Abstract
The aim of this study was to validate a method for fast three-dimensional (3D) superimposition of cone beam computed tomography (CBCT) in growing patients and adults (surgical cases). The sample consisted of CBCT scans of 18 patients. For 10 patients, as the gold standard, the spatial position of the pretreatment CBCT was reoriented, saved as a reoriented volume, and then superimposed on the original image. For eight patients, four non-growing and four growing, the pre- and post-treatment scans were superimposed. Fast voxel-based superimposition was performed, with registration at the anterior cranial base. This superimposition process took 10–15 s. The fit of the cranial base superimposition was verified by qualitative visualization of the semi-transparent axial, sagittal, and coronal cross-sectional slices of all corresponding anatomical structures. Virtual 3D surface models of the skull were generated via threshold segmentation, and superimposition errors in the reoriented models and the results of treatment for the treated cases were evaluated by 3D surface distances on colour-coded maps. The superimposition error of the spatial reorientation and for growing and non-growing patients was <0.5 mm, which is acceptable and clinically insignificant. The voxel-based superimposition method evaluated was reproducible in different clinical conditions, rapid, and applicable for research and clinical practice.
Keywords: cone-beam computed tomography, voxel-based superimposition, 3D image registration, orthodontic and orthopaedic treatment, orthognathic surgery
Cone beam computed tomography (CBCT) has become a well-established diagnostic tool in dentistry.1–8 In orthodontics and in oral and maxillofacial surgery, CBCT now allows clinicians to better identify and distinguish treatment outcomes. While two-dimensional (2D) cephalometric superimposition is the conventional method used to evaluate growth and treatment outcomes, improvements in image registration algorithms have made the superimposition of CBCT volumes the state-of-the-art technique for outcomes assessment.
In medical imaging, the process of spatially superimposing three-dimensional (3D) images obtained from different imaging modalities is also called image registration, or fusion.9 The superimposition of CBCT volumes in 3D space when changes in shape and position of the craniofacial components have occurred over time or with treatment is challenging and requires knowledge of the different types of superimposition. The three basic types of superimposition algorithm are: (1) point landmark-based, (2) surface-based, and (3) voxel-based.10 The latter, and most efficient method, compares the non-changing reference structures in volumetric data voxel by voxel, does not depend on landmark identification as in the point landmark-based method, and is not limited by segmentation errors as in the surface-based method.
Cevidanes et al.11 were the first to introduce the voxel-based method for fully automated 3D superimposition of CBCT volumes into dentistry. The method proposed in that study was based on mutual information theory10 and required the construction of surface models of the reference structure prior to the registration steps. The application of this method in both growing and non-growing subjects has been described in the literature.4,5,11,12 The drawbacks are that the superimposition process requires several different steps in various software programmes and is time-consuming (45–60 min). In 2010, Choi and Mah13 introduced a new method for cranial base superimposition that is also voxel-based, but does not require the construction of 3D surface models prior to the registration process. They also added volume and slice visualization capabilities, providing a clinician-friendly user interface. The result was a new software programme (the fusion module of OnDe-mand3D; Cybermed, Seoul, Korea) that performs CBCT volume superimpositions faster (10–15 s), with fewer steps required. While some research studies14–16 have applied the superimposition method introduced by Choi and Mah13 in the OnDemand3D software, there has been no published validation study of this method for fast CBCT volume superimposition in growing patients and adults. There appears to be a lack of scientific evidence regarding the use of this method for fast superimposition of CBCT at the anterior cranial base, especially for the longitudinal assessment of growth and treatment changes in young patients.
The aim of this study was to evaluate a fast method for 3D superimposition of CBCT volumes. Specifically, this study first tested whether there are differences when the same CBCT volumes, with different spatial orientations, are superimposed at the anterior cranial base. Second, this study tested whether there are differences in the anterior cranial base when longitudinal CBCT volumes of growing patients and adults, which also present maxilla–mandibular changes due to growth and/or treatment response, are superimposed at the anterior cranial base.
Methods
This was a retrospective study. Records were obtained from the patient database of the department of orthodontics and included pre-treatment and post-treatment CBCT scans. The sample consisted of the CBCT scans of 18 patients. For 10 patients, as a gold standard, the spatial position of the pretreatment CBCT volume was reoriented, saved as a reoriented volume, and then superimposed on the original image (Fig. 1). For eight patients – four non-growing and four growing – pre- and post-treatment scans were superimposed. The 10 pre-treatment scans (gold standard) were obtained from patients with a mean age of 11.4 ± 1 years. The four non-growing adult patients (mean age 26.3 ± 5.7 years) had CBCT scans taken pre- and 1 year post-orthognathic surgery. The four growing patients (mean age 9.5 ± 1.8 years) had CBCT scans taken pre- and post-treatment with rapid palatal expansion (RPE). The CBCT scans were obtained using an i-CAT scanner (Imaging Sciences International, Hatfield, PA, USA) set at 120 kVp, 8 mA, large field of view, and scan time of 40 s. The images were reconstructed with 0.25-mm slice thickness and exported as Digital Imaging and Communications in Medicine (DICOM) files.17
Fig. 1.
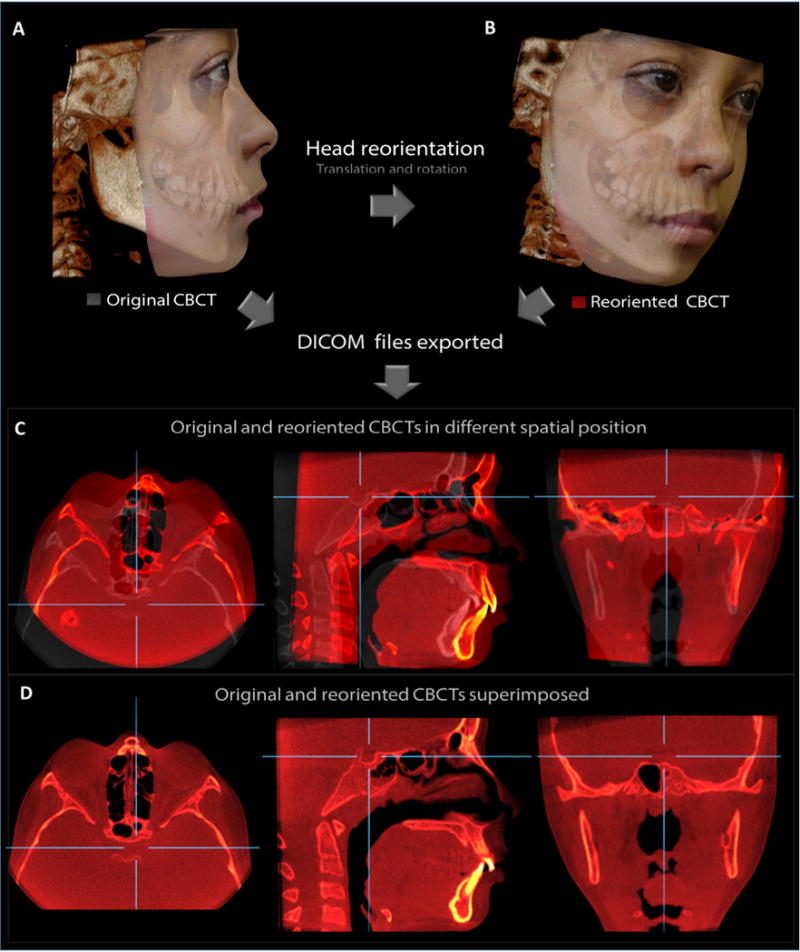
Example of a case used as the gold standard. (A) Original CBCT. (B) Same patient CBCT reoriented to a different spatial position. (C) Slices of multiplanar reconstruction showing original (grey) and reoriented CBCT (red) before superimposition. (D) Slices showing both CBCTs after superimposition at the anterior cranial base.
Creating CBCT volumes with different spatial orientations
The DICOM files corresponding to the pretreatment CBCT scans of the 10 growing patients (gold standard) were imported into OnDemand3D software (version 1.0.9.1451; Cybermed, Seoul, Korea) and organized in the database management module. Each CBCT volume was opened and the patient’s head was reoriented in space (translation and rotation) to a different spatial position and data exported in a new DICOM file. Thus, for each original CBCT volume, a second CBCT volume was created with the same voxel size but with different head orientation (Fig. 1A and B). This procedure was performed for all 10 pre-treatment CBCT volumes, creating 10 additional CBCT volumes with different head orientation.
CBCT volume superimposition
For the fully automatic voxel-based rigid registration, the fusion module in OnDemand3D was used. Axial, sagittal, and coronal slice views of the volumes were used to select the anatomical structures of the anterior cranial base in the CBCT volumes (Fig. 2A and B). Next, the OnDemand3D automated registration tool was used to perform the rigid registration (translation and rotation) that optimally aligned the reoriented CBCT volume to the original CBCT volume, using the intensity of the grey levels for each voxel in the anterior cranial base of the two CBCT volumes. The same voxel-based superimposition procedure was used to align pre-treatment and post-treatment CBCT volumes of growing patients subjected to RPE and adults subjected to orthognathic surgery, using the anterior cranial base as reference (Fig. 2C and D). The superimposition process took a total of 10–15 s to complete.
Fig. 2.
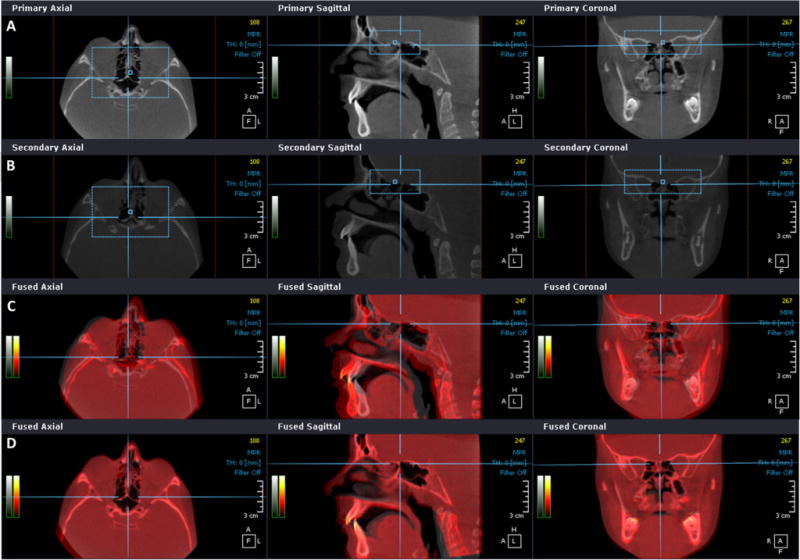
OnDemand3D voxel-based superimposition process. (A) Anterior cranial base selection (blue rectangle) in multiplanar slices of pretreatment CBCT and (B) post-treatment CBCT. (C) Multiplanar slices view of pre-treatment (grey) and post-treatment (red) CBCT files before superimposition and (D) after superimposition at the anterior cranial base. (For interpretation of the references to colour in figure legend, the reader is referred to the web version of the article.)
Superimposition assessment
The precision of the OnDemand3D voxel-based superimpositions was verified by quantification of the surface distances using closest-point colour maps on 3D surface models, as done in previous studies for growing patients.18,19 It was also assessed by qualitative visualization of the semi-transparent axial, sagittal, and coronal cross-sectional slices of all corresponding anatomical structures between the original and reoriented scans, as well as the pre-treatment and post-treatment scans (Figs 3–5). To measure the outcomes of the superimposition, after the registration process, the superimposed CBCT volumes were exported as DICOM files using the OnDemand3D programme and imported into ITK-SNAP software programme (http://www.itksnap.org) for segmentation and construction of 3D virtual surface models of the skull.20 In the ITK-SNAP programme, automatic segmentation was performed for each CBCT volume in four different steps: mandible, maxilla, frontal bone/anterior cranial fossa, and middle cranial fossa. The 3D virtual surface model of the skull generated was then exported as a stereolithography file (STL) using the ITK-SNAP programme and converted to an Open Inventor file (IV) using STL to SGI Inventor 2.0 Utility Beta programme (developed by Reuben Reyes, hitechmax@austin.rr. com). This IV extension allowed the 3D virtual surface model of the skull to be opened in the Cranio-MaxilloFacial application software (CMFapp, developed at the M. E. Müller Institute for Surgical Technology and Biomechanics, University of Bern, Bern, Switzerland),21 which calculates the closest point surface distance between thousands of surface triangles in the 3D surface models; the resulting colour-coded surface distance maps allow quantification of the registration errors (Figs 3C, 4C, and 5C). The complete method is summarized in Table 1.
Fig. 3.
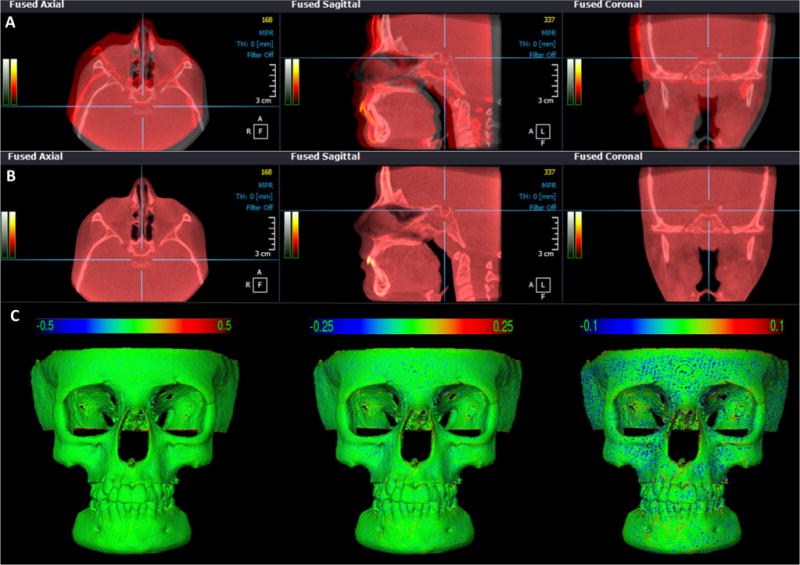
CBCT superimposition of a gold standard patient. (A) Multiplanar slices of original CBCT (grey) and reoriented CBCT (red) files before superimposition and (B) after superimposition at the anterior cranial base, in OnDemand3D. Note the complete correspondence of registration in all areas of the skull. (C) Skull models after superimposition showing 3D displacements (registration error) via colour maps with scales of 0.5 mm, 0.25 mm, and 0.10 mm. Positive and negative values indicate outward (red) and inward (blue) changes, respectively. Note the error was less than 0.25 mm (CMF application software). (For interpretation of the references to colour in figure legend, the reader is referred to the web version of the article.)
Fig. 5.
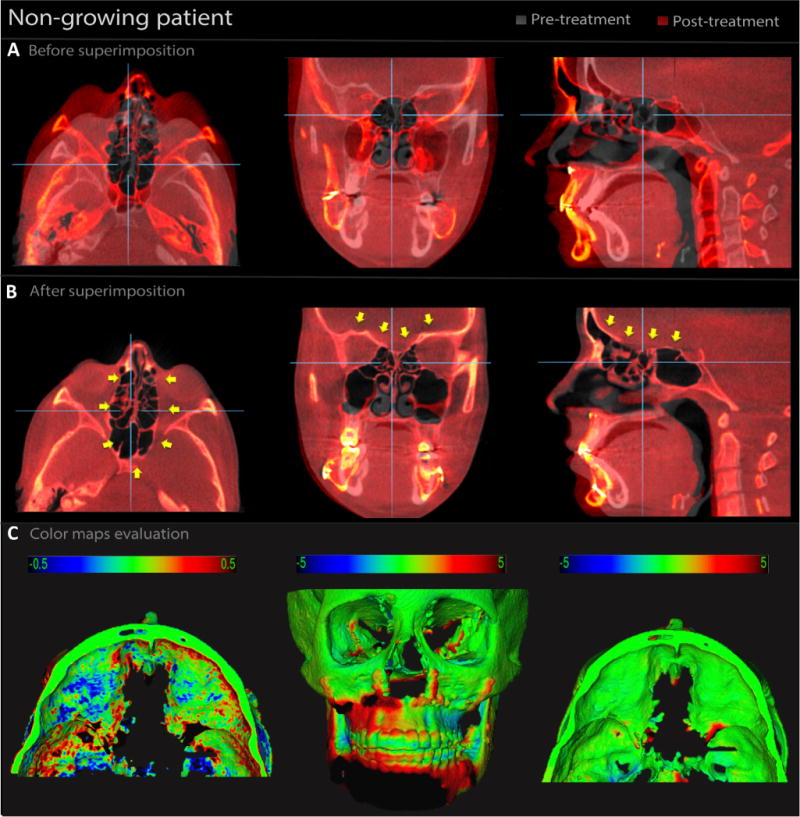
CBCT superimposition of an adult patient subjected to orthognathic surgery with 1-year follow-up. (A) Multiplanar slices of pre-treatment CBCT (grey) and post-treatment CBCT (red) before superimposition and (B) after superimposition, in OnDemand3D. Note the complete correspondence of registration at the anterior cranial base (yellow arrows). (C) 3D models after superimposition showing 3D displacements via colour maps. In the 0.5-mm colour map, the black areas represent changes of 0.5 mm, blue/red areas represent changes less than 0.5 mm, and green areas represents no changes. In the 5-mm colour map, the areas in black, red, and blue are changes due to the surgical treatment. The changes at the cranial base were minimal (green) (CMF application software). (For interpretation of the references to colour in figure legend, the reader is referred to the web version of the article.)
Fig. 4.
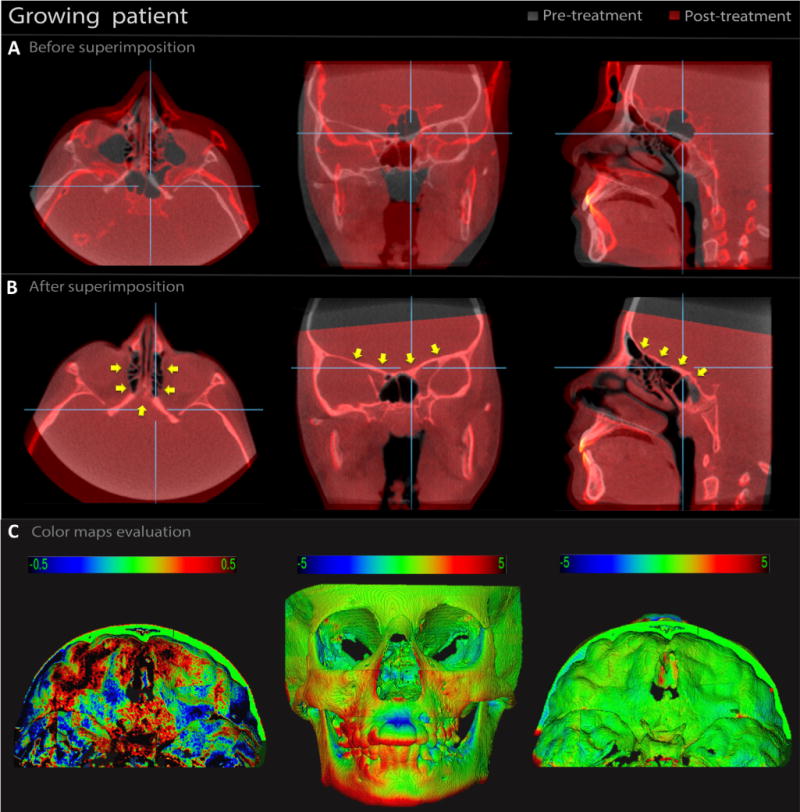
CBCT superimposition of a growing patient subjected to rapid palatal expansion (RPE) with 1-year follow-up. (A) Multiplanar slices of pre-treatment CBCT (grey) and post-treatment CBCT (red) before superimposition and (B) after superimposition, in OnDemand3D. Note the complete correspondence of registration at the anterior cranial base (yellow arrows). (C) 3D models after superimposition showing 3D displacements via colour maps. In the 0.5-mm colour map, the black areas represent changes of 0.5 mm, blue/red areas represent changes less than 0.5 mm, and green areas represent no changes. In the 5-mm colour map, the areas in black, red, and blue are due to the RPE and normal growth. The changes at the cranial base were minimal (green) (CMF application software). (For interpretation of the references to colour in figure legend, the reader is referred to the web version of the article.)
Table 1.
Software programmes used in this study.
| Software | Purpose | |
|---|---|---|
| OnDemand3D | Superimposition process | Registration of different CBCTs at the anterior cranial base |
| ITK-Snap | Superimposition evaluation | Construction of 3D surface models using DICOM files and export as STL |
| STL to SGI Inventor 2.0 | Superimposition evaluation | Convert files from STL to IV |
| CMF app | Superimposition evaluation | Provided closest point colour maps between registered 3D surface models |
CBCT, cone beam computed tomography; 3D, three-dimensional; DICOM, Digital Imaging and Communications in Medicine; SGI, Silicon Graphics Image file; STL, stereolithography file; IV, Open Inventor file.
Results
The superimposition results for the original and reoriented CBCT scans of the 10 growing patients were similar. The visualization of the semi-transparent axial, sagittal, and coronal cross-sectional slices of all corresponding anatomical structures confirmed the adequate registration of all skull structures, including the anterior cranial base, in all axial, sagittal, and coronal slices (Fig. 3B). The quantification of the superimposition errors by colour-coded surface distances revealed that the error was less than 0.25 mm (Fig. 3C).
The superimposition results for longitudinal scans of growing patients and adults were similar. The visualization of the semi-transparent axial, sagittal, and coronal cross-sectional slices of all corresponding anatomical structures confirmed the adequate registration of the extremely complex cranial base structures, such as the ethmoidal air cells, for both growing patients (Fig. 4B) and adults (Fig. 5B). The quantification of the superimposition errors by colour-coded surface distances revealed that distances in the anterior cranial base between registered surface models were less than 0.5 mm for most regions for both growing patients (Fig. 4C) and adults (Fig. 5C).
Discussion
CBCT is currently a well-established diagnostic tool for the 3D evaluation of patients, especially orthodontic–surgical cases. This study validated a method for fast CBCT superimposition in growing patients and adults.
Improvements in image registration algorithms have led to the development of new methods for CBCT volume superimposition. McCance et al. proposed a method for cranial base superimposition with CT scans using five landmarks in areas not affected by surgery in non-growing patients.22 Kawamata et al. suggested a similar method, rotating semi-transparent pre-surgery and post-surgery models aiming to overlap them in the same structure.23 These point landmark-based methods for CBCT superimposition are also presented in the 2014 versions of the software programmes Dolphin3D (Dolphin Imaging and Management Solutions, Chatsworth, CA, USA) and InVivo Dental (Anatomage, San Jose, CA, USA) and have the disadvantage of being observer-dependent. The first method introduced by Cevidanes et al. is more efficient than the point landmark-based method because it compares the non-changing reference structures in volumetric data voxel by voxel, is observer-independent, and does not rely on specific landmarks.11 However, this registration process lacks a clinician-friendly user interface and visualization tool, uses several different steps in various software programmes, requires extensive training, and is time-consuming (45 to 60 min), making the process unworkable for clinicians and only suitable for research. With recent improvements in computing capabilities, the time for image registration has decreased. Nada et al.24 used the voxel-based registration method of Maxilim software (Medicim NV, Mechelen, Belgium) for the evaluation of surgical orthodontic patients. They reported that it took 30 to 40 min to complete a single superimposition of two longitudinal CBCT volumes. Compared to these studies, the registration method evaluated in the present study is faster (10–15 s).
This study validated the superimposition method introduced by Choi and Mah for voxel-based registration.13 The method used in this study for superimposition of longitudinal CBCT volumes in growing patients and adults has advantages over previously used voxel-based methods.4–6,11,12 The advantages of this method are that it is rapid (takes about 10 to 15 s), has a user-friendly software interface, does not require extensive training, uses only one software programme, and can be used by the clinician. Additional advantages of the method presented are that the CBCT volume superimpositions are fast, even when the CBCT scans have small voxel sizes (0.25 mm) and high spatial resolution, and the registration process does not require previous segmentation to designate the area of superimposition. Also, CBCT superim-positions with registration at areas outside the cranial base are possible and can potentially be applied for regional superimpositions, although this was not tested in the present study. Park et al. have recently used regional superimpositions with OnDemand3D software to evaluate the condylar head remodelling after bimaxillary surgery using rigid registration at the condylar neck and posterior ramal area of pre- and post-operative CBCT Images.14
In this validation study, the construction of standardized 3D surface models and part-comparison analysis with colour maps confirmed the accuracy of the voxel-based superimposition method. The differences observed in the colour-coded surface distance maps for the 10 pre-treatment CBCT scans were minimal, at less than 0.25 mm (Fig. 3). However, superimposition of the same CBCT volumes, with different spatial orientation, should be evaluated with caution because they have the same grey level intensity and no modifications by growth and/or treatment. The challenge for image registration is to superimpose CBCT volumes of patients with craniofacial modifications due to the normal growth and/or treatment response at different time-points. In these situations, the CBCT volumes may have different grey level intensity, field of view, and dental/skeletal components modified by growth and/or treatments, making the registration process difficult and prone to failure. Additionally, CBCT scans obtained with different scanners may have different grey levels,25 which could affect the superimposition process.
For these reasons, this study tested the superimpositions of longitudinal CBCT volumes with a 1-year interval for growing patients treated with RPE and adult patients treated with orthognathic surgery. The results of the colour-coded map analysis revealed that distances in the anterior cranial base between registered surface models were <0.5 mm (green colour-code areas) for most regions, indicating adequate superimposition for both growing patients and adults. Some areas of larger surface distances, as shown in black, red, and blue colour-coded areas displayed in the superior view of the anterior cranial base (Figs 4C and 5C), did not represent superimposition errors; this was confirmed in the semi-transparent multiplanar cross-sectional slices (Figs 4B and 5B). Since the CBCT scans obtained at different time-points had differences in grey levels for the same anatomical structures (i.e., cranial base), the automatic segmentation was not performed by using the same threshold interval. This variation introduced by the user input to define the properties of 3D surface model creation leads to small surface variations in the cranial base. Additionally, areas with low grey-scale contrast such as the ethmoidal air cells were not included automatically in the segmentation. In these situations, manual editing was necessary and produced slightly different outlining of surface boundaries during the segmentation process, as demonstrated in a previous study.26 This could explain the black, red, and blue areas in the internal surface of the cranial base.
For some scans, the registration of the two CBCT volumes failed, requiring two or three repeat procedures. In these cases, it was necessary to resize the selection area for registration (anterior cranial base) in both primary and secondary volumes in order to obtain an adequate superimposition. In a previous study, Alexandroni also reported similar failed attempts using the same superimposition method to evaluate orthognathic surgery skeletal prediction in 44 patients.16 However, only visual inspection was used to verify adequate CBCT volume superimpositions. The requirement for repeated registration procedures in the present study could have been due to the small area used for CBCT volume registration (anterior cranial base) in comparison to the global anatomical structure of the dry skull used by Lee et al.27 In addition, the amount of misalignment between the CBCT volumes may have had some influence on the superimposition process. According to Pluim et al., when using registration methods based on mutual information theory, results may be suboptimal, or may even fail, if the initial misalignment of the two images is large or if the overlay region of the two images is relatively small.28 For this reason, it is recommended that a quick manual superimposition is performed prior to the automated superimposition.
Lee et al.27 also evaluated the accuracy of CBCT image registration with OnDemand3D, but using a dry skull with titanium markers, simulating different head orientations. The location of the titanium markers was assessed by two examiners, and the distance between the markers was calculated using a 3D coordinates system. The superimposition mean error was 0.39 mm (±0.142 mm) and there were no significant differences in the dry skull superimpositions. Although they did not evaluate the accuracy of longitudinal CBCT superimposition for growing patients and used the whole cranial base as reference instead of the anterior cranial base, the superimposition results were similar. Nada et al.24 tested the reliability of another commercial voxel-based method using Maxilim software for CBCT superimposition on the anterior cranial base and zygomatic arch of 16 surgical orthodontic patients. The authors reported small average superimposition errors. However the closest-point colour-coded maps used for quantification of errors do not allow local quantification of surface errors and minimize surface differences.
A potential limitation of the OnDemand3D software is that it is only available commercially, whereas the method proposed by Cevidanes et al. in previous studies11,12,19 can be performed using readily available open-source software programmes. In this evaluation, the voxel-based superimposition method tested was precise and not time-consuming. The fast 3D superimposition method of CBCT volumes validated in this study may be applied for the longitudinal assessment of both growing patients and adults. Furthermore, it is considered suitable for both research and clinical practice in the orthodontic and maxillofacial surgery fields, since CBCT is indicated.
Acknowledgments
We would like to thank Robert J. Lee for technical and writing assistance during the preparation of this article.
Funding
Supported by the Brazilian Federal Agency for Support and Evaluation of Graduate Education (CAPES Foundation, process number BEX 5335-11-6.
Footnotes
Competing interests
None declared.
Ethical approval
This study was approved by the Ethics Committee of Pontifical Catholic University of Rio Grande do Sul, Brazil (research protocol CEP 08/04147).
Patient consent
Not required.
References
- 1.Kapila S, Conley RS, Harrell WE., Jr The current status of cone beam computed tomography imaging in orthodontics. Dentomaxillofac Radiol. 2011;40:24–34. doi: 10.1259/dmfr/12615645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weissheimer A, Menezes LM, Sameshima GT, Enciso R, Pham J, Grauer D. Imaging software accuracy for 3-dimensional analysis of the upper airway. Am J Orthod Dentofacial Orthop. 2012;142:801–13. doi: 10.1016/j.ajodo.2012.07.015. [DOI] [PubMed] [Google Scholar]
- 3.Grauer D, Cevidanes LS, Proffit WR. Working with DICOM craniofacial images. Am J Orthod Dentofacial Orthop. 2009;136:460–70. doi: 10.1016/j.ajodo.2009.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cevidanes LH, Heymann G, Cornelis MA, DeClerck HJ, Tulloch JF. Superimposition of 3-dimensional cone-beam computed tomography models of growing patients. Am J Orthod Dentofacial Orthop. 2009;136:94–9. doi: 10.1016/j.ajodo.2009.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cevidanes LH, Motta A, Proffit WR, Ackerman JL, Styner M. Cranial base superimposition for 3-dimensional evaluation of soft-tissue changes. Am J Orthod Dentofacial Orthop. 2010;137(4 Suppl. 1):S120–9. doi: 10.1016/j.ajodo.2009.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cevidanes LH, Tucker S, Styner M, Kim H, Chapuis J, Reyes M, et al. Three-dimensional surgical simulation. Am J Orthod Dentofacial Orthop. 2010;138:361–71. doi: 10.1016/j.ajodo.2009.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cevidanes LH, Alhadidi A, Paniagua B, Styner M, Ludlow J, Mol A, et al. Three-dimensional quantification of mandibular asymmetry through cone-beam computerized tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:757–70. doi: 10.1016/j.tripleo.2011.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cevidanes LH, Hajati AK, Paniagua B, Lim PF, Walker DG, Palconet G, et al. Quantification of condylar resorption in temporomandibular joint osteoarthritis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:110–7. doi: 10.1016/j.tripleo.2010.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li G, Xie H, Ning H, Capala J, Arora BC, Coleman CN, et al. A novel 3D volumetric voxel registration technique for volume-view-guided image registration of multiple imaging modalities. Int J Radiat Oncol Biol Phys. 2005;63:261–73. doi: 10.1016/j.ijrobp.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 10.Maes F, Collignon A, Vandermeulen D, Marchal G, Suetens P. Multimodality image registration by maximization of mutual information. IEEE Trans Med Imaging. 1997;16:187–98. doi: 10.1109/42.563664. [DOI] [PubMed] [Google Scholar]
- 11.Cevidanes LH, Bailey LJ, Tucker GR, Jr, Styner MA, Mol A, Phillips CL, et al. Superimposition of 3D cone-beam CT models of orthognathic surgery patients. Dentomaxillofac Radiol. 2005;34:369–75. doi: 10.1259/dmfr/17102411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cevidanes LH, Styner MA, Proffit WR. Image analysis and superimposition of 3-dimensional cone-beam computed tomography models. Am J Orthod Dentofacial Orthop. 2006;129:611–8. doi: 10.1016/j.ajodo.2005.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Choi J, Mah J. A new method for superimposition of CBCT volumes. J Clin Orthod. 2010;44:303–12. [PubMed] [Google Scholar]
- 14.Park SB, Yang YM, Kim YI, Cho BH, Jung YH, Hwang DS. Effect of bimaxillary surgery on adaptive condylar head remodeling: metric analysis and image interpretation using cone-beam computed tomography volume superimposition. J Oral Maxillofac Surg. 2012;70:1951–9. doi: 10.1016/j.joms.2011.08.017. [DOI] [PubMed] [Google Scholar]
- 15.Park SB, Yoon JK, Kim YI, Hwang DS, Cho BH, Son WS. The evaluation of the nasal morphologic changes after bimaxillary surgery in skeletal class III malocclusion by using the superimposition of cone-beam computed tomography (CBCT) volumes. J Craniomaxillofac Surg. 2012;40:e87–92. doi: 10.1016/j.jcms.2011.05.008. [DOI] [PubMed] [Google Scholar]
- 16.Alexandroni ES. Utilizing voxel based superimposition to assess orthognathic surgical treatment. Los Angeles: University of Southern California; 2012. [Google Scholar]
- 17.DICOM digital imaging and communications in medicine. Rosslyn, VA: National Electrical Manufacturers Association (NEMA); 2011. [Google Scholar]
- 18.De Clerck H, Nguyen T, de Paula LK, Cevidanes L. Three-dimensional assessment of mandibular and glenoid fossa changes after bone-anchored class III intermaxillary traction. Am J Orthod Dentofacial Orthop. 2012;142:25–31. doi: 10.1016/j.ajodo.2012.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nguyen T, Cevidanes L, Cornelis MA, Heymann G, de Paula LK, De Clerck H. Three-dimensional assessment of maxillary changes associated with bone anchored maxillary protraction. Am J Orthod Dentofacial Orthop. 2011;140:790–8. doi: 10.1016/j.ajodo.2011.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yushkevich PA, Piven J, Hazlett HC, Smith RG, Ho S, Gee JC, et al. User-guided 3D active contour segmentation of anatomical structures: significantly improved efficiency and reliability. Neuroimage. 2006;31:1116–28. doi: 10.1016/j.neuroimage.2006.01.015. [DOI] [PubMed] [Google Scholar]
- 21.Chapuis J, Schramm A, Pappas I, Hallermann W, Schwenzer-Zimmerer K, Langlotz F, et al. A new system for computer-aided preoperative planning and intraoperative navigation during corrective jaw surgery. IEEE Trans Inf Technol Biomed. 2007;11:274–87. doi: 10.1109/titb.2006.884372. [DOI] [PubMed] [Google Scholar]
- 22.McCance AM, Moss JP, Fright WR, James DR, Linney AD. A three dimensional analysis of soft and hard tissue changes following bimaxillary orthognathic surgery in skeletal III patients. Br J Oral Maxillofac Surg. 1992;30:305–12. doi: 10.1016/0266-4356(92)90180-q. [DOI] [PubMed] [Google Scholar]
- 23.Kawamata A, Fujishita M, Nagahara K, Kanematu N, Niwa K, Langlais RP. Three-dimensional computed tomography evaluation of postsurgical condylar displacement after mandibular osteotomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85:371–6. doi: 10.1016/s1079-2104(98)90059-2. [DOI] [PubMed] [Google Scholar]
- 24.Nada RM, Maal TJ, Breuning KH, Bergé SJ, Mostafa YA, Kuijpers-Jagtman AM. Accuracy and reproducibility of voxel based superimposition of cone beam computed tomography models on the anterior cranial base and the zygomatic arches. PLoS ONE. 2011;6:e16520. doi: 10.1371/journal.pone.0016520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Azeredo F, de Menezes LM, Enciso R, Weissheimer A, de Oliveira RB. Computed gray levels in multislice and cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2013;144:147–55. doi: 10.1016/j.ajodo.2013.03.013. [DOI] [PubMed] [Google Scholar]
- 26.Lee RJ, Weissheimer A, Pham J, Go L, de Menezes LM, Redmond WR, et al. Three-dimensional monitoring of root movement during orthodontic treatment. Am J Orthod Dentofacial Orthop. 2015;147:132–42. doi: 10.1016/j.ajodo.2014.10.010. [DOI] [PubMed] [Google Scholar]
- 27.Lee JH, Kim MJ, Kim SM, Kwon OH, Kim YK. The 3D CT superimposition method using image fusion based on the maximum mutual information algorithm for the assessment of oral and maxillofacial surgery treatment results. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114:167–74. doi: 10.1016/j.tripleo.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 28.Pluim JP, Maintz JB, Viergever MA. Mutual-information-based registration of medical images: a survey. IEEE Trans Med Imaging. 2003;22:986–1004. doi: 10.1109/TMI.2003.815867. [DOI] [PubMed] [Google Scholar]


