Abstract
Background & objectives:
India is a large country with each State having distinct social, cultural and economic characteristics. Tobacco epidemic is not uniform across the country. There are wide variations in tobacco consumption across age, sex, regions and socio-economic classes. This study was conducted to understand the wide inequalities in patterns of smoking and smokeless tobacco consumption across various States of India.
Methods:
Analysis was conducted on Global Adult Tobacco Survey, India (2009-2010) data. Prevalence of both forms of tobacco use and its association with socio-economic determinants was assessed across States and Union Territories of India. Wealth indices were calculated using socio-economic data of the survey. Concentration index of inequality and one way ANOVA assessed economic inequality in tobacco consumption and variation of tobacco consumption across quintiles. Multiple logistic regression was done for tobacco consumption and wealth index adjusting for age, sex, area, education and occupation.
Results:
Overall prevalence of smoking and smokeless tobacco consumption was 13.9 per cent (14.6, 13.3) and 25.8 per cent (26.6, 25.0), respectively. Prevalence of current smoking varied from 1.6 per cent (richest quintile in Odisha) to 42.2 per cent (poorest quintile in Meghalaya). Prevalence of current smokeless tobacco consumption varied from 1.7 per cent (richest quintile in Jammu and Kashmir) to 59.4 per cent (poorest quintile in Mizoram). Decreasing odds of tobacco consumption with increasing wealth was observed in most of the States. Reverse trend of tobacco consumption was observed in Nagaland. Significant difference in odds of smoking and smokeless tobacco consumption with wealth quintiles was observed. Concentration index of inequality was significant for smoking tobacco -0.7 (-0.62 to-0.78) and not significant for smokeless tobacco consumption -0.15 (0.01to-0.33)
Interpretation & conclusions:
The findings of our analysis indicate that tobacco control policy and public health interventions need to consider widespread socio-economic inequities in tobacco consumption across the States in India.
Keywords: Control, India, socio-economic, tobacco
Tobacco has been identified as an important risk factor contributing to the burden of non-communicable diseases1. Control of tobacco epidemic in India is an issue of concern considering the enormity of population consuming tobacco2. Globally, India is the third largest tobacco producer and second largest tobacco consumer after China3. GATS (Global Adult Tobacco Survey) India reported tobacco consumption in more than one-third (35%) of adults in India4. Importantly, tobacco epidemic is not uniform across the country. Inequalities in tobacco consumption exist across age, sex, regions and economic classes5,6,7,8. Tobacco has also been identified as the single biggest cause of inequality in morbidity and mortality between rich and poor9. Tobacco consumption is disproportionately higher among lower socio-economic groups, which is visible in terms of lower age of initiation, more consumption and lower quit rates10,11,12.
Little effort has been done to understand the pattern of tobacco epidemic (socioeconomically and geographically) existing in various Indian States. Studies in past have combined both forms of tobacco consumption for analysis10,13,14 or have assessed smoking only15,16. Both forms of tobacco consumption result in nearly equivalent damage and control strategies of one form bear a significant impact on another. Understanding geographical pattern of tobacco consumption across income quintiles is essential for designing State specific strategies.
Material & Methods
The GATS 2009-2010 data were used for analysis conducted in the School of Public Health, Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh, India. The GATS conducted by Ministry of Health and Family Welfare in 2010 is a survey for systematically monitoring adult tobacco consumption and tracking key tobacco control indicators4. A nationally representative probability sample was used to provide national and States level estimates of tobacco use. This survey covered 29 States (including Delhi) and two Union Territories (UTs), Chandigarh and Puducherry representing 99.92 per cent of the total population of India. Nearly 69, 030 respondents aged 15 yr and above were covered in the survey using multi-stage probability sampling design. Eligible respondents were all non-institutionalized persons who were residing in the country and provided written informed consent to participate in the survey. Data were collected in pretested, validated questionnaires, translated in local Indian languages and modified to incorporate relevant questions. Prevalence of both forms of tobacco consumption and its association with socio-economic determinants was assessed across States and UTs.
Sampling design and weights: Following the standard methodology adopted in GATS, initial sample size for each region was 8,000 households4. At State/UT level, a minimum sample size of 2,000 for larger States and 1,500 for smaller-size States from North-East region was decided. Multistage sampling methodology was followed with the total target sample size of 70,802 households at the national level. Sample data were weighted to improve representativeness of the sample in terms of size, distribution and characteristics of study population. Overall response rate in the study was 91.8 per cent at the household and individual levels. Sample weights considered in the analysis were taken from GATS dataset, computed for every respondent individually.
Statistical analysis: About 221 respondents with incomplete data for assets were excluded from analysis. Current smoking and smokeless tobacco consumption were the dependent variables used in the process. Current smoking/smokeless tobacco consumption was defined in the study as use of any smoked/smokeless tobacco product, either daily or occasionally4 using the following questions: (i) ‘Do you currently smoke tobacco on a daily basis, less than daily, or not at all’, and (ii) ‘Do you currently use smokeless tobacco on a daily basis, less than daily, or not at all’. Former tobacco users were ever tobacco smokers or smokeless tobacco users who currently did not smoke or use any form of tobacco. Never tobacco users were adults who reported that they neither smoked nor used smokeless tobacco in their life time. Former tobacco users were excluded from analysis. Wealth quintile was assessed by household assets from GATS data 2009-2010 using Principal component analysis (PCA)17,18.
SPSS version 17.0 (SPSS Inc., Chicago, USA) was used for analysis. Concentration index of inequality was used for assessment of inequality of tobacco consumption among population ranked by wealth status measured19. Concentration index ranged from +1 to -1; with positive value suggesting pro-rich distribution and negative value suggesting pro-poor distribution. The concentration index was used in assessing inequalities in prevalence of risk factors, health outcomes, health care utilization and payments for health care20,21,22. One way ANOVA was used to compare on the within quintile variation of tobacco consumption. State-wise odds ratios for current smoking and smokeless tobacco consumption versus no tobacco consumption were computed using multiple logistic regression model adjusting for all other socio-demographic variables, e.g. age, sex, area, education status and occupation.
Results
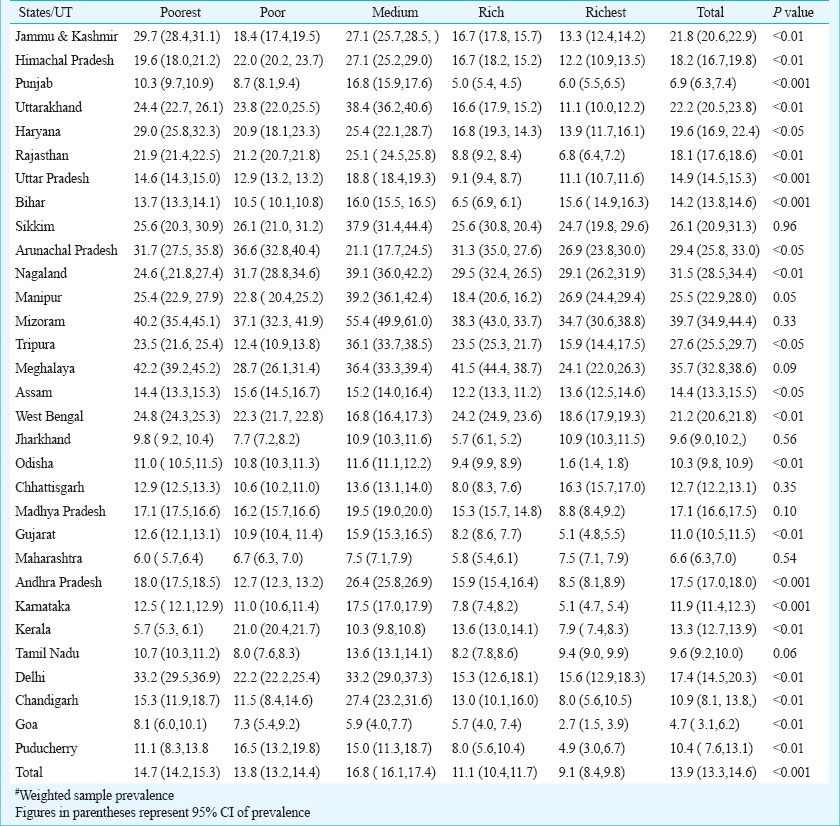
Prevalence of current smoking was analyzed across wealth quintiles in States and UTs as given in Table I. Across the States prevalence of current smoking varied from 1.6 per cent in Odisha (richest quintile) to 42.2 per cent (poorest quintile) in Meghalaya. In poorest quintile category, current smoking varied from 6 per cent in Maharashtra to 42.2 per cent in Meghalaya and in the richest quintile variation was from 1.6 per cent in Odisha to 34.7 per cent in Mizoram. Subjects in the medium wealth quintile reported higher prevalence of current smoking across all States (5.9% in Goa to 55.4% in Mizoram) (Table I). Reverse trend of smoking was observed in Nagaland where the rich and richest quintiles reported higher prevalence of smoking.
Table I.
Prevalence (%) of current smoking across wealth quintiles in States/Union Territories (UT) of India#
The prevalence of current smokeless tobacco consumption across wealth quintiles in States and UTs is given in Table II. Across States the prevalence of current smokeless tobacco consumption varied from 1.7 per cent in Jammu and Kashmir (richest quintile) to 59.4 per cent (poorest quintile) in Mizoram. In the poorest quintile, the smokeless tobacco consumption varied from 4.7 per cent in Himachal Pradesh to 59.4 per cent in Mizoram. In the richest quintile, variation was from 1.7 per cent in Jammu and Kashmir to 45.1 per cent in Nagaland. Significant difference in odds of smoking in the poorest class compared to richest was observed in States of Jammu and Kashmir, Himachal Pradesh, Uttarakhand, Haryana, Rajasthan, Nagaland, Odisha, Andhra Pradesh and Goa. Overall odds of smoking were significant across all wealth categories compared with the reference category. The decreasing odds of smoking with increasing wealth was observed in all States except Sikkim, Arunachal Pradesh, Nagaland, Mizoram, Tripura, West Bengal, Odisha, Chhattisgarh, Madhya Pradesh, Kerala, Chandigarh and Puducherry (Table III).
Table II.
Prevalence (%) of current smokeless tobacco consumption across wealth quintiles in states/Union Territories (UT) of India#
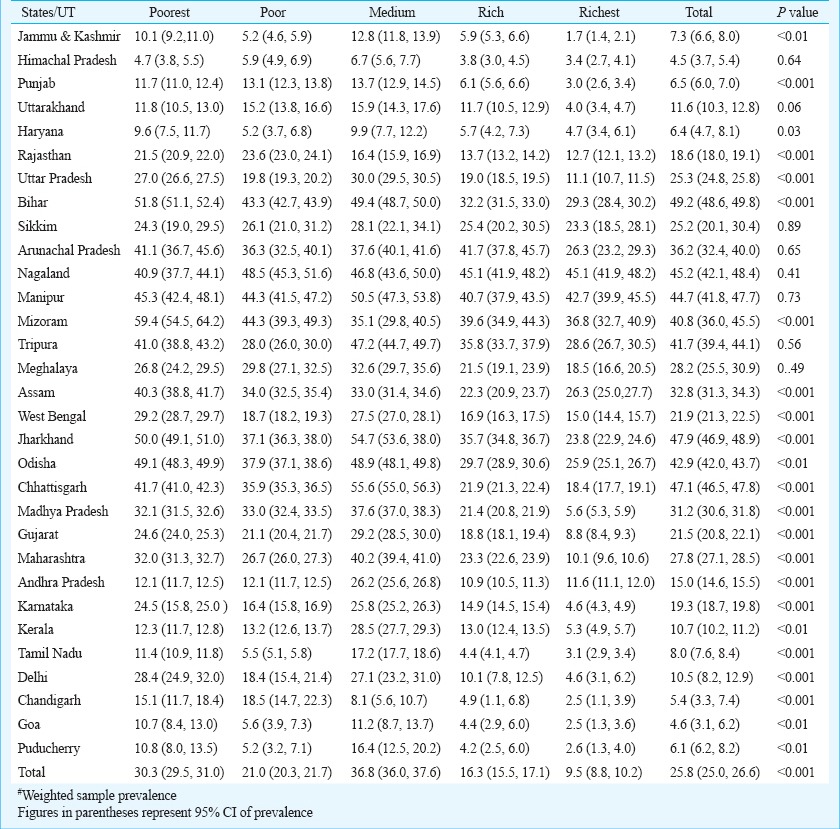
Table III.
Socio-economic predictor of current smoking among adults age 15 yr and above in States/Union Territories (UT) of India using logistic regression analysis: Global Adult Tobacco Survey, 2009-2010
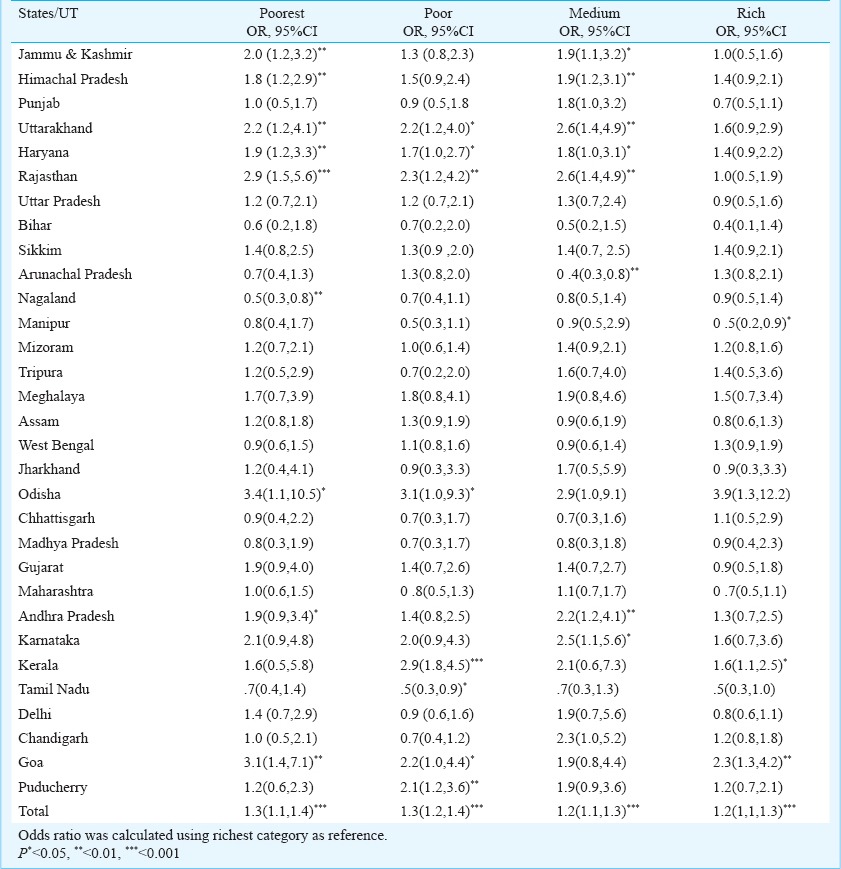
Significant difference in odds of smokeless tobacco consumption in the poorest compared to richest quintile was observed in the States of Jammu and Kashmir, Punjab, Delhi, Rajasthan, Uttar Pradesh, Bihar, Mizoram, Assam, Odisha, Chhattisgarh, Madhya Pradesh, Gujarat, Maharashtra, Karnataka and Goa. Overall in India, odds of smokeless tobacco consumption were significant across all wealth categories compared with the reference category. Decreasing odds of smokeless tobacco use with increasing wealth was observed in all States except Uttarakhand, Sikkim, Arunachal Pradesh, Nagaland, Manipur, Meghalaya, Andhra Pradesh and Kerala (Table IV).
Table IV.
Socio-economic predictor of current smokeless tobacco consumption among adults age 15 yr and above in States/Union Territories (UT) of India using logistic regression analysis: Global Adult Tobacco Survey, 2009-2010

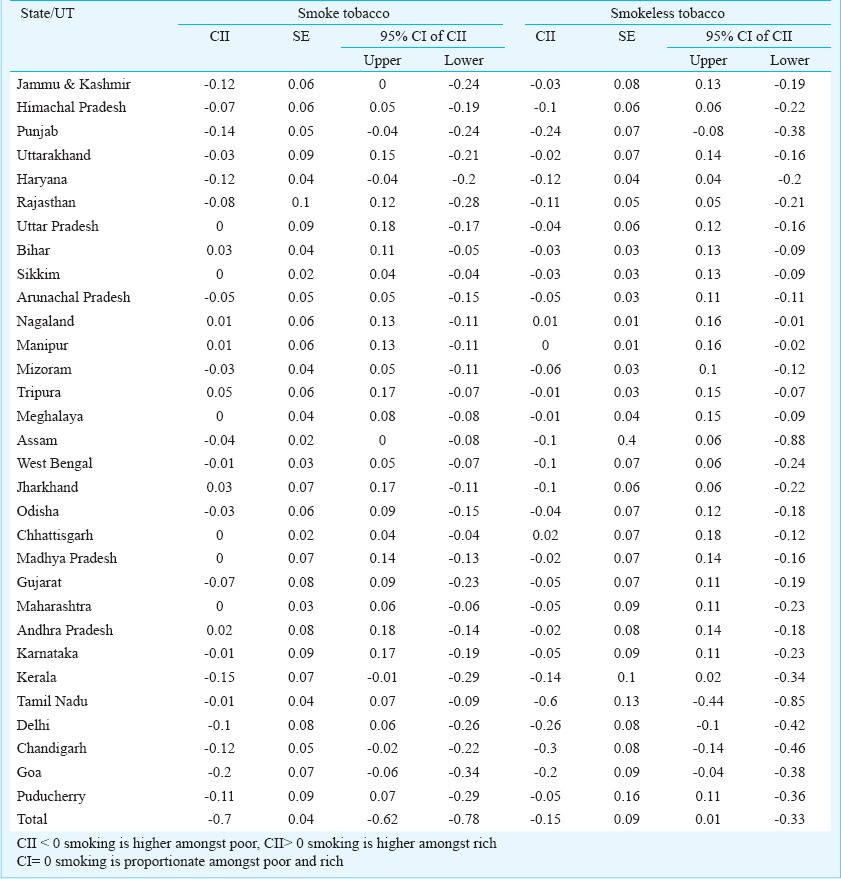
Concentration index of inequality calculated across States and UTs in India is shown in Table V. Overall, smoking was concentrated more among the poor in India, which was significant -0.7 (-0.62 to -0.78). Punjab, Haryana, Kerala, Chandigarh and Goa had significantly higher concentration of smoking among the poor population. Smoking was similar among rich and poor subjects in Sikkim, Meghalaya, Chhattisgarh, Madhya Pradesh and Maharashtra. Significantly more concentration of smoking among rich was observed in Bihar, Jharkhand, Andhra Pradesh and some North Eastern States, e.g. Nagaland, Manipur and Tripura. Consumption of smokeless tobacco was more by the poor class, however, it was not significant -0.15 (0.01 to -0.33). Significantly greater consumption was noted among rich in Nagaland. Manipur reported similar intake of smokeless tobacco across rich and poor sections of population.
Table V.
Concentration index of inequality (CII) for tobacco consumption in States and Union Territories of India
Discussion
India is a large country with each State having its own set of regional and cultural variations. Determinants of tobacco consumption have been studied extensively and socio- economic criterion had been identified as a significant predictor for the same. In this study significant socio-economic gradient of both forms of tobacco consumption was found across the States in India23.
Risk of smoking tobacco in the poorest quintile was more than the richest quintile across all States and UTs except Bihar, Nagaland and Tripura. Most of the States reported fall in smoking and smokeless tobacco consumption with rising wealth quintile barring a few exceptions. Most of the North Eastern States reported high consumption of smokeless tobacco and increase in consumption with rising wealth quintile.
In this analysis, economic determinants were studied as predictors of tobacco consumption. Social inequalities are both a factor and outcome of long term tobacco consumption. Tobacco often replaces essential expenditures of family and the resulting morbidity and mortality widen the gap further24.
Public policy and health promotion interventions (a part of the socio-political context) need to have an inequality perspective to have desired impact and accordingly modify tobacco control policies. Uniform population-based approach of health education had worsened social inequalities as major benefits are harnessed by upper economic classes25. Tobacco control measures that differentially target the poor include banning of advertisements, raising tobacco prices, work place interventions, free supply of cessation aids, and telephone help lines26. Taxation has been reported as the most effective policy measure to curb smoking epidemic in poor27. A 10 per cent increase in bidi prices cut down bidi consumption by 9.2 per cent3. However, taxes on tobacco products are very low especially for the products consumed by lower socio-economic class in India, e.g. bidis, open tobacco products, smokeless tobacco like gutkha, etc. Rational tobacco taxation measures should be adopted by eliminating regulatory distinctions between hand-made and machine-made bidis, removing exemptions to small producers and restricting availability of unbranded bidis28.
Tobacco cessation interventions are aimed to increase tobacco quit rates. Feasibility study on tobacco cessation clinics in India found that at six weeks, 14 per cent had gradually quit and 22 per cent had reduced their tobacco intake by 50 per cent or more29. A tobacco cessation clinic in Delhi reported continuous abstinence rate using medication and counselling to be 60, 58, 54, and 53 per cent at 1, 3, 6 and 12 months, respectively30. However, there was no long term follow up with methodological issues. Studies in West had shown that tobacco cessation advice provided by health professionals enhances quit rate31. However, significant barrier for tobacco cessation activities is lack of knowledge of the health effects of tobacco use32.
Addressing the inequalities in tobacco consumption did not necessitate introducing new set of interventions for tobacco control, but modifying the existing ones. Suitable policy initiatives could result in promoting appropriate interventions to address inequities through large scale public health programmes33. Integration of tobacco control with non-communicable disease control programme could address the problem holistically34.
The findings of this analysis have several limitations. Prevalence results were based on self-reports with no measure of validation applied. Former tobacco users were excluded from the logistic regression analysis. The proportion of former users and their distribution by socio-demographic variables might differ. Important inequalities of tobacco consumption based on other socio-demographic variables like age, gender, occupation, area, etc. were not considered for analysis. Data on frequency and length of smoking were not used in the analysis. Moreover, the reasons behind this pattern of tobacco consumption needed to be explored through qualitative research studies.
Overall, epidemiological evidence of wide economic inequalities in patterns of smoking and smokeless tobacco consumption could be seen across all States of India. Addressing these inequalities is necessary to achieve significant reductions in tobacco consumption in India.
Acknowledgment
Authors thank the Global Adult Tobacco Survey (GATS) study team for data support and World Health Organization, South East Asia Regional Office (WHO, SEARO), New Delhi for technical guidance. The views expressed in this article are solely those of the authors and do not necessarily represent the official position of GATS partner organizations.
References
- 1.World Health Organization. 2008-2013 action plan for the global strategy for the prevention and control of noncommunicable diseases: prevent and control cardiovascular diseases, cancers, chronic respiratory diseases and diabetes. 2008. [accessed on July 17, 2013]. Available from: http://whqlibdoc.who.int/publications/2009/9789241597418_eng.pdf .
- 2.Sarkar BK, Reddy KS. Priorities of tobacco control research in India. Addiction. 2012;107:2066–8. doi: 10.1111/j.1360-0443.2012.03942.x. [DOI] [PubMed] [Google Scholar]
- 3.John RM, Rao RK, Rao MG, Moare J, Deshpande RS, Sengupta J, et al. Paris: International Union against Tuberculosis and Lung Disease; 2010. [accessed on June 20, 2013]. The economics of tobacco and tobacco taxation in India. Available from: http://global.tobaccofreekids.org/files/pdfs/en/India_tobacco_taxes_report_en.pdf . [Google Scholar]
- 4.Ministry of Health and Family Welfare, Government of India. Global Adult Tobacco Survey (GATS), India, Report, 2009-2010. [accessed on June 20, 2013]. Available from: http://whoindia.org/en/Section20/Section25_1861.htm .
- 5.Subramanian S V, Nandy S, Kelly M, Gordon D, Davey Smith G, et al. Patterns and distribution of tobacco consumption in India: cross-sectional multilevel evidence from the 1998-9 national family health survey. BMJ. 2004;328:801–6. doi: 10.1136/bmj.328.7443.801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pampel FC, Denney JT. Cross-national sources of health inequality: education and tobacco use in the world health survey. Demography. 2011;48:653–74. doi: 10.1007/s13524-011-0027-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gupta R. Smoking, educational status and health inequity in India. Indian J Med Res. 2006;124:15–22. [PubMed] [Google Scholar]
- 8.Gupta B. Burden of smoked and smokeless tobacco consumption in India - results from the global adult tobacco survey India (GATS-India)- 2009-2010. Asian Pac J Cancer Prev. 2013;14:3323–9. doi: 10.7314/apjcp.2013.14.5.3323. [DOI] [PubMed] [Google Scholar]
- 9.Jarvis MJ, Wardle J. Social patterning of individual health behaviours: the case of cigarette smoking. In: Marmot M, Wilkinson RG, editors. Social determinants of health. 2nd ed. Oxford: Oxford University Press; 2006. pp. 224–37. [Google Scholar]
- 10.Harper S, McKinnon B. Global socioeconomic inequalities in tobacco use: internationally comparable estimates from the World Health Surveys. Cancer Causes Control. 2012;23(Suppl 1):11–25. doi: 10.1007/s10552-012-9901-5. [DOI] [PubMed] [Google Scholar]
- 11.Mathur C, Stigler MH, Perry CL, Arora M, Reddy KS. Differences in prevalence of tobacco use among Indian urban youth: the role of socioeconomic status. Nicotine Tob Res. 2008;10:109–16. doi: 10.1080/14622200701767779. [DOI] [PubMed] [Google Scholar]
- 12.Jha P, Peto R, Zatonski W, Boreham J, Jarvis MJ, Lopez AD. Social inequalities in male mortality, and in male mortality from smoking: indirect estimation from national death rates in England and Wales, Poland, and North America. Lancet. 2006;368:367–70. doi: 10.1016/S0140-6736(06)68975-7. [DOI] [PubMed] [Google Scholar]
- 13.Palipudi KM, Gupta PC, Sinha DN, Andes LJ, Asma S, McAfee T, et al. GATS Collaborative Group. Social determinants of health and tobacco use in thirteen low and middle income countries: evidence from global adult tobacco survey. PLoS One. 2012;7:e33466. doi: 10.1371/journal.pone.0033466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eek F, Ostergren PO, Diderichsen F, Rasmussen NK, Andersen I, Moussa K, et al. Differences in socioeconomic and gender inequalities in tobacco smoking in Denmark and Sweden; a cross sectional comparison of the equity effect of different public health policies. BMC Public Health. 2010;10:9. doi: 10.1186/1471-2458-10-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hosseinpoor AR, Parker LA, Tursan Espaignet E, Chatterji S. Socioeconomic inequality in smoking in low-income and middle-income countries: results from the World Health Survey. PLoS one. 2012;7:e42843. doi: 10.1371/journal.pone.0042843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nagelhout GE, de Korte-de Boer D, Kunst AE, van der Meer RM, de Vries H, van Gelder BM, et al. Trends in socioeconomic inequalities in smoking prevalence, consumption, initiation, and cessation between 2001 and 2008 in the Netherlands. Findings from a national population survey. BMC Public Health. 2012;12:303. doi: 10.1186/1471-2458-12-303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McKenzie DJ. Measuring inequality with asset indicators. J Popul Econ. 2005;18:229–60. [Google Scholar]
- 18.Vyas S, Kumaranayake L. Constructing socio-economic status indices: how to use principal components analysis. Health Policy Plan. 2006;21:459–68. doi: 10.1093/heapol/czl029. [DOI] [PubMed] [Google Scholar]
- 19.O’Donnell O, Van Doorslaer E, Wagstaff A, Lindelow M. Washington, DC: The World Bank; 2008. Analyzing health equity using household survey data a guide to techniques and their implementation. [Google Scholar]
- 20.Prinja S, Aggarwal AK, Kumar R R, Kanavos P. User charges in health care: evidence of effect on service utilization & equity from North India. Indian J Med Res. 2012;136:868–76. [PMC free article] [PubMed] [Google Scholar]
- 21.Prinja S, Kanavos P, Kumar R. Health care inequities in North India: Role of public sector in universalizing health care. Indian J Med Res. 2012;136:421–31. [PMC free article] [PubMed] [Google Scholar]
- 22.Prinja S, Kumar M, Pinto AD, Jan S, Kumar R. Equity in hospital services utilization in India. Econ Polit Wkly. 2013;48:52–8. [Google Scholar]
- 23.Sreeramareddy CT, Pradhan PM, Mir IA, Sin S. Smoking and smokeless tobacco use in nine South and Southeast Asian countries: prevalence estimates and social determinants from demographic and health surveys. Popul Health Metics. 2014;12:22. doi: 10.1186/s12963-014-0022-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Johnson NW, Warnakulasuriya S, Gupta PC, Dimba E, Chindia M, Otoh EC, et al. Global oral health inequalities in incidence and outcomes for oral cancer: causes and solutions. Adv Dent Res. 2011;23:237–46. doi: 10.1177/0022034511402082. [DOI] [PubMed] [Google Scholar]
- 25.Prinja S, Kumar R. Reducing health inequities in a generation: a dream or reality? Bull World Health Organ. 2009;87:84–4. doi: 10.2471/BLT.08.062695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kunst A, Giskes K, Mackenbach J. Socio-economic inequalities in smoking in the European Union. Applying an equity lens to tobacco control policies (2004) [accessed on July 16, 2013]. Available from: http://www.ensp.org/sites/default/files/ensp_socioeconomic_inequalities_in_smoking_in_eu.pdf .
- 27.Chaloupka FJ, Yurekli A, Fong GT. Tobacco taxes as a tobacco control strategy. Tob Control. 2012;21:172–80. doi: 10.1136/tobaccocontrol-2011-050417. [DOI] [PubMed] [Google Scholar]
- 28.Thakur JS, Garg R, Narain JP, Menabde N. Tobacco use: a major risk factor for non-communicable diseases in South East Asia region. Indian J Public Health. 2011;55:155–60. doi: 10.4103/0019-557X.89943. [DOI] [PubMed] [Google Scholar]
- 29.Varghese Cc, Kaur J, Desai NG, Murthy P, Malhotra S, Subbakrishna DK, et al., editors. Initiating tobacco cessation services in India: challenges and opportunities. WHO South-East Asia J Public Health. 2012;1:159–68. doi: 10.4103/2224-3151.206929. [DOI] [PubMed] [Google Scholar]
- 30.Kumar R, Kushwah AS, Mahakud GCc, Prakash S, Vijayan VK. Smoking cessation interventions and continuous abstinence rate at one year. Indian J Chest Dis Allied Sci. 2007;49:201–7. [Google Scholar]
- 31.Gorin SS, Heck JE. Meta-analysis of the efficacy of tobacco 31. counseling by health care providers. Cancer Epidemiol Biomarkers Prev. 2004;13:2012–22. [PubMed] [Google Scholar]
- 32.Murthy P, Saddichha S. Tobacco cessation services in India: recent developments and the need for expansion. Indian J Cancer. 2010;47(Suppl 1):69–74. doi: 10.4103/0019-509X.63873. [DOI] [PubMed] [Google Scholar]
- 33.Blas E, Sommerfeld J, Kurup AS. Geneva: World Health Organization; 2011. Social determinants approaches to public health: from concept to practice. [Google Scholar]
- 34.Thakur J, Prinja S, Garg CC, Mendis S, Menabde N. Social and economic implications of non-communicable diseases in India. Indian J Community Med. 2011;36(Suppl 1):S13–22. doi: 10.4103/0970-0218.94704. [DOI] [PMC free article] [PubMed] [Google Scholar]


