Introduction
Pediatric mental health disease is on the rise in the United States (US). It has been estimated that 6 to 9 million children have serious emotional disturbances1. Studies show that over half a million children a year present to an emergency department (ED) with a mental health problem and of the children successfully committing suicide, over half of them had been seen by a physician in the 1 to 6 month prior to their death2-3. Policy statements and technical reports have been issued by organizations endorsing the need for ED's to serve as a safety net for this large population. In addition, they call for increased research and data collection to further define, and hopefully improve upon the problems related to mental health at a clinical and systems-wide level4-5.
Prior studies have described that mental health visits in the pediatric emergency department (PED) were increasing over time. One study extrapolated data on visits and treatments in emergency departments across the nation from the National Hospital Ambulatory Medical Care Survey (NHAMCS) from 1993-19996. This public-use database collects representative data on visits and treatments in emergency departments across the nation7. Their study showed that 1.6% of all ED visit in children were for mental health reasons. Of these patients, ∼20% were admitted to hospital – more than double the rate of patients without a mental health diagnosis. Subsequent studies have shown continued increase in visits between the late 1990s to 20018-9. In these studies, mental health visits accounted for approximately 5% of all ED visits in children, and over half of these patients received medications ranging from benzodiazepines to antipsychotic agents10-11.
Many pediatric patients with mental health disease will either present or be transferred to a PED, potentially from a general ED or clinic, for further evaluation or admission. Pediatric specific ED studies12-17, including a large study done by the Pediatric Emergency Care Applied Research Network (PECARN) in 200517, have shown that higher percentages of children with a mental health diagnosis arrive by ambulance, have longer length of stays (LOS), require more admissions and approximately 25% of them have multiple visits to the ED for similar complaints. Beyond issues related to crowding and individual ED resource utilization, this also raises concern over costs to the healthcare system. In addition, recent studies18,19 have focused on the importance of outpatient mental health providers and ways children can receive specific therapeutic interventions in the ED.
Though previous studies have demonstrated increased trends in PED use for mental health complaints it is unknown whether these trends have continued over the past decade. Given the high admission rate in this patient population, access to inpatient psychiatric beds may be a critical determinant of resource utilization for PEDs when caring for these patients, though this has yet to be studied. The objective of this study was to evaluate trends in ED care for children with mental health complaints at a single pediatric tertiary care hospital that does not have an associated inpatient psychiatric facility and must transfer all patients who need psychiatric admission to other centers in the greater metropolitan area. We hypothesize that annual ED presentations and LOS increase have increased over time.
Materials and Methods
This was a retrospective observational study. Data were abstracted from the electronic medical record (EMR) system (EPIC™ 2010) from January 2009-July 2013. This study was approved by the Institutional Review Board at Oregon Health & Science University (OHSU).
The study population was identified as all patients who presented to the PED at OHSU less than 19 years of age with a discharge diagnosis of a mental health condition. A mental health condition was defined by presence of an international classification of disease (ICD-9) code of 291, 292, 295-309 (except 305.1 & 305.8) and 311-314 on the discharge diagnosis list. Data were electronically abstracted by the Oregon Clinical and Translational Research Institute (OCTRI) from the EMR for the population of interest, including patient demographics, pre-hospital information such as means of arrival, home medications and past ED visits, PED visit data including treatments, diagnostic tests, restraint use and length of stay, and disposition data. Home medications were determined if they were present on the patients electronic reconciled medication list on PED arrival. Medications administered in the PED were electronically abstracted from the patient medication administration list for each encounter. Any medications that were ordered, but not marked as given were not considered as being received. We defined restraint use as being an order for physical restraints or a chemical restraint administered including lorazepam, midazolam, haloperidol, olanzapine or ziprasidone. Patient charges were obtained from the financial offices for each PED encounter. PED level daily operational variables (census, percent of patients admitted to hospital, percent of patients left without being seen and total boarding hours) were obtained based on aggregated data from our electronic health record (Epic; Verona, WI).
In addition to the electronic collection of data as described above, all study subject charts were reviewed manually. This was done to collect data on whether or not the patient expressed suicidal ideation or had attempted suicide prior to the visit. ED physician provider notes were reviewed by trained research assistants to determine if a patient had active suicidal ideations on presentation and if they had attempted to physically harm themselves prior to their PED visit.
Statistical Analysis
Patient demographic and clinical characteristics were summarized using descriptive statistics. Multiple regression models were used to assess the trend over time in PED utilization. For mental health related PED presentations, we analyzed the annual aggregated number of ED visits using a Poisson regression with logarithm of annual census as the offset variable. For LOS and charges, patient level data were analyzed and we used a linear mixed effects model to assess time trend for LOS since normal assumption was adequately satisfied, and a lognormal mixed effects model for charges to address the right-skewed distribution of charges. Both models adjusted for potential patient and ED level confounding variables as well as the clustering of multiple ED visits within each patient. All analyses were conducted using SAS 9.3 (SAS Institute Inc., Cary, NC, USA.).
Results
During the study period there were 732 PED encounters that met the inclusion criteria representing 646 unique patients. Of those encounters, 12% were patients with repeat visits for a mental health issue (Table 1). The average age was 13.8 years and 53% were male. The most common means of arrival was by private car (55.7%) followed by ambulance (36.8%), police escort (4.8%), unknown (1.3%), walk-in (0.8%), bus (0.5%) and fixed wing airplane (0.1%). The overall annual census in 2013 for our PED was approximately 14,000 patients.
Table 1. Patient Demographics.
| Encounters | Total- 732 |
| repeat visits- 86 | |
|
| |
| Gender | Male- 53% |
| Female- 47% | |
|
| |
| Means of Arrival | Private Car- 55.7% |
| Ambulance- 36.8% | |
| Police Escort- 4.8% | |
| Unknown- 1.3% | |
| Walk in- 0.8% | |
| Public Bus- 0.5% | |
| Airplane- 0.1% | |
|
| |
| Disposition | Discharge- 77.6% |
| Admit- 13.7% | |
| Transfer- 7.1% | |
| Unknown- 1.4% | |
| AMA- 0.3% | |
AMA= against medical advice;
Mental Health Presentation/Disposition
During the study period, the overall PED volume and mental health volume increased. The proportion of pediatric mental health diagnoses to overall PED visits increased from 1.1% to 1.7% during the study time period (Table 2). This increase was a statistically significant increase (p=0.004) during the 5 year study with an annual increase of 10% (rate ratio 1.10; 95% CI, 1.05 to 1.17). Of the 732 encounters, 192 (26%) were suicidal on presentation. Eighty four (44%) of the patients who were suicidal on presentation had attempted to commit suicide with mechanisms ranging from ingestion, cutting, hanging or jumping from high elevations.
Table 2. Trends Over Study Period.
| 2009 | 2010 | 2011 | 2012 | 2013 | p-value | |
|---|---|---|---|---|---|---|
| PresentProp | 1.13% | 1.33% | 1.24% | 1.56% | 1.69% | *p=0.004 |
| Mean LOS in hours (SD) | 6.7 (7.7) | 8.3 (16.2) | 8.0 (15.1) | 11.2 (20.1) | 20.8 (32.3) | *p=0.0367 |
| Median Charges in dollars (IQR) | 1128 (736-1688) | 1137 (683 – 1688) | 1186 (900 – 1688) | 1292 (779 – 1817) | 1335 (821 – 1834) | *p=0.011 |
PresentProp: proportion of mental health presentations out of overall PED volume; LOS: length of stay; IQR: inter-quartile range
P-values were obtained from the multiple regression models after adjusting for patient and ED level confounding variables. For proportion of mental health presentations, a Poisson regression was used. For LOS, a linear mixed effects model was used; and for charges, a lognormal mixed effects model was used.
The majority of patients (77.6%) were able to be discharged from the PED. Approximately 21% needed admission or transfer for further cares. This was not for medical clearance in the vast majority of cases, but transfer for acute psychiatric admission. Two patients left against medical advice and 10 encounters were missing their disposition data in this study population.
Mood disorders were the most common diagnoses (23.9% of encounters) with depression encompassing over 78% of these disorders (Table 3). Substance related disorders were second most frequent (19% of encounters) with alcohol abuse being present in 72% of these encounters. Other frequent disorders included anxiety disorders (15%), personality disorders (14%) and schizophrenia/psychotic disorders (5%). Home medications present on patient medication reconciliation on presentation were identified by pharmacy subclass of each medication. The frequency of medications that patients reported taking prior to arrival included antidepressants (27%), antipsychotics (19%), anti-anxiety (17%), anti-convulsants (12%) and medications used to treat attention deficit/hyperactivity disorder (12%).
Table 3. Final PED Diagnosis.
| Final Diagnosis (n) | Subgroup (n) |
|---|---|
|
| |
| Mood Disorders (175) | Depressive Disorder (137) |
| Bipolar Disorder (18) | |
| Dysthymic Disorder (12) | |
| Mood Disorder NOS (8) | |
|
| |
| Substance Related Disorders (140) | Alcohol Abuse (101) |
| Unspecified (21) | |
| Cannabis (9) | |
| Amphetamine (3) | |
| Opioids (5) | |
| Cocaine (1) | |
|
| |
| Anxiety Disorders (110) | General Anxiety Disorder (75) |
| Panic Disorder (29) | |
| OCD (4) | |
| PTSD (2) | |
|
| |
| Personality Disorder (102) | Conduct Disorder (61) |
| Explosive Personality Disorder (30) | |
| Oppositional Defiant Disorder (4) | |
| Paranoid State (4) | |
| Borderline (3) | |
|
| |
| Other Disorders (60) | Other syndrome NOS (19) |
| Other emotional disturbance (17) | |
| Other nonpsychotic mental health disorder (12) | |
| Sleep disturbance (7) | |
| GI malfunction from mental disorder (3) | |
| Tension headache (2) | |
| Elimination disorder (2) | |
| Respiratory malfunction from mental factors (1) | |
|
| |
| Schizophrenia/Psychotic Disorders (35) | Unspecified Psychosis (31) |
| Schizophrenia (2) | |
| Delusional Disorder (2) | |
|
| |
| Somatoform Disorder (29) | Conversion Disorder (26) |
| Psychogenic Pain (2) | |
| Hypochondriasis (1) | |
|
| |
| Other Developmental Disorders (26) | Autistic/Pervasive Development Disorder (13) |
| ADHD (13) | |
|
| |
| Tic Disorders (25) | Tic Disorder NOS (23) |
| Tourette's Disorder (2) | |
|
| |
| Eating Disorders (17) | Anorexia Nervosa (8) |
| Eating Disorder NOS (8) | |
| Bulimia (1) | |
|
| |
| Adjustment Disorders (13) | Adjustment Disorders/Reaction (13) |
N=number of encounters; NOS=not otherwise specified; OCD=obsessive compulsive disorder; PTSD=post-traumatic stress disorder; GI=gastrointestinal; ADHD=attention deficit and hyperactivity disorder;
PED interventions
The majority of patient encounters (52%) underwent a laboratory workup. The most frequent laboratory test was to examine patient electrolytes in almost half of the encounters (49%). Nearly half the patient encounters (45%) underwent a urine drug screen. The most frequent other labs ordered in decreasing frequency included a complete blood count (39%), blood ethanol level (31%), thyroid studies of either free T4 or thyroid stimulating hormone (29%), and salicylate/acetaminophen levels (26% of encounters).
Restraint use was analyzed including physical or chemical restraints as defined above. Approximately 33% of encounters had either chemical or physical restraints. 170 patient encounters (23%) received chemical restraints with lorazepam being the most common (73%) and the following medications used in decreasing order of frequency included olanzapine (13%), midazolam (11%), haloperidol (2%) and ziprasidone (1%). Physical restraints were ordered in 135 encounters (18%). There were 61 patient encounters (8%) where patients received both chemical and physical restraints. The time from PED arrival to restraint order was also collected. For patients receiving a chemical restraint, on average this occurred 5 hours and 27 minutes into their stay. When a physical restraint was ordered, the average time to order was 4 hours and 35 minutes.
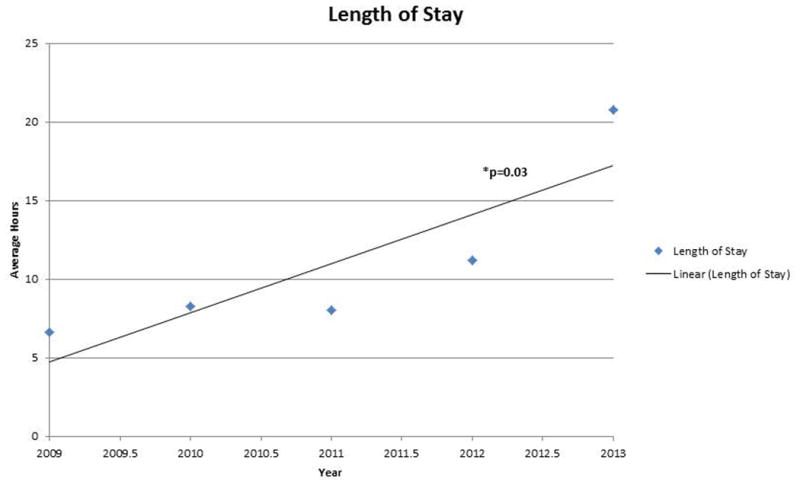
Length of Stay
The average LOS for the entire study population was 11.1 hours (SD 23.3 hours). There was a statistically significant (p<0.001) increase in the mean length of stay (LOS) over the study time period from 6.7 hours in 2009 to 20.8 hours in 2013 (Figure 1). This increase remained significant after controlling for PED admission rate, PED overall LOS and total boarding time (Table 2), and the adjusted annual increase was 0.94 hours (SE 0.44; P = 0.0367). Maximum LOS also increased every year from 54.2 hours in 2009 to 110.4 hours in 2010 was, 115.7 hours in 2011, 118.8 hours in 2012 and 144.5 hours in 2013. There was one patient in 2013 that had a LOS of 337.2 hours (over 14 days) and this was felt to be a significant outlier, not representing the overall trend of LOS so was not included in the LOS analysis. There was no statistical difference in LOS for patients that were suicidal compared to non-suicidal (P = 0.62).
Figure 1. Length of Stay.
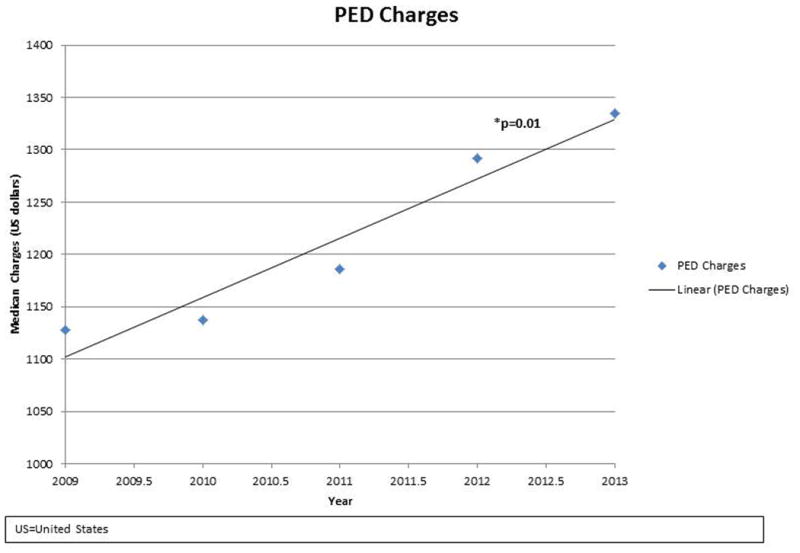
Charges
PED charges were obtained from the billing office for each encounter. If a patient was admitted, we only included the charges incurred in the PED and did not include charges incurred during their inpatient stay. The median overall PED charges for the entire study population were $1208 (inter-quartile range, 779 to 1768). There was a statistically significant (p = 0.0022) increase in PED charges over the study period (Figure 2, Table 2). This increase remained significant after adjusting the patient LOS with an adjusted 4% increase each year (SE 1.5%; P = 0.011). Increased LOS was also significantly associated with increased charges and for each hour increase in LOS, the charges increases by 0.3% (SE 0.1%, p = 0.0062). There was no statistical difference in the charges incurred for suicidal patients compared to non-suicidal encounters (P = 0.46).
Figure 2. PED Charges.
Discussion
Mental health visits in the PED are increasing over time and in our center have significantly increased in proportion to all PED visits. We also find that LOS and charges have increased over time after controlling for admission rates and other confounders likely indicating that the demand for inpatient pediatric mental health services is growing more quickly than the supply of inpatient beds with the PED serving as a monitored holding area for patients awaiting admission. The resource utilization in this group of patients is high as this study shows frequent arrivals by ambulance, use of laboratory testing, and long lengths of stay that reduce beds available for seeing new patients and require significant nursing resources in the PED. These findings largely mirror those seen in previous studies, matching the historical trend of increasing mental health complaints in the PED, though our results provide more recent data and provide more detail on resource utilization in the specific environment of a tertiary care PED without an onsite inpatient mental health unit which must transfer patients in need of inpatient mental health services.
When compared to previous studies15,17, the LOS was higher in our study population. This may reflect current national trends, but may also reflect a more acute mismatch of high demand for inpatient services relative to bed availability at the state level, as the acute inpatient pediatric mental health resources in our relatively sparsely populated state are limited to 2 small facilities in the major urban metro area. Patients in our PED who need acute psychiatric admission are not admitted to the general ward, but wait in our PED while awaiting transfer to a facility with an inpatient unit. Though our study found relatively high length of stay, our admission/transfer rate was much lower at approximately 20% compared to 30-50% in previous studies. The relatively low admission rate may be associated with long LOS in that patients who have stayed in the ED for several days after an acute mental health crisis may have stabilized and be more amenable to an outpatient care plan. In addition, providers who are making disposition decisions are incentivized to form outpatient plans given the burden of sometimes week long ED stays. It is critical to determine if this is a current national trend, or if it is a local phenomenon alone. With a national shortage of inpatient pediatric psychiatric beds, we suspect we are not the only institution seeing this change over the last several years.
The majority of psychiatric patients undergo laboratory workup in the PED. This is generally a standard at most centers in preparation for admission and medical clearance to an inpatient ward. However, the utility of these tests and the resources they employ is questionable. At our center, there is an order set for these, but no standing orders or clinical pathway that generates automatic labs. A recent study by Santiago, et al.20 examined these issues in the ED. In their study they noted that over half of all the psychiatric patients in their study underwent a laboratory evaluation. Of the patients that had labs drawn, half of them were for medically indicated reasons and half were ordered for the purpose of admission or transfer; thus not medically indicated by their study definition. Of the patients that had them drawn for a medical indication such as abdominal pain or ingestion, 44% had abnormal results and only 5.4% of them required an intervention. Of the patients who had them drawn for a non-medical indication, 9% had an abnormal result, but no patients required any medical intervention. They defined abnormal results as anything that was abnormal for the laboratory standard ranges. Although the test was considered out of the normal range, this does not mean that it had clinical relevance highlighted by the low intervention rate. Our study did not record the results of laboratory tests, but demonstrated a similar number of encounters undergoing testing. These studies raise the question of whether patients need extensive laboratory evaluations in the future as presentations are increasing and a specific clinical indication may not exist.
Approximately one third of encounters during this time period underwent either chemical or physical restraints. These numbers are higher than previous reports that were generally between 6-10%15,20-22. The previous study by Santiago, et al.20 commented on the environment of the PED and how it may increase the likelihood of dangerous behavior among psychiatric patients. Previous inpatient studies23,24 have demonstrated restraint use rates of 40-60% which is much closer to our reported rate. This is likely due to our long lengths of stay which are sometimes comparable to inpatient lengths of stay. The average time from PED arrival to the actual EMR order for a chemical or physical restraint was 5 hours 27 minutes and 4 hours 35 minutes respectively. It is not clear how this compares to inpatient treatment facilities. Another potential contributing factor to restraint use is that the ED environment is not ideal for mental health care. EDs are generally not locked units in that patients can leave the unit as they please. Thus patients require 1-on-1 supervision and are generally confined to their rooms most of the day, which may increase agitation and restraint use compared to a secure mental health unit where patients may have more space to move freely. In addition, the ED environment is not conducive to good sleep hygiene which may increase agitation and the need for chemical restraint.
This study has several limitations. First, our study was from a single center which may or may not be reflective of current national trends. However, we do feel that the data are novel and useful to other clinicians, policymakers, and administrators in that our findings reflect practice at a tertiary care PED without an associated inpatient psychiatric unit which has not been reported on previously. The largest challenge for our center is the children who are in high need for acute psychiatric hospitalization and outpatient safety plans cannot be established. This study includes all patients with mental health diagnoses, but includes children who may not be seen by the psychiatry team; for example a freshman college student with acute alcohol intoxication, but without any intent to harm themselves. This intoxicated patient will be evaluated by a social worker in our ED and a discussion is made between the PED physician and social work staff about the need for psychiatric evaluation, as with all patients with mental health concerns. Future studies are needed to limit the population to patients seen by psychiatry to investigate if length of stay and resource utilization is even higher in this subpopulation. As a retrospective study, the data are dependent on the available data in the EMR and manual chart abstraction.
In an effort to address the rising mental health needs in our PED, our institution has developed a children's mental health committee focused on systematic change and best practice to both identify and better serve this patient population. As a potential solution, our Child Psychiatry Consultation/Liaison Service has increased Child Psychiatry full-time employment percentage (FTE) and brought on a full-time Licensed Clinician Social Worker. With the expansion of the service the goal is to improve patient care (ie. reduce restraint use, initiate therapy while developing dispositions) in the hospital and incorporate outreach services to decrease length of stays. By starting therapy in the PED while awaiting further disposition, it may be possible to establish a safety plan and divert inpatient admission. Outreach services will consist of the Clinical Social Worker providing short-term acute stabilization care in patient's homes and community while coordinating patient's long-term mental health care. This program has the potential to address a growing need in our PED and we hope to publish data on its efficacy in the future. It will be important for all national centers to develop innovative programs to continue to advance and improve the care we provide children with mental health needs in the PED.
As community services remain limited for pediatric mental health, care provided and resources used in our PED are significantly increasing. As a tertiary pediatric center without an inpatient psychiatric unit, LOS has increased out of proportion to other measures. Further research is necessary to determine national trends in pediatric psychiatric care in the PED.
Acknowledgments
This publication was supported by the Research Data Warehouse at the Oregon Clinical and Translational Research Institute (OCTRI), grant number (UL1TR000128) from the National Center for Advancing Translational Sciences (NCATS) at the National Institutes of Health (NIH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
The authors have no financial disclosures or conflicts of interest
References
- 1.Friedman R, Katz-Leavy J, Manderscheid R, et al. Prevalence of serious emotional disturbance in children and adolescents. In: Manderscheid RW, Sonnenschein MA, editors. Mental Health, United States. Washington, DC: US Government Printing Office; 1996. pp. 77–112. [Google Scholar]
- 2.Dolan MA, Fein JA Committee on Pediatric Emergency Medicine. Pediatric and adolescent mental health emergencies in the emergency medical services system. Pediatrics. 2011 May;127(5):e1356–66. doi: 10.1542/peds.2011-0522. [DOI] [PubMed] [Google Scholar]
- 3.American Academy of Pediatrics; American College of Emergency Physicians. Dolan MA, Mace SE. Pediatric mental health emergencies in the emergency medical services system. American College of Emergency Physicians. Ann Emerg Med. 2006 Oct;48(4):484–6. doi: 10.1016/j.annemergmed.2006.08.015. [DOI] [PubMed] [Google Scholar]
- 4.Sater N, Constantino JN. Pediatric emergencies in children with psychiatric conditions. Pediatr Emerg Care. 1998 Feb;14(1):42–50. doi: 10.1097/00006565-199802000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Christodulu KV, Lichenstein R, Weist MD, et al. Psychiatric emergencies in children. Pediatr Emerg Care. 2002 Aug;18(4):268–70. doi: 10.1097/00006565-200208000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Sills MR, Bland SD. Summary statistics for pediatric psychiatric visits to US emergency departments, 1993-1999. Pediatrics. 2002 Oct;110(4):e40. doi: 10.1542/peds.110.4.e40. [DOI] [PubMed] [Google Scholar]
- 7.NHAMCSdescription. US Centers for Disease Control and Prevention Web site. [Accessed August 11, 2012]; http://www.cdc.gov/nchs/about/major/ahcd/nhamcsds.htm.
- 8.Case SD, Case BG, Olfson M, et al. Length of stay of pediatric mental health emergency department visits in the United States. J Am Acad Child Adolesc Psychiatry. 2011 Nov;50(11):1110–9. doi: 10.1016/j.jaac.2011.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grupp-Phelan J, Harman JS, Kelleher KJ. Trends in mental health and chronic condition visits by children presenting for care at U.S. emergency departments. Public Health Rep. 2007 Jan-Feb;122(1):55–61. doi: 10.1177/003335490712200108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hilt RJ, Woodward TA. Agitation treatment for pediatric emergency patients. J Am Acad Child Adolesc Psychiatry. 2008 Feb;47(2):132–8. doi: 10.1097/chi.0b013e31815d95fd. [DOI] [PubMed] [Google Scholar]
- 11.Adimando AJ, Poncin YB, Baum CR. Pharmacological management of the agitated pediatric patient. Pediatr Emerg Care. 2010 Nov;26(11):856–60. doi: 10.1097/PEC.0b013e3181f9dce4. [DOI] [PubMed] [Google Scholar]
- 12.Waseem M, Prasankumar R, Pagan K, et al. A retrospective look at length of stay for pediatric psychiatric patients in an urban emergency department. Pediatr Emerg Care. 2011 Mar;27(3):170–3. doi: 10.1097/PEC.0b013e31820d644b. [DOI] [PubMed] [Google Scholar]
- 13.Mahajan P, Thomas R, Rosenberg D, et al. Evaluation of a child-guidance model for visits for mental disorders to an inner city pediatric emergency department. Pediatr Emerg Care. 2007;23(4):212–217. doi: 10.1097/PEC.0b013e31803e177f. [DOI] [PubMed] [Google Scholar]
- 14.Santiago LI, Tunik MG, Foltin GL, et al. Children requiring psychiatric consultation in the pediatric emergency department: epidemiology, resource utilization, and complications. Pediatr Emerg Care. 2006 Feb;22(2):85–9. doi: 10.1097/01.pec.0000199568.94758.6e. [DOI] [PubMed] [Google Scholar]
- 15.Grupp-Phelan J, Mahajan P, Foltin GL, et al. Pediatric Emergency Care Applied Research Network. Referral and resource use patterns for psychiatric-related visits to pediatric emergency departments. Pediatr Emerg Care. 2009 Apr;25(4):217–20. doi: 10.1097/pec.0b013e31819e3523. [DOI] [PubMed] [Google Scholar]
- 16.Wharff EA, Ginnis KB, Ross AM, et al. Predictors of psychiatric boarding in the pediatric emergency department: implications for emergency care. Pediatr Emerg Care. 2011 Jun;27(6):483–9. doi: 10.1097/PEC.0b013e31821d8571. [DOI] [PubMed] [Google Scholar]
- 17.Mahajan P, Alpern ER, Grupp-Phelan J, et al. Pediatric Emergency Care Applied Research Network (PECARN) Epidemiology of psychiatric-related visits to emergency departments in a multicenter collaborative research pediatric network. Pediatr Emerg Care. 2009 Nov;25(11):715–20. doi: 10.1097/PEC.0b013e3181bec82f. [DOI] [PubMed] [Google Scholar]
- 18.Frosch E, dosReis S, Maloney K. Connections to outpatient mental health care of youths with repeat emergency department visits for psychiatric crises. Psychiatr Serv. 2011 Jun;62(6):646–9. doi: 10.1176/ps.62.6.pss6206_0646. [DOI] [PubMed] [Google Scholar]
- 19.Wharff EA, Ginnis KM, Ross AM. Family-based crisis intervention with suicidal adolescents in the emergency room: a pilot study. Soc Work. 2012 Apr;57(2):133–43. doi: 10.1093/sw/sws017. [DOI] [PubMed] [Google Scholar]
- 20.Santiago LI, Tunik MG, Foltin GL, et al. Children requiring psychiatric consultation in the pediatric emergency department: epidemiology, resource utilization, and complications. Pediatr Emerg Care. 2006 Feb;22(2):85–9. doi: 10.1097/01.pec.0000199568.94758.6e. [DOI] [PubMed] [Google Scholar]
- 21.Dorfman DH, Kastner B. The use of restraint for pediatric psychiatric patients in emergency departments. Pediatr Emerg Care. 2004 Mar;20(3):151–6. doi: 10.1097/01.pec.0000117921.65522.fd. [DOI] [PubMed] [Google Scholar]
- 22.Dorfman DH, Mehta SD. Restraint use for psychiatric patients in the pediatric emergency department. Pediatr Emerg Care. 2006 Jan;22(1):7–12. doi: 10.1097/01.pec.0000195758.12447.69. [DOI] [PubMed] [Google Scholar]
- 23.Troutman B, Myers K, Borchardt C, et al. Case study: when restraints are the least restrictive alternative for managing aggression. J Am Acad Child Adolesc Psychiatry. 1998 May;37(5):554–8. doi: 10.1097/00004583-199805000-00018. [DOI] [PubMed] [Google Scholar]
- 24.Donovan A, Plant R, Peller A, et al. Two-year trends in the use of seclusion and restraint among psychiatrically hospitalized youths. Psychiatr Serv. 2003 Jul;54(7):987–93. doi: 10.1176/appi.ps.54.7.987. [DOI] [PubMed] [Google Scholar]


