Abstract
Objectives: Association of MTA2 expression with presence, development, metastasis and prognosis of colorectal cancer (CRC) was investigated. Methods: 90 CRC-related cases with follow-up information were made into tissue microarrays according to the paired principle of cancer tissues and the adjacent tissues. Subsequently, the expression of MAT2 was detected with immunohistochemical analysis and SPSS software was finally utilized to analyze the relationships between experimental data and clinical indicatives. Results: Expression of MTA2 in CRC tissues were notably higher than their adjacent tissues (P < 0.001) and showed significant positive correlation with tumor grade (r2 > 0, P < 0.01). Moreover, survival analysis indicated that MTA2 expression in cancer tissues, serving as an independent correlation factor, was significantly correlated with poor prognosis (P = 0.004). Conclusions: MTA2 is a crucial biomarker that is closely related with prognosis of CRC and also a potential molecular target for evaluating the prognosis and treatment of CRC.
Keywords: MAT2, CRC, tissue microarray, immunohistochemistry, biomarker, prognosis
Introduction
Colorectal cancer (CRC) is one of the most common cancers in the world, and it has high death ratio, which ranks as the fourth deadliest malignancy after lung, stomach, liver cancer. Clinically, more than one million people were diagnosed as CRC every year and the number of deaths grew rapidly from 490,000 in 1990 to 715,000 in 2012 [1]. Meanwhile, approximately 60% colorectal patients were died of tumor distant metastasis. Therefore, we can reduce CRC mortality if we find an effective prognostic biomarker related with the progression and metastasis of CRC.
Distant metastasis is a complex process, which is regulated by multiple pathways and involved several gene products. However, the potential metastasis mechanisms in CRC are still not clearly understood. It is found that CRC cell dissemination was the result of a serious of events including extracellular matrix remodeling, invasion, which were regulated by metastatic mediators [2,3]. In recent years, Li et al. discovered that metastasis associated protein 1 (MTA1) which was acted as a main regulator of tumor transformation played a critical role in the progress of CRC [4]. MTA1 was firstly found in the adenocarcinoma cell lines of rat breast, and then detected in many solid tumor types of human, such as ovarian cancer, endometrial cancer, and breast cancer [5-7]. Meanwhile, the association between poor prognosis and expression of MTA1 had also been discovered [8]. MTA1 belongs to the family member of MTA protein (including three subtypes: MTA1, MTA2, MTA3) and relates with the nucleosome remodeling and histone deacetylation (NuRD) complex, which regulate transcription via histone deacetylation and chromatin remodeling [8]. In addition to DNA binding domains, MTA1 also has two srchomology (SH)-binding domains played roles in signal transduction and one bromo adjacent homology (BAH) involved in the interactions between protein and protein [9,10]. Similarly, MTA2 has high homology with MTA1 in the sequence of amino acid, and it is also an important part of NuRD complex [11,12]. MTA2 was overexpressed in the metastatic cell lines of breast and prostate cancer through the studies of gene expression [12,13]. Overexpression of MTA2 in the level of transcription was also discovered in other solid cancers (e.g. gastrointestinal cancer), and it is also related with tumor metastasis [14]. The study did by Yao et al. found that inhibition of MTA2 expression could lead to growth inhibition of cancer cells [15]. These results showed that MTA2 might play a critical role in the growth of cancer cells and migration. However, the relationship between function of MTA2 and CRC is still unclear.
In the present study, we aimed to assess the correction between biological function of MTA2 and the progression, migration, and prognosis of CRC via immunohistochemical method and Tissue Microarrays.
Materials and methods
Source of samples
The study sample was consisted of 90 patients with colorectal cancer, which was obtained from tissue specimen bank within Shanghai biological technology co., LTD. The patient operation time was during July 2006 to May 2007, the last follow-up time of seven of them was August 2012 (loss to follow-up), and then the rest 83 patients were followed-up until August 2014. All the patients were pathologically diagnosed with colorectal cancer and without any pre-surgery treatment. There were 47 males and 43 females with median age 57 years. Each study specimen was provided with cancer tissue and adjacent-carcinoma tissue which was 1.5 cm distanced from cancer.
Tissue chip production
The tissue chip was produced by Shanghai super biological technology co., LTD. After all provided tissue wax block were conducted routine pathological hematoxylin-eosin(HE) staining, secondary diagnosis was performed by pathology experts, and tagged the typical pathological parts on HE sliced. Using tissue chip production apparatus (Beecher Instruments, Inc) receptors in wax block (blank wax block) to punch holes (1.5 mm) in diameter, then according to the tag position on the HE slice, the corresponding tissue was obtained from donor tissue wax block. Then the target tissue chip was put into the array aperture of receptor wax block. Repeating above steps, finally, a colorectal cancer tissue and matched adjacent tissue containing 180 array block points (HCol-Ade180Sur-04) was completed. Slicer (Leica, Germany) was used in 4-5 um thickness serial section, section was attached to the glass slide which through overhand slice processing, then made into tissue microarray.
Immunohistochemical staining
The two-step EnVision method has been conducted to perform immune histochemical experiments. Three magnification visions randomly observed under optical microscope, the number of positive cells in no less than 3 × 100 cells was record, then calculate the positive rate of positive cells to all cells. The dyeing positive rate was included for the statistical analysis: the positive rate equal or less than 95% was treated as low expression group, otherwise, it was included in high expression group.
Statistical analysis
The expression of MTA2 protein in colorectal cancer and adjacent cancer tissues were compared with paired Wilcoxon test. The association between clinical characteristics of colorectal cancer patients and MTA2 protein expression were using Pearson and Spearman’s correlation test. The prognostic of colorectal cancer and MTA2 protein expression were using Kaplan-Meier survival analysis and log-rank test for univariate analysis; the significant variables resulted from univariate test were included in the Cox multivariate regression analysis. The P-value less than 0.05 was considered statistically significant.
Results
Clinical characteristics of study population
The clinical characteristics of 90 CRC patients were shown in Table 1. Age and gender of study subjects were well matched. Similar proportions of patients with tumor size of ≤ 5.0 cm or > 5.0 cm were observed between two groups. Approximately 94.4% of CRC patients were categorized as grade 2 and grade 3. Among CRC patients, 3, 6, 68 and 11 people were respectively identified as T1, T2, T3 and T4 on the basis of T staging. According to lymph node metastasis in N region, 56 CRC patients were considered as N0 and 25 extra patients were determined as N1, while the remaining 9 patients were regarded as N2. 96.7% of all 90 patients were diagnosed as M0 distant metastasis, while another 2 patients received the diagnosis of M1 distant metastasis. The clinical staging classified the CRC patients into stage 1 (7 people), stage 2 (47 people), stage 3 (32 people) and stage 4 (2 people).
Table 1.
Expression of MTA2 in relation to pathologic and clinical variables
| Variables studied | No. of cases | MAT2 expression | r2 | P | |
|---|---|---|---|---|---|
|
| |||||
| Low | High | ||||
| Sex | 0.209 | 0.048 | |||
| Male | 47 (52.2%) | 42 | 5 | ||
| Female | 43 (47.8%) | 36 | 7 | ||
| Age (year-old) | -0.113 | 0.294 | |||
| ≤ 65 | 34 (37.8%) | 5 | |||
| > 65 | 54 (60.0%) | 6 | |||
| Tumor size | -0.057 | 0.598 | |||
| ≤ 5.0 cm | 46 (51.1%) | 39 | 7 | ||
| > 5.0 cm | 42 (46.7%) | 37 | 5 | ||
| Grade | 0.236 | 0.025 | |||
| 1 | 5 (5.6%) | 5 | 0 | ||
| 2 and 3 | 85 (94.4%) | 73 | 12 | ||
| T Staging | 0.075 | 0.489 | |||
| T1 | 3 (3.3%) | 3 | 0 | ||
| T2 | 6 (6.7%) | 4 | 2 | ||
| T3 | 68 (75.6%) | 61 | 7 | ||
| T4 | 11 (12.2%) | 8 | 3 | ||
| Lymph node metastasis (N region) | 0.090 | 0.400 | |||
| N0 | 56 (62.2%) | 50 | 6 | ||
| N1 | 25 (27.8%) | 20 | 5 | ||
| N2 | 9 (10%) | 8 | 1 | ||
| M distant metastasis | -0.024 | 0.822 | |||
| M0 | 87 (96.7%) | 75 | 12 | ||
| M1 | 2 (2.2%) | 2 | 0 | ||
| Clinical staging | 0.139 | 0.196 | |||
| 1 | 7 (7.8%) | 6 | 1 | ||
| 2 | 47 (52.2%) | 42 | 5 | ||
| 3 | 32 (35.6%) | 26 | 6 | ||
| 4 | 2 (2.2%) | 2 | 0 | ||
r2: correlation coefficient. The positive r2 means positive correlation, while the negative r2 is indicative of negative correlation. The closer the absolute value of r2 is to 1, the greater the relativity.
Expression of MTA2 in relation to prognosis of CRC
The immunohistochemical characteristics of MTA2 expression in the nucleus of colorectal cancer tissues and the adjacent tissues (Figure 1) were investigated with the assistance of paired Wilcoxon test, implying that MTA2 expression in colorectal cancer tissues (1.133 ± 0.342 μg/ml) appeared to be notably higher than that in the adjacent tissues (0.989 ± 0.107 μg/ml).
Figure 1.
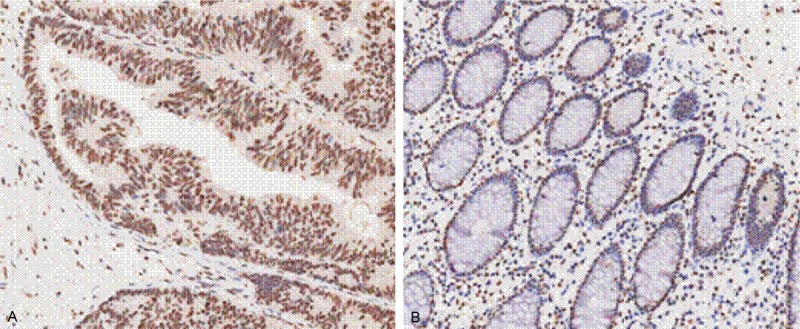
Expression of MTA2 in nucleus of colorectal cancer tissues (A) and tissues adjacent to colorectal cancer (B) studied by immunohistochemistry in tissue microarrays. [Original magnification, × 200].
Additionally, Spearman’s rank correlation analysis was also conducted to display the relationship between expression of MTA2 in colorectal cancer tissues and sex, age, tumor size, tumor grade, T staging, lymph node metastasis in N region, M distant metastasis and clinical staging of study subjects (Table 1). Interestingly, it was found that there existed significantly more MTA2 in patients who suffer from 2nd or 3rd grade of colorectal cancer than those with 1st grade (r2 = 0.236, P = 0.025 < 0.05).
Moreover, in accordance with follow-up visits for 90 colorectal cancer cases, 7 defaulters were statistically analyzed as survivals, who were ultimately called on in August, 2012; the follow-up duration until August, 2014 were available for the remaining 83 cases, among which 49 patients died of colorectal cancer in a median follow-up of 22 months (rang, 3-82 months) and another 34 patients still survived with a median follow-up of 88 months (range, 87-97 months).
With the above statistics, a univariate survival analysis was conducted with both Kaplan-Meier survival analysis and Log-Rank statistical test, indicating that colorectal cancer patients with lower MTA2 expression in cancer tissues enjoyed longer life expectancy (P = 0.004) and significantly higher 5-year survival rate (50.0%) than those with high MTA2 expression (16.7%) (Figure 2).
Figure 2.
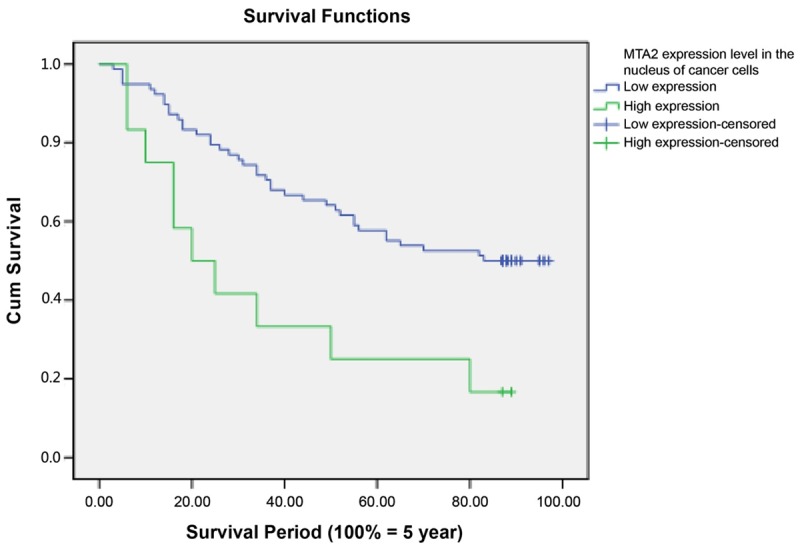
Kaplan-Meier survival analysis for a univariate survival analysis.
Variables with statistical significance in the univariate analysis were included in a Cox multivariate regression analysis, from which conclusions could be drawn that MAT2 expression (P = 0.001), regional lymph node metastasis (P < 0.001), distant metastasis (P = 0.004) and age of patients (P = 0.001) were respectively independent correlation factors of colorectal cancer prognosis (Table 2).
Table 2.
Analysis of independent correlation factors of colorectal cancer prognosis with Cox multivariate regression analysis
| Factor | Regression coefficient | SE | Wald | DF | P-value | Risk | 95% CI | |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| lower | upper | |||||||
| X1 expression | 1.263 | 0.395 | 10.246 | 1 | 0.001 | 3.537 | 1.632 | 7.666 |
| Age | 1.322 | 0.382 | 11.967 | 1 | 0.001 | 3.749 | 1.773 | 7.927 |
| N metastasis | 1.662 | 0.404 | 16.936 | 1 | 0.000 | 5.268 | 2.388 | 11.624 |
| M metastasis | 2.621 | 0.917 | 8.177 | 1 | 0.004 | 13.752 | 2.281 | 82.916 |
| TNM staging | -0.517 | 0.377 | 1.882 | 1 | 0.170 | 0.596 | 0.285 | 1.248 |
X1 expression: X1 expression in nucleus of colorectal cancer cells; SE: standard error; DF: degree of freedom; CI: confidence interval; Lower: lower limit; Upper: upper limit.
Discussion
In this study, we examined the expression level of MTA2 in the cancer and adjacent tissues by immunohistochemical techniques. Our results showed that the level of MTA2 in the cancer tissues was significantly higher than that in the adjacent tissues. Subsequently, the Spearman’s rank-order correlation analysis indicated a positive correlation between MTA2 level and colorectal cancer. Moreover, the univariate survival analysis including the Kaplan-Meier survival analysis and Log-rank statistical test revealed that colorectal cancer patients with lower MTA2 expression in cancer tissues have a significantly higher 5-year survival rate (50.0%) than those with high MTA2 expression in cancer tissues (16.7%). Cox multivariate regression analysis tested all the variables with statistical significance in the univariate survival analysis, and showed that MTA2 expression, regional lymph node metastasis, distant metastasis and age were the independent correlation variables for the colorectal cancer prognosis.
Cancer metastasis is a complex process involving a series of events like detachment from primary tumor, invasion into tissues around the initial sites, penetration into blood vessels and lymphatics, arriving at the distant sites, and the formation of new lesion along with neoangiogenesis [16]. The reorganization of cytoskeleton and interaction with extracellular environment is required for the cancer metastasis [17]. It’s a sign of cancer deterioration that pose a threat to patients’ life due to limited therapies and treatment available. A number of metastasis-related genes have been identified in various cancers, such as WDNM1, WDNM2, KAI-1, MKK4, mst1, nm23, PGM21, stromelysin-3 etc [5,18-24]. Although in most of cases there’s still lack of specific mechanism or direct evidence that may explain the role of these genes and their encoded products in the process of cancer metastasis, it’s observed that these genes were deregulated in the cancer tissues compared with the adjacent tissues. MACC1 is one of identified prognostic indicator for colorectal cancer metastasis. MACC1 is reported to be involved in the HGF-MET signaling through regulating the MET expression [25].
MTA2 is one of metastasis-associated tumor gene family members and shares high homology with another MTA member, MTA1, in the amino acid sequence [26]. The sequential similarity between MTA1 and MTA2 suggest that MTA2 may have the analogous function as MTA1. MTA2 also is an essential component of the nucleosome remodeling and histone deacetylation complex that may be implicated in the adenosine triphosphate dependent chromatin remodeling and histone deacetylase activity [27,28]. The correlation between MTA2 level and malignancies was first revealed in cervical cancer by Zhang Y et al. [29]. The altered expression of MTA2 was observed as well in the hepatocellular cancer, ovarian epithelial cancer, and non small cell lung cancer patients [30-32]. However, no report has reported the association between MTA2 level and colorectal cancer. In this study, we showed a significant correlation between elevated MTA2 level and colorectal cancer. As for its role in the cancer metastasis, Fu et al. reported a decreased invasive and metastatic activity of mouse 4 T1 mammary tumor cells after introducing MTA2 gene interference, which suggest the implication of MTA2 in the tumor metastasis and invasion [33]. The underlying mechanism of MTA2 in the cancer cell metastasis was not fully understood. Previous studies indicated that MTA2 is a part of Twist complex and affect the gene transcription of E-cadherin. Twist plays important role in the induction of mesoderm as well as epithelial to mesenchymal transition [33-35]. The MTA2-containing NuRD complex is needed to bind with Twist to suppress the E-cadherin transcription [33]. Additionally, MTA2 regulates the cytoskeletal and motility pathways through Rho/ROCK signaling. MTA2 decreases the level of Rho GTP dissociation inhibitor alpha (Rho GDIα) and induces the GTP-bound Rho expression. Meanwhile, the restore of Rho GDIα or ROCK inhibitors are able to offset the effect of MTA2-enhanced migration [36-38]. Barone et al. showed the knockdown of Rho GDIα may lead to an elevated level of MTA2 in the ERα-positive breast cancer cells, which contribute to the tamoxifen-resistant phenotypes [39]. Collectively, MTA2 is shown to function as an important regulator in the process of metastasis. It’s of great clinical value to further elucidate the specific mechanism of MTA2 in the metastatic dissemination.
In conclusion, our results showed that high level of MTA2 may be associated with colorectal cancer metastasis; hence it has great potential to serve as a prognostic marker to identify the patients with metastasis. MTA2 may also be a potential target for the colorectal cancer treatments.
Disclosure of conflict of interest
None.
References
- 1.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, Ahn SY, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Barker-Collo S, Bartels DH, Bell ML, Benjamin EJ, Bennett D, Bhalla K, Bikbov B, Bin Abdulhak A, Birbeck G, Blyth F, Bolliger I, Boufous S, Bucello C, Burch M, Burney P, Carapetis J, Chen H, Chou D, Chugh SS, Coffeng LE, Colan SD, Colquhoun S, Colson KE, Condon J, Connor MD, Cooper LT, Corriere M, Cortinovis M, de Vaccaro KC, Couser W, Cowie BC, Criqui MH, Cross M, Dabhadkar KC, Dahodwala N, De Leo D, Degenhardt L, Delossantos A, Denenberg J, Des Jarlais DC, Dharmaratne SD, Dorsey ER, Driscoll T, Duber H, Ebel B, Erwin PJ, Espindola P, Ezzati M, Feigin V, Flaxman AD, Forouzanfar MH, Fowkes FG, Franklin R, Fransen M, Freeman MK, Gabriel SE, Gakidou E, Gaspari F, Gillum RF, Gonzalez-Medina D, Halasa YA, Haring D, Harrison JE, Havmoeller R, Hay RJ, Hoen B, Hotez PJ, Hoy D, Jacobsen KH, James SL, Jasrasaria R, Jayaraman S, Johns N, Karthikeyan G, Kassebaum N, Keren A, Khoo JP, Knowlton LM, Kobusingye O, Koranteng A, Krishnamurthi R, Lipnick M, Lipshultz SE, Ohno SL, Mabweijano J, MacIntyre MF, Mallinger L, March L, Marks GB, Marks R, Matsumori A, Matzopoulos R, Mayosi BM, McAnulty JH, McDermott MM, McGrath J, Mensah GA, Merriman TR, Michaud C, Miller M, Miller TR, Mock C, Mocumbi AO, Mokdad AA, Moran A, Mulholland K, Nair MN, Naldi L, Narayan KM, Nasseri K, Norman P, O’Donnell M, Omer SB, Ortblad K, Osborne R, Ozgediz D, Pahari B, Pandian JD, Rivero AP, Padilla RP, Perez-Ruiz F, Perico N, Phillips D, Pierce K, Pope CA 3rd, Porrini E, Pourmalek F, Raju M, Ranganathan D, Rehm JT, Rein DB, Remuzzi G, Rivara FP, Roberts T, De León FR, Rosenfeld LC, Rushton L, Sacco RL, Salomon JA, Sampson U, Sanman E, Schwebel DC, Segui-Gomez M, Shepard DS, Singh D, Singleton J, Sliwa K, Smith E, Steer A, Taylor JA, Thomas B, Tleyjeh IM, Towbin JA, Truelsen T, Undurraga EA, Venketasubramanian N, Vijayakumar L, Vos T, Wagner GR, Wang M, Wang W, Watt K, Weinstock MA, Weintraub R, Wilkinson JD, Woolf AD, Wulf S, Yeh PH, Yip P, Zabetian A, Zheng ZJ, Lopez AD, Murray CJ, AlMazroa MA, Memish ZA. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lubbe WJ, Zuzga DS, Zhou Z, Fu W, Pelta-Heller J, Muschel RJ, Waldman SA, Pitari GM. Guanylyl cyclase C prevents colon cancer metastasis by regulating tumor epithelial cell matrix metalloproteinase-9. Cancer Res. 2009;69:3529–3536. doi: 10.1158/0008-5472.CAN-09-0067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Giles RH, van Es JH, Clevers H. Caught up in a Wnt storm: Wnt signaling in cancer. Biochim Biophys Acta. 2003;1653:1–24. doi: 10.1016/s0304-419x(03)00005-2. [DOI] [PubMed] [Google Scholar]
- 4.Li DQ, Pakala SB, Nair SS, Eswaran J, Kumar R. Metastasis-associated protein 1/nucleosome remodeling and histone deacetylase complex in cancer. Cancer Res. 2012;72:387–394. doi: 10.1158/0008-5472.CAN-11-2345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sklodowska A. Oxidation of thiosulphate and sulphite by Thiobacillus neapolitanus. Acta Microbiol Pol. 1985;34:271–276. [PubMed] [Google Scholar]
- 6.Kong X, Xu X, Yan Y, Guo F, Li J, Hu Y, Zhou H, Xun Q. Estrogen regulates the tumour suppressor MiRNA-30c and its target gene, MTA-1, in endometrial cancer. PLoS One. 2014;9:e90810. doi: 10.1371/journal.pone.0090810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kang HJ, Lee MH, Kang HL, Kim SH, Ahn JR, Na H, Na TY, Kim YN, Seong JK, Lee MO. Differential regulation of estrogen receptor alpha expression in breast cancer cells by metastasis-associated protein 1. Cancer Res. 2014;74:1484–1494. doi: 10.1158/0008-5472.CAN-13-2020. [DOI] [PubMed] [Google Scholar]
- 8.Toh Y, Nicolson GL. The role of the MTA family and their encoded proteins in human cancers: molecular functions and clinical implications. Clin Exp Metastasis. 2009;26:215–227. doi: 10.1007/s10585-008-9233-8. [DOI] [PubMed] [Google Scholar]
- 9.Toh Y, Pencil SD, Nicolson GL. A novel candidate metastasis-associated gene, mta1, differentially expressed in highly metastatic mammary adenocarcinoma cell lines. cDNA cloning, expression, and protein analyses. J Biol Chem. 1994;269:22958–22963. [PubMed] [Google Scholar]
- 10.Singh RR, Kumar R. MTA family of transcriptional metaregulators in mammary gland morphogenesis and breast cancer. J Mammary Gland Biol Neoplasia. 2007;12:115–125. doi: 10.1007/s10911-007-9043-7. [DOI] [PubMed] [Google Scholar]
- 11.Hofer MD, Menke A, Genze F, Gierschik P, Giehl K. Expression of MTA1 promotes motility and invasiveness of PANC-1 pancreatic carcinoma cells. Br J Cancer. 2004;90:455–462. doi: 10.1038/sj.bjc.6601535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Qian H, Lu N, Xue L, Liang X, Zhang X, Fu M, Xie Y, Zhan Q, Liu Z, Lin C. Reduced MTA1 expression by RNAi inhibits in vitro invasion and migration of esophageal squamous cell carcinoma cell line. Clin Exp Metastasis. 2005;22:653–662. doi: 10.1007/s10585-006-9005-2. [DOI] [PubMed] [Google Scholar]
- 13.Cui Y, Niu A, Pestell R, Kumar R, Curran EM, Liu Y, Fuqua SA. Metastasis-associated protein 2 is a repressor of estrogen receptor alpha whose overexpression leads to estrogen-independent growth of human breast cancer cells. Mol Endocrinol. 2006;20:2020–2035. doi: 10.1210/me.2005-0063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen DW, Fan YF, Li J, Jiang XX. MTA2 expression is a novel prognostic marker for pancreatic ductal adenocarcinoma. Tumour Biol. 2013;34:1553–1557. doi: 10.1007/s13277-013-0685-3. [DOI] [PubMed] [Google Scholar]
- 15.Yao YL, Yang WM. The metastasis-associated proteins 1 and 2 form distinct protein complexes with histone deacetylase activity. J Biol Chem. 2003;278:42560–42568. doi: 10.1074/jbc.M302955200. [DOI] [PubMed] [Google Scholar]
- 16.Toh Y, Oki E, Oda S, Tokunaga E, Ohno S, Maehara Y, Nicolson GL, Sugimachi K. Overexpression of the MTA1 gene in gastrointestinal carcinomas: correlation with invasion and meta- stasis. Int J Cancer. 1997;74:459–463. doi: 10.1002/(sici)1097-0215(19970822)74:4<459::aid-ijc18>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 17.Yilmaz M, Christofori G. EMT, the cytoskeleton, and cancer cell invasion. Cancer Metastasis Rev. 2009;28:15–33. doi: 10.1007/s10555-008-9169-0. [DOI] [PubMed] [Google Scholar]
- 18.Ebralidze A, Tulchinsky E, Grigorian M, Afanasyeva A, Senin V, Revazova E, Lukanidin E. Isolation and characterization of a gene specifically expressed in different metastatic cells and whose deduced gene product has a high degree of homology to a Ca2+-binding protein family. Genes Dev. 1989;3:1086–1093. doi: 10.1101/gad.3.7.1086. [DOI] [PubMed] [Google Scholar]
- 19.Steeg PS, Bevilacqua G, Kopper L, Thorgeirsson UP, Talmadge JE, Liotta LA, Sobel ME. Evidence for a novel gene associated with low tumor metastatic potential. J Natl Cancer Inst. 1988;80:200–204. doi: 10.1093/jnci/80.3.200. [DOI] [PubMed] [Google Scholar]
- 20.Dear TN, McDonald DA, Kefford RF. Transcriptional down-regulation of a rat gene, WDNM2, in metastatic DMBA-8 cells. Cancer Res. 1989;49:5323–5328. [PubMed] [Google Scholar]
- 21.Phillips SM, Bendall A, Ramshaw I. Isolation of gene associated with high metastatic potential in rat mammary adenocarcinomas. J Natl Cancer Inst. 1990;82:199–203. doi: 10.1093/jnci/82.3.199. [DOI] [PubMed] [Google Scholar]
- 22.Basset P, Bellocq J, Wolf C, Stoll I, Hutin P, Limacher JM, Podhajcer OL, Chenard MP, Rio MC, Chambon P. A novel metalloproteinase gene specifically expressed in stromal cells of breast carcinomas. Nature. 1990;348:699–704. doi: 10.1038/348699a0. [DOI] [PubMed] [Google Scholar]
- 23.Dong JT, Lamb PW, Rinker-Schaeffer CW, Vukanovic J, Ichikawa T, Isaacs JT, Barrett JC. KAI1, a metastasis suppressor gene for prostate cancer on human chromosome 11p11.2. Science. 1995;268:884–886. doi: 10.1126/science.7754374. [DOI] [PubMed] [Google Scholar]
- 24.Samant RS, Seraj MJ, Saunders MM, Sakamaki TS, Shevde LA, Harms JF, Leonard TO, Goldberg SF, Budgeon L, Meehan WJ, Winter CR, Christensen ND, Verderame MF, Donahue HJ, Welch DR. Analysis of mechanisms underlying BRMS1 suppression of metastasis. Clin Exp Metastasis. 2000;18:683–693. doi: 10.1023/a:1013124725690. [DOI] [PubMed] [Google Scholar]
- 25.Stein U, Walther W, Arlt F, Schwabe H, Smith J, Fichtner I, Birchmeier W, Schlag PM. MACC1, a newly identified key regulator of HGF-MET signaling, predicts colon cancer metastasis. Nat Med. 2009;15:59–67. doi: 10.1038/nm.1889. [DOI] [PubMed] [Google Scholar]
- 26.Kumar R, Wang RA, Bagheri-Yarmand R. Emerging roles of MTA family members in human cancers. Semin Oncol. 2003;30(Suppl 16):30–37. doi: 10.1053/j.seminoncol.2003.08.005. [DOI] [PubMed] [Google Scholar]
- 27.Xue Y, Wong J, Moreno GT, Young MK, Côté J, Moreno GT, Young MK, Côté J, Wang W. NURD, a novel complex with both ATP-dependent chromatin-remodeling and histone deacetylase activities. Molecular Cell. 1998;2:851–861. doi: 10.1016/s1097-2765(00)80299-3. [DOI] [PubMed] [Google Scholar]
- 28.Zhang Y, LeRoy G, Seelig HP, Lane WS, Reinberg D. The dermatomyositis-specific autoantigen Mi2 is a component of a complex containing histone deacetylase and nucleosome remodeling activities. Cell. 1998;95:279–289. doi: 10.1016/s0092-8674(00)81758-4. [DOI] [PubMed] [Google Scholar]
- 29.Zhang Y, Ng HH, Erdjument-Bromage H, Tempst P, Bird A, Reinberg D. Analysis of the NuRD subunits reveals a histone deacetylase core complex and a connection with DNA methylation. Genes Dev. 1999;13:1924–1935. doi: 10.1101/gad.13.15.1924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yuxin J, Ping Z, Yunping L, Ding M. Expression of MTA2 gene in ovarian epithelial cancer and its clinical implication. J Huazhong Univ Sci Technolog Med Sci. 2006;26:359–362. doi: 10.1007/BF02829576. [DOI] [PubMed] [Google Scholar]
- 31.Lee H, Ryu SH, Hong SS, Seo DD, Min HJ, Yu E, Chung YH, Kim KW. Overexpression of metastasis-associated protein 2 is associated with hepatocellular carcinoma size and differentiation. J Gastroenterol Hepatol. 2009;24:1445–1450. doi: 10.1111/j.1440-1746.2009.05965.x. [DOI] [PubMed] [Google Scholar]
- 32.Liu SL, Han Y, Zhang Y, Xie CY, Wang EH, Miao Y, Li HY, Xu HT, Dai SD. Expression of metastasis-associated protein 2 (MTA2) might predict proliferation in non-small cell lung cancer. Target Oncol. 2012;7:135–143. doi: 10.1007/s11523-012-0215-z. [DOI] [PubMed] [Google Scholar]
- 33.Fu J, Qin L, He T, Qin J, Hong J, Wong J, Liao L, Xu J. The TWIST/Mi2/NuRD protein complex and its essential role in cancer metastasis. Cell Res. 2011;21:275–289. doi: 10.1038/cr.2010.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yang J, Mani SA, Donaher JL, Ramaswamy S, Itzykson RA, Come C, Savagner P, Gitelman I, Richardson A, Weinberg RA. Twist, a master regulator of morphogenesis, plays an essential role in tumor metastasis. Cell. 2004;117:927–939. doi: 10.1016/j.cell.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 35.Casas E, Kim J, Bendesky A, Ohno-Machado L, Wolfe CJ, Yang J. Snail2 is an essential mediator of Twist1-induced epithelial mesenchymal transition and metastasis. Cancer Res. 2011;71:245–254. doi: 10.1158/0008-5472.CAN-10-2330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Covington KR, Brusco L, Barone I, Tsimelzon A, Selever J, Corona-Rodriguez A, Brown P, Kumar R, Hilsenbeck SG, Fuqua SA. Metastasis tumor-associated protein 2 enhances metastatic behavior and is associated with poor outcomes in estrogen receptor-negative breast cancer. Breast Cancer Res Treat. 2013;141:375–384. doi: 10.1007/s10549-013-2709-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kedrin D, van Rheenen J, Hernandez L, Condeelis J, Segall JE. Cell motility and cytoskeletal regulation in invasion and metastasis. J Mammary Gland Biol Neoplasia. 2007;12:143–152. doi: 10.1007/s10911-007-9046-4. [DOI] [PubMed] [Google Scholar]
- 38.Amano M, Nakayama M, Kaibuchi K. Rho-kinase/ROCK: a key regulator of the cytoskeleton and cell polarity. Cytoskeleton. 2010;67:545–554. doi: 10.1002/cm.20472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Barone I, Brusco L, Gu G, Selever J, Beyer A, Covington KR, Tsimelzon A, Wang T, Hilsenbeck SG, Chamness GC, Andò S, Fuqua SA. Loss of Rho GDIα and resistance to tamoxifen via effects on estrogen receptor α. J Natl Cancer Inst. 2011;103:538–52. doi: 10.1093/jnci/djr058. [DOI] [PMC free article] [PubMed] [Google Scholar]


