Abstract
Malignant perivascular epithelioid cell tumor (malignant PEComa) is a rare disease for which the diagnostic criteria and treatment options have not been established. Since PEComa is associated with upregulation of mammalian target of rapamycin (mTOR) pathway which controls Glut-1 (glucose transporter) function, increased 18F-fluorodeoxyglucose (18F-FDG) uptake may indicate the over activation of mTOR pathway and may guide selectively inhibiting mTOR pathway treatment. We report a malignant PEComa patient who presented for 18F-FDG positron emission tomography/computed tomography (PET/CT) restaging. The tumor had shown significant avidity on PET/CT as well as an evident response to sirolimus (rapamycin, Rapamune™) that supports the utility of mTOR inhibitors as an effective treatment for malignant PEComa. Therefore, 18F-FDG PET/CT is helpful in restaging and guiding treatment for malignant PEComa with mTOR inhibitors.
Keywords: malignant perivascular epithelioid cell tumor, PEComa, mTOR inhibitor, FDG, PET/CT
Introduction
Perivascular epithelioid cell tumor (PEComa) is a mesenchymal tumor composed of distinctive cells that show a focal association with blood vessel walls and usually express melanocytic and smooth muscle markers.1 PEComa arising at soft-tissue and visceral sites is rare, with approximately 200 reported cases worldwide. Approximately one-third of the PEComas show locally aggressive behavior, and are called “malignant PEComa”.2 Since few cases have been reported, there is still no consensus about imaging/pathology diagnostic characteristics, staging/restaging, and treatment options for the management of malignant PEComa.1,3 PEComa is driven by a tuberous sclerosis complex gene mutation causing upregulation of mammalian target of rapamycin (mTOR) pathway. Selectively inhibiting mTOR pathways has shown efficiency in malignant PEComa.4 Meanwhile, mTOR pathway controls multiple cellular processes, especially Glut-1 (glucose transporter) function.5 Therefore, 18F-fluorodeoxyglucose positron emission tomography/computed tomography (18F-FDG PET/CT) may have potential in diagnosing, staging/restaging, and guiding treatment of malignant PEComa with mTOR inhibitors by detecting the increased glucose metabolism in tumor. To our knowledge, no report has been published about the role of 18F-FDG PET/CT in patients with malignant PEComa treated with mTOR inhibitors. In this report, we present a case of malignant uterus PEComa with intense FDG uptake in disseminating metastatic foci, successfully treated with sirolimus (rapamycin, Rapamune™), an mTOR inhibitor.
Case report
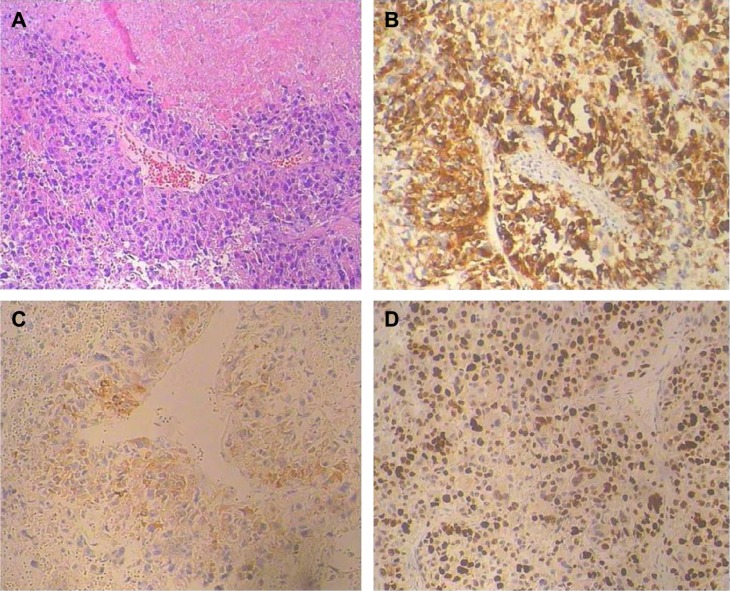
A 46-year-old female presented to our institution with solitary renal and pulmonary lesions 2 years after the initial diagnosis of uterine leiomyosarcoma. Left nephrectomy and right lower lung lobe wedge resection were performed. Histological and immunohistochemical analysis of the renal and pulmonary lesions, in addition to retrospective re-evaluation of the initial uterine tumor, led to the final diagnosis of malignant uterine PEComa with late renal and pulmonary metastases. Pulmonary metastases from malignant uterine PEComa display nests of epithelioid cells with small round nuclei surrounding thin-walled capillary vessels (Figure 1A). Tumor shows diffusely positive staining for melanocytic marker and smooth muscle marker (Figure 1B and C). A high Ki-67 labeling index of 40% indicates the aggressive behavior of the tumor (Figure 1D).
Figure 1.
Pathological findings of the pulmonary metastases from malignant uterine PEComa.
Notes: (A) Hematoxylin and eosin stain, magnification ×100. (B and C) HMB-45 and SMA immunohistochemical stain, magnification ×200. (D) Ki-67 immunohistochemical stain, magnification ×200. The average Ki-67 labeling index is 40% in this tumor. Background staining was identified by negative controls in which the sections were performed by substitution of primary antibodies with phosphate buffer solution.
Abbreviations: HMB-45, human melanoma black 45; PEComa, perivascular epithelioid cell tumor; SMA, smooth muscle actin.
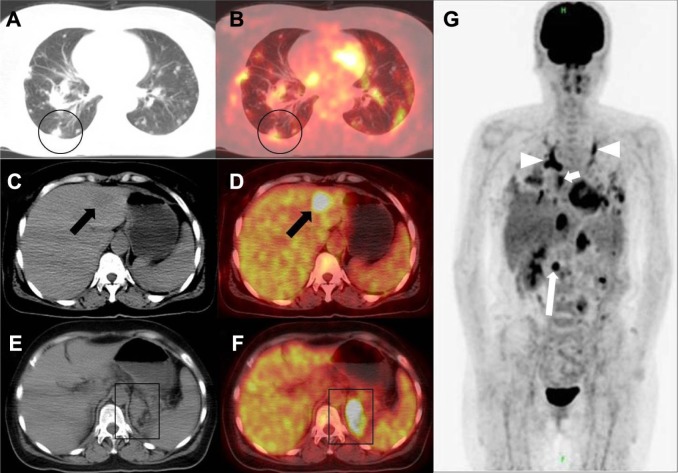
18F-FDG PET/CT scan was performed 1 month after pulmonary and kidney surgery to restage the disease. The PET/CT imaging showed bilateral multiple pulmonary metastases with maximum standardized uptake value (SUVmax) of 6.5 (circles in Figure 2A and B), liver metastases with SUVmax of 12.1 (arrows in Figure 2C and D), metastatic foci growing from previous left kidney bed with SUVmax of 7.3 (boxes in Figure 2E and F). In addition, whole body FDG PET showed multiple distant metastases, including the disseminating tumor emboli with intense FDG uptake (Figure 2G).
Figure 2.
The 18F-FDG PET/CT scans of the patient.
Notes: (A and B) Axial CT image in the lung window and axial PET/CT fusion image at the level of inferior pulmonary vein. Circles: pulmonary metastases. (C and D) Axial CT image in the abdominal window and axial PET/CT fusion image at the level above hepatic portal. Arrows: liver metastases. (E and F) Axial CT image in the abdominal window and axial PET/CT fusion image at the level of hepatic portal. Boxes: metastatic foci growing from previous left kidney bed. (G) Maximum intensity projection image 18F-FDG PE T showed tumor emboli in bilateral upper pulmonary artery (arrowheads), left atrium (short arrow), and inferior vena cava (long arrow).
Abbreviations: CT, computed tomography; FDG, fluorodeoxyglucose; PET, positron emission tomography.
The patient was treated with sirolimus (rapamycin, Rapamune™; Wyeth, Madison, NJ, USA), an inhibitor of mTOR. Serial CT scans were performed to monitor the treatment response. The follow-up axial CT images (Figure 3A and B) showed that the pulmonary metastatic foci were gradually diminishing and eliminating. A favorable and sustained response was observed at 7 months after the PET/CT scanning. The patient continued using the mTOR inhibitors untill the last follow-up. Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Figure 3.
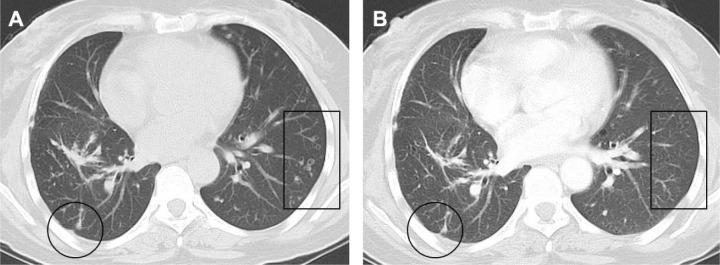
Follow-up CT scans of the patient.
Notes: (A) Partial response was observed by CT at 3 month after the initiation of the mTOR inhibitor treatment. For example, the size of the largest lesion in lung was reduced from 9 to 4 mm (circle). Some other pulmonary metastases were cavitated (box). (B) Nearly complete response was observed by CT at 7 months after the initiation of the mTOR inhibitor treatment. Fibrosis was observed at the largest pulmonary metastatic focus (circle). No other residual lesion was discernible (box).
Abbreviations: CT, computed tomography; mTOR, mammalian target of rapamycin.
Discussion
The PEComa family includes lymphangioleiomyomatosis, angiomyolipoma, clear cell sugar tumor of the lung; and a group of histologically and immunophenotypically similar tumors arising at a variety of soft-tissue and visceral sites. PEComas other than lymphangioleiomyomatosis and angiomyolipoma are rare, especially “malignant PEComa” which is accounting for one-third of the PEComa. The consensus about the diagnostic criteria and treatment options for malignant PEComa have not been established.1
18F-FDG PET/CT has shown the potential role in differentiating malignant and benign PEComas.2,6–13 Previous reports have shown that all the malignant PEComas (n=4) presented with intense FDG uptake at both primary lesions and metastatic foci with SUVmax ranging from 3.19 to 72.2,6–8 However, 55 out of 62 benign PEComas have exhibited low or negative FDG uptake on PET imaging with SUVmax lower than 2.0.9–13 Since PEComa is driven by tuberous sclerosis complex gene mutation causing upregulation of mTOR pathway which controls multiple cellular processes, including Glut-1 function,5 high FDG uptake in malignant PEComa could reflect over activation of mTOR pathway and is useful for staging/restaging in clinic.
Pretreatment FDG PET/CT has shown the ability in predicting outcome of treatment with chemotherapy, radiotherapy, and targeted therapy in variable cancer. In general, the patients with higher FDG uptake were associated with poorer prognosis compared to those with lower FDG uptake. Similarly, malignant PEComa patients with intense FDG uptake in previous case reports all failed to chemo- or radiotherapy.6,7 For example, Ciarallo et al reported a malignant PEComa revealed by FDG PET/CT that were resistant to radiotherapy, chemotherapy, and imatinib mesylate.7 At the same time, prior studies demonstrated that mTOR inhibitors such as sirolimus may be recommended in this rare disease type.4,5 Based on these evidences, the patient was treated with mTOR inhibitor and got a nearly complete clinical response. Hence, we presumed that if increased glucose metabolism in malignant PEComa was linked with the upregulation of mTOR pathway, high FDG uptake may suggest that targeting on inhibiting mTOR pathway would be an effective treatment as shown in our case. However, one case from Dickson et al’s study, the only case as far as we knew, showed resistance to sirolimus although with avid FDG uptake.14 Indeed, it still needs more patients to establish a general statement. Further studies are required with functional imaging including FDG PET/CT to understand the determinants of response and mechanisms of acquired resistance.
Conclusion
18F-FDG PET/CT is helpful in staging/restaging for malignant PEComa and guiding treatment with mTOR inhibitors.
Acknowledgments
This work is supported by grants (NSFC 81272502, ZR2014YL033, and 2014WS0030).
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Hornick JL, Pan CC. PEComa. In: Fletcher CD, Bridge J, Hogendoorn P, Mertens F, editors. World Health Organization Classification of Tumours of Soft Tissue and Bone. 4th ed. Lyon: International Agency for Research on Cancer; 2013. pp. 230–231. [Google Scholar]
- 2.Armah HB, Parwani AV. Malignant perivascular epithelioid cell tumor (PEComa) of the uterus with late renal and pulmonary metastases: a case report with review of the literature. Diagn Pathol. 2007;2:45. doi: 10.1186/1746-1596-2-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tirumani SH, Shinagare AB, Hargreaves J, et al. Imaging features of primary and metastatic malignant perivascular epithelioid cell tumors. AJR Am J Roentgenol. 2014;202(2):252–258. doi: 10.2214/AJR.13.10909. [DOI] [PubMed] [Google Scholar]
- 4.Wagner AJ, Malinowska-Kolodziej I, Morgan JA, et al. Clinical activity of mTOR inhibition with sirolimus in malignant perivascular epithelioid cell tumors: targeting the pathogenic activation of mTORC1 in tumors. J Clin Oncol. 2010;28(5):835–840. doi: 10.1200/JCO.2009.25.2981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Benson C, Vitfell-Rasmussen J, Maruzzo M, et al. A retrospective study of patients with malignant PEComa receiving treatment with sirolimus or temsirolimus: the Royal Marsden Hospital experience. Anticancer Res. 2014;34(7):3663–3668. [PubMed] [Google Scholar]
- 6.Navarro-Pelayo Lainez MM, Ramos-Font C, Rebollo Aguirre AC, Rodriguez-Fernandez A, Llamas-Elvira JM. Perivascular epithelioid tumors: Utility of the positron emission tomography with 18F-fluorodesoxyglucose (PET-TAC FDG) in their staging and follow-up. Rev Esp Med Nucl. 2010;29(5):258–262. doi: 10.1016/j.remn.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 7.Ciarallo A, Makis W, Hickeson M, Derbekyan V. Malignant perivascular epithelioid cell tumor (PEComa) of the uterus: serial imaging with F-18 FDG PET/CT for surveillance of recurrence and evaluation of response to therapy. Clin Nucl Med. 2011;36(4):e16–e19. doi: 10.1097/RLU.0b013e31820ae032. [DOI] [PubMed] [Google Scholar]
- 8.Rakheja R, Abikhzer G, Alabed YZ, Nahal A, Lisbona R. The appearance of osseous PEComa on F-18 FDG PET/CT. Clin Nucl Med. 2012;37(2):190–192. doi: 10.1097/RLU.0b013e31823e9aec. [DOI] [PubMed] [Google Scholar]
- 9.Welling RD, Lungren MP, Coleman RE. Extrarenal retroperitoneal angiomyolipoma mimicking metastatic melanoma: CT and FDG PET correlation. Clin Nucl Med. 2012;37(7):705–706. doi: 10.1097/RLU.0b013e3182443c7d. [DOI] [PubMed] [Google Scholar]
- 10.Ho CL, Chen S, Ho KM, et al. Dual-tracer PET/CT in renal angiomyolipoma and subtypes of renal cell carcinoma. Clin Nucl Med. 2012;37(11):1075–1082. doi: 10.1097/RLU.0b013e318266cde2. [DOI] [PubMed] [Google Scholar]
- 11.Young LR, Franz DN, Nagarkatte P, et al. Utility of [18F]2-fluoro-2- deoxyglucose-PET in sporadic and tuberous sclerosis-associated lymphangioleiomyomatosis. Chest. 2009;136(3):926–933. doi: 10.1378/chest.09-0336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dong A, Wang Y, Zuo C. Synchronous pure epithelioid angiomyolipoma of the kidney and retroperitoneal schwannoma in the same patient on 18F-FDG PET/CT imaging. Clin Nucl Med. 2013;38(2):e98–e100. doi: 10.1097/RLU.0b013e31825b2218. [DOI] [PubMed] [Google Scholar]
- 13.Kumasaka S, Arisaka Y, Tokue A, Higuchi T, Nakajima T, Tsushima Y. A case of multiple hepatic angiomyolipomas with high (18) F-fluorodeoxyglucose uptake. BMC Med Imaging. 2014;14:17. doi: 10.1186/1471-2342-14-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dickson MA, Schwartz GK, Antonescu CR, Kwiatkowski DJ, Malinowska IA. Extrarenal perivascular epithelioid cell tumors (PEComas) respond to mTOR inhibition: clinical and molecular correlates. Int J Cancer. 2013;132(7):1711–1717. doi: 10.1002/ijc.27800. [DOI] [PMC free article] [PubMed] [Google Scholar]