaka P E, Rastogi N. A first assessment of Mycobacterium tuberculosis genetic diversity and drug-resistance patterns in twelve caribbean territories. Biomed Res Int. 2014;2014:718496. doi: 10.1155/2014/718496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Skrahin A, Ahmed R K, Ferrara G et al. Autologous mesenchymal stromal cell infusion as adjunct treatment in patients with multidrug and extensively drug-resistant tuberculosis: an open-label phase 1 safety trial. Lancet Respir Med. 2014;2:108–122. doi: 10.1016/S2213-2600(13)70234-0. [DOI] [PubMed] [Google Scholar]
- 19.Stoffels K, Allix-Beguec C, Groenen G et al. From multidrug- to extensively drug-resistant tuberculosis: upward trends as seen from a 15-year nationwide study. PLOS ONE. 2013;8:e63128. doi: 10.1371/journal.pone.0063128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dauby N, Muylle I, Mouchet F, Sergysels R, Payen M C. Meropenem/clavulanate and linezolid treatment for extensively drug-resistant tuberculosis. Pediatr Infect Dis J. 2011;30:812–813. doi: 10.1097/INF.0b013e3182154b05. [DOI] [PubMed] [Google Scholar]
- 21.Trébucq A, Anagonou S, Gninafon M, Lambregts K, Boulahbal F. Prevalence of primary and acquired resistance of Mycobacterium tuberculosis to antituberculosis drugs in Benin after 12 years of short-course chemotherapy. Int J Tuberc Lung Dis. 1999;3:466–470. [PubMed] [Google Scholar]
- 22.Monteserin J, Camacho M, Barrera L, Palomino J C, Ritacco V, Martin A. Genotypes of Mycobacterium tuberculosis in patients at risk of drug resistance in Bolivia. Infect Genet Evol. 2013;17:195–201. doi: 10.1016/j.meegid.2013.04.010. [DOI] [PubMed] [Google Scholar]
- 23.Spiric N, Marinkovic T, Milakovic D, Kecman R. Case report of hyperuricemia caused by pyrazinamide in the clinical centre Banja Luka. Int J Clin Pharmacy. 2012;34:792–793. [Google Scholar]
- 24.Hafkin J, Modongo C, Newcomb C et al. Impact of the human immunodeficiency virus on early multidrug-resistant tuberculosis treatment outcomes in Botswana. Int J Tuberc Lung Dis. 2013;17:348–353. doi: 10.5588/ijtld.12.0100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Araujo-Filho J A, Vasconcelos A C, Jr, Sousa E M et al. Extensively drug-resistant tuberculosis: a case report and literature review. Brazilian J Infect Dis. 2008;12:447–452. doi: 10.1590/s1413-86702008000500019. [DOI] [PubMed] [Google Scholar]
- 26.Valcheva V, Mokrousov I, Narvskaya O, Rastogi N, Markova N. Molecular snapshot of drug-resistant and drug-susceptible Mycobacterium tuberculosis strains circulating in Bulgaria. Infect Genet Evol. 2008;8:657–663. doi: 10.1016/j.meegid.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 27.Yordanova S, Bachiyska E, Atanasova Y, Todorova Y, Baikova A, Kantardjiev T. Multidrug-resistant tuberculosis in Bulgaria: microbiological aspects. Problems Infectious Parasitic Dis. 2013;41:5–8. [Google Scholar]
- 28.Saleri N, Badoum G, Ouedraogo M et al. Extensively drug-resistant tuberculosis, Burkina Faso. Emerg Infect Dis. 2010;16:840–842. doi: 10.3201/eid1605.091262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Diande S, Sangare L, Kouanda S et al. Risk factors for multidrug-resistant tuberculosis in four centers in Burkina Faso, West Africa. Microb Drug Resist. 2009;15:217–221. doi: 10.1089/mdr.2009.0906. [DOI] [PubMed] [Google Scholar]
- 30.Khann S, Mao E T, Rajendra Y P, Satyanarayana S, Nagaraja S B, Kumar A M. Linkage of presumptive multidrug resistant tuberculosis (MDR-TB) patients to diagnostic and treatment services in Cambodia. PLOS ONE. 2013;8:e59903. doi: 10.1371/journal.pone.0059903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sidze L K, Mouafo Tekwu E, Kuaban C et al. Strong decrease in streptomycin-resistance and absence of XDR 12 years after the reorganization of the National Tuberculosis Control Program in the central region of Cameroon. PLOS ONE. 2014;9:e98374. doi: 10.1371/journal.pone.0098374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Minion J, Gallant V, Wolfe J, Jamieson F, Long R. Multidrug and extensively drug-resistant tuberculosis in Canada 1997–2008: demographic disease characteristics. PLOS ONE. 2013;8:e53466. doi: 10.1371/journal.pone.0053466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Garin B, Glaziou P, Kassa-Kelembho E, Yassibanda S, Mbelesso P, Morvan J. High mortality rates among patients with tuberculosis in Bangui, Central African Republic. Lancet. 1997;350:1298. doi: 10.1016/S0140-6736(05)62475-0. [DOI] [PubMed] [Google Scholar]
- 34.Abdelhadi O, Ndokain J, Ali M M, Friocourt V, Mortier E, Heym B. [Drug resistance testing of Mycobacterium tuberculosis isolates from sputum in Chad] Bull Soc Pathol Exot. 2012;105:16–22. doi: 10.1007/s13149-011-0186-9. [French] [DOI] [PubMed] [Google Scholar]
- 35.Yáñez del V. Á. Tuberculosis en inmigrantes: situación Chile-Peru. Rev Chil Enf Respir. 2010;26:161–164. [Spanish] [Google Scholar]
- 36.Tang S, Tan S, Yao L et al. Risk factors for poor treatment outcomes in patients with MDR-TB and XDR-TB in China: retrospective multi-center investigation. PLOS ONE. 2013;8:e82943. doi: 10.1371/journal.pone.0082943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu C H, Li L, Chen Z et al. Characteristics and treatment outcomes of patients with MDR and XDR tuberculosis in a TB referral hospital in Beijing: a 13-year experience. PLOS ONE. 2011;6:e19399. doi: 10.1371/journal.pone.0019399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Leung E C, Leung C C, Kam K M et al. Transmission of multidrug-resistant and extensively drug-resistant tuberculosis in a metropolitan city. Eur Respir J. 2013;41:901–908. doi: 10.1183/09031936.00071212. [DOI] [PubMed] [Google Scholar]
- 39.Cheong S V, Lao U L. [Epidemiological survey on the trend of drug resistance of Mycobacterium tuberculosis complex in Macao during 2001 to 2005] Zhonghua Jie He He Hu Xi Za Zhi. 2007;30:411–414. [Chinese] [PubMed] [Google Scholar]
- 40.Villegas S L, Ferro B E, Perez-Velez C M et al. High initial multidrug-resistant tuberculosis rate in Buenaventura, Colombia: a public-private initiative. Eur Respir J. 2012;40:1569–1572. doi: 10.1183/09031936.00018212. [DOI] [PubMed] [Google Scholar]
- 41.Nieto L M, Ferro B E, Villegas S L et al. Characterization of extensively drug-resistant tuberculosis cases from Valle del Cauca, Colombia. J Clin Microbiol. 2012;50:4185–4187. doi: 10.1128/JCM.01946-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ahui B J, Horo K, Bakayoko A S et al. [Evaluation of multidrug-resistant tuberculosis treatment in Ivory Coast from 2008 to 2010] Rev Pneumol Clin. 2013;69:315–319. doi: 10.1016/j.pneumo.2013.08.002. [French] [DOI] [PubMed] [Google Scholar]
- 43.Suarez-Mendez R, Garia-Garcia I, Fernandez-Olivera N et al. Adjuvant interferon-gamma in patients with drug-resistant pulmonary tuberculosis: a pilot study. BMC Infect Dis. 2004;4:44. doi: 10.1186/1471-2334-4-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lemus D, Echemendía M, Díaz R, Llop A, Llanes M J. Vigilancia de la resistencia a los medicamentos antituberculosos en Cuba, 2010–2011. Biomédica. 2014;34:108–113. doi: 10.1590/S0120-41572014000500013. [Spanish] [DOI] [PubMed] [Google Scholar]
- 45.Bartu V, Kopecka E, Havelkova M. Factors associated with multidrug-resistant tuberculosis: comparison of patients born inside and outside of the Czech Republic. J Int Med Res. 2010;38:1156–1163. doi: 10.1177/147323001003800345. [DOI] [PubMed] [Google Scholar]
- 46.Seung K J, Linton S W. The growing problem of multidrug-resistant tuberculosis in North Korea. PLOS MED. 2013;10:e1001486. doi: 10.1371/journal.pmed.1001486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kim H-R, Hwang S S, Kim H J et al. Impact of extensive drug resistance on treatment outcomes in non-HIV-infected patients with multidrug-resistant tuberculosis. Clin Infect Dis. 2007;45:1290–1295. doi: 10.1086/522537. [DOI] [PubMed] [Google Scholar]
- 48.Kaswa M K, Bisuta S, Kabuya G et al. Multidrug-resistant tuberculosis in Mosango, a rural area in the Democratic Republic of Congo. PLOS ONE. 2014;9:e94618. doi: 10.1371/journal.pone.0094618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Boyer-Cazajous G, Martinaud C, Dehan C et al. High prevalence of multi-drug resistant tuberculosis in Djibouti: a retrospective study. J Infect Dev Ctries. 2014;8:233–236. doi: 10.3855/jidc.3837. [DOI] [PubMed] [Google Scholar]
- 50.Rouzier V A, Oxlade O, Verduga R, Gresely L, Menzies D. Patient and family costs associated with tuberculosis, including multidrug-resistant tuberculosis, in Ecuador. Int J Tuberc Lung Dis. 2010;14:1316–1322. [PubMed] [Google Scholar]
- 51.Rasslan O, Hafez S F, Hashem M et al. Microscopic observation drug susceptibility assay in the diagnosis of multidrug-resistant tuberculosis. Int J Tuberc Lung Dis. 2012;16:941–946. doi: 10.5588/ijtld.11.0547. [DOI] [PubMed] [Google Scholar]
- 52.Hafez S A, Elhefnawy A M, Hatata E A, El Ganady A A, Ibrahiem M I. Detection of extensively drug resistant pulmonary tuberculosis. Egyptian J Chest Dis Tuberc. 2013;62:635–646. [Google Scholar]
- 53.Aguilar R, Garay J, Villatoro M et al. Results of a national study on anti-mycobacterial drug resistance in El Salvador. Int J Tuberc Lung Dis. 2005;9:514–520. [PubMed] [Google Scholar]
- 54.Blondal K, Rahu K, Altraja A, Viiklepp P, Rahu M. Overall and cause-specific mortality among patients with tuberculosis and multidrug-resistant tuberculosis. Int J Tuberc Lung Dis. 2013;17:961–968. doi: 10.5588/ijtld.12.0946. [DOI] [PubMed] [Google Scholar]
- 55.Blondal K, Viiklepp P, Guethmundsson L J, Altraja A. Predictors of recurrence of multidrug-resistant and extensively drug-resistant tuberculosis. Int J Tuberc Lung Dis. 2012;16:1228–1233. doi: 10.5588/ijtld.12.0037. [DOI] [PubMed] [Google Scholar]
- 56.Abate D, Taye B, Abseno M, Biadgilign S. Epidemiology of antituberculosis drug resistance patterns and trends in tuberculosis referral hospital in Addis Ababa, Ethiopia. BMC Res Notes. 2012;5:462. doi: 10.1186/1756-0500-5-462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Vasankari T, Soini H, Liippo K, Ruutu P. MDR-TB in Finland: still rare despite the situation in our neighbouring countries. Clin Respir J. 2012;6:35–39. doi: 10.1111/j.1752-699X.2011.00242.x. [DOI] [PubMed] [Google Scholar]
- 58.National Institute for Health and Welfare. Infectious diseases in Finland 2011. Helsinki, Finland: NIHW; 2012. [Google Scholar]
- 59.Bernard C, Brossier F, Sougakoff W et al. A surge of MDR and XDR tuberculosis in France among patients born in the Former Soviet Union. Euro Surveill. 2013;18:20555. doi: 10.2807/1560-7917.es2013.18.33.20555. [DOI] [PubMed] [Google Scholar]
- 60.Chauny J V, Lorrot M, Prot-Labarthe S et al. Treatment of tuberculosis with levofloxacin or moxifloxacin: report of 6 pediatric cases. Pediatr Infect Dis J. 2012;31:1309–1311. doi: 10.1097/INF.0b013e318269cc6a. [DOI] [PubMed] [Google Scholar]
- 61.Haustraete E, Campbell K, Magnier R, Zalcman G, Bergot E. [Interest of collapse therapy in pulmonary extensively drug-resistant tuberculosis.] Rev Pneumol Clin. 2014;70:240–244. doi: 10.1016/j.pneumo.2013.08.007. [French] [DOI] [PubMed] [Google Scholar]
- 62.Adegbola R A, Hill P, Baldeh I et al. Surveillance of drug-resistant Mycobacterium tuberculosis in The Gambia. Int J Tuberc Lung Dis. 2003;7:390–393. [PubMed] [Google Scholar]
- 63.Vashakidze S, Gogishvili S, Nikolaishvili K et al. Favorable outcomes for multidrug and extensively drug resistant tuberculosis patients undergoing surgery. Ann Thoracic Surg. 2013;95:1892–1898. doi: 10.1016/j.athoracsur.2013.03.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gegia M, Jenkins H E, Kalandadze I, Furin J. Outcomes of children treated for tuberculosis with second-line medications in Georgia, 2009–2011. Int J Tuberc Lung Dis. 2013;17:624–629. doi: 10.5588/ijtld.12.0792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Eker B, Ortmann J, Migliori G B et al. Multidrug- and extensively drug-resistant tuberculosis, Germany. Emerg Infect Dis. 2008;14:1700–1706. doi: 10.3201/eid1411.080729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kato T, Addo K K, Nartey N, Nyarko A K, Bonsu F A, Mitarai S. First susceptibility testing of Mycobacterium tuberculosis for second-line antituberculosis drugs in Ghana. Trop Med Health. 2014;42:53–55. doi: 10.2149/tmh.2013-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Syridou G, Mavrikou M, Amanatidou V et al. Trends in the epidemiology of childhood tuberculosis in Greece. Int J Tuberc Lung Dis. 2012;16:749–755. doi: 10.5588/ijtld.10.0717. [DOI] [PubMed] [Google Scholar]
- 68.Leuow K, Papaventsis D, Kourkoundi S et al. Fatal case of extensively drug-resistant Mycobacterium tuberculosis Beijing genotype infection in an injecting drug user, Athens, Greece, 2012. Euro Surveill. 2013;18:20430. [PubMed] [Google Scholar]
- 69.Katragkou A, Antachopoulos C, Hatziagorou E, Sdougka M, Roilides E, Tsanakas J. Drug-resistant tuberculosis in two children in Greece: report of the first extensively drug-resistant case. Eur J Pediatr. 2013;172:563–567. doi: 10.1007/s00431-012-1811-8. [DOI] [PubMed] [Google Scholar]
- 70.Harrow E M, Rangel J M, Arriega J M et al. Epidemiology and clinical consequences of drug-resistant tuberculosis in a Guatemalan hospital. Chest. 1998;113:1452–1458. doi: 10.1378/chest.113.6.1452. [DOI] [PubMed] [Google Scholar]
- 71.Bah H, Cisse F A, Camara L M, Diallo O H, Diallo M, Sow O Y. [Prevalence of tuberculosis in the prison population of Conakry, Guinea Republic.] Rev Med Légale. 2012;3:146–150. [French] [Google Scholar]
- 72.Menner N, Gunther I, Orawa H et al. High frequency of multidrug-resistant Mycobacterium tuberculosis isolates in Georgetown, Guyana. Trop Med Int Health. 2005;10:1215–1218. doi: 10.1111/j.1365-3156.2005.01521.x. [DOI] [PubMed] [Google Scholar]
- 73.Pineda-Garcia L, Ferrera A, Galvez C A, Hoffner S E. Drug-resistant Mycobacterium tuberculosis and atypical mycobacteria isolated from patients with suspected pulmonary tuberculosis in Honduras. Chest. 1997;111:148–153. doi: 10.1378/chest.111.1.148. [DOI] [PubMed] [Google Scholar]
- 74.Kodmon C, Niemann S, Lukacs J, Sor E, David S, Somoskovi A. Molecular epidemiology of drug-resistant tuberculosis in Hungary. J Clin Microbiol. 2006;44:4258–4261. doi: 10.1128/JCM.01254-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Asgeirsson H, Blondal K, Blondal T, Gottfredsson M. [Multidrug-resistant tuberculosis in Iceland: case series and review of the literature] Laeknabladid. 2009;95:499–507. [Icelandic] [PubMed] [Google Scholar]
- 76.Salvo F, Dorjee K, Dierberg K et al. Survey of tuberculosis drug resistance among Tibetan refugees in India. Int J Tuberc Lung Dis. 2014;18:655–662. doi: 10.5588/ijtld.13.0516. [DOI] [PubMed] [Google Scholar]
- 77.Kulkarni K, Singh M, Soneja P, Mathew J, Marwaha R K. Extensively drug resistant tuberculosis in a 7-year-old child with interferon-gamma and interleukin-12 deficiency. BMJ Case Rep. 2009;2009 doi: 10.1136/bcr.06.2008.0293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Putri F A, Burhan E, Nawas A et al. Body mass index predictive of sputum culture conversion among MDR-TB patients in Indonesia. Int J Tuberc Lung Dis. 2014;18:564–570. doi: 10.5588/ijtld.13.0602. [DOI] [PubMed] [Google Scholar]
- 79.Masjedi M R, Tabarsi P, Baghaei P et al. Extensively drug-resistant tuberculosis treatment outcome in Iran: a case series of seven patients. Int J Infect Dis. 2010;14:e399–402. doi: 10.1016/j.ijid.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 80.Ahmed M, Mohammed S, Nasurallah H. Mutation in katG315 is, possibly, a good prognostic marker for treatment with second-line drugs in multi-drug resistant tuberculosis: A preliminary study. Indian J Med Microbiol. 2013;31:394–400. doi: 10.4103/0255-0857.118899. [DOI] [PubMed] [Google Scholar]
- 81.Bradshaw L, Davies E, Devine M et al. The role of the interferon gamma release assay in assessing recent tuberculosis transmission in a hospital incident. PLOS ONE. 2011;6:e20770. doi: 10.1371/journal.pone.0020770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kennedy B, Lyons O, McLoughlin A M, Gibbons N, O’Flanagan D, Keane J. Extensively drug-resistant tuberculosis: first report of a case in Ireland. Euro Surveill. 2008;13:18935. [PubMed] [Google Scholar]
- 83.Papiashvili M, Barmd I, Sasson L et al. Pulmonary resection for multi-drug-resistant tuberculosis: the Israeli experience (1998–2011) Israel Med Assoc J. 2012;14:733–736. [PubMed] [Google Scholar]
- 84.Mor Z, Cedar N, Pinsker G, Bibi H, Grotto I. Childhood tuberculosis in Israel: epidemiological trends and treatment outcomes, 1999–2010. Eur Respir J. 2013;41:1157–1162. doi: 10.1183/09031936.00033912. [DOI] [PubMed] [Google Scholar]
- 85.Bendayan D, Hendler A, Polansky V, Weinberger M. Outcome of hospitalized MDR-TB patients: Israel 2000–2005. Eur J Clin Microbiol Infect Dis. 2011;30:375–379. doi: 10.1007/s10096-010-1096-7. [DOI] [PubMed] [Google Scholar]
- 86.Fattorini L, Mustazzolu A, Piccaro G et al. Drug-resistant tuberculosis among foreign-born persons in Italy. Eur Respir J. 2012;40:497–500. doi: 10.1183/09031936.00021012. [DOI] [PubMed] [Google Scholar]
- 87.Migliori G B, De Iaco G, Besozzi G, Centis R, Cirillo D M. First tuberculosis cases in Italy resistant to all tested drugs. Euro Surveill. 2007;12:E070517.1. doi: 10.2807/esw.12.20.03194-en. [DOI] [PubMed] [Google Scholar]
- 88.Sasaki Y, Yamagishi F, Yagi T. [Current situation of contacts examination and chemoprophylaxis for persons exposed to multidrug-resistant tuberculosis in ordinance designated cities in Japan] Kekkaku. 2005;80:637–642. [Japanese] [PubMed] [Google Scholar]
- 89.Shiraishi Y, Katsuragi N, Kita H, Toishi M, Onda T. Experience with pulmonary resection for extensively drug-resistant tuberculosis. Interact Cardiovasc Thorac Surg. 2008;7:1075–1078. doi: 10.1510/icvts.2008.185124. [DOI] [PubMed] [Google Scholar]
- 90.Nimri L, Samara H, Batchoun R. Detection of mutations associated with multidrug-resistant Mycobacterium tuberculosis clinical isolates. FEMS Immunol Med Microbiol. 2011;62:321–327. doi: 10.1111/j.1574-695X.2011.00814.x. [DOI] [PubMed] [Google Scholar]
- 91.Maimakov T, Sadykova L, Kalmataeva Z, Kurakpaev K, Smigelskas K. Treatment of tuberculosis in South Kazakhstan: clinical and economical aspects. Medicina (Kaunas, Lithuania) 2013;49:335–340. [PubMed] [Google Scholar]
- 92.Ndung’u P W, Kariuki S, Ng’ang’a Z, Revathi G. Resistance patterns of Mycobacterium tuberculosis isolates from pulmonary tuberculosis patients in Nairobi. J Infect Dev Ctries. 2012;6:33–39. doi: 10.3855/jidc.2281. [DOI] [PubMed] [Google Scholar]
- 93.Al-Mutairi N M, Ahmad S, Mokaddas E. First report of molecular detection of fluoroquinolone resistance-associated gyrA mutations in multidrug-resistant clinical Mycobacterium tuberculosis isolates in Kuwait. BMC Res Notes. 2011;4:123. doi: 10.1186/1756-0500-4-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Mokrousov I, Isakova J, Valcheva V, Aldashev A, Rastogi N. Molecular snapshot of Mycobacterium tuberculosis population structure and drug-resistance in Kyrgyzstan. Tuberculosis (Edinburgh, Scotland) 2013;93:501–507. doi: 10.1016/j.tube.2013.05.008. [DOI] [PubMed] [Google Scholar]
- 95.Iem V, Somphavong S, Buisson Y et al. Resistance of Mycobacterium tuberculosis to antibiotics in Lao PDR: first multicentric study conducted in 3 hospitals. BMC Infect Dis. 2013;13:275. doi: 10.1186/1471-2334-13-275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Miller T L, Cirule A, Wilson F A et al. The value of effective public tuberculosis treatment: an analysis of opportunity costs associated with multidrug resistant tuberculosis in Latvia. Cost Eff Resour Alloc. 2013;11:9. doi: 10.1186/1478-7547-11-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Leimane V, Dravniece G, Riekstina V et al. Treatment outcome of multi-drug/extensively drug-resistant tuberculosis in Latvia, 2000–2004. Eur Respir J. 2010;36:584–593. doi: 10.1183/09031936.00003710. [DOI] [PubMed] [Google Scholar]
- 98.Satti H, McLaughlin M M, Seung K J. Drug-resistant tuberculosis treatment complicated by antiretroviral resistance in HIV coinfected patients: a report of six cases in Lesotho. Am J Trop Med Hyg. 2013;89:174–177. doi: 10.4269/ajtmh.13-0046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Satti H, McLaughlin M M, Omotayo D B et al. Outcomes of comprehensive care for children empirically treated for multidrug-resistant tuberculosis in a setting of high HIV prevalence. PLOS ONE. 2012;7:e37114. doi: 10.1371/journal.pone.0037114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Satti H, Seung K, Keshavjee S, Furin J. Extensively drug-resistant tuberculosis, Lesotho. Emerg Infect Dis. 2008;14:992–993. doi: 10.3201/eid1406.071654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Balabanova Y, Radiulyte B, Davidaviciene E et al. Risk factors for drug-resistant tuberculosis patients in Lithuania, 2002–2008. Eur Respir J. 2012;39:1266–1269. doi: 10.1183/09031936.00133911. [DOI] [PubMed] [Google Scholar]
- 102.Vorkas C, Kayira D, van der Horst C et al. Tuberculosis drug resistance and outcomes among tuberculosis inpatients in Lilongwe, Malawi. Malawi Med J. 2012;24:21–24. [PMC free article] [PubMed] [Google Scholar]
- 103.Traore B, Diarra B, Dembele B P et al. Molecular strain typing of Mycobacterium tuberculosis complex in Bamako, Mali. Int J Tuberc Lung Dis. 2012;16:911–916. doi: 10.5588/ijtld.11.0397. [DOI] [PubMed] [Google Scholar]
- 104.Powell K, Briand K, Pavlin B, Bamrah S. Emergence of multidrug-resistant tuberculosis in the republic of the Marshall Islands, 2004–2010. Am J Respir Crit Care Med. 2011;183:A1823. [Google Scholar]
- 105.Gonzalez D, Mase S, Jereb J et al. Population pharmacokinetics of levoflox-acin in children treated for, or exposed to, multidrug resistant tuberculosis in the federated states of Micronesia and Republic of Marshall Islands. J Pharmacokinet Pharmacodyn. 2013;40:S47–S48. [Google Scholar]
- 106.Brostrom R, Fred D, Heetderks A et al. Islands of hope: building local capacity to manage an outbreak of multidrug-resistant tuberculosis in the Pacific. Am J Public Health. 2011;101:14–18. doi: 10.2105/AJPH.2009.177170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Two simultaneous outbreaks of multidrug-resistant tuberculosis—Federated States of Micronesia, 2007–2009. MMWR Morb Mortal Wkly Rep. 2009;58:253–256. [PubMed] [Google Scholar]
- 108.Pires G M, Folgosa E, Nquobile N, Gitta S, Cadir N. Mycobacterium tuberculosis resistance to antituberculosis drugs in Mozambique. J Bras Pneumol. 2014;40:142–147. doi: 10.1590/S1806-37132014000200007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Aung W W, Ti T, Than K K et al. Study of drug resistant cases among new pulmonary tuberculosis patients attending a tuberculosis center, Yangon, Myanmar. Southeast Asian J Trop Med Public Health. 2007;38:104–110. [PubMed] [Google Scholar]
- 110.Ricks P M, Mavhunga F, Modi S et al. Characteristics of multidrug-resistant tuberculosis in Namibia. BMC Infect Dis. 2012;12:385. doi: 10.1186/1471-2334-12-385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Malla P, Kanitz E E, Akhtar M et al. Ambulatory-based standardized therapy for multidrug-resistant tuberculosis: experience from Nepal, 2005–2006. PLOS ONE. 2009;4:e8313. doi: 10.1371/journal.pone.0008313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Yoshiyama T, Shrestha B, Maharjan B. Risk of relapse and failure after retreatment with the Category II regimen in Nepal. Int J Tuberc Lung Dis. 2010;14:1418–1423. [PubMed] [Google Scholar]
- 113.Poudel A, Maharjan B, Nakajima C et al. Characterization of extensively drug-resistant Mycobacterium tuberculosis in Nepal. Tuberculosis (Edinburgh, Scotland) 2013;93:84–88. doi: 10.1016/j.tube.2012.10.007. [DOI] [PubMed] [Google Scholar]
- 114.van Ingen J, Boeree M J, Wright A, van der Laan T, Dekhuijzen P N, van Soolingen D. Second-line drug resistance in multidrug-resistant tuberculosis cases of various origins in the Netherlands. Int J Tuberc Lung Dis. 2008;12:1295–1299. [PubMed] [Google Scholar]
- 115.Goh T L, Towns C R, Jones K L, Freeman J T, Wong C S. Extensively drug-resistant tuberculosis: New Zealand’s first case and the challenges of management in a low-prevalence country. Medical J Austr. 2011;194:602–604. doi: 10.5694/j.1326-5377.2011.tb03115.x. [DOI] [PubMed] [Google Scholar]
- 116.Chacon L, Lainez M, Rosales E, Mercado M, Caminero JA. Evolution in the resistance of Mycobacterium tuberculosis to antituberculosis drugs in Nicaragua. Int J Tuberc Lung Dis. 2009;13:62–67. [PubMed] [Google Scholar]
- 117.Oladimeji O, Isaakidis P, Obasanya O J et al. Intensive-phase treatment outcomes among hospitalized multidrug-resistant tuberculosis patients: results from a nationwide cohort in Nigeria. PLOS ONE. 2014;9:e94393. doi: 10.1371/journal.pone.0094393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Nwokeukwu H I, Okafor P N, Okorie O, Ukpabi I K. Paediatric multidrug-resistant tuberculosis with HIV coinfection: a case report. Case Rep Med. 2013;2013:756152. doi: 10.1155/2013/756152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.von der Lippe B, Sandven P, Brubakk O. Efficacy and safety of linezolid in multidrug resistant tuberculosis (MDR-TB): a report of ten cases. J Infect. 2006;52:92–96. doi: 10.1016/j.jinf.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 120.Mohammadi A, Nassor Z S, Behlim T et al. Epidemiological and cost analysis of multidrug-resistant tuberculosis in Oman. Eastern Mediterranean Health J. 2008;14:1240–1245. [PubMed] [Google Scholar]
- 121.Ali A, Hasan R, Jabeen K, Jabeen N, Qadeer E, Hasan Z. Characterization of mutations conferring extensive drug resistance to Mycobacterium tuberculosis isolates in Pakistan. Antimicrob Agents Chemother. 2011;55:5654–5659. doi: 10.1128/AAC.05101-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Lanzas F, Karakousis P C, Sacchettini J C, Ioerger T R. Multidrug-resistant tuberculosis in panama is driven by clonal expansion of a multidrug-resistant Mycobacterium tuberculosis strain related to the KZN extensively drug-resistant M. tuberculosis strain from South Africa. J Clin Microbiol. 2013;51:3277–3285. doi: 10.1128/JCM.01122-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Ballif M, Harino P, Ley S et al. Genetic diversity of Mycobacterium tuberculosis in Madang, Papua New Guinea. Int J Tuberc Lung Dis. 2012;16:1100–1107. doi: 10.5588/ijtld.11.0779. [DOI] [PubMed] [Google Scholar]
- 124.McIver L J, Parish S T, Jones S P, Kippin A N, Furlong T J. Acute glomerulo-nephritis in a child with multidrug-resistant tuberculosis and multibacillary leprosy. Med J Austr. 2011;195:150–152. doi: 10.5694/j.1326-5377.2011.tb03245.x. [DOI] [PubMed] [Google Scholar]
- 125.Kirby T. Extensively drug-resistant tuberculosis hovers threateningly at Australia’s door. Med J Austr. 2013;198:1–2. doi: 10.5694/mja13.10178. [DOI] [PubMed] [Google Scholar]
- 126.Candia N, Lopez B, Zozio T et al. First insight into Mycobacterium tuberculosis genetic diversity in Paraguay. BMC Microbiol. 2007;7:75. doi: 10.1186/1471-2180-7-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Institute of Medicine of the National Academies & Russian Academy of Medical Sciences. The new profile of drug-resistant tuberculosis in Russia: a global and local perspective: summary of a joint workshop. Washington, DC, USA: National Academies Press; 2011. [PubMed] [Google Scholar]
- 128.Becerra M C, Appleton S C, Franke M F et al. Tuberculosis burden in households of patients with multidrug-resistant and extensively drug-resistant tuberculosis: a retrospective cohort study. Lancet. 2011;377:147–152. doi: 10.1016/S0140-6736(10)61972-1. [DOI] [PubMed] [Google Scholar]
- 129.Del Castillo H, Mendoza-Ticona A, Saravia J C, Somocurcio J G. Epidemia de tuberculosis multidrogo resistente y extensivamente resistente a drogas (TB MDR/XDR) en el Peru: situacion u propuestas para su control. Rev Peru Med Exp Salud Publica. 2009;26:380–386. [Google Scholar]
- 130.Gler M T, Guilatco R, Caoili J C, Ershova J, Cegielski P, Johnson J L. Weight gain and response to treatment for multidrug-resistant tuberculosis. Am J Trop Med Hyg. 2013;89:943–949. doi: 10.4269/ajtmh.13-0011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Gler M T, Podewils L J, Munez N, Galipot M, Quelapio M I, Tupasi T E. Impact of patient and program factors on default during treatment of multi-drug-resistant tuberculosis. Int J Tuberc Lung Dis. 2012;16:955–960. doi: 10.5588/ijtld.11.0502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Kozinska M, Brzostek A, Krawiecka D, Rybczynska M, Zwolska Z, Augustynowicz-Kopec E. [MDR, pre-XDR and XDR drug-resistant tuberculosis in Poland in 2000–2009] Pneumonologia i Alergologia Polska. 2011;79:278–287. [Polish] [PubMed] [Google Scholar]
- 133.Oliveira O, Gaio R, Villar M, Duarte R. Predictors of treatment outcome in multidrug-resistant tuberculosis in Portugal. Eur Respir J. 2013;42:1747–1749. doi: 10.1183/09031936.00197912. [DOI] [PubMed] [Google Scholar]
- 134.Villar M, Sotgiu G, D’Ambrosio L et al. Linezolid safety, tolerability and efficacy to treat multidrug- And extensively drug-resistant tuberculosis. Eur Respir J. 2011;38:730–733. doi: 10.1183/09031936.00195210. [DOI] [PubMed] [Google Scholar]
- 135.Kjöllerström P, Brito M J, Gouveia C, Ferreira G, Varandas L. Linezolid in the treatment of multidrug-resistant/extensively drug-resistant tuberculosis in paediatric patients: experience of a paediatric infectious diseases unit. Scand J Infect Dis. 2011;43:556–559. doi: 10.3109/00365548.2011.564649. [DOI] [PubMed] [Google Scholar]
- 136.Jo K W, Lee S D, Kim W S, Kim D S, Shim T S. Treatment outcomes and moxifloxacin susceptibility in ofloxacin-resistant multidrug-resistant tuberculosis. Int J Tuberc Lung Dis. 2014;18:39–43. doi: 10.5588/ijtld.13.0307. [DOI] [PubMed] [Google Scholar]
- 137.Kim D H, Kim H J, Park S K et al. Treatment outcomes and survival based on drug resistance patterns in multidrug-resistant tuberculosis. Am J Respir Crit Care Med. 2010;182:113–119. doi: 10.1164/rccm.200911-1656OC. [DOI] [PubMed] [Google Scholar]
- 138.Rugina S, Dumitru I M, Resul G, Cernat R C, Petcu A E. Disseminated tuberculosis in HIV-infected patients from the Regional HIV/AIDS Center Constanta, Romania. Germs. 2014;4:16–21. doi: 10.11599/germs.2014.1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Brinza N, Mihaescu T. [Difficulties in the treatment of pulmonary tuberculosis in children] Rev Med Chir Soc Med Nat Iasi. 2007;111:852–855. [Romanian] [PubMed] [Google Scholar]
- 140.Lunca C, Dorneanu O S, Diculencu D et al. Molecular detection of rifampicin resistance in multidrug-resistant Mycobacterium tuberculosis strains from North-Eastern Romania. Romanian Rev Labor Med. 2013;21:293–299. [Google Scholar]
- 141.Kontsevaya I, Ignatyeva O, Nikolayevskyy V et al. Diagnostic accuracy of the genotype MTBDRsl assay for rapid diagnosis of extensively drug-resistant tuberculosis in HIV-coinfected patients. J Clin Microbiol. 2013;51:243–248. doi: 10.1128/JCM.02513-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Panova L V, Ovsiankina E S, Stakheeva l B. [The epidemic drug-resistant tuberculosis situation among the children and adolescents of Moscow] Problemy Tuberkuleza i Boleznei Legkikh. 2006:21–22. [Russian] [PubMed] [Google Scholar]
- 143.Umubyeyi A, Rigouts L, Shamputa I C, Dediste A, Struelens M, Portaels F. Low levels of second-line drug resistance among multidrug-resistant Mycobacterium tuberculosis isolates from Rwanda. Int J Infect Dis. 2008;12:152–156. doi: 10.1016/j.ijid.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 144.Levin R. Lessons from Rwanda. Minn Med. 2007;90:32–35. [PubMed] [Google Scholar]
- 145.Chevalier B, Margery J, Sane M et al. [Epidemiology of the resistance of Mycobacterium tuberculosis to antituberculosis drugs at the main hospital in Dakar, Senegal. A 4-year retrospective study (2000–2003)] Rev Pneumol Clin. 2010;66:266–271. doi: 10.1016/j.pneumo.2010.07.001. [French] [DOI] [PubMed] [Google Scholar]
- 146.Vukovic D, Rüsch-Gerdes S, Savic B, Niemann S. Molecular epidemiology of pulmonary tuberculosis in Belgrade, Central Serbia. J Clin Microbiol. 2003;41:4372–4377. doi: 10.1128/JCM.41.9.4372-4377.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Živanović I, Vukovi D, Davić I, Stefanović G, Savić B. Detection of drug-resistant mycobacterium tuberculosis strains isolated in Servia by the genotype MTBDRSL assay. Arch Biol Sci. 2012;64:1311–1318. [Google Scholar]
- 148.Gibson J. Drug-resistant tuberculosis in Sierra Leone. Tubercle. 1986;67:119–124. doi: 10.1016/0041-3879(86)90005-x. [DOI] [PubMed] [Google Scholar]
- 149.Falzon D, Infuso A, Ait-Belghiti F. In the European Union, TB patients from former Soviet countries have a high risk of multidrug resistance. Int J Tuberc Lung Dis. 2006;10:954–958. [PubMed] [Google Scholar]
- 150.Cox H, Hughes J, Daniels J et al. Community-based treatment of drug-resistant tuberculosis in Khayelitsha, South Africa. Int J Tuberc Lung Dis. 2014;18:441–448. doi: 10.5588/ijtld.13.0742. [DOI] [PubMed] [Google Scholar]
- 151.Padayatchi N, Gopal M, Naidoo R et al. Clofazimine in the treatment of extensively drug-resistant tuberculosis with HIV coinfection in South Africa: a retrospective cohort study. J Antimicrob Chemother. 2014 doi: 10.1093/jac/dku235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Thomas T A, Shenoi S V, Heysell S K et al. Extensively drug-resistant tuberculosis in children with human immunodeficiency virus in rural South Africa. Int J Tuberc Lung Dis. 2010;14:1244–1251. [PMC free article] [PubMed] [Google Scholar]
- 153.Ramirez Lapausa M, Pascual Pareja J F, Amer Lopez M, Vidal Perez J L, Noguerado Asensio A. [Outcome and treatment among patients with multi-drug-resistant tuberculosis] Medicina Clinica. 2012;138:643–649. doi: 10.1016/j.medcli.2011.10.029. [Spanish] [DOI] [PubMed] [Google Scholar]
- 154.Senaratne W V. Outcome of treatment of multidrug resistant tuberculosis. The Ceylon Med J. 2004;49:86–87. doi: 10.4038/cmj.v49i3.3246. [DOI] [PubMed] [Google Scholar]
- 155.Sharaf Eldin G S, Fadl-Elmula I, Ali M S et al. Tuberculosis in Sudan: a study of Mycobacterium tuberculosis strain genotype and susceptibility to antituberculosis drugs. BMC Infect Dis. 2011;11:219. doi: 10.1186/1471-2334-11-219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Sanchez-Padilla E, Dlamini T, Ascorra A et al. High prevalence of multi-drug-resistant tuberculosis, Swaziland, 2009–2010. Emerg Infect Dis. 2012;18:29–37. doi: 10.3201/eid1801.110850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Ghebremichael S, Petersson R, Koivula T et al. Molecular epidemiology of drug-resistant tuberculosis in Sweden. Microbes Infect. 2008;10:699–705. doi: 10.1016/j.micinf.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 158.Somoskovi A, Helbling P, Deggim V, Homke R, Ritter C, Bottger E C. Transmission of multidrug-resistant tuberculosis in a low-incidence setting, Switzerland, 2006 to 2012. Euro Surveill. 2014;19:20736. doi: 10.2807/1560-7917.es2014.19.11.20736. [DOI] [PubMed] [Google Scholar]
- 159.Rahmo A H, Hamze M. Characterization of Mycobacterium tuberculosis in Syrian patients by double-repetitive-element polymerase chain reaction. East Mediterr Health J. 2010;16:820–830. [PubMed] [Google Scholar]
- 160.Gibb C. Treating TB in Tajikistan. Nurs N Z. 2012;18:31. [PubMed] [Google Scholar]
- 161.Reechaipichitkul W, Tubtim S, Chaimanee P. Drug susceptibility patterns of Mycobacterium tuberculosis and clinical outcomes of drug-resistant tuberculosis at Srinagarind Hospital, a tertiary care center in northeastern Thailand. Southeast Asian J Trop Med Public Health. 2011;42:1154–1162. [PubMed] [Google Scholar]
- 162.Kelly P M, Lumb R, Pinto A, da Costa G, Sarmento J, Bastian I. Analysis of Mycobacterium tuberculosis isolates from treatment failure patients living in East Timor. Int J Tuberc Lung Dis. 2005;9:81–86. [PubMed] [Google Scholar]
- 163.Mardassi H, Namouchi A, Haltiti R et al. Tuberculosis due to resistant Haarlem strain, Tunisia. Emerg Infect Dis. 2005;11:957–961. doi: 10.3201/eid1106.041365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Muwonge A, Malama S, Bronsvoort B M, Biffa D, Ssengooba W, Skjerve E. A comparison of tools used for tuberculosis diagnosis in resource-limited settings: a case study at Mubende Referral Hospital, Uganda. PLOS ONE. 2014;9:e100720. doi: 10.1371/journal.pone.0100720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Dymova M A, Liashenko O O, Poteiko P I, Krutko V S, Khrapov E A, Filipenko M L. Genetic variation of Mycobacterium tuberculosis circulating in Kharkiv Oblast, Ukraine. BMC Infect Dis. 2011;11:77. doi: 10.1186/1471-2334-11-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Abubakar I, Moore J, Drobniewski F et al. Extensively drug-resistant tuberculosis in the UK: 1995 to 2007. Thorax. 2009;64:512–515. doi: 10.1136/thx.2008.108712. [DOI] [PubMed] [Google Scholar]
- 167.Al-Zarouni M, Dash N, Al Ali M, Al-Shehhi F, Panigrahi D. Tuberculosis and MDR-TB in the northern emirates of United Arab Emirates: a 5-year study. Southeast Asian J Trop Med Public Health. 2010;41:163–168. [PubMed] [Google Scholar]
- 168.Mpagama S G, Ndusilo N, Stroup S et al. Plasma drug activity in patients on treatment for multidrug-resistant tuberculosis. Antimicrob Agents Chemother. 2014;58:782–788. doi: 10.1128/AAC.01549-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Anger H A, Dworkin F, Sharma S, Munsiff S S, Nilsen D M, Ahuja S D. Linezolid use for treatment of multidrug-resistant and extensively drug-resistant tuberculosis, New York City, 2000–06. J Antimicrobial Chemother. 2010;65:775–783. doi: 10.1093/jac/dkq017. [DOI] [PubMed] [Google Scholar]
- 170.Banerjee R, Allen J, Westenhouse J et al. Extensively drug-resistant tuberculosis in California, 1993–2006. Clin Infect Dis. 2008;47:450–457. doi: 10.1086/590009. [DOI] [PubMed] [Google Scholar]
- 171.Lalor M K, Greig J, Allamuratova S et al. Risk factors associated with default from multi- and extensively drug-resistant tuberculosis treatment, Uzbekistan: a retrospective cohort analysis. PLOS ONE. 2013;8:e78364. doi: 10.1371/journal.pone.0078364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Ritacco V, Iglesias M-J, Ferrazoli L et al. Conspicuous multidrug-resistant Mycobacterium tuberculosis cluster strains do not trespass country borders in Latin America and Spain. Infect Genet Evol. 2012;12:711–717. doi: 10.1016/j.meegid.2011.06.006. [DOI] [PubMed] [Google Scholar]
- 173.Buu T N, Huyen M N, Lan N T N et al. The Beijing genotype is associated with young age and multidrug-resistant tuberculosis in rural Viet Nam. Int J Tuberc Lung Dis. 2009;13:900–906. [PubMed] [Google Scholar]
- 174.Kapata N, Chanda-Kapata P, Bates M et al. Multidrug-resistant TB in Zambia: review of national data from 2000 to 2011. Trop Med Int Health. 2013;18:1386–1391. doi: 10.1111/tmi.12183. [DOI] [PubMed] [Google Scholar]
- 175.Makombe R R, Easterbrook P J, Lowe O et al. Epidemiological features of drug resistant tuberculosis in Harare, 1994 to 1996. Cent Afr J Med. 1999;45:282–287. doi: 10.4314/cajm.v45i11.8500. [DOI] [PubMed] [Google Scholar]
Footnotes
Conflicts of interest: none declared.
References
- 1.Seddon J A, Hesseling A C, Marais B J et al. Paediatric use of second-line antituberculosis agents: a review. Tuberculosis. 2012;92:9–17. doi: 10.1016/j.tube.2011.11.001. [DOI] [PubMed] [Google Scholar]
- 2.Jenkins H E, Tolman A W, Yuen C M et al. Incidence of multidrug-resistant tuberculosis disease in children: systematic review and global estimates. Lancet. 2014;383:1572–1579. doi: 10.1016/S0140-6736(14)60195-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zignol M, Sismanidis C, Falzon D, Glaziou P, Dara M, Floyd K. Multidrug-resistant tuberculosis in children: evidence from global surveillance. Eur Respir J. 2013;42:701–707. doi: 10.1183/09031936.00175812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Country tuberculosis profiles. Geneva, Switzerland: WHO; 2015. https://extranet.who.int/sree/Reports?op=vs&path=/WHO_HQ_Reports/G2/PROD/EXT/MDRTB_Indicators_charts. [Google Scholar]
- 5.Marais B J, Schaaf H S. Childhood tuberculosis: an emerging and previously neglected problem. Infect Dis Clin North Am. 2010;24:727–749. doi: 10.1016/j.idc.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 6.Reubenson G. Pediatric drug-resistant tuberculosis: a global perspective: a global perspective. Paediatr Drugs. 2011;13:349–355. doi: 10.2165/11593160-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 7.Marais B J, Schaaf H S. Childhood tuberculosis: an emerging and previously neglected problem. Infect Dis Clin North Am. 2010;24:727–749. doi: 10.1016/j.idc.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 8.Becerra M C, Swaminathan S. A targets framework: dismantling the invisibility trap for children with drug-resistant tuberculosis. J Public Health Policy. 2014;35:425–454. doi: 10.1057/jphp.2014.35. [DOI] [PubMed] [Google Scholar]
- 9.Ettehad D, Schaaf H S, Seddon J A, Cooke G S, Ford N. Treatment outcomes for children with multidrug-resistant tuberculosis: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12:449–456. doi: 10.1016/S1473-3099(12)70033-6. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization. Global tuberculosis report, 2013. Geneva, Switzerland: WHO; 2013. WHO/HTM/TB/2013.11. [Google Scholar]
- 11.Lewinsohn D A, Gennaro M L, Scholvinck L, Lewinsohn D M. Tuberculosis immunology in children: diagnostic and therapeutic challenges and opportunities. Int J Tuberc Lung Dis. 2004;8:658–674. [PubMed] [Google Scholar]
- 12.Donald P R. Childhood tuberculosis: out of control? Curr Opin Pulm Med. 2002;8:178–182. doi: 10.1097/00063198-200205000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Keshavjee S, Farmer P E. Picking up the pace: scale-up of MDR tuberculosis treatment programs. N Engl J Med. 2010;363:1781–1784. doi: 10.1056/NEJMp1010023. [DOI] [PubMed] [Google Scholar]
- 14.Ramos J M, Padilla S, Masia M, Gutierrez F. A bibliometric analysis of tuberculosis research indexed in PubMed, 1997–2006. Int J Tuberc Lung Dis. 2008;12:1461–1468. [PubMed] [Google Scholar]
- 15.Sentinel Project. Stories of children with drug-resistant TB. Boston, MA, USA: Sentinel Project; 2015. http://sentinel-project.org/stories/ Accessed January 2015. [Google Scholar]
- 16.Perez-Velez C M, Marais B J. Tuberculosis in children. N Engl J Med. 2012;367:348–361. doi: 10.1056/NEJMra1008049. [DOI] [PubMed] [Google Scholar]
- 17.Seddon J A, Furin J J, Gale M et al. Caring for children with drug-resistant tuberculosis: practice-based recommendations. Am J Respir Crit Care Med. 2012;186:953–964. doi: 10.1164/rccm.201206-1001CI. [DOI] [PubMed] [Google Scholar]
- 18.Seddon J A, Perez-Velez C M, Schaaf H S et al. Consensus statement on research definitions for drug-resistant tuberculosis in children. J Pediatric Infect Dis Soc. 2013;2:100–109. doi: 10.1093/jpids/pit012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization. Guidance for national tuberculosis programmes on the management of tuberculosis in children. Geneva, Switzerland: WHO; 2006. WHO/HTM/TB/2006.371. WHO/FCH/CAH/2006.7. [PubMed] [Google Scholar]
- 20.World Health Organization. Childhood TB subgroup of the Stop TB Partnership. Roadmap for childhood tuberculosis: towards zero deaths. Geneva, Switzerland: WHO; 2013. WHO/HTM/TB/2013.12. [Google Scholar]


