Abstract
Objective: 1) To assess patient delay among new smear-positive pulmonary tuberculosis (PTB) patients in accessing health services in seven FIDELIS (Fund for Innovative DOTS Expansion through Local Initiatives to Stop TB) projects from 2003 to 2008 in China; 2) to compare treatment delay by province; and 3) to assess factors associated with delay.
Method: Records of new smear-positive PTB patients were reviewed. Data sources were the consultation book, laboratory register, patient record, treatment card and the PWLAHS (people with limited access to health services) evaluation form. Data were collected using a standard questionnaire, cross-checked by staff from the sites and by the International Union Against Tuberculosis and Lung Disease (The Union) and analysed by The Union.
Results: Of the 75 401 new smear-positive PTB patients included in the study, 63–89% were PWLAHS. The average gross domestic product of the project sites and at national level were respectively US$557 and US$998. The median patient delay was 93 days (range 68–128). Delays were longer among females, older patients, rural residents and PWLAHS. Delayed access to health services was significantly associated with a greater number of symptoms.
Conclusion: Patient delay in accessing health care in China was lengthy; TB care and control needs to be improved.
Keywords: tuberculosis, delay, associate factors, China
Abstract
Objectif : Evaluer le délai d’accès aux services des santé de nouveaux patients atteints de tuberculose pulmonaire (TBP) à frottis positif détectés au sein de sept projets FIDELIS (Fund for Innovative DOTS Expansion through Local Initiatives to Stop TB) exécutés en Chine entre 2003 et 2008 ; 2) comparer les retards du traitement par province ; et 3) évaluer les facteurs associés aux retards.
Méthode : Les dossiers des patients TPB à frottis positif ont été revus. Les données émanaient du registre des consultations, de celui du laboratoire, des dossiers des patients, des cartes de traitement et des formulaires d’évaluation des personnes ayant un accès limité aux services de santé (PWLAHS). Les données ont été recueillies grâce à un questionnaire standard et vérifiées par le personnel des sites et de l’Union Internationale contre la Tuberculose et les Maladies Respiratoires (L’Union) et analysées par L’Union.
Résultats : De 75 401 nouveaux patients atteints de TBP à frottis positif, 63–89% étaient des PWLAHS. Le produit intérieur brut moyen des sites du projet et du niveau national était de 557 et 998 $US respectivement. Le délai médian d’accès aux soins était de 93 jours (extrêmes 68–128). Ce délai était plus long pour les femmes, les patients âgés, les résidents ruraux et ceux estimés être des PWLAHS. Ce délai d’accès aux services était significativement associé à un nombre de symptômes plus élevé.
Conclusions : Le délai d’accès aux services de santé en Chine est long et offre des opportunités d’amélioration en matière de lutte contre la TB et de traitement.
Abstract
Objetivo: 1) Evaluar el retraso en el acceso a los servicios de salud de los pacientes en quienes se diagnosticó tuberculosis pulmonar (TBP) con baciloscopia positiva en siete centros del Proyecto FIDELIS (Fondo para la Expansión Innovadora de DOTS por conducto de Iniciativas Locales a fin de poner Alto a la Tuberculosis) del 2003 al 2008 en la China; 2) comparar el retraso en el tratamiento entre provincias; y 3) evaluar los factores asociados con estos retrasos.
Método: Se analizaron las historias clínicas de los pacientes con TBP y baciloscopia positiva. Las fuentes de los datos fueron los libros de consulta, el registro de laboratorio, las historias clínicas, las tarjetas de tratamiento y el formulario de evaluación de las personas con acceso limitado a los servicios de salud. Se recogieron los datos mediante un cuestionario normalizado y verificado que analizaron profesionales de los centros locales y de la Unión contra la Tuberculosis y las Enfermedades Respiratorias.
Resultados: Se incluyeron en el estudio 75 401 casos nuevos de TBP con baciloscopia positiva. El producto interno bruto promedio por habitante a escala de los centros del proyecto era 557 USD y a escala nacional era 998 USD. De los pacientes con TB, entre el 63% y el 89% contaban con un acceso limitado a los servicios de salud. La mediana del retraso de los pacientes en acceder a la atención fue 93 días (extremos 68 a 128 días). Los retrasos fueron más prolongados en las mujeres, los pacientes de mayor edad, los residentes en zonas rurales y las personas que se calificaron con un acceso limitado a los servicios sanitarios. El acceso tardío a los servicios de salud se asoció de manera significativa con una mayor cantidad de síntomas.
Conclusión: Se observó un retraso considerable de los pacientes para acceder a la atención de salud; esta situación ofrece oportunidades para mejorar la atención y el control de la TB.
Delays in diagnosis and treatment of tuberculosis (TB) may result in higher mortality and morbidity due to prolonged disease and the development of complications, as well as increased risk of further transmission of infection.1 Delay in accessing TB care is common in both industrialised and developing countries. However, there is no international consensus on what constitutes an acceptable delay.1
The 2000 National TB Prevalence survey revealed two major reasons for patients not accessing TB care:2 1) ignoring symptoms or not understanding their significance, and 2) financial difficulty. It reported that 67% of TB patients identified by the survey had never been diagnosed with TB, and 43% had not sought any health care at all. Several reports indicate that patient delay in accessing TB care is common in both rural and urban areas in China, with the length of delay varying from 21 to >80 days;3–5 however, there has been no extensive study across provinces/cities to document the actual situation. This paper 1) reports on patient delay in accessing health services among the 75 401 new smear-positive pulmonary TB (PTB) patients detected by the seven FIDELIS (Fund for Innovative DOTS Expansion through Local Initiatives to Stop TB) projects in China; 2) compares treatment delay by province; and 3) assesses factors associated with delay.
METHODS
Design
This was a cross-sectional study; the main outcome measured was treatment delay in the seven FIDELIS projects in China from 2003 to 2008.
Settings and sites
To address the urgent issue of inadequate global TB case detection, the Canadian Government, through the Canadian International Development Agency (CIDA), provided support to the International Union Against Tuberculosis and Lung Disease (The Union, Paris, France) to embark on a ground-breaking initiative. The FIDELIS project aimed to increase case detection of new smear-positive TB cases while maintaining high cure rates.6 Project applications were reviewed by an independent panel of experts, and were selected for funding based on the proposed interventions and on the estimated increase in case finding of people with limited access to health services (PWLAHS).
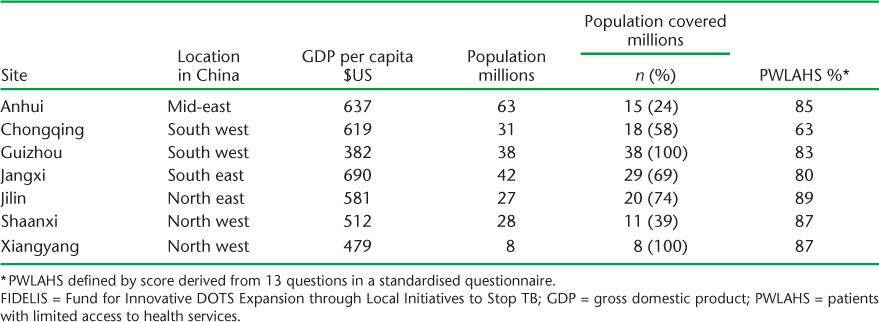
Of the 15 FIDELIS projects in China, seven were selected for evaluation in this study. We selected one from each region (geographically combining several adjacent provinces) as representing middle-level economic development settings in the region. Two projects were selected from regions with more than two FIDELIS projects. The types of interventions are shown in Table 1. The mean GDP in the selected sites and in those not selected was respectively US$557 (ranging from US$382 in Guizhou to US$690 in Jiangxi) and US$632 (Table 2).
TABLE 1.
Types of interventions used in the seven FIDELIS projects in China, 2003–2008
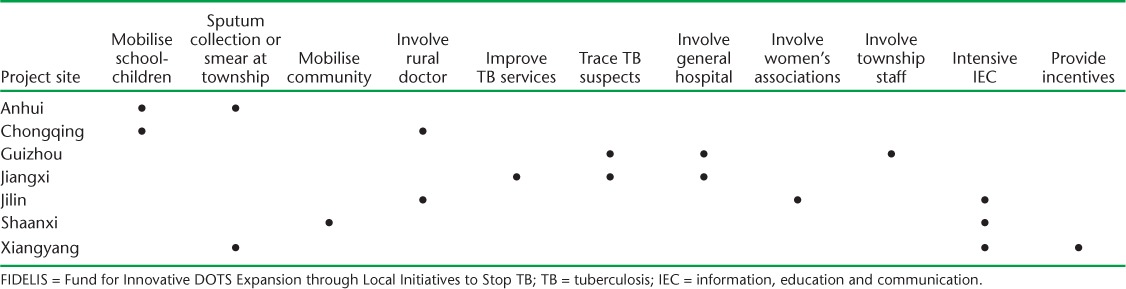
TABLE 2.
Background information on the seven FIDELIS projects at the time of starting the project by site, China, 2003–2008
Study population
The study population comprised consecutively diagnosed patients with new smear-positive PTB registered between 1 May 2004 and 31 January 2008 in the selected projects.
Definitions
New smear-positive PTB: a smear-positive TB patient who had never received treatment for TB for as much as one month.
Patient delay: interval (>0 days) between the onset of symptoms and the first visit to a health care facility.
PWLAHS: a specially designed questionnaire was used in the project to assess the period from symptom onset to initiation of anti-tuberculosis treatment, as well as the type of health care provider visited. Patients were graded according to the items on the questionnaire; those with the highest values for items relating to delay were regarded as PWLAHS.
Chest X-ray (CXR) cavity: cavities were identified on CXR by two medical officers/radiologists at the TB clinics/hospitals, and defined according to the national TB guidelines as well as the Practical Diagnostic Image Atlas for Pulmonary Tuberculosis published by the TB Branch of the China Medical Association (Beijing, China).7,8
Data collection and recording
A standardised questionnaire used for data collection and recording contained questions on demographic information, the patient’s PWLAHS status, disease history and health care-seeking behaviour from the onset of symptoms to commencement of anti-tuberculosis treatment. Data sources were the consultation book, laboratory register, patient records, treatment cards and PWLAHS evaluation form. If the patient was only able to recall the month and not the specific date, the 15th day of the month was automatically assigned. The questionnaire was compiled by county/district TB clinic staff and reviewed by prefectural and provincial TB control staff. Supervision and site visits were carried out by Union staff and the contractor of the FIDELIS projects within 3 months of beginning the project.
Data analysis and statistics
A database was created using EpiData 3.1 (EpiData Association, Odense, Denmark). Individual patient data were received and cross-checked by the staff at the Union China Office, then double-entered into the database and analysed using SAS version 9.1 (Statistical Analysis System Institute, Cary, NC, USA). The two groups were compared using the Mann-Whitney test; the Kruskal-Wallis test was used for three or more groups. The level of significance was set at α = 0.05.
Ethics approval
A formal agreement was signed between The Union and national authorities implementing the FIDELIS projects. As the study evaluated routinely collected patient information, formal ethics approval was deemed not to be necessary. Patient information was handled only by care givers, and no individual identifiers were revealed to individuals outside the health service.
RESULTS
Of 81 573 new smear-positive PTB patients whose data were collected, 6172 (7.6%) were excluded due to incomplete keying information or duplicate records; a final 75 401 new smear-positive PTB patients were included in this study.
FIDELIS projects provided services to 139 million individuals in various regions of China. At the time the projects were initiated, the proportion of patients judged as having limited access ranged from 63% (Chongqing) to 89% (Jilin).
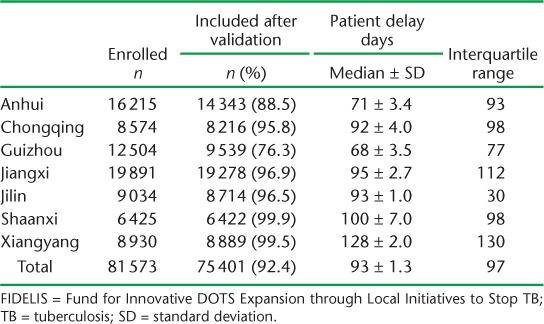
Patient delay among patients registered in the projects is shown in Table 3. The distribution of patient delay was skewed to the right. The median delay for all patients in the projects was 93 days (range 68–128).
TABLE 3.
Number of records collected and validated and patient delay in accessing health services after onset of tuberculosis symptoms in seven FIDELIS projects by project, China, 2003–2008
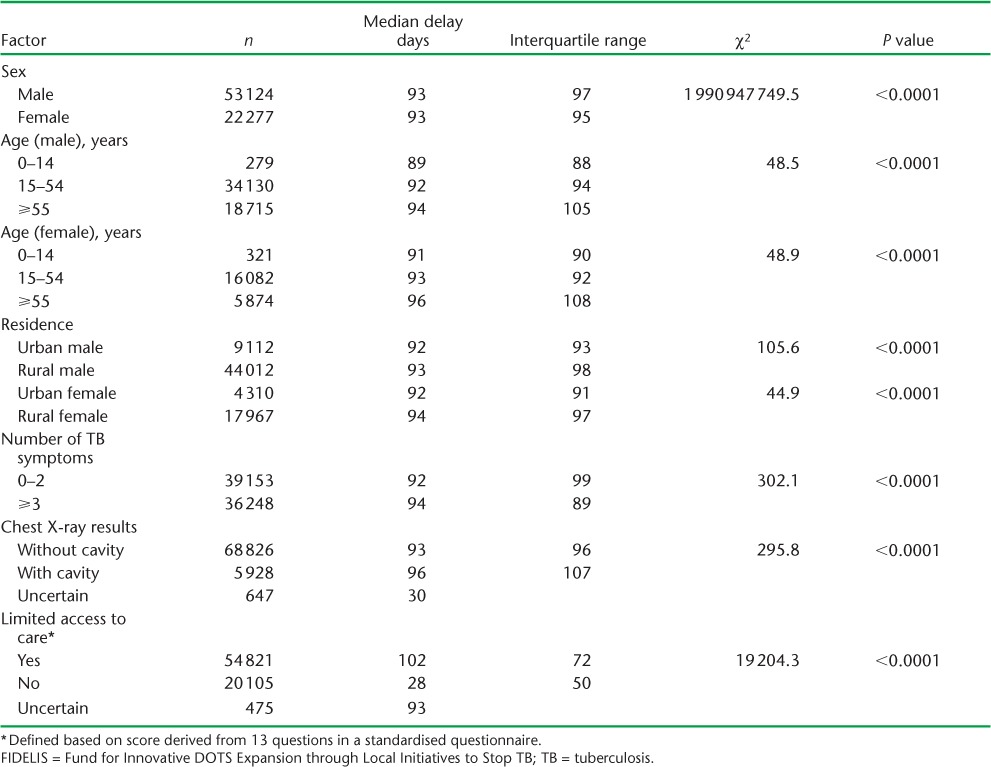
The association of delay with various factors is shown in Table 4. Delays were longer for females, older patients, rural residents and those judged to be PWLAHS. Delayed access to health services was significantly associated with a greater number of symptoms and more extensive disease on CXR.
TABLE 4.
Factors associated with patient delay (in days) of 75 401 new smear-positive TB patients registered in seven FIDELIS projects, China, 2003–2008
DISCUSSION
The median patient delay was 93.0 days, in line with international reports,1,9,10 but much longer than that reported from previous small-scale studies in China.3,4,11 This finding reflects the FI-DELIS focus on PWLAHS. The median patient delay among the seven projects varied between 71 and 128 days.
The average GDP per capita in the seven FIDELIS project areas was equal to 55.8% of the national GDP (US$998) at that time.12 Financial barriers to seeking TB care was also partially highlighted in the study. In the regions of Anhui, Jiangxi and Chongqing, which had a slightly higher GDP, the median patient delay was shorter. In contrast, Shaanxi and Xianyang, which had the lowest GDP, demonstrated a much longer median patient delay.12 However, the shorter periods of patient delay in Guizhou and Jilin do not correlate with their economic indicators. A well-established TB network, the sound health education component in the FIDELIS projects, as well as active case finding, such as using primary schoolchildren to deliver information, education and communication (IEC) material to parents or grandparents with presumed TB symptoms and to return the TB forms back to the school, may contribute to improved health care seeking behaviour among patients.13 Furthermore, this change in health-seeking behaviour may be due to the FIDELIS projects and/or other projects in the same areas at the same time or before the study. Some previous studies in China reported better TB control, with patients spending less on TB care, in project areas than in non-project areas.14,15 Other TB control projects were being run by the World Bank (Washington DC, USA), the Chinese Ministry of Health (Beijing, China), the Global Fund (Geneva, Switzerland) and FIDELIS in Chongqing, Guizhou, Jiangxi, Anhui and Jilin. Shaanxi and Xianyang possibly had longer patient delays due to the lower number of TB control projects or late launch of the projects. However, one study reported that patient delay in accessing TB care in a county using DOTS was longer than in a non-DOTS-using county.4 Such comparative analysis needs further data extraction and research, and was therefore outside the scope of this paper.
As in other studies, this study group was predominantly male.1,9,16 Our study findings share other similarities with these studies.17–19 Around 30% of the 75 401 TB patients registered were female and experienced longer patient delays. Longer delays among females in accessing TB care may be due to sex differences in socio-economic status and educational level. A recent study found that only 15% of women knew that prolonged cough for ⩾3 weeks was a symptom of TB, and were more likely to seek health care than men after the onset of TB symptoms. They were also more likely to visit low-level health care providers or pharmacies.19 This health care seeking pathway may also cause health service delays among female patients.
We observed that delays in accessing health services were significantly associated with increased age. The effect of age on delay would potentially be affected by economic status and educational level as well as general socio-economic status.20,21 Previous reports have indicated that less educated patients had less access to knowledge about TB, and would therefore be less aware of the potential implications of symptoms.3,19,22 They may also ignore TB symptoms due to existing comorbid conditions, such as smoking or chronic cough.16 Our study is in agreement with previous study findings that both male and female patients in rural areas experience much longer delays.10,11,23 In addition to economic reasons, this could also be due to the limited medical resources in rural and remote areas, as well as limited access to IEC materials.19,24
Reasons for the longer delays in the 15–54 year age group than in the 0–14 year age group could be due to a combination of many social factors: as 15–54 year olds are of working age, they may not be able to take time away from work to visit health services. Another intriguing finding that requires further study was that timely accessing of medical services was not consistent with the severity of TB symptoms or extent of lung damage. Longer delays generally result in more symptoms and advanced cavitation. Of the 75 401 new smear-positive TB patients, 48% had ⩾3 TB symptoms and 8% had lung cavities on CXR; however, these subgroups also experienced much longer patient delays. This finding contradicts the traditional assumption that patients with more TB symptoms would consult a health care provider earlier.2 Some previous reports showed that TB patients with more severe TB symptoms, particularly those with haemoptysis, were less likely to experience delay in accessing TB care.25–27 One of the possible reasons for longer delays in our study may be that study patients did not perceive prolonged cough, fatigue, fever, weight loss and night sweat as symptoms of TB, or this might have been further complicated by financial limitations. As passive case finding, i.e., the method whereby patients with symptoms voluntarily access health facilities, is the main strategy for the identification of TB patients, this finding suggests that there is room for improved TB case finding by encouraging patients with symptoms suggestive of TB to access services in a timely manner. Similar findings were observed in relation to health service delay; however, this was not addressed in the present paper. Although those with ⩾3 TB symptoms should be more likely to attract the attention of health workers, this subgroup had much longer health service delay than those with <3 TB symptoms. This shows that both patient awareness about TB symptoms and health worker ability to identify patients with presumed TB need improvement. A previous report suggested that better training of health care workers and distribution of educational material could improve case finding.28
In terms of CXR results (Table 4), it is not known why patients with lung cavity had slightly longer delay in accessing TB care than those without. Possible reasons could be the high proportion of patients with PWLAHS and/or the high proportion of rural residents. However, any further analysis would require further adjustments for age, sex and socio-economic status.
There are some limitations in our study. Overall, we collected data from seven FIDELIS projects of the 15 available. This may be subject to potential selection bias. We did not collect data on the type of health care institution patients initially visited, nor did we analyse individual delay in relation to the patient’s economic status. Furthermore, data on the type of patients attending township health centres and the other types of health facilities were not collected. Some previous studies reported that socially disadvantaged patients, such as the unemployed, rural to urban migrant workers and those without health insurance are at high risk of patient delay,19,29,30 as these patients were more likely to visit low-level health care providers.19,29 Finally, we did not interview patients directly, but relied on information already collected in routine settings.
The strength of this study is that data on a large number of patients from routine TB services reflecting conditions in the field were collected.
CONCLUSION
This study provides direct evidence of patient delay using large patient populations from routine TB services across several provinces in China. As one of the world’s highest TB burden countries, there would be substantial potential public health benefits if patient delay could be reduced by addressing the issues raised in this study.
Acknowledgments
The authors thank the CIDA for funding support to the FIDELIS projects. The authors would like to thank all the staff at the seven FIDELIS sites for their efforts in managing and monitoring patients.
Footnotes
Conflicts of interest: none declared.
References
- 1.Storla D G, Yimer S, Bjune G A. A systematic review of delay in the diagnosis and treatment of tuberculosis. BMC Public Health. 2008;8:15. doi: 10.1186/1471-2458-8-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ministry of Health. China. Report of nationwide random survey on epidemiology of tuberculosis in 2000. Beijing, China: The People’s Medical Publisher House; 2003. pp. 4–69. [Google Scholar]
- 3.Cheng G, Tolhurst R, Li R Z et al. Factors affecting delays in tuberculosis in rural China: a case study in four counties in Shandong Province. Trans R Soc Trop Med Hyg. 2005;99:355–362. doi: 10.1016/j.trstmh.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 4.Xu B, Diwan K V, Bogg L. Access to tuberculosis care: what did chronic cough patients experience in the way of healthcare-seeking? Scand J Public Health. 2007;35:396–402. doi: 10.1080/14034940601160664. [DOI] [PubMed] [Google Scholar]
- 5.Yan F, Thomson R, Tang S et al. Multi perspectives on diagnosis delay for tuberculosis from key stakeholders in poor rural China: case study in four provinces. Health Policy. 2007;82:186–199. doi: 10.1016/j.healthpol.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 6.Rusen I D, Enarson D A. FIDELIS-innovative approaches to increasing global case detection of tuberculosis. Am J Public Health. 2006;96:14–16. doi: 10.2105/AJPH.2004.056762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xiao D L. Practical diagnostic image atlas for pulmonary tuberculosis. Beijing, China: The People’s Medical Publisher House; 2006. pp. 19–77. [Google Scholar]
- 8.Tuberculosis Branch of China Medical Association. Operation menu of clinical tuberculosis. Beijing, China: The People’s Military Medical Publisher House; 2004. pp. 23–61. [Google Scholar]
- 9.Sreeramareddy C T, Panduru K V, Menten J, Ende J V. Time delays in diagnosis of pulmonary tuberculosis: a systematic review of literature. BMC Infect Dis. 2009;9:91. doi: 10.1186/1471-2334-9-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rifat M, Rusen I D, Islam Md A et al. Why are tuberculosis patients not treated earlier? A study of informal health practitioners in Bangladesh. Int J Tuberc Lung Dis. 2011;15:647–651. doi: 10.5588/ijtld.10.0205. [DOI] [PubMed] [Google Scholar]
- 11.Wang Y, Long Q, Liu Q et al. Treatment seeking for symptoms suggestive of TB: comparison between migrants and permanent urban residents in Chongqing, China. Trop Med Int Health. 2008;13:927–933. doi: 10.1111/j.1365-3156.2008.02093.x. [DOI] [PubMed] [Google Scholar]
- 12.National Bureau of Statistics of China. China Statistical Yearbook 2003. Beijing, China: China Statistics Press; 2003. [Google Scholar]
- 13.Bai L Q, Yang H L, Jian X W et al. Increasing tuberculosis case detection through intensive referral and tracing in Hunan, China. Int J Tuberc Lung Dis. 2008;12:1431–1435. [PubMed] [Google Scholar]
- 14.Chen X, Zhao F, Duanmu H et al. The DOTS strategy in China: results and lessons after 10 years. Bull World Health Organ. 2002;80:430–436. [PMC free article] [PubMed] [Google Scholar]
- 15.Wei X-L, Liang X-L, Walley J D et al. Analysis of care-seeking pathways of tuberculosis patients in Guangxi, China, with and without decentralised tuberculosis services. Int J Tuberc Lung Dis. 2009;13:514–520. [PubMed] [Google Scholar]
- 16.Bam T S, Enarson D A, Hinderaker S G, Bam D S. Long delay in accessing treatment among current smokers with new sputum smear-positive tuberculosis in Nepal. Int J Tuberc Lung Dis. 2012;16:822–827. doi: 10.5588/ijtld.11.0678. [DOI] [PubMed] [Google Scholar]
- 17.Paynter S, Hayward A, Wilkinson P et al. Patient and health service delays in initiating treatment for patients with pulmonary tuberculosis: retrospective cohort study. Int J Tuberc Lung Dis. 2004;8:180–185. [PubMed] [Google Scholar]
- 18.Rundi C, Fielding K, Godfrey-Faussett P et al. Delays in seeking treatment for symptomatic tuberculosis in Sabah, East Malaysia: factors for patient delay. Int J Tuberc Lung Dis. 2011;15:1231–1238. doi: 10.5588/ijtld.10.0585. [DOI] [PubMed] [Google Scholar]
- 19.Wang J, Fei Y, Shen H, Xu B. Gender difference in knowledge of tuberculosis and associated health-care seeking behaviours: a cross-sectional study in rural area of China. BMC Public Health. 2008;8:354–360. doi: 10.1186/1471-2458-8-354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kamolratanakul P, Sawert H, Kongsin S et al. Economic impact of tuberculosis at the household level. Int J Tuberc Lung Dis. 1999;3:596–602. [PubMed] [Google Scholar]
- 21.Liu X Y, Thomson R, Gong Y L et al. How affordable are tuberculosis diagnosis and treatment in rural China? An analysis from community and TB patient perspectives. Trop Med Int Health. 2007;12:1464–1471. doi: 10.1111/j.1365-3156.2007.01953.x. [DOI] [PubMed] [Google Scholar]
- 22.Lorent N, Mugwaneza P, Mugabekazi J et al. Risk factors for delay in the diagnosis and treatment of tuberculosis at a referral hospital in Rwanda. Int J Tuberc Lung Dis. 2008;12:392–396. [PubMed] [Google Scholar]
- 23.Wang W B, Jiang Q W, Chen Y, Xu B. Pathways from first health care seeking to diagnosis: obstacles to tuberculosis care in rural China. Int J Tuberc Lung Dis. 2007;11:386–391. [PubMed] [Google Scholar]
- 24.Ministry of Health. China Statistics Digest. Beijing, China: Ministry of Health; 2005. pp. 2–39. [Google Scholar]
- 25.Leung E C, Leung C C, Tam C M. Delay presentation and treatment of newly diagnosed pulmonary tuberculosis patients in Hong Kong. Hong Kong Med J. 2007;13:221–227. [PubMed] [Google Scholar]
- 26.Wang W, Jiang Q, Abdullah A S et al. Barriers in accessing to tuberculosis care among non-residents in Shanghai : a descriptive study of delays in diagnosis. Eur J Public Health. 2007;17:419–423. doi: 10.1093/eurpub/ckm029. [DOI] [PubMed] [Google Scholar]
- 27.Pehme L, Rahu M, Altraja A. Factors related to patient delay in pulmonary tuberculosis in Estonia. Scand J Infect Dis. 2006;38:1017–1022. doi: 10.1080/00365540600809994. [DOI] [PubMed] [Google Scholar]
- 28.Xiong C F, Fang Y, Zhou L P et al. Increasing TB case detection through intensive referral of TB suspects by village doctors to county TB dispensaries. Int J Tuberc Lung Dis. 2007;11:1004–1007. [PubMed] [Google Scholar]
- 29.Tattevin P, Che D, Fraisse P et al. Factors associated with patient and health care system delay in the diagnosis of tuberculosis in France. Int J Tuberc Lung Dis. 2012;16:510–515. doi: 10.5588/ijtld.11.0420. [DOI] [PubMed] [Google Scholar]
- 30.Enarson D. Migrant tuberculosis: a moving target. Int J Tuberc Lung Dis. 2006;10:945. [PubMed] [Google Scholar]


