Abstract
The purpose of this study was to investigate the potential of a high-throughput, easily implemented, cost-effective, video analysis software–based mobility protocol to quantify spine kinematics. This prospective cohort study of clinical biomechanics implemented 2-dimensional (2D) image processing at a tertiary-care academic institution. Ten healthy, able-bodied volunteers were recruited for 2D videography of gait and functional motion. The reliability of a 2D video analysis software program for gait and range of motion metrics was evaluated over 2 independent experimental sessions, assessing for inter-trial, inter-session, and inter-rater reliability. Healthy volunteers were evaluated for simple forward and side bending, rotation, treadmill stride length, and more complex seated-to-standing tasks. Based on established intraclass correlation coefficients, results indicated that reliability was considered good to excellent for simple forward and side bending, rotation, stride length, and more complex sit-to-standing tasks. In conclusion, a cost-effective, 2D, video analysis software–based mobility protocol represents a feasible and clinically useful approach for objective spine kinematics and gait metrics. As the complication rate of operative management in the setting of spinal deformity is weighed against functional performance and quality of life measures, an objective analysis tool in combination with an appropriate protocol will aid in clinical assessments and lead to an increased evidence base for management options and decision algorithms.
Introduction
Postural characterizations and descriptions of kinematics and kinetics use motion and gait analysis systems [1–4], but the equipment and analysis software for 3-dimensional gait analysis can be cumbersome and prohibitively expensive. A more technically simple and inexpensive system is needed for widespread use in the physician's office to inform surgeons, physiatrists, therapists, and patients of the impact of surgery on motion [5]. This study examines the utility of 2-dimensional (2D) video analysis of gait and spinopelvic motion, which would be particularly useful for spinal deformity assessment. In severe cases of spinal deformity, spinal fusion is often required [6], but little is known about the effects of surgical fusion on motion, particularly longitudinally.
Methods
Ten healthy, able-bodied volunteers were recruited for 2D videography of gait and functional motion. The subjects included 6 men and 4 women who ranged in age from 23–30 years (mean, 24.5 years; standard deviation [SD], 2.4) and had an average body mass index of 22.5 kg/m2 (SD, 3.15 kg/m2; range, 15.8–25.7). Subjects were volunteers recruited through our institution, according to the Institutional Review Board–approved protocol.
Medical tape was used to affix high-contrast markers to bony landmarks palpated by a certified exercise physiologist. The landmarks included the left lateral acromion, the left greater trochanter, the left knee in the mid-axial line at the level of the patella, and the left malleolus, bilateral posterior superior iliac spines (PSIS), and bilateral superior angles of the scapula.
Two Canon VIXIA HV40 high-definition digital camcorders (Canon USA, Inc, Melville, NY) were placed at a distance adequate to fit the full body within the frame of view (10–12 ft) with space available for the motions indicated below. Camera 1 was stationed posterior to the midline of the back, and camera 2 was stationed in a lateral position as related to the orientation of the subject.
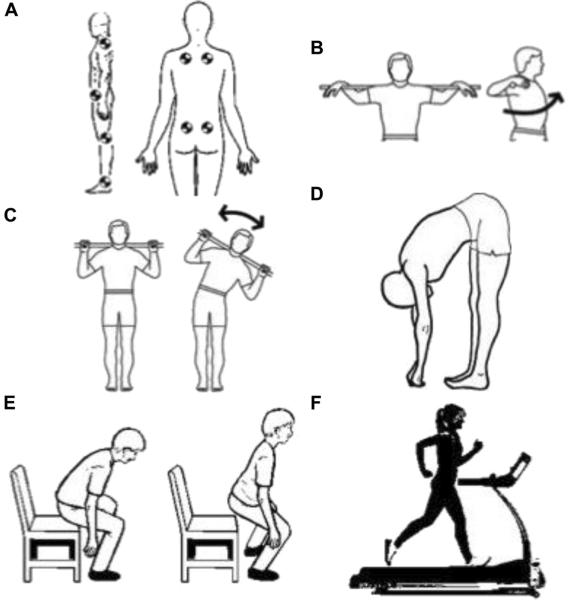
Stationary uniplanar range of motion exercises were performed with a 48-inch dowel, which was used for reference measurements during the analysis. The dowel was placed over the crest of the cervicothoracic junction with the hands spaced according to comfort. Tasks were performed in succession (Figure 1B–F) with 5 full blocks of each for the following trials: (1) alternating maximum right and left rotation; (2) left and right side bend; (3) forward bend; and (4) rise to standing from seated position in a chair. Subjects then walked on a treadmill at a speed of 1.0 m/s. Subjects returned for retest after an interval of between 1 and 4 weeks based on scheduling and space availability.
Figure 1.
(A) Marker arrangement in both anteroposterior and lateral planes. (B) Alternating left and right rotation (5 cycles). (C) Alternating lateral maximum bends to the right and left (5 cycles). (D) Forward bend (5 cycles). (E) Sit to stand (5 cycles). (F) Treadmill gait at 1.0 m/s.
2D Videography Reliability Evaluation and Statistical Analysis
Sagittal plane reliability of the Dartfish software (Dartfish USA, Inc, Alpharetta, GA) during simple forward bending was evaluated with use of the standing hip (shoulder-hip-knee) and knee (hip-knee-ankle) angles from the lateral view. The spinopelvic angle, defined as the angle created by the intersection of the line between the two PSIS markers and the line through the left superior scapula and left PSIS markers, was evaluated during lateral bend in the coronal view. The axis of rotation, estimated by dowel length change visible to the camera during alternating left and right maximum rotation exercises, was also evaluated in the coronal view. During treadmill gait analysis, Dartfish software was used to analyze dynamic stride length and knee angles in the sagittal view.
The Dartfish software generated values for angles and positional coordinates that were used to determine inter-trial, inter-session, and inter-rater reliability. Inter-rater reliability was determined between 2 assessors who used the same software and video files but were blinded to the other's measurements. For each task, motion curves were generated from the positional coordinates starting from the neutral position and ending after 5 complete cycles. The coordinates were recorded at a frequency of 30 Hz and the sinusoidal motion curves were formed using the best-fit lines of the coordinate data.
Analysis was performed across motion curves using intraclass correlation coefficients (ICCs) and coefficient of multiple correlation. In addition, the minimum detectable change was determined for 95% confidence by multiplying the standard error of the mean by SQRT(2) and by the z score—that is, 1.96 for 95% confidence in this study. Reliability was graded accordingly: excellent, ICC >0.90; good, 0.80≤ICC<0.90; fair, 0.70≤ICC<0.80; and poor, ICC <0.70.
Results
The reliability of side bending in the coronal plane was very good with regard to the spine inclination angle (ICC: 0.92–0.97, Table 1). Standing hip and knee angles during simple forward bending were similar (hip ICC: 0.959–0.962; knee ICC: 0.914–0.934, Table 1). Rotation measurements showed lower reliability than those of other exercises and movements (ICC: 0.717–0.846, Table 1).
Table 1.
Reliability of trunk, gait, and sit-to-stand ranges of motion
| Comparison | ROM | Parameter | ICC* (2,1) | CMC† | MDC |
|---|---|---|---|---|---|
| Inter-trial (within session)‡ | Trunk | Shoulder-pelvis angle | 0.97 (0.961–0.978) | 0.971 (0) | 4.6° |
| Front bend hip angle | 0.959 (0.946–0.97) | 0.964 (0.032) | 8.9° | ||
| Front bend knee angle | 0.934 (0.892–0.959) | 0.956 (0.045) | 2° | ||
| Rotation | 0.846 (0.782–0.899) | 0.867 (0.138) | 8.6° | ||
| Gait | Stride length | 0.97 (0.948–0.984) | 0.97 (0.032) | 0.025 m | |
| Knee angle | 0.911 (0.856–0.951) | 0.911 (0.071) | 5.6° | ||
| Sit to stand | Knee angle | 0.926 (0.898–0.947) | 0.942 (0.032) | 8.4° | |
| Hip angle | 0.917 (0.885–0.942) | 0.924 (0.071) | 9.5° | ||
| Inter-session (between sessions)§ | Trunk | Shoulder-pelvis angle | 0.96 (0.945–0.971) | 0.965 (0.032) | 6.8° |
| Front bend hip angle | 0.962 (0.951–0.971) | 0.966 (0) | 9.5° | ||
| Front bend knee angle | 0.914 (0.875–0.94) | 0.932 (0.045) | 4.8° | ||
| Rotation | 0.717 (0.593–0.825) | 0.717 (0.158) | 3.4° | ||
| Gait | Stride length | 0.968 (0.945–0.984) | 0.97 (0.032) | 0.035 m | |
| Knee angle | 0.904 (0.844–0.948) | 0.911 (0.071) | 6.2° | ||
| Sit to stand | Knee angle | 0.904 (0.838–0.942) | 0.934 (0.063) | 9.9° | |
| Hip angle | 0.933 (0.911–0.951) | 0.939 (0.063) | 10.7° | ||
| Inter-rater ICC (2,1)¶ | Trunk | Shoulder-pelvis angle | 0.92 (0.887–0.945) | 0.932 (0.071) | 4.1° |
| Front bend hip angle | 0.962 (0.943–0.974) | 0.971 (0.032) | 6.1° | ||
| Front bend knee angle | 0.922 (0.897–0.941) | 0.938 (0) | 5.1° | ||
| Rotation | 0.771 (0.661–0.854) | 0.847 (0.155) | 6.4° | ||
| Gait | Stride length | 0.894 (0.815–0.945) | 0.916 (0.071) | 0.048 m | |
| Knee angle | 0.975 (0.947–0.988) | 0.984 (0) | 8.4° | ||
| Sit to stand | Knee angle | 0.927 (0.903–0.946) | 0.928 (0.077) | 9.1° | |
| Hip angle | 0.884 (0.85–0.912) | 0.891 (0.084) | 12.6° |
ROM = range of motion; ICC(2,1) = Shrout and Fleiss intraclass correlation type (2,1), representing 2-way random single measure (consistency/absolute agreement); CMC = coefficient of multiple correlation; MDC = minimal detectable change.
ICC: For discrete values for variables (peak measures), between 0.4 and 0.75 was considered good and >0.90 was considered excellent.
CMC: For waveforms across gait or motion curve.
Inter-trial of 5 trials (2 sessions × 10 patients, N = 20).
Inter-session of 2 sessions (average of 5 trials, 10 patients, N = 10).
Inter-rater (between assessors).
Knee angles measured during treadmill gait demonstrated strong inter-trial and inter-session ICC values and very strong inter-rater ICC values (ICC: 0.904–0.927, Table 1). The ICC values for stride length during the same movement were less strong (ICC: 0.894–0.970, Table 1).
During the complex motion of rising from a seated position, the hip and knee angles demonstrated strong ICC values (ICC: 0.884–0.933, Table 1).
Implications
This study is the first to characterize the clinical potential of a high-throughput, easily implemented, cost-effective, video analysis software–based mobility protocol for objective spine kinematics and gait metrics. Motion analysis has not been accepted as a standard clinical tool [7], despite the ability of researchers to generate important objective quantification of spine motion [8–15].
Large-scale comparative analyses will enrich our understanding of the effects of orthopedic surgery on motion. At present, the rate-limiting step is that laboratory methods require expensive equipment and a high degree of technical expertise. The current price for a complete Vicon system is approximately $12,500, whereas a complete Dartfish system is approximately $1800. This proof of concept study helps bring motion analysis from the laboratory to the clinical setting, where it is equally, if not more, meaningful.
The objective kinematic protocol described here, for use with the Dartfish system, can be replicated easily while minimizing cost, technical requirements, interpretation, and analysis. The motion exercises tested in this study met acceptable standards for clinical/research use, because most ICC values were considered good or excellent. The minimum detectable change values are presented to underscore the sensitivity of this method. If a clinician/researcher aims to detect a difference of less than 5 cm before and after an intervention, this tool is unlikely to detect such change. This would help with tracking improvements or decompensation after surgery. This reduction in time and financial costs will allow clinicians and scientists to form a meaningful collaboration, standardizing simple metrics to enable development of large longitudinal studies of kinematics between disciplines from basic science to clinical medicine. Rather, this tool is ideal to track improvements or decompensation after surgery.
Acknowledgments
Disclosures outside this publication: board membership, Nemaris Inc (money to author); consultancy, MSD (money to author); grants/grants pending, DePuy, ISSG, SRS (money to institution); payment for lectures including service on speakers bureaus, MSD, DePuy, K2M (money to author); stock/stock options, Nemaris Inc (money to author)
Disclosures outside this publication: grants/grants pending, Paradigm Spine (research salary support), Fridolin Trust (research salary support), OMEGA (fellowship support), AOSpine NA (fellowship support), OREF (fellowship support) (money to institution); payment for lectures including service on speakers bureaus, K2M (money to author); royalties, K2M (money to author); stock/stock options, Fastenetix (money to author); travel/accommodations/meeting expenses unrelated to activities listed, K2M (money to author)
Footnotes
Disclosure: nothing to disclose
References
- 1.Kramers-de Quervain IA, Muller R, Stacoff A, Grob D, Stussi E. Gait analysis in patients with idiopathic scoliosis. Eur Spine J. 2004;13:449–456. doi: 10.1007/s00586-003-0588-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Engsberg JR, Lenke LG, Uhrich ML, Ross SA, Bridwell KH. Prospective comparison of gait and trunk range of motion in adolescents with idiopathic thoracic scoliosis undergoing anterior or posterior spinal fusion. Spine. 2003;28:1993–2000. doi: 10.1097/01.BRS.0000087209.34602.42. [DOI] [PubMed] [Google Scholar]
- 3.Dalleau G, Damavandi M, Leroyer P, Verkindt C, Rivard CH, Allard P. Horizontal body and trunk center of mass offset and standing balance in scoliotic girls. Eur Spine J. 2011;20:123–128. doi: 10.1007/s00586-010-1554-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Giakas G, Baltzopoulos V, Dangerfield PH, Dorgan JC, Dalmira S. Comparison of gait patterns between healthy and scoliotic patients using time and frequency domain analysis of ground reaction forces. Spine. 1996;21:2235–2242. doi: 10.1097/00007632-199610010-00011. [DOI] [PubMed] [Google Scholar]
- 5.Soda P, Carta A, Formica D, Guglielmelli E. A low-cost video-based tool for clinical gait analysis; Proceedings of the Annual International Conference of the Institute of Electrical and Electronics Engineers Engineering in Medicine and Biology Society; Minneapolis, MN. September 3–6, 2009; pp. 3979–3982. 2009. [DOI] [PubMed] [Google Scholar]
- 6.Rinsky LA, Gamble JG. Adolescent idiopathic scoliosis. West J Med. 1988;148:182–191. [PMC free article] [PubMed] [Google Scholar]
- 7.Wren TA, Gorton GE, 3rd, Ounpuu S, Tucker CA. Efficacy of clinical gait analysis: A systematic review. Gait Posture; 2011. pp. 149–153. [DOI] [PubMed] [Google Scholar]
- 8.Wang R, Leow WK, Leong HW. 3D-2D spatiotemporal registration for sports motion analysis. Proceedings of the Institute of Electrical and Electronics Engineers Conference on Computer Vision and Pattern Recognition; Anchorage, AK. June 23–28, 2008; pp. 1–8. 2008. [Google Scholar]
- 9.Messenger N, Bowker P. The role of gait analysis in clinical medicine: A survey of UK centres. Eng Med. 1987;16:221–227. doi: 10.1243/emed_jour_1987_016_050_02. [DOI] [PubMed] [Google Scholar]
- 10.Baker R. Gait analysis methods in rehabilitation. J Neuroeng Rehabil. 2006;3:4. doi: 10.1186/1743-0003-3-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kadaba MP, Ramakrishnan HK, Wootten ME. Measurement of lower extremity kinematics during level walking. J Orthop Res. 1990;8:383–392. doi: 10.1002/jor.1100080310. [DOI] [PubMed] [Google Scholar]
- 12.Engsberg JR, Lenke LG, Reitenbach AK, Hollander KW, Bridwell KH, Blanke K. Prospective evaluation of trunk range of motion in adolescents with idiopathic scoliosis undergoing spinal fusion surgery. Spine. 2002;27:1346–1354. doi: 10.1097/00007632-200206150-00018. [DOI] [PubMed] [Google Scholar]
- 13.Engsberg JR, Bridwell KH, Wagner JM, Uhrich ML, Blanke K, Lenke LG. Gait changes as the result of deformity reconstruction surgery in a group of adults with lumbar scoliosis. Spine. 2003;28:1836–1843. doi: 10.1097/00007632-200308150-00012. discussion 1844. [DOI] [PubMed] [Google Scholar]
- 14.Mahaudens P, Mousny M. Gait in adolescent idiopathic scoliosis. Kinematics, electromyographic and energy cost analysis. Stud Health Technol Inform. 2010;158:101–106. [PubMed] [Google Scholar]
- 15.Wilk B, Karol LA, Johnston CE, 2nd, Colby S, Haideri N. The effect of scoliosis fusion on spinal motion: A comparison of fused and nonfused patients with idiopathic scoliosis. Spine. 2006;31:309–314. doi: 10.1097/01.brs.0000197168.11815.ec. [DOI] [PubMed] [Google Scholar]