Abstract
Background & objectives:
Several diabetes prevention programmes have demonstrated a reduction in incidence of diabetes in individuals with prediabetes through weight loss. Short-term yoga-based lifestyle intervention programmes have also been shown to be efficacious in weight loss. This study was undertaken to investigate if interleukin (IL)-6, vitamin D, neopterin, vaspin, and diabetes risk factors can be modified by a short-term yoga-based lifestyle intervention in overweight/obese subjects.
Methods:
In this pilot study, 34 overweight/obese [body mass index (BMI) ≥23 to <35 kg/m2 per Asian cut-off values] individuals were enrolled, and received directly supervised intervention for 10 days. Thereafter, they were advised to follow this yoga-based lifestyle at home for one month, and were reassessed for study variables at day 30.
Results:
There was a reduction from baseline to day 10 in weight (P<0.001), BMI (P<0.001), waist/hip-ratio (P<0.05), blood glucose (P<0.01), and a significant improvement in lipid profile. There was a decrease in median fasting insulin (P<0.05), homeostatic model assessment-insulin resistance (P<0.01), and IL-6 (P<0.05). A non-significant increase in 25-OH-vitamin D, and a decrease in neopterin and vaspin were observed. Twenty subjects returned for follow up assessments. At day 30, weight loss was sustained while systolic blood pressure also showed reduction (P<0.05). Changes in vitamin D levels were significantly and negatively correlated with changes in weight, BMI and fasting blood glucose, and positively with change in high density lipoprotein. Changes in body weight and BMI significantly and positively correlated with insulin. Changes in IL-6 levels positively and significantly correlated with change in neopterin levels.
Interpretation & conclusions:
The findings showed that IL-6, vitamin D, and diabetes risk factors were favourably modified by a short-term yoga-based lifestyle intervention in obesity. This study also highlighted the challenges in compliance associated with the follow up of subjects following an aggressive supervised intervention of 10 days.
Keywords: Diabetes risk reduction, IL-6, overweight/obesity, short-term yoga-based lifestyle intervention, vitamin D, weight-loss
Obesity is an independent risk factor for insulin resistance1 leading to persistently impaired glucose tolerance culminating into diabetes mellitus type 2. This association between obesity and diabetes has been attributed to adipocytokines, namely adiponectin, interleukin-6 (IL-6), interferon-γ, and tissue necrosis factor-α that not only alter insulin resistance2, but are also associated with adverse cardiovascular outcomes related to diabetes3. Visceral adipose tissue also expresses vaspin (visceral adipose tissue serine protease inhibitor), which has unique insulin sensitizing effects on adipose tissue4. Another important diabetes risk factor is hypovitaminosis of vitamin D5, as it has an inverse association with insulin resistance6. Additionally, dyslipidaemia in obesity leads to high levels of triglycerides and circulating fatty acids that impair insulin-mediated glucose uptake by muscle cells further contributing to insulin resistance7.
Baseline overweight is the strongest predictor of diabetes and accounts for 82 per cent of the diabetes risk together with reduced physical activity, alcohol abuse, smoking, and low serum vitamin D shown to be efficacious8 mainly due to improved insulin sensitivity and glucose homeostasis9, thus playing a significant role in diabetes prevention programmes (DPP). The US DPP and the Finnish DPP, which enrolled a large number of patients, demonstrated that the incidence of diabetes could be reduced by almost 60 per cent in patients with prediabetes through weight loss resulting from changes in diet and physical activity10,11, though only one study reported a significant reduction in blood glucose in individuals with prediabetes12.
Such benefit can also be ensued by interventions that reduce inflammation, improve insulin sensitivity and delay disease onset and/or progression such as lifestyle interventions, though not much information is available. We have earlier shown that even a short-term yoga-based lifestyle intervention was efficacious in weight loss, reduced inflammation and stress13, and positively influenced cardiovascular risk factors14,15. However, the efficacy of a short-term yoga-based lifestyle intervention in improving inflammation and levels of vitamin D along with diabetes risk factors in overweight/obese subjects has not been evaluated. The current pilot study was, therefore, planned to evaluate the effectiveness of such an intervention on IL-6, vitamin D, neopterin, vaspin, fasting blood glucose, insulin resistance, waist/hip ratio, lipid profile, and blood pressure in overweight/obese subjects with a follow up at one-month.
Material & Methods
This pilot study was conducted between December 2011 and December 2012, at the All India Institute of Medical Sciences (AIIMS), New Delhi, India. The study evaluated the effect of a short-term yoga-based lifestyle intervention on IL-6, vitamin D, and diabetes risk factors in obesity. The study was also aimed to determine the feasibility, sustainability, compliance and effectiveness of this short-term intervention (10 days) during a longer follow up i.e. up to one month. The study protocol was approved by the Institute's Ethics Committee. All participants provided their written informed consent. This preliminary trial was registered at Clinical Trial Registry India (CTRI), CTRI/2013/01/004502.
Study participants: This study included 34 overweight/obese individuals (21 male and 13 female, mean age 36.79 ± 9.9 yr), who were recruited from the Integral Health Clinic (IHC), Department of Physiology, AIIMS, New Delhi. All the consecutive individuals who fulfilled the inclusion criteria were included in the study. The overweight/obese subjects come directly to IHC or are referred from outpatient departments (OPDs) like Medicine/ Endocrinology. The body mass index (BMI) range of overweight/obese subjects (BMI ≥ 23 to <35 kg/m2) was taken as per Asian cut-off values as a BMI of ≥ 23 is now considered overweight and more than 25 is taken as obese for Asian population, which is lower than that for the Western population16. Subjects with previously diagnosed diabetes, cardiovascular diseases, hypertension, and other chronic diseases were excluded. Also, excluded were heavy alcoholics and smokers, physically challenged subjects who were unable to perform the exercises, and those on other extensive dietary and/or exercise intervention programmes or regimens in the last three months. Pregnant and lactating women were also excluded from the study.
Lifestyle intervention: This lifestyle intervention was an outpatient, short-term yoga-based programme, and consisted of a 10-days integrated and pretested intervention. It comprised theory and practice sessions under direct supervision of yoga and medical experts13,14,15. Briefly, a typical day in the programme started with a set of simple physical exercises (asanas) and breathing exercises (pranayama) for approximately one hour. This was followed by an interactive educative lecture on weight management, and group discussion that allowed the participants to understand the importance of a healthy lifestyle and weight management in prevention of diabetes. Specific sessions were devoted to the importance of physical activity and diet in achieving optimal weight, and stress management. The participants were advised to take a healthy diet including 50-60 per cent carbohydrates, 15-30 per cent fats and about 10 per cent proteins17. Grossly, it was advised that diet should include a variety of fiber-rich cereals and pulses, about 400 to 500 g of fresh fruits and vegetables, preferably mono- and poly-unsaturated fats, and moderate amounts of dairy products. For the non-vegetarians, it was suggested that the consumption of red meats should be avoided, and preference should be given to white/lean meat (fish or chicken). Also, it was advised that alcohol consumption may be mild to moderate, if taken at all. Each day's programme ended with relaxation through either a relaxation technique (shavasana) or meditation. The sampling at Day 10 was done at the end of the concluding session to balance the immediate effects of relaxation techniques. The concluding session was of approximately one hour, and included feedback from each and every participant and study closeout activities. The programme batches were usually kept small (6 to 8 participants) to ensure that each participant spent enough time with the yoga and medical experts, and the quality of the programme was sustained. Spouse and other members of the participant's family were motivated to attend the programme in order to facilitate compliance. The participants were educated about benefits of yoga-based lifestyle intervention, and long-term benefits of the same were explained. The study participants were advised to follow the yoga-based lifestyle at home and to come for follow up assessments at day 30. However, there were no specific instructions given. The compliance was tracked through an attendance register during the first 10 days into the study while subjects attended the short-term intervention programme. During follow up period compliance was checked through phone calls and subject diaries which were collected on day 30, and was cross-checked with family member/spouse.
Study assessments: The study assessments included IL-6, 25-OH-vitamin D and diabetes risk factors such as obesity, fasting blood glucose, fasting insulin, insulin resistance, waist/hip ratio, blood pressure, heart rate, lipid profile (total cholesterol, LDL, HDL and triglycerides). The levels of neopterin, and vaspin were also assessed. All the assessments were done at baseline, day 10, and day 30.
For biochemical assessments, fasting venous blood samples (7 ml) were collected in plain and heparinized vials at baseline, at day 10, and at day 30, as appropriate. All the assessments were done while subjects were relaxed, and between 0800-0930 h to avoid any biases due to circadian rhythms. Samples were centrifuged at 2000x g for 15 min at 4° C and the plasma was stored at -80º C until analyzed. Fasting blood glucose was assessed using glucose oxidase method (RANDOX Laboratories Limited, UK). Other biochemical markers were estimated using commercially available ELISA kits for insulin, IL-6 (Diaclone, France), vitamin D (Diagnostika GmbH, Humberg, Germany), vaspin and neopterin (BMASSAY, China). Insulin resistance was assessed using homeostatic model assessment-insulin resistance (HOMA-IR)18. Serum total cholesterol, high density lipoprotein (HDL)-cholesterol and triglyceride levels were estimated using commercially available kits (Fortress diagnostics, UK), and serum low density lipoprotein (LDL) cholesterol was calculated by using Friedwald formula19. Quality control assays were taken for the biochemical markers, and methods were validated. The intra-assay coefficients of variations for neopterin, vaspin, IL-6, insulin, and vitamin D were 4.7, 4.19, 3.24, 4.77, and 3.97 per cent, respectively.
Statistical analysis: Descriptive statistics are provided for the demographic data and baseline profile. The mean and standard deviation (SD) values are presented for parametric data, and median and interquartile range (IQR) are presented for non-parametric data. The biomarkers before and after intervention at day 0 and day 10 were compared using paired sample t-test or Wilcoxon-signed rank test, as appropriate. The data at days 0, 10 and 30 were analyzed using repeated measures ANOVA or Friedman test, as appropriate. The correlations were tested using Pearson's test or Spearman's test, as appropriate. A two-sided P value of <0.05 was taken as significant.
Results
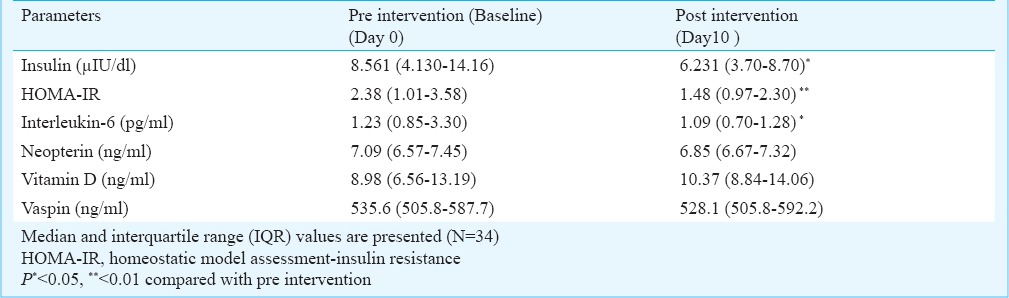
All the 34 overweight/obese participants in this study completed short-term intervention of 10 days. They were advised to practice the intervention while at home, and return for follow up assessments at day 30. The data for 20 subjects could be collected at day 30 as rest of the participants did not return for the follow up assessments (drop-outs). The results showed that there was a significant reduction in weight at day 10 vs. baseline (P<0.001), which reflected in a significant reduction in BMI and waist/hip ratio. Also, there was a significant reduction in the levels of fasting blood glucose at day 0 vs. day 10 (P<0.01) (Table I). The data for insulin, insulin resistance, IL-6, neopterin, vitamin D, and vaspin are presented in Table II. There was a significant decrease in median levels of insulin (P<0.05), HOMA-IR (P<0.01), and IL-6 (P<0.05) from baseline to day 10.
Table I.
Diabetes risk factors before and after lifestyle intervention programme at baseline and day 10
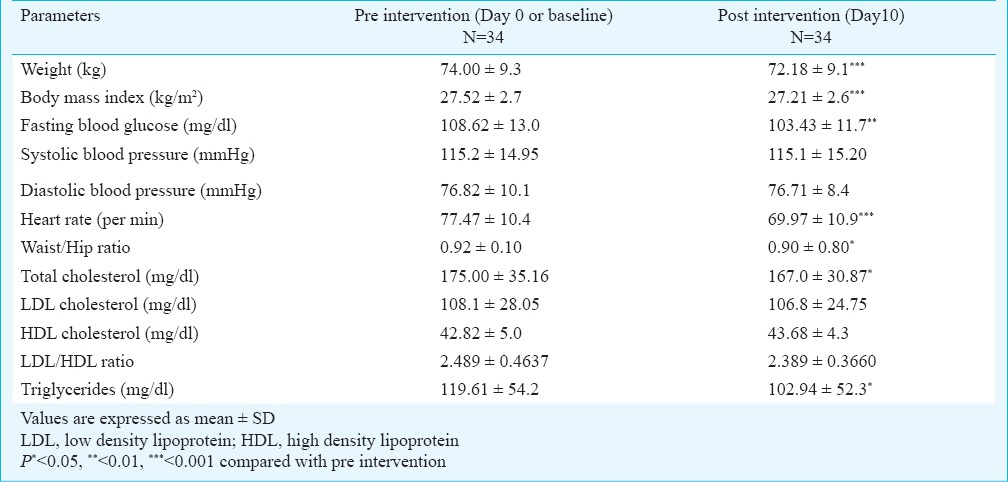
Table II.
Diabetes risk factors before and after lifestyle intervention programme at baseline and day 10
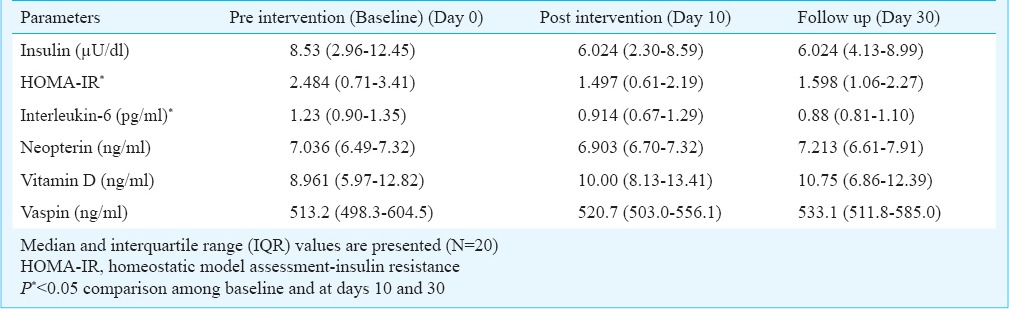
The data for one month follow up are presented in Tables III and IV. There was a sustained and significant weight reduction from baseline vs. day 10 vs. day 30 (P<0.01) with a similar sustained and significant reduction in BMI. In addition, there was a reduction in SBP (P<0.05). There was a significant reduction in insulin resistance and IL-6 levels from baseline to day 30.
Table III.
Effect of lifestyle intervention programme on diabetes risk factors at baseline, days 10 and 30
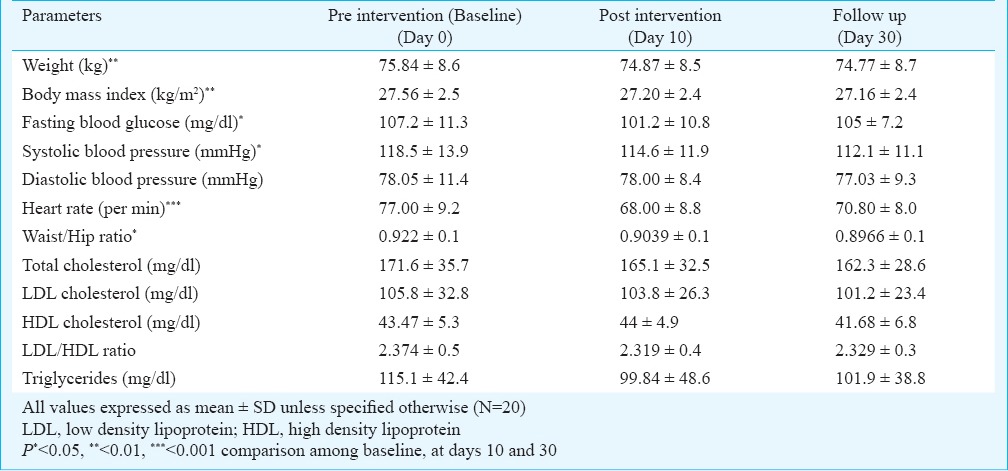
Table IV.
Effect of lifestyle intervention programme on diabetes risk factors at baseline, days 10 and 30
The correlation analysis showed that changes in vitamin D levels were significantly and negatively correlated with changes in weight, BMI and fasting blood glucose, while positively with change in HDL (Fig. 1). There was a significant positive correlation between change in body weight and BMI with insulin. Also, changes in IL-6 levels and body weight positively and significantly correlated with change in neopterin levels (Fig. 2).
Fig. 1.
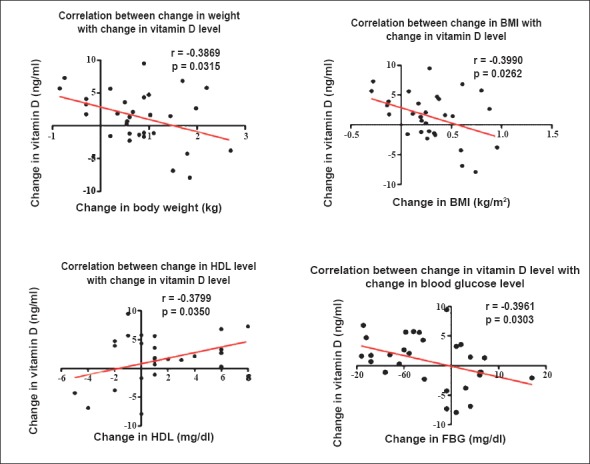
Correlation between vitamin D and body weight, body mass index (BMI), fasting blood glucose (FBG) and high density lipoprotein (HDL).
Fig. 2.

Correlation between interleukin-6 (IL-6), neopterin, insulin with body weight and BMI.
Discussion
There was a significant weight loss, reduction in waist/hip ratio, fasting blood glucose, fasting insulin levels, insulin resistance, IL-6, total cholesterol, triglycerides, and heart rate following a brief 10-day yoga-based lifestyle intervention, while reduction in weight and IL-6 sustained till day 30. Importantly, the sustainability and compliance of this supervised intervention of 10 days (short-term) intervention seems a big challenge in long-term follow up when there is no direct supervision as seen by the results at day 30.
Lifestyle interventions aiming at weight loss have been successful in diabetes risk reduction10,11. In the current study, there was a small but significant weight loss (average weight loss about 1 kg) within a short time of 10 days. This is of clinical relevance as for every one kg of weight lost, the risk of diabetes is reduced by 16 per cent20. There was also a reduction in the waist/hip ratio, which is an important predictor of diabetes21. This is especially pertinent to Indian population which exhibits central obesity and high fat percentage when compared to other ethnic groups with same BMI. Moreover, despite being leaner than population from West, Indians tend to have higher insulin resistance, possibly due to higher visceral fat22. A previous lifestyle intervention study had similar findings though changes in fasting blood glucose were not significant23. We also noted a significant improvement in serum lipid profile at day 10, and a significant reduction in systolic blood pressure at day 30.
Adipocytokines like IL-6 and interferon-γ (IFN-γ) are known to be related with insulin resistance, diabetes, and its complications2,24, indicating that controlling for these may reduce the risk of diabetes, and its complications. In the present study, there was a significant reduction in IL-6 levels at days 10 and 30. This was similar to our earlier studies where this short-term yoga-based lifestyle intervention was efficacious in reducing stress and inflammation13, and prevention/progression of cardiovascular diseases14. In addition to reduction in IL-6, there was a reduction in the level of neopterin, which is an indirect measure of IFN-γ25. The change in neopterin levels were significantly and positively correlated with change in body weight and IL-6.
We also studied vaspin, another adipocytokine with insulin-sensitizing effects and related to obesity. There was a subtle increase in vaspin levels in overweight/obese subjects following intervention, however, the available data for participants who were followed for one month remained inconclusive. This might be because of variable insulin resistance which is known to affect vaspin levels26. Since vaspin appears to be associated with insulin sensitivity, blood glucose concentration and BMI27, the results are important.
Fasting insulin and HOMA-IR responded favourably to the intervention with a significant reduction at day 10, though reduction was subtle at day 30. Since insulin resistance is a key link between obesity and the risk of diabetes and cardiovascular disease28, its reduction is clinically relevant. We also observed that the levels of fasting insulin decreased with decrease in weight, and BMI, supporting a previous finding that overweight/obesity was associated with higher levels of fasting insulin29. The present study also showed that there were favourable changes in lipid profile. Similar finding have been shown in previous studies using yogic intervention30,31.
Type 2 diabetes has been shown to be associated with hypovitaminosis D, which is important for normal insulin secretory responses including release of insulin from pro-insulin, and increasing β cell insulin sensitivity32. Insulin resistance is known to be inversely correlated with vitamin D levels in overweight/obese individuals6, and its levels may predict the risk of diabetes and adverse cardiovascular outcome33. In our study there was only a small increase in the levels of vitamin D following lifestyle intervention. The change in vitamin D was significantly and negatively correlated with changes in weight and BMI, and positively with the change in HDL-cholesterol levels suggesting that besides influencing glucose metabolism, vitamin D levels might also influence lipid profile34.
This study had a few limitations. The key limitation was a short duration of follow up. The compliance during the supervised short-term yoga-based intervention was good, however, the compliance during follow up was not as per our expectations. This clearly indicated that following an aggressively supervised yoga-based intervention of 10 days, sustainability of this intervention during a follow up period (home-based) was a big challenge. Therefore, a larger study with long-term follow up is warranted with more focus on compliance.
Overall, this short-term yoga-based lifestyle intervention programme was efficacious in modifying IL-6, vitamin D, and diabetes risk factors including fasting blood glucose, insulin resistance, and waist/hip ratio in overweight/obese individuals as early as 10 days.
References
- 1.Dandona P, Aljada A, Bandyopadhyay A. Inflammation: the link between insulin resistance, obesity and diabetes. Trends Immunol. 2004;25:4–7. doi: 10.1016/j.it.2003.10.013. [DOI] [PubMed] [Google Scholar]
- 2.King GL. The role of inflammatory cytokines in diabetes and its complications. J Periodontol. 2008;79(Suppl 8):1527–34. doi: 10.1902/jop.2008.080246. [DOI] [PubMed] [Google Scholar]
- 3.Sjoholm A, Nystrom T. Inflammation and the etiology of type 2 diabetes. Diabetes Metab Res Rev. 2006;22:4–10. doi: 10.1002/dmrr.568. [DOI] [PubMed] [Google Scholar]
- 4.Hida K, Wada J, Eguchi J, Zhang H, Baba M, Seida A, et al. Visceral adipose tissue-derived serine protease inhibitor: a unique insulin-sensitizing adipocytokine in obesity. Proc Natl Acad Sci USA. 2005;102:10610–5. doi: 10.1073/pnas.0504703102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Isaia G, Giorgino R, Adami S. High prevalence of hypovitaminosis D in female type 2 diabetic population. Diabetes Care. 2001;24:1496. doi: 10.2337/diacare.24.8.1496. [DOI] [PubMed] [Google Scholar]
- 6.Scragg R, Sowers M, Bell C. Third National Health and Nutrition Examination Survey. Serum 25-hydroxyvitamin D, diabetes, and ethnicity in the Third National Health and Nutrition Examination Survey. Diabetes Care. 2004;27:2813–8. doi: 10.2337/diacare.27.12.2813. [DOI] [PubMed] [Google Scholar]
- 7.Bilan PJ, Samokhvalov V, Koshkina A, Schertzer JD, Samaan MC, Klip A. Direct and macrophage-mediated actions of fatty acids causing insulin resistance in muscle cells. Arch Physiol Biochem. 2009;115:176–90. doi: 10.1080/13813450903079314. [DOI] [PubMed] [Google Scholar]
- 8.Hu FB, Manson JE, Stampfer MJ, Colditz G, Liu S, Solomon CG, et al. Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. N Engl J Med. 2001;345:790–7. doi: 10.1056/NEJMoa010492. [DOI] [PubMed] [Google Scholar]
- 9.Jazet IM, Schaart G, Gastaldelli A, Ferrannini E, Hesselink MK, Schrauwen P, et al. Loss of 50% of excess weight using a very low energy diet improves insulin-stimulated glucose disposal and skeletal muscle insulin signalling in obese insulin-treated type 2 diabetic patients. Diabetologia. 2008;51:309–19. doi: 10.1007/s00125-007-0862-2. [DOI] [PubMed] [Google Scholar]
- 10.Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tuomilehto J, Lindstrom J, Eriksson JG, Valle TT, Hamalainen H, Ilanne-Parikka P, et al. Finnish Diabetes Prevention Study group. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344:1343–50. doi: 10.1056/NEJM200105033441801. [DOI] [PubMed] [Google Scholar]
- 12.Katula JA, Vitolins MZ, Rosenberger EL, Blackwell CS, Morgan TM, Lawlor MS, et al. One-year results of a community-based translation of the Diabetes Prevention Program: Healthy-Living Partnerships to Prevent Diabetes (HELP PD) Project. Diabetes Care. 2011;34:1451–7. doi: 10.2337/dc10-2115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yadav RK, Magan D, Mehta N, Sharma R, Mahapatra SC. Efficacy of a short-term yoga-based lifestyle intervention in reducing stress and inflammation: preliminary results. J Altern Complement Med. 2012;18:662–7. doi: 10.1089/acm.2011.0265. [DOI] [PubMed] [Google Scholar]
- 14.Sarvottam K, Magan D, Yadav RK, Mehta N, Mahapatra SC. Adiponectin, interleukin-6, and cardiovascular disease risk factors are modified by a short-term yoga-based lifestyle intervention in overweight and obese men. J Altern Complement Med. 2013;19:397–402. doi: 10.1089/acm.2012.0086. [DOI] [PubMed] [Google Scholar]
- 15.Bijlani RL, Vempati RP, Yadav RK, Ray RB, Gupta V, Sharma R, et al. A brief but comprehensive lifestyle education program based on yoga reduces risk factors for cardiovascular disease and diabetes mellitus. J Altern Complement Med. 2005;11:267–74. doi: 10.1089/acm.2005.11.267. [DOI] [PubMed] [Google Scholar]
- 16.2nd ed. Sydney, Australia: Health Communications Australia Pvt. Limited; 2000. World Health Organization (WHO), Western Pacific Region, International Association for the Study of Obesity/International Obesity Taskforce. The Asia-Pacific perspective: redefining obesity and its treatment. [Google Scholar]
- 17.Hyderabad: National Institute of Nutrition; 2010. Dietary guidelines for Indians, a manual. [Google Scholar]
- 18.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 19.Friedwald WT, Levy RT, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preprative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 20.Hamman RF, Wing RR, Edelstein SL, Lachin JM, Bray GA, Delahanty L, et al. Effect of weight loss with lifestyle intervention on risk of diabetes. Diabetes Care. 2006;29:2102–7. doi: 10.2337/dc06-0560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhao X, Zhu X, Zhang HS, Zhao W, Li J, Shu Y, et al. Prevalence of diabetes and predictions of its risks using anthropometric measures in southwest rural areas of China. BMC Public Health. 2012;12:821. doi: 10.1186/1471-2458-12-821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chandalia M, Abate N, Garg A, Stray-Gundersen J, Grundy SM. Relationship between generalized and upper body obesity to insulin resistance in Asian Indian men. J Clin Endocrinol Metab. 1999;84:2329–35. doi: 10.1210/jcem.84.7.5817. [DOI] [PubMed] [Google Scholar]
- 23.Kramer MK, Kriska AM, Venditti EM, Miller RG, Brooks MM, Burke LE, et al. Translating the Diabetes Prevention Program: a comprehensive model for prevention training and program delivery. Am J Prev Med. 2009;37:505–11. doi: 10.1016/j.amepre.2009.07.020. [DOI] [PubMed] [Google Scholar]
- 24.Bastard JP, Maachi M, Van Nhieu JT, Jardel C, Bruckert E, Grimaldi A, et al. Adipose tissue IL-6 content correlates with resistance to insulin activation of glucose uptake both in vivo and in vitro . J Clin Endocrinol Metab. 2002;87:2084–9. doi: 10.1210/jcem.87.5.8450. [DOI] [PubMed] [Google Scholar]
- 25.Fuchs D, Avanzas P, Arroyo-Espliguero R, Jenny M, Consuegra-Sanchez L, Kaski JC. The role of neopterin in atherogenesis and cardiovascular risk assessment. Curr Med Chem. 2009;16:4644–53. doi: 10.2174/092986709789878247. [DOI] [PubMed] [Google Scholar]
- 26.Chang HM, Lee HJ, Park HS, Kang JH, Kim KS, Song YS, et al. Effects of weight reduction on serum vaspin concentrations in obese subjects: modification by insulin resistance. Obesity (Silver Spring) 2010;18:2105–10. doi: 10.1038/oby.2010.60. [DOI] [PubMed] [Google Scholar]
- 27.Youn BS, Kloting N, Kratzsch J, Lee N, Park JW, Song ES, et al. Serum vaspin concentrations in human obesity and type 2 diabetes. Diabetes. 2008;57:372–7. doi: 10.2337/db07-1045. [DOI] [PubMed] [Google Scholar]
- 28.Kahn SE, Hull RL, Utzschneider KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature. 2006;444:840–6. doi: 10.1038/nature05482. [DOI] [PubMed] [Google Scholar]
- 29.Chung JO, Cho DH, Chung DJ, Chung MY. Associations among body mass index, insulin resistance, and pancreatic â-cell function in Korean patients with new-onset type 2 diabetes. Korean J Intern Med. 2012;27:66–71. doi: 10.3904/kjim.2012.27.1.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chaya MS, Ramakrishnan G, Shastry S, Kishore RP, Nagendra H, Nagarathna R, et al. Insulin sensitivity and cardiac autonomic function in young male practitioners of yoga. Natl Med J India. 2008;21:217–21. [PubMed] [Google Scholar]
- 31.Singh S, Kyizom T, Singh KP, Tandon OP, Madhu SV. Influence of pranayamas and yoga-asanas on serum insulin, blood glucose and lipid profile in type 2 diabetes. Indian J Clin Biochem. 2008;23:365–8. doi: 10.1007/s12291-008-0080-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Daga RA, Laway BA, Shah ZA, Mir SA, Kotwal SK, Zargar AH. High prevalence of vitamin D deficiency among newly diagnosed youth-onset diabetes mellitus in north India. Arq Bras Endocrinol Metabol. 2012;56:423–8. doi: 10.1590/s0004-27302012000700003. [DOI] [PubMed] [Google Scholar]
- 33.Forouhi NG, Ye Z, Rickard AP, Khaw KT, Luben R, Langenberg C, et al. Circulating 25-hydroxyvitamin D concentration and the risk of type 2 diabetes: results from the European Prospective Investigation into Cancer (EPIC)-Norfolk cohort and updated meta-analysis of prospective studies. Diabetologia. 2012;55:2173–82. doi: 10.1007/s00125-012-2544-y. [DOI] [PubMed] [Google Scholar]
- 34.Jorde R, Figenschau Y, Hutchinson M, Emaus N, Grimnes G. High serum 25-hydroxyvitamin D concentrations are associated with a favorable serum lipid profile. Eur J Clin Nutr. 2010;64:1457–64. doi: 10.1038/ejcn.2010.176. [DOI] [PubMed] [Google Scholar]


