Abstract
Background:
Cognitive deficits are an important component of depression and may remain impaired after recovery from depression.
Objectives:
To evaluate the efficacy of cognitive rehabilitation in depression on cognitive dysfunction in the area of attention and memory.
Materials and Methods:
The study was hospital based pre- and post-intervention with follow-up assessment design. Selection of the depressive patients was by purposive sampling. The sample size consists of 30 intervention depressive patients included in the study after giving written informed consent. After preassessment, all patients underwent 15 sessions as part of cognitive rehabilitation. Postassessment was done to see the outcome of cognitive rehabilitation after 3 months follow-up.
Results:
After the intervention, there was significant improvement in attention and memory area. Along with these deficits, their basic living skills were also improved.
Conclusion:
Cognitive rehabilitation techniques are useful in remediating cognitive dysfunction in the area of attention and memory in patients with depression.
Keywords: Attention, cognitive rehabilitation, depression, memory
Cognitive Rehabilitation is a complex collection of technique that is designed to enhance perception, attention, comprehension, learning, remembering, problem solving and reasoning in individuals who are impaired in these areas.[1,2,3,4] Cognitive rehabilitation therapy is the art and science of restoring these mental processes and teaching compensatory strategies. While it is established that depression increases the risk of cognitive impairment, recent evidence suggests that cognitive dysfunction during remission increases the individuals’ vulnerability to onset, maintenance and recurrence of depression.[5,6,7,8] Depressive cognition consistently affects working memory, attention, and executive dysfunction.[8,9,10] Cognitive rehabilitation is useful in improving psychological functioning of the patient. The improvement in turns reduces the difficulties faced by the patient in his everyday interaction in the family, occupation, and society. In the past 20 years, cognitive rehabilitation has been used to reduce deficits in the areas of attention, memory, information processing, visuo-spatial perception, visuo-constructive abilities, planning and reasoning, mainly in patients with brain injuries, early stage dementia, schizophrenia, attention deficit hyperactivity disorder and mild intellectual impairment. However, a recent study reported that a new cognitive remediation treatment designed to treat residual depressive symptoms and for the 1st time, address cognitive impairment was associated with improvement in psychosocial functioning in patients of bipolar disorder with residual depressive symptoms.[11] In view of paucity of Indian reports in this area, the present work was undertaken to study the efficacy of cognitive rehabilitation of attention and memory in depressive patients.
MATERIALS AND METHODS
Sample
The sample comprised of depressive patients diagnosed on the basis of International Classification of Disease-10 diagnostic criteria for research criteria and with minimum 2 years duration of illness.[12] Patients were selected by purposive sampling technique from Department of Psychiatry Bokaro General Hospital Bokaro Steel City, Psychiatric Unit and Private Clinics of Bokaro. Only right-handed patients having basic reading and writing ability to understand the instructions given were included in the study. Patients having co-morbid psychiatric disorder, substance abuse, visual and hearing impairment, organic pathology, and significant physical illness were not included in the study.
Design
The study was hospital based pre - and post-intervention with follow-up assessment design.
Assessment tools used
Procedure
After screening according to inclusion and exclusion criteria, 30 depressive patients were included in study with their informed consent. The initial session included clinical interview and filling of sociodemographic and clinical data sheet. Annett's hand preference battery was used to screen handedness and only right-handed patient were selected. BDI was administered to assess the severity of depression. To assess the attention and concentration digit span test from WAIS-R (digit span test) was administered. WMS was administered to assess the memory. After preassessment, cognitive rehabilitation was given to the depressive patients [Appendix 1]. Initially, 15 sessions of cognitive rehabilitation package was given (which includes postassessment). Thereafter, postassessment was done to assess the outcome of rehabilitation after 3 months follow-up [Figure 1]. Scores of patients on digit span test and WMS before and after intervention were compared with the Student's t-test.
Figure 1.
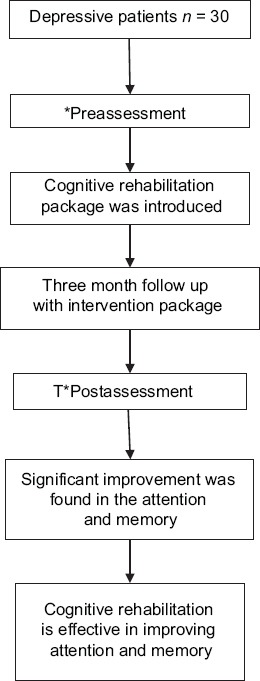
Plan of study [*Digit Span test (Wechsler Adult intelligence Test), Wechsler Memory Scale]
RESULTS
A total of 30 depression meeting the inclusion and exclusion criteria were included in the study with their informed consent. The age range of the patients included in the study was 20–60 years. Patients had been on psychiatric treatment that was continued during the study. The distribution of severity of depression based on scores on BDI was: Mild in 2 (6.66%) patients, moderate in 26 (86.66%) patients and severe in 2 (6.66%) patients.
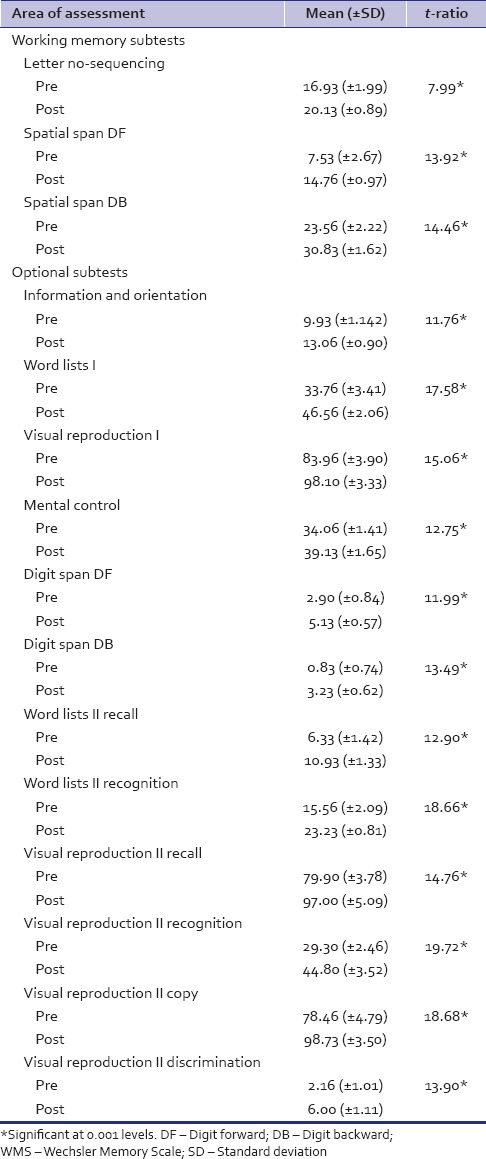
Scores of the depression patients on digit span test of WAIS-R before and after the Intervention are shown in Table 1. Pre- and post-intervention scores of immediate and delayed memory subtests along with working and optional memory subtests of WMS in depression patients are given in Tables 2 and 3 respectively.
Table 1.
Scores of the depression patients on digit span test of WAIS-R before and after the intervention
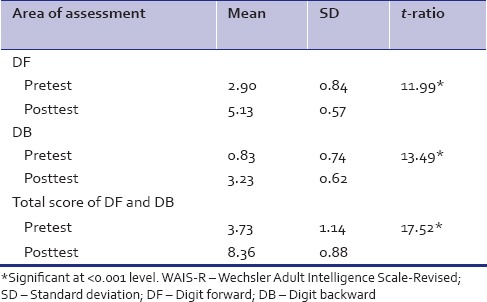
Table 2.
Pre- and post-intervention scores of immediate and delayed memory subtests of WMS in depression patients
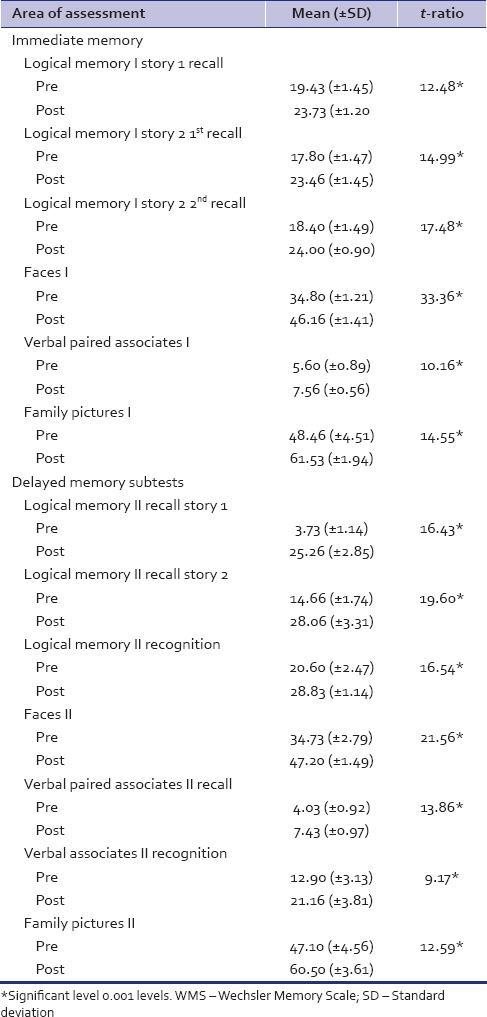
Table 3.
Pre- and post-intervention scores of working and optional memory subtests of WMS in depression patients
DISCUSSION
In the present study, the aim was to assess the improvement in cognitive functioning of the patient through cognitive remediation techniques. The main areas of intervention were: Attention and memory. Therefore a pretest was done to assess the level of sustain attention, selective attention, information and orientation, logical memory, verbal paired, visual reproduction, spatial span, mental control, and memory through appropriate test. After 3 months of regular intervention, a posttest was again done and all areas were again assessed through the same test, that is, as in pretest.
Results revels that there was a significant improvement in attention and concentration after the intervention, which can be explained as areas of brain mainly involved in attention are ascending reticular activation system (arousal/vigilance); superior colliculus (involuntary eye movement); pulvinar of thalamus (filtering and redirecting visual attention); cingulate cortex (executive effortful attention); parietal lobe (engage/disengage); frontal lobe (directing attention). Of these areas, sustained attention is the effort of right parietal and right frontal areas.[17] Experiment that require sustained attention with discrimination were found to activate and maintain activity in right-sided prefrontal (dorsolateral and ventrolateral) and parietal lobe.[18] The circuit mainly involved in it is frontal-striatal pathway connecting frontal lobe and help in maintaining an activity for a considerable period of time (La Berge triangular circuit of attention).[19] Of all these attentive processes, patients with depression have difficulty in sustaining attention. Therefore, deficits in sustained attention have been proposed as a vulnerability marker for depression.[20] The functional importance of this finding and the neuronal networks involved remain to be elucidated. Thus direct training involved repeated drills and exercises (based on the model of Parente and Parente model of attention)[21] of sustained attention has been targeted to strengthen the triangular circuit of attention involving dorsolateral prefrontal cortex, parietal lobe and Pulvinar, and it has been found to be fruitful in restoring the deficits of the patients.[19] Although the physiological mechanism behind the restoration is not known, but the technique has been found to be beneficial for the patients which is supported by another study which also reported that repeated practices is a viable method of cognitive remediation in patients with depression.[22]
The performance on WMS in pretest shows poor results on different areas of memory immediate memory (logical memory I, visual reproduction I, faces I, verbal paired associates I, family pictures I) which shows that during the phase of depression they are not able to remember information immediately after auditory and visual presentation. Also in delayed memory (logical memory II, visual reproduction II, faces II, verbal paired associates II, family pictures II), patients are not able to remember orally, auditory and visual information. In working memory, depressive patients are unable to remember and manipulate both visually and orally presented information in short-term memory (letter number sequencing, spatial span). This is consistent with the findings of an earlier study that reported that depressive patients have deficits in their ability to monitor the contents of working memory.[23] It has also been reported that depressed patients showed inability to inhibit neutral information access to working memory, restrain and delete irrelevant information.[24] However, there was a significant improvement found in the performance of the patients after the intervention that was targeted to remediate the areas that were deficient in the patients in the present study. This is consistent with the findings of a previous study that observed that patients who receive cognitive training improve on a range of neuropsychological tests targeting attention, verbal learning and memory, psychomotor speed, and executive function.[22] In the present study, comparison of the pretest and posttest scores revealed significant improvement in all the areas of memory. This finding is consistent with a recent observation that cognitive training in depressive disorders improves memory performance.[25]
Study limitations include the relatively low number of subjects due to time constraints and the lack of a control group. The current intervention package required a significant investment of time and human resources to deliver the therapeutic sessions that may not be available in other settings because of the requirement for trained therapist and cost. Future studies should include larger number of patients along with a control group. In addition, the contribution of individual components of the rehabilitation package to the outcome measures should be investigated because the present work only assessed the impact of the global rehabilitation protocol.
CONCLUSION
Depressive patients have severe cognitive deficits that may last for prolonged period despite treatment with medications and counseling. Cognitive rehabilitation provides a better scope for the patients with depression to show improvement in global functioning. The psychosocial rehabilitation of depressive patients should involve cognitive rehabilitation as it directly or indirectly strengthen the patient and motivate him for better performance that is, more the attention and memory capacity better the patient's performance.
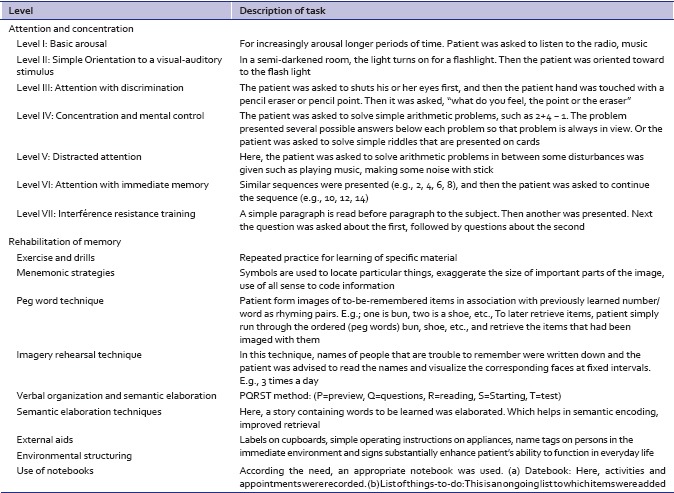
Appendix 1: Brief description of Cognitive rehabilitation package of attention, concentration (Seven-level Model of Attention Training, Parente and Anderson-Parente 1991) and memory
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Galletly C, Rigby A. An Overview of cognitive remediation therapy for people with severe mental illness. ISRN Rehabil 2013. 2013 984932. [Google Scholar]
- 2.Callahan CD. The traumatic brain injury act amendments of 2000. J Head Trauma Rehabil. 2001;16:210–3. doi: 10.1097/00001199-200104000-00009. [DOI] [PubMed] [Google Scholar]
- 3.Evans J, Over DE. East Sussex, UK: Psychology Press; 1996. Rationality and Reasoning. [Google Scholar]
- 4.Patten BM. The history of memory arts. Neurology. 1990;40:346–52. doi: 10.1212/wnl.40.2.346. [DOI] [PubMed] [Google Scholar]
- 5.Gotlib IH, Joormann J. Cognition and depression: Current status and future directions. Annu Rev Clin Psychol. 2010;6:285–312. doi: 10.1146/annurev.clinpsy.121208.131305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kessing LV. Course and Cognitive Outcome in Major Affective Disorders. Doctoral Thesis. Lægeforeningens Forlag, Copenhagen. 2001 [Google Scholar]
- 7.Paelecke-Habermann Y, Pohl J, Leplow B. Attention and executive functions in remitted major depression patients. J Affect Disord. 2005;89:125–35. doi: 10.1016/j.jad.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 8.Papazacharias A, Nardini M. The relationship between depression and cognitive deficits. Psychiatr Danub. 2012;24(Suppl 1):S179–82. [PubMed] [Google Scholar]
- 9.Doumas M, Smolders C, Brunfaut E, Bouckaert F, Krampe RT. Dual task performance of working memory and postural control in major depressive disorder. Neuropsychology. 2012;26:110–8. doi: 10.1037/a0026181. [DOI] [PubMed] [Google Scholar]
- 10.Elderkin-Thompson V, Moody T, Knowlton B, Hellemann G, Kumar A. Explicit and implicit memory in late-life depression. Am J Geriatr Psychiatry. 2011;19:249–55. doi: 10.1097/JGP.0b013e3181e89a5b. [DOI] [PubMed] [Google Scholar]
- 11.Deckersbach T, Nierenberg AA, Kessler R, Lund HG, Ametrano RM, Sachs G, et al. Research: Cognitive rehabilitation for bipolar disorder: An open trial for employed patients with residual depressive symptoms. CNS Neurosci Ther. 2010;16:298–307. doi: 10.1111/j.1755-5949.2009.00110.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Geneva: WHO; 1993. World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders, Diagnostic Criteria for Research. [Google Scholar]
- 13.Annett M. A classification of hand preference by association analysis. Br J Psychol. 1970;61:303–21. doi: 10.1111/j.2044-8295.1970.tb01248.x. [DOI] [PubMed] [Google Scholar]
- 14.Beck AT, Steer RA, Garbin MG. Psychometric properties of the BDI: Twenty five of evaluation. Clin Psychol Rev. 1988;8:77–100. [Google Scholar]
- 15.Wechsler D. New York: Psychological Corporation; 1981. Manual for the Wechsler Adult Intelligence Scale-Revised. [Google Scholar]
- 16.Wechsler D. San Antonio, TX: Harcourt Assessment; 1997. Wechsler Memory Scale – Third Edition (WMS-III) [Google Scholar]
- 17.Posner MI, Petersen SE. The attention system of the human brain. Annu Rev Neurosci. 1990;13:25–42. doi: 10.1146/annurev.ne.13.030190.000325. [DOI] [PubMed] [Google Scholar]
- 18.Coull JT, Frackowiak RS, Frith CD. Monitoring for target objects: Activation of right frontal and parietal cortices with increasing time on task. Neuropsychologia. 1998;36:1325–34. doi: 10.1016/s0028-3932(98)00035-9. [DOI] [PubMed] [Google Scholar]
- 19.LaBerge D. Cambridge, MA: Harvard University Press; 1995. Attentional Processing: The Brain's Art of Mindfulness. [Google Scholar]
- 20.Weiland-Fiedler P, Erickson K, Waldeck T, Luckenbaugh DA, Pike D, Bonne O, et al. Evidence for continuing neuropsychological impairments in depression. J Affect Disord. 2004;82:253–8. doi: 10.1016/j.jad.2003.10.009. [DOI] [PubMed] [Google Scholar]
- 21.Parente R, Anderson-Parente JK. Houston, Tx: CSY Publishers; 1991. Retraining Memory: Technique and Applications. [Google Scholar]
- 22.Elgamal S, McKinnon MC, Ramakrishnan K, Joffe RT, MacQueen G. Successful computer-assisted cognitive remediation therapy in patients with unipolar depression: A proof of principle study. Psychol Med. 2007;37:1229–38. doi: 10.1017/S0033291707001110. [DOI] [PubMed] [Google Scholar]
- 23.Thompson JM, Gray JM, Hughes JH, Watson S, Young AH, Ferrier IN. Impaired working memory monitoring in euthymic bipolar patients. Bipolar Disord. 2007;9:478–89. doi: 10.1111/j.1399-5618.2007.00470.x. [DOI] [PubMed] [Google Scholar]
- 24.Gohier B, Ferracci L, Surguladze SA, Lawrence E, El Hage W, Kefi MZ, et al. Cognitive inhibition and working memory in unipolar depression. J Affect Disord. 2009;116:100–5. doi: 10.1016/j.jad.2008.10.028. [DOI] [PubMed] [Google Scholar]
- 25.Naismith SL, Redoblado-Hodge MA, Lewis SJ, Scott EM, Hickie IB. Cognitive training in affective disorders improves memory: A preliminary study using the near approach. J Affect Disord. 2010;121:258–62. doi: 10.1016/j.jad.2009.06.028. [DOI] [PubMed] [Google Scholar]


