Abstract
Objectives: Peroxiredoxin 4 (Prx 4) is a newly emerging antioxidant protein that has been studied in several human cancers. Recently, it was revealed that Prx 4 is highly expressed in human lung cancer and is needed for the promotion of lung cancer progression in vitro. However, there are no clinical data regarding the association of Prx 4 and prognosis in lung cancer. Materials and methods: The Prx 4 expression state as a prognostic indicator was assessed by immunohistochemical staining in 142 patients with stage II non-small cell lung cancer (NSCLC) who had undergone curative surgery between 2006 and 2010. The association between the degree of Prx 4 expression and several clinicopathologic parameters was then evaluated by statistical analyses. Results: The degree of Prx 4 expression was associated with histology and recurrence in the overall NSCLC patient group, with the proportion of patients with positive Prx 4 expression significantly higher for the adenocarcinoma subtype (39/70, 56%) than the squamous cell carcinoma subtype (23/72, 32%) (P = 0.004). However, when subgroup analyses according to histopathology were performed in terms of recurrence, positive Prx 4 expression was significantly correlated with higher recurrence rates (P = 0.003) and shorter disease-free survival (DFS) (P = 0.003, hazard ratio = 3.910) in patients with squamous cell carcinoma. In contrast, no meaningful relationship was observed between the level of Prx 4 expression and DFS in the adenocarcinoma subgroup. Conclusion: Positive Prx 4 expression is significantly correlated with recurrence and shorter DFS in patients with early-stage lung squamous cell carcinoma.
Keywords: Lung cancer, peroxiredoxin, immunohistochemistry
Introduction
Lung cancer is the most common cause of cancer death worldwide, with an estimated 228,190 newly diagnosed cases in the United states in 2013 [1]. Approximately 85% to 90% of lung cancer cases are of non-small cell lung cancer (NSCLC), of which the main types are adenocarcinoma and squamous cell carcinoma. The prognosis is poor, with an overall 5-year survival rate for NSCLC (all stages combined) of less than 15% [2]. Although early-stage NSCLC may be cured by surgical resection, the recurrence rates are high, possibly due to early metastasis [3,4]. Hence, it is important to identify biological markers that are predictive of poor outcomes for early pertinent treatment.
Many carcinogens are known to induce formation of DNA adducts and the accumulation of oxygen-free radicals, which cause oxidative stress that leads to tumorigenesis, cancer progression and metastasis [5]. Meanwhile, cancer cells show an increased defense mechanism featuring higher expression of antioxidant proteins [6]. Peroxiredoxins (Prxs) have recently drawn attention as a new family of thiol-specific antioxidant proteins that play a crucial role in peroxide detoxification by using reducing equivalents provided through the thioredoxin system [7-10]. There are six isoforms of Prx in mammalian cells, Prx 1 to Prx 6. Of these, Prx 4 is an antioxidant enzyme mainly localized in the endoplasmic reticulum (ER) within cells [11,12]. Its antioxidant function is via the cysteine residue, which is oxidized to sulfenic acid form, and then, reduced by thioredoxin. However, under oxidative stress conditions, Prx 4 can be hyperoxidized and loses its antioxidant properties, which can only be reduced by sulfiredoxin (Srx) [13-15]. Then, instead, it may function as a molecular chaperone that facilitates protein folding [16,17]. Recently, Wei et al [18]. revealed that Srx and Prx 4 are highly expressed in human lung cancer cells from squamous cell carcinoma and adenocarcinoma and that Srx preferentially binds to Prx 4, so that Srx-Prx 4 complex significantly contributes to the maintenance of the tumor cell phenotype (anchorage-independent colony formation, cell migration, and invasion of lung cancer cells) in vitro and the formation of metastases in vivo (mouse xenograft) through positive regulation of specific phosphokinase signaling cascades including the AP-1/MMP 9 axis, CREB, and MAPK pathways. Furthermore, many researches have been in progress recently concerning the associations between Prx 4 and cancer progression in various cancers, including ovarian cancer, oral cavity squamous cell carcinoma, and breast cancer [19-21]. However, there are no clinical data on the correlation between Prx 4 and prognosis in lung cancer.
We therefore examined the association between the level of Prx 4 expression and prognosis in patients with early-stage NSCLC who underwent curative surgical resection.
Materials and methods
Patients and clinicopathologic data
Institutional Review Board approval was obtained to use the relevant human archival tissues to investigate the immunohistochemical (IHC) expression of Prx 4. A total of 142 cases of patients with stage II NSCLC who had undergone complete surgical resection at Asan Medical Center (Seoul, Korea) between 2006 and 2010 were chosen from the archives of the Department of Pathology and tissue arrays were prepared. All available histological slides, which had been routinely stained with hematoxylin and eosin (H&E), were reviewed.
All information about staging or clinicopathologic characteristics was complete and tissue specimens were available for all 142 patients. Data was collected on patient demographics, smoking history, type of surgery, histopathologic diagnosis, grade of differentiation, tumor stage, date of diagnosis, date of recurrence, date of death (or last follow-up), and whether each patient received adjuvant therapy (chemotherapy and/or radiotherapy) or not. In the process, cases of the patients who had experienced non-lung cancer related death were excluded. Tumor stages were assessed according to the AJCC Cancer Staging Manual, 7th edition [22].
Specimen preparation and IHC staining
IHC staining was performed on formalin-fixed, paraffin-embedded tissue sections using an automated IHC staining device (Benchmark XT; Ventana Medical Systems, Tucson, AZ) (Figure 1). Briefly, 4 um-thick whole tissue sections were transferred onto poly-L-lysine-coated adhesive slides and dried at 74°C for 30 min. After standard heat epitope retrieval for 1 h in ethylene diamine tetraacetic acid (EDTA), pH 8.0, in the autostainer, samples were incubated with antibodies against human Prx 4 antibody (1:100 dilution, rabbit polyclonal, AbFrontier, Seoul, South Korea). Sections were subsequently incubated with an OptiView Universal DAB kit (Ventana Medical Systems). Slides were counterstained with Harris hematoxylin. They were evaluated separately by 2 independent experienced pathologists (J.S., Y.P.) with good agreement (Cohen’s ĸ = 0.696, P < 0.001).
Figure 1.
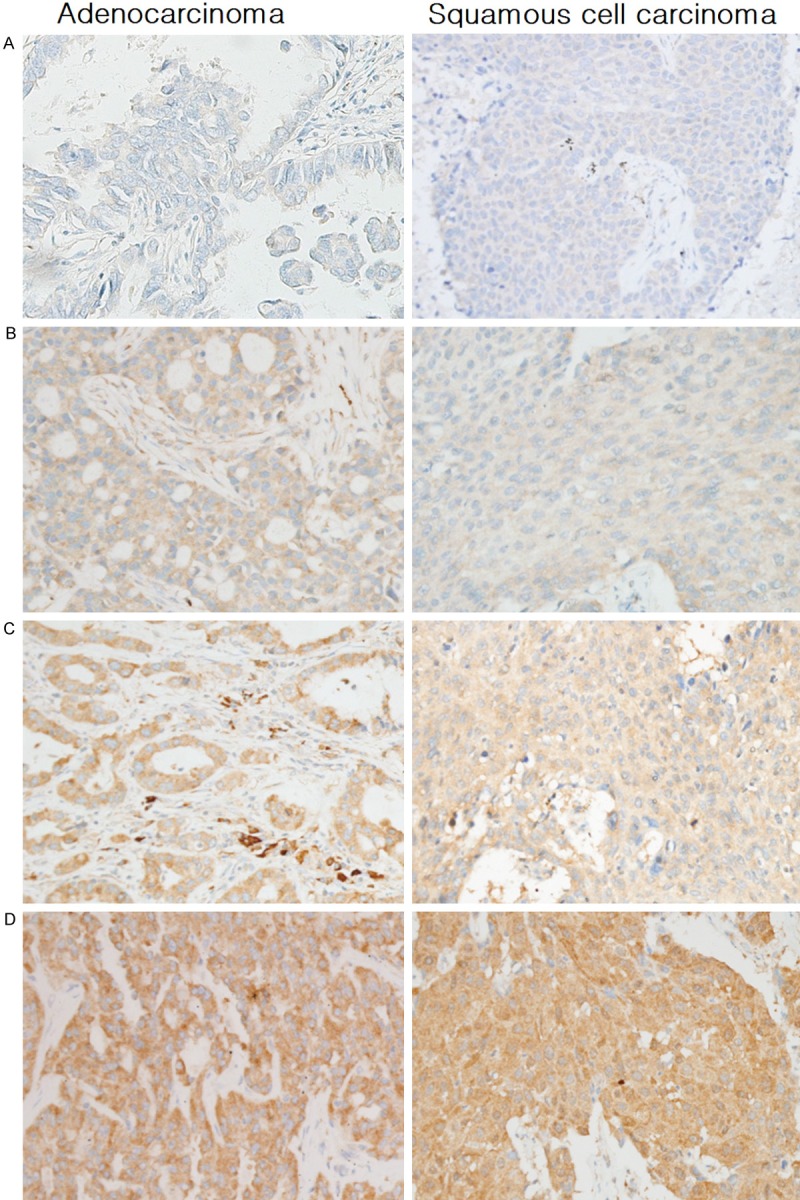
Representative photomicrographs of Prx 4 immunohistochemical staining in arrayed NSCLC tissues. The left and right columns show samples of adenocarcinoma and squamous cell carcinoma representing (A) 0, negative, (B) 1+, weak, (C) 2+, moderate, (D) 3+, strong immunoreactivity in tumor cells, respectively. Original magnification: ×200. Prx 4 was not expressed in normal alveolar or bronchial epithelial cells. Normal bronchial epithelial cell image (Figure S1), negative and positive control cell images (Figure S2) were provided in supplementary data. NSCLC = non-small cell lung cancer; Prx 4 = peroxiredoxin 4.
The expression of Prx 4 was semiquantitatively evaluated using the method of Conklin et al. [23]. All individual tissue microarray cores were scored according to the cytoplasmic pattern intensity from 0 to 3 as follows: 0, no reactivity; 1+, faint/weak; 2+, moderate; 3+, strong reactivity in tumor cells. The expression levels of Prx 4 were categorized into two groups: cases with score 0 or 1 were considered negative and cases with score 2 or 3 were considered positive.
Statistical analysis
Statistical analyses were performed using SPSS software (version 18.0). The association between the Prx 4 immunoreactivity index and other clinicopathologic factors was analyzed by using the Pearson’s chi-square test or Fisher’s exact test. The Kaplan-Meier method and log-rank test were applied to estimate survival rates and compare the survival curves between groups. The Cox proportional hazard regression model was used for the analyses of the relationship between disease-free survival (DFS) and Prx 4 expression or other clinicopathologic variables. All results were considered statistically significant at P-value < 0.05.
Results
The clinicopathologic characteristics of the patients with stage II NSCLC who had undergone complete surgical resection are summarized in Table 1. Of the 142 patients, 108 (76%) were male. 40 (28%) of the patients had never smoked, whereas 102 (72%) were current or past smokers. The median patient age was 63 (range, 32-85). All patients had undergone curative surgery by lobectomy (79.6%), bilobectomy (10.6%), or pneumonectomy (9.8%). In the pathologic review after surgery, all patients had pathologic N1 node-positive disease. 73 patients (51%) were in the T1 stage and 69 (49%) were in T2. Ninety patients (63%) had received adjuvant therapy. The median follow-up period was 42.9 months (range, 3.4-88.4 months). During the follow-up period after surgery, 59 patients (41.5%) experienced recurrence and 48 (33.8%) expired. In the IHC staining of the resected tumor, 80 tissue samples (56.4%) showed negative Prx 4 expression and 62 (43.6%) showed positive Prx 4 immunoreactivity.
Table 1.
Clinicopathologic characteristics of the patients with stage II NSCLC who underwent complete resection
| Variablesa | No. of subjects (n = 142) |
|---|---|
| Sex | |
| Male | 108 (76.1%) |
| Female | 34 (23.9%) |
| Smoking | |
| Nonsmoker | 40 (28.2%) |
| Ex-smoker | 73 (51.4%) |
| Current smoker | 29 (20.4%) |
| Age (median, years) | 63 (range, 32-85) |
| Tumor size (median, cm) | 3.0 (range, 1.0-7.0) |
| T stageb | |
| T1 | 73 (51.4%) |
| T2 | 69 (48.6%) |
| Type of surgical resection | |
| Lobectomy | 113 (79.6%) |
| Bilobectomy | 15 (10.6%) |
| Pneumonectomy | 14 (9.8%) |
| Adjuvant therapy | |
| Not done | 52 (36.6%) |
| Done | 90 (63.4%) |
| Median follow-up period (median, months) | 42.9 (range, 3.4-88.4) |
| Recurrence cases (recurrence rate) | 59 (41.5%) |
| Death cases (death rate) | 48 (33.8%) |
| Immunohistochemistry of Prx 4c | |
| Negative | 80 (56.4%) |
| Positive | 62 (43.6%) |
NSCLC = non-small cell lung cancer; Prx 4 = peroxiredoxin 4.
Continuous data are shown as the median value and the range from the minimum to the maximum value in parentheses, whereas dichotomous or discontinuous data are shown as number (%).
No patient was in the T3 stage and all patients had pathologic N1 node-positive disease.
The expression of Prx 4 was categorized into two groups using the method of Conklin et al. [23].
Initially, all individual tissue microarray cores were scored by the intensity of the cytoplasmic pattern from 0 to 3 as follows: 0, no reactivity; 1+, faint/weak; 2+, moderate; 3+, strong reactivity in tumor cells. Cases with score 0 or 1 were considered negative and cases with score 2 or 3 were considered positive.
The association between Prx 4 expression and various clinicopathologic factors that might be predictive of prognosis was evaluated in all 142 patients. It turned out that only histology was significantly associated with the degree of Prx 4 expression. Concretely, the proportion of patients with positive Prx 4 immunoreactivity was significantly higher in the adenocarcinoma subtype (39 out of 70, 56%) than in the squamous cell carcinoma subtype (23 out of 72, 32%) (P = 0.004). However, Prx 4 expression was not correlated with sex (P = 0.393), smoking status (P = 0.194), pathologic differentiation (P = 0.392), or pathologic stage (P = 0.290) (Table 2).
Table 2.
Correlation of Prx 4 expression with clinicopathologic variables in patients with resectable stage II NSCLC
| Variablesa | Total number | Prx 4 expression | P-valueb | |
|---|---|---|---|---|
|
| ||||
| Negative | Positive | |||
| Sex | ||||
| Male | 108 (76) | 63 (58) | 45 (42) | 0.393 |
| Female | 34 (24) | 17 (50) | 17 (50) | |
| Smoking | ||||
| Nonsmoker | 40 (28) | 18 (45) | 22 (55) | 0.194 |
| Ex-smoker | 73 (52) | 43 (59) | 30 (41) | |
| Current smoker | 29 (20) | 19 (66) | 10 (34) | |
| Histology | ||||
| Adenocarcinoma | 70 (49) | 31 (44) | 39 (56) | 0.004 |
| Squamous cell carcinoma | 72 (51) | 49 (68) | 23 (32) | |
| Differentiation | ||||
| Well | 14 (10) | 7 (50) | 7 (50) | 0.392 |
| Moderate | 108 (76) | 59 (55) | 49 (45) | |
| Poor | 20 (14) | 14 (70) | 6 (30) | |
| T stage | ||||
| 1 | 73 (51) | 38 (52) | 35 (48) | 0.290 |
| 2 | 69 (49) | 42 (61) | 27 (39) | |
NSCLC = non-small cell lung cancer; Prx 4 = peroxiredoxin 4.
The percentages for the variables are shown within parentheses.
The significance was tested with chi-square or Fisher’s exact tests (P).
In terms of clinical outcome, Prx 4 expression level was meaningfully related to recurrence in the overall NSCLC population (P = 0.013) and in patients with squamous cell carcinoma (P = 0.003), but not in patients with adenocarcinoma (P = 0.934) (Table 3). In accordance with these results, Kaplan-Meier curves and log-rank tests showed that positive Prx 4 expression was significantly correlated with shorter DFS in all NSCLC patients (P = 0.018) and in patients with the squamous cell carcinoma subtype (P = 0.002). However, in the adenocarcinoma sutype group, there was no meaningful diffeence between positive and negative Prx 4 expression state with regard to DFS (P = 0.528 by log-rank test) (Figure 2). Meanwhile, as to overall survival, no statistically significant difference was found according to Prx 4 expression level in the overall NSCLC group or in each subtype group.
Table 3.
Correlation of Prx 4 expression with recurrence or deatha in patients with resectable stage II NSCLC
| Total number | Prx 4 expression | P-valueb | ||
|---|---|---|---|---|
|
|
||||
| Negative | Positive | |||
| Recurrence | ||||
| No | 83 (59) | 54 (65) | 29 (35) | 0.013 |
| Yes | 59 (41) | 26 (44) | 33 (56) | |
| Recurrence in patients with adenocarcinoma | ||||
| No | 32 (46) | 14 (44) | 18 (56) | 0.934 |
| Yes | 38 (54) | 17 (45) | 21 (55) | |
| Recurrence in patients with squamous cell carcinoma | ||||
| No | 51 (71) | 40 (78) | 11 (22) | 0.003 |
| Yes | 21 (29) | 9 (43) | 12 (57) | |
| Death | ||||
| No | 94 (66) | 52 (55) | 42 (45) | 0.732 |
| Yes | 48 (34) | 28 (58) | 20 (42) | |
NSCLC = non-small cell lung cancer; Prx 4 = peroxiredoxin 4.
The percentage for each frequency is shown within parenthesis.
The significance was tested with chi-square or Fisher’s exact tests (P).
Figure 2.
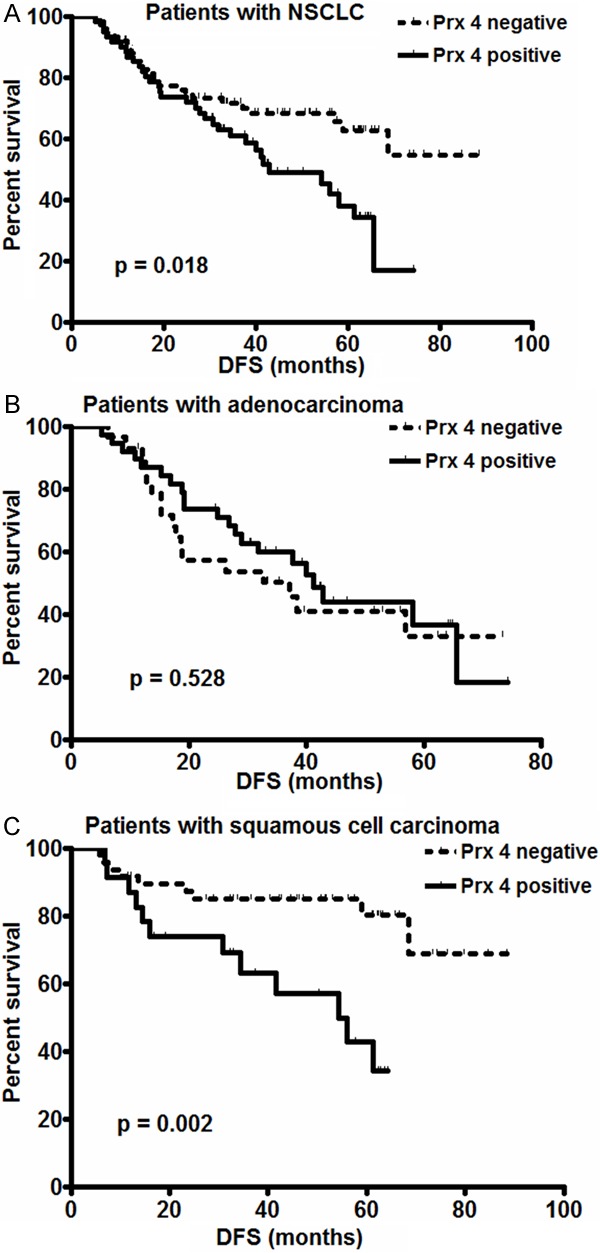
Kaplan-Meier plots of DFS according to the different levels of Prx 4 expression in the overall group of NSCLC patients (A), in patients with the adenocarcinoma subtype (B), or in patients with the squamous cell carcinoma subtype (C). The DFS of patients with positive Prx 4 expression (solid line) was significantly shorter than that of patients with negative Prx 4 expression (dotted line) in both the overall NSCLC patient group (A) and the squamous cell carcinoma subgroup (C). However, there was no significant statistical difference in the adenocarcinoma subgroup (B). The P value was obtained using the log-rank test of the difference. (x-axis: months after surgery; y-axis: DFS probability). DFS = disease-free survival; NSCLC = non-small cell lung cancer; Prx 4 = peroxiredoxin 4.
Cox’s proportional hazard regression analysis was then applied between DFS and Prx 4 expression or clinicopathologic variables in patients with NSCLC (Table 4). Multivariate analysis revealed that only Prx 4 expression state was significantly related to DFS (P = 0.02, hazard ratio = 1.899). Subgroup analyses were next performed with regard to each histological subtype, using an additional Cox proportional hazard model. In the adenocarcinoma subgroup, no other variables, including Prx 4 level, were related to DFS. In contrast, in the squamous cell carcinoma subgroup, positive Prx 4 expression was significantly correlated with shorter DFS (P = 0.003, hazard ratio = 3.910) (Table 5).
Table 4.
Cox proportional hazard regression model analysis between DFS and Prx 4 expression or clinicopathologic variables in patients with NSCLC (n = 142)
| Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|
|
|
||||
| HR (95% CI) | P-value | HR (95% CI) | P-value | |
| Age | 0.993 (0.969-1.018) | 0.601 | 0.992 (0.966-1.018) | 0.528 |
| Sex | ||||
| Male | 1 | |||
| Female | 0.961 (0.527-1.753) | 0.898 | ||
| Smoking status | 0.077 | 0.172 | ||
| Nonsmoker | 1 | 1 | ||
| Ex-smoker | 0.567 (0.313-1.027) | 0.061 | 0.661 (0.361-1.211) | 0.180 |
| Current smoker | 1.072 (0.548-2.100) | 0.839 | 1.205 (0.597-2.434) | 0.603 |
| Differentiation | 0.902 | |||
| Well | 1 | |||
| Moderate | 0.928 (0.436-1.975) | 0.847 | ||
| Poor | 0.796 (0.288-2.200) | 0.660 | ||
| T stage | ||||
| T1 | 1 | 1 | ||
| T2 | 1.158 (0.694-1.931) | 0.575 | 1.184 (0.687-2.042) | 0.543 |
| Operation type | 0.204 | |||
| Lobectomy | 1 | |||
| Bilobectomy | 0.932 (0.420-2.064) | 0.861 | ||
| Pneumonectomy | 0.343 (0.106-1.112) | 0.075 | ||
| Adjuvant treatment | ||||
| No | 1 | |||
| Yes | 1.066 (0.625-1.817) | 0.816 | ||
| Prx 4 expression | ||||
| Negative | 1 | 1 | ||
| Positive | 1.859 (1.106-3.127) | 0.019 | 1.899 (1.104-3.266) | 0.02 |
HR = hazard ratio; CI = confidence interval; DFS = disease-free survival; NSCLC = non-small cell lung cancer; Prx 4 = peroxiredoxin 4.
Table 5.
Cox proportional hazard regression model analysis between DFS and Prx 4 expression or clinicopathologic variables in patients with the lung squamous cell carcinoma subtype (n = 72)
| Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|
|
|
||||
| HR (95% CI) | P-value | HR (95% CI) | P-value | |
| Age | 1.020 (0.965-1.077) | 0.486 | 1.028 (0.967-1.092) | 0.379 |
| Sexa | 0.312 | |||
| Smoking status | 0.335 | 0.360 | ||
| Nonsmoker | 1 | 1 | ||
| Ex-smoker | 1.184 (0.153-9.172) | 0.871 | 1.453 (0.187-11.269) | 0.720 |
| Current smoker | 2.266 (0.281-18.281) | 0.442 | 2.930 (0.340-25.212) | 0.328 |
| Differentiation | ||||
| Well/Moderateb | 1 | |||
| Poor | 0.449 (0.06-3.353) | 0.435 | ||
| T stage | ||||
| T1 | 1 | 1 | ||
| T2 | 2.049 (0.794-5.286) | 0.138 | 1.756 (0.624-4.944) | 0.286 |
| Operation type | 0.664 | |||
| Lobectomy | 1 | |||
| Bilobectomy | 1.180 (0.419-3.324) | 0.754 | ||
| Pneumonectomy | 0.611 (0.170-2.197) | 0.451 | ||
| Adjuvant treatment | ||||
| No | 1 | |||
| Yes | 0.759 (0.320-1.798) | 0.530 | ||
| Prx 4 expression | ||||
| Negative | 1 | |||
| Positive | 3.658 (1.490-8.978) | 0.005 | 3.910 (1.587-9.632) | 0.003 |
HR= hazard ratio; CI = confidence interval; DFS = disease-free survival; Prx 4 = peroxiredoxin 4.
The significance (P-value) in the correlation between sex and recurrence in the squamous cell carcinoma subgroup was tested with a Fisher’s exact test.
The “well” and “moderate” differentiation groups were combined for the analysis because only one case belonged to the “well” differentiation group.
Discussion
Previous reports about Prx 4 have focused on its general role as an antioxidant or the change in its expression under various pathological conditions such as sepsis, diabetes, cardiovascular disease, or cancer [24-28]. Regarding lung cancer, it is known that the level of Prx 4 is significantly elevated in human cancer tissues compared to nonmalignant tissues [29]. Recently, Wei et al. [18] showed in their experiment that Prx 4 exists mainly in the form of the Srx-Prx 4 complex in human lung cancer cells, especially in squamous cell carcinoma and adenocarcinoma, and that Srx staining intensity correlates positively with tumor progression state. They also disclosed that loss of Srx or enhancement of the Srx-Prx 4 axis in A549 cells derived from a patient with lung adenocarcinoma causes a reduction or acceleration, respectively, of tumor growth and lung metastasis formation in mouse xenografts in vivo. However, there has been no human data reported to date about how compatible these results are with the real clinical situation or about the correlation between the level of Prx 4 expression and prognosis in patients with NSCLC.
In our present study, in IHC staining of stage II NSCLC tissues, Prx 4 expression state was found to be associated with histology and recurrence rate. That is, the proportion of patients with positive Prx 4 expression was higher for the adenocarcinoma subtype than for the squamous cell carcinoma subtype (P = 0.004). And this result is in line with that of a previous study by Lehtonen et al. [29]. However, when subgroup analyses according to histopathology were performed in terms of recurrence, there was no significant association between Prx 4 expression and DFS in the adenocarcinoma subgroup, whereas, in the squamous cell carcinoma subgroup, a significant correlation was found between Prx 4 expression and DFS: the Prx 4-positive group had significantly higher recurrence rates (P = 0.003) and shorter DFS (P = 0.003) than the Prx 4-negative group. To sum up, Prx 4 expression is a good prognostic marker of cancer progression in lung squamous cell carcinoma, albeit not associated with the prognosis in adenocarcinoma. With regard to this finding, it is possible to infer that different additive molecular mechanisms will exist according to different NSCLC subtypes, other than previously known mechanisms and functions of Prx 4 in tumor progression.
Meanwhile, unlike adenocarcinoma in NSCLC, where many target agents have recently been developed and are actively used clinically, few molecular targets have been identified, and very restricted targeted agents are being currently applied, for squamous cell carcinoma. Thus, our current study results showing the close correlation between Prx 4 expression and DFS in squamous cell carcinoma sheds light on the potential of Prx 4 as a molecular target in lung squamous cell carcinoma.
To date, there have been no reports on the differences in the Prx 4 expression state and its prognostic value by lung cancer subtype. Thus, it remains to be disclosed why Prx 4 has an influence on recurrence or disease progression only for squamous cell lung carcinoma. However, in a recent study of head-and-neck squamous cell carcinoma (HNSCC), Park et al. [30] revealed that Prx 4 protects cells from radiation-induced apoptosis by decreasing the production of intracellular ROS, thereby enhancing the radioresistance in HNSCC cell lines. In their experiments, the knock down of Prx 4 expression increased apoptosis and enhanced sensitivity to ionizing radiation treatment. It was also noteworthy that the same changes were observed in Prx 4 knockdown cells in the absence of ionizing radiation treatment, suggesting that Prx 4 itself may regulate cell survival irrespective of irradiation. And this may somewhat explain our result - the uneven prognostic role of Prx 4 according to different tumor subtypes - in the aspect of post-surgical treatment resistance and the role of Prx 4 in itself upon cell survival. However, whether these results about HNSCC also apply to lung squamous cell carcinoma and the exact mechanism involved should be revealed through further research.
Conclusions
Altogether, this study showed positive Prx 4 expression state is significantly associated with recurrence and shorter DFS in lung squamous cell carcinoma. This implies that Prx 4 can be a good prognostic marker of cancer progression in early-stage squamous cell carcinoma, although it is not related to the prognosis of adenocarcinoma in NSCLC. Our findings also suggest that Prx 4 may be a potential therapeutic target in patients with squamous cell lung carcinoma.
Acknowledgements
This study was supported by a grant of the Korean Health Technology R&D Project, Ministry of Health & Welfare (HI12C1146000013).
Disclosure of conflict of interest
None.
Supporting Information
References
- 1.American Cancer Society, Surveillance Research, 2013. Available at: http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-037114.pdf. Accessed May 20, 2014.
- 2.Schiller JH, Harrinton D, Belani CP, Langer C, Sandler A, Krook J, Zhu J, Johnson DH. Comparison of four chemotherapy regimens for advanced non small-cell lung cancer. N Engl J Med. 2002;346:92–98. doi: 10.1056/NEJMoa011954. [DOI] [PubMed] [Google Scholar]
- 3.Singhal S, Vachani A, Antin-Ozerkis D, Kaiser LR, Albelda SM. Prognostic implications of cell cycle, apoptosis, and angiogenesis biomarkers in non-small cell lung cancer: a review. Clin Cancer Res. 2005;11:3974–3986. doi: 10.1158/1078-0432.CCR-04-2661. [DOI] [PubMed] [Google Scholar]
- 4.Mountain CF. Revisions in the International System for staging Lung cancer. Chest. 1997;111:1710–1717. doi: 10.1378/chest.111.6.1710. [DOI] [PubMed] [Google Scholar]
- 5.Herbst RS, Heymach JV, Lippman SM. Lung cancer. N Engl J Med. 2008;359:1367–1380. doi: 10.1056/NEJMra0802714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Trachootham D, Alexandre J, Huang P. Targeting cancer cells by ROS-mediated mechanisms: A radical therapeutic approach? Nat Rev Drug Discov. 2009;8:579–591. doi: 10.1038/nrd2803. [DOI] [PubMed] [Google Scholar]
- 7.De Haan JB, Bladier C, Lotfi-Miri M, Taylor J, Hutchinson P, Crack PJ, Hertzoq P, Kola I. Fibroblasts derived from Gpx1 knockout mice display senescent like features and are susceptible to H2O2-mediated cell death. Free Radic Biol Med. 2004;1:53–64. doi: 10.1016/j.freeradbiomed.2003.10.020. [DOI] [PubMed] [Google Scholar]
- 8.Das KC. Thioredoxin system in premature and newborn biology. Antioxid Redox Signal. 2004;6:177–184. doi: 10.1089/152308604771978480. [DOI] [PubMed] [Google Scholar]
- 9.Fujii J, Ikeda Y. Advances in our understanding of peroxiredoxin, a multifunctional mammalian redox protein. Redox Rep. 2002;7:123–130. doi: 10.1179/135100002125000352. [DOI] [PubMed] [Google Scholar]
- 10.Wood ZA, Schroder E, Robin Harris J, Poole LB. Structure, mechanism and regulation of peroxiredoxins. Trends Biochem Sci. 2003;28:32–40. doi: 10.1016/s0968-0004(02)00003-8. [DOI] [PubMed] [Google Scholar]
- 11.Haridas V, Ni J, Meager A, Su J, Yu GL, Zhai Y, Kyaw H, A KT, Hu J, Van Eldik LJ, Aggarwal BB. TRANK, a novel cytokine that activates NF-kappa B and c-Jun N-terminal kinase. J Immunol. 1998;161:1–6. [PubMed] [Google Scholar]
- 12.Tavender TJ, Bulleid NJ. Peroxiredoxin IV protects cells from oxidative stress by removing H2O2 produced during disulphide formation. J Cell Sci. 2010;123:2672–2679. doi: 10.1242/jcs.067843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jeong W, Bae SH, Toledano MB, Rhee SG. Role of sulfiredoxin as a regulator of peroxiredoxin function and regulation of its expression. Free Radic Biol Med. 2012;53:447–456. doi: 10.1016/j.freeradbiomed.2012.05.020. [DOI] [PubMed] [Google Scholar]
- 14.Biteau B, Labarre J, Toledano MB. ATP-dependent reduction of cysteine-sulphinic acid by S. cerevisiae sulphiredoxin. Nature. 2003;425:980–984. doi: 10.1038/nature02075. [DOI] [PubMed] [Google Scholar]
- 15.Chang TS, Jeong W, Woo HA, Lee SM, Park S, Rhee SG. Characterization of mammalian sulfiredoxin and its reactivation of hyperoxidized peroxiredoxin through reduction of cysteine sulfinic acid in the active site to cysteine. J Biol Chem. 2004;279:50994–51001. doi: 10.1074/jbc.M409482200. [DOI] [PubMed] [Google Scholar]
- 16.Rhee SG, Woo HA. Multiple functions of peroxiredoxins: peroxidases, sensors and regulators of the intracellular messenger Hv(2)ov(2), and protein chaperones. Antioxid Redox Signal. 2011;15:781–794. doi: 10.1089/ars.2010.3393. [DOI] [PubMed] [Google Scholar]
- 17.Zito E, Melo EP, Yang Y, Wahlander A, Neubert TA, Ron D. Oxidative protein folding by an endoplasmic reticulum-localized peroxiredoxin. Mol Cell. 2010;40:787–797. doi: 10.1016/j.molcel.2010.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wei Q, Jiang H, Xiao Z, Baker A, Young MR, Veenstra TD, Colburn NH. Sulfiredoxin-Peroxiredoxin IV axis promotes human lung cancer progression through modulation of specific phosphokinase signaling. Proc Natl Acad Sci U S A. 2011;108:7004–7009. doi: 10.1073/pnas.1013012108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Karihtala P, Soini Y, Vaskivuo L, Bloiqu R, Puistola U. DNA adduct 8-hydroxydeoxyguanosine, a novel putative marker of prognostic significance in ovarian carcinoma. Int J Gynecol Cancer. 2009;19:1047–1051. doi: 10.1111/IGC.0b013e3181ad0f0d. [DOI] [PubMed] [Google Scholar]
- 20.Chang KP, Yu JS, Chien KY, Lee CW, Liang Y, Liao CT, Yen TC, Lee LY, Huang LL, Liu SC, Chang YS, Chi LM. Identification of PRDX4 and P4HA2 as metastasis-associated proteins in oral cavity squamous cell carcinoma by comparative tissue proteomics of microdissected specimens using iTRAQ technology. J Proteome Res. 2011;10:4935–4947. doi: 10.1021/pr200311p. [DOI] [PubMed] [Google Scholar]
- 21.Karihtala P, Mantyniemi A, Kang SW, Kinnula VL, Soini Y. Peroxiredoxins in breast carcinoma. Clin Cancer Res. 2003;9:3418–3424. [PubMed] [Google Scholar]
- 22.Edge S, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A. The AJCC Cancer Staging Manual. 7th edition. Springer; 2010. p. XV.p. 649. [Google Scholar]
- 23.Conklin CM, Craddock KJ, Have C, Laskin J, Couture C, Lonescu DN. Immunohistochemistry is a reliable screening tool for identification of ALK rearrangement in non-small-cell lung carcinoma and is antibody dependent. J Thoracic Oncol. 2013;8:45–51. doi: 10.1097/JTO.0b013e318274a83e. [DOI] [PubMed] [Google Scholar]
- 24.Janin S. Peroxiredoxin 4: a multifunctional biomarker worthy of further exploration. BMC Medicine. 2011;137:1741–1747. doi: 10.1186/1741-7015-9-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brixius K, Schwinger RH, Hoyer F, Napp A, Renner R, Bolck B, Kumin A, Fischer U, Mehlhorn U, Werner S, Bloch W. Isoform-specific downregulation of peroxiredoxin in human failing myocardium. Life sciences. 2007;81:823–831. doi: 10.1016/j.lfs.2007.07.014. [DOI] [PubMed] [Google Scholar]
- 26.Schulte J, Struck J, Kohrle J, Muller B. Circulating levels of peroxiredoxin 4 as a novel biomarker of oxidative stress in patients with sepsis. Shock. 2011;35:460–465. doi: 10.1097/SHK.0b013e3182115f40. [DOI] [PubMed] [Google Scholar]
- 27.Jiang YL, Ning Y, Ma XL, Liu YY, Wang Y, Zhang Z, Shan CX, Xu YD, Yin LM, Yang YQ. Alteration of the proteome profile of the pancreas in diabetic rats induced by streptozotocin. Int J Mol Med. 2011;28:153–160. doi: 10.3892/ijmm.2011.696. [DOI] [PubMed] [Google Scholar]
- 28.Chen G, Gharib TG, Huang CC, Thomas DG, Shedden KA, Taylor JM, Kardia SL, Misek DE, Giordano TJ, Iannettoni MD, Orringer MB, Hanash SM, Beer DG. Proteomic analysis of lung adenocarcinoma: identification of a highly expressed set of proteins in tumors. Clin Cancer Res. 2002;8:2298–2305. [PubMed] [Google Scholar]
- 29.Lehtonen ST, Svensk AM, Soini Y. Peroxiredoxin IV, a novel protein family in lung cancer. Int J Cancer. 2004;111:514–521. doi: 10.1002/ijc.20294. [DOI] [PubMed] [Google Scholar]
- 30.Park JJ, Chang HW, Jeoung EJ, Roh JL, Choi SH, Jeon SY, Ko GH, Kim SY. Peroxiredoxin IV protects cells from radiation-induced apoptosis in head-and-neck squamous cell carcinoma. Int J Radiat Oncol Biol Phys. 2009;73:1196–1202. doi: 10.1016/j.ijrobp.2008.10.070. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


