Abstract
Infection is one of the most common complications associated with medical interventions and implants. As tissue engineering strategies to replace missing or damaged tissue advance, the focus on prevention and treatment of concomitant infection has also begun to emerge as an important area of research. Because the in vivo environment is a complex interaction between host tissue, implanted materials, and native immune system that cannot be replicated in vitro, animal models of infection are integral in evaluating the safety and efficacy of experimental treatments for infection. In this review, considerations for selecting an animal model, established models of infection, and areas that require further model development are discussed with regard to cutaneous, fascial, and orthopedic infections.
Keywords: Tissue engineering, infection, in vivo, animal model, preclinical
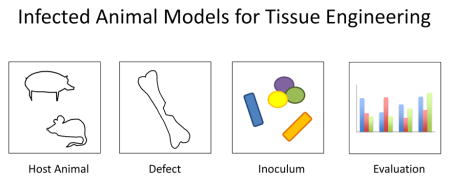
Graphical Abstract
1.0 Introduction
While tissue engineering holds great promise in the restoration of normal structure and function in a variety of disease states, infection continues to remain a significant challenge for the field. Tissue engineering strategies classically involve cells (either implanted or recruited), a scaffold (synthetic or natural), and chemical signals (such as growth factors). Infection prevents normal healing and inhibits the success of tissue-engineered constructs. The inflammatory environment caused by infection diminishes the natural capacity of tissue to heal and alters cellular phenotype [1]. Foreign objects, such as implanted scaffolds intended for cellular infiltration, may also act as a safe haven for bacteria and can result in pathogenic colonization [2, 3]. In addition, the regenerative effects of delivered growth factors, such as bone morphogenetic protein 2 (BMP-2), have been shown to be mitigated in patients with infection [4]. As a common complication associated with wounds and tissue defects, addressing infection is an increasingly important aspect of tissue engineering strategies.
Due to the complex interactions between host and pathogen, in vitro systems cannot faithfully recapitulate conditions of infection and tissue healing. Therefore, there is a need for animal models which reflect tissue infection for evaluating tissue engineering strategies. There are many critical variables to consider when choosing a model of wound infection. In general when choosing any animal model for tissue engineering, one must consider the size and nature of the tissue defect, the physiological and anatomical differences in wound healing between the model and human disease, ethics of animal experimentation, as well as pragmatic aspects such as costs and housing requirements. However, in the case of infected animal models, one must also consider factors such as the species of pathogen (type of inoculum), amount of pathogen (concentration of inoculum), inoculation vehicle, and how the course of infection should be monitored and validated. It is important to note that no animal model can completely recapitulate the human condition, especially in a complex disease state such as infection. As different animal models can reflect different aspects of the same disease, often multiple models (including non-traditional models) are necessary to thoroughly explore a tissue engineering strategy before approval for clinical trials [5]. This review will cover considerations when choosing an infected animal model as well as discuss established models available in several defects (cutaneous, fascial, and orthopedic) as examples.
2.0 Considerations in Model Selection
When selecting or designing an infected animal model to evaluate a tissue engineering strategy, it is important to consider the host animal species and strain, the host animal defect, the pathogen species and strain, the inoculum concentration and vehicle, and many other factors specific to the disease state of interest. It is critical to fully explore previous infected animal models available in the literature and often necessary to conduct pilot studies to ensure an infection has been created that is self-sustaining but does not overwhelm the host. Highlighted below are some specific considerations that are broadly applicable for tissue engineering purposes.
2.1 Host Animal and Defect
Overall, general trends in animal species selection for tissue defects hold true for infected defects. For the purposes of this review, smaller species include mice, rats, and rabbits. Larger species include pig, goat, sheep, dogs, and non-human primates. In addition to model species, strain can be important given physiologic differences such as immune response to infection [6].
In general, small animals are less expensive to purchase and house, require less complex surgical and anaesthetic equipment for tissue defect creation, and present less regulatory challenges for use in research. Infected mouse models have several advantages. Mouse studies are, in general, relatively inexpensive and as a result, can be powered to make strong statistical conclusions. In addition, mouse models are appealing due to the genetic tools available that are relevant to infection, such as strains that have immune deficits or metabolic imbalances [7, 8]. In addition, genetically-modified mice can provide useful tools for understanding pathophysiology- for example, mice modified to have fluorescently-tagged neutrophils have been used to study cutaneous wound healing in real-time [9]. Because mice are small, in vivo imaging of bacteria via bioluminescence or fluorescence is somewhat less challenging since the depth of light penetration is shorter than in larger animals. Finally, there is currently more literature available on small animal models of tissue infection, which is an advantage when selecting an infected model for study.
Larger species tend to more accurately reflect oxygen diffusion limitations, musculoskeletal loads, and permit infected defects more similar in volume and geometry to clinically-relevant sized tissue defects. However, larger species are also more costly, have extra housing requirements, and raise additional ethical questions. In particular, the use of companion animals (such as dogs) and non-human primates raise complex ethical issues and should be avoided if possible.
Once a species and strain is chosen, the intended defect for infection must be designed. While the infected defect should recapitulate the intended human disease state as closely as possible, it may not be anatomically accurate, especially in smaller animals. For example, a subcutaneous pouch model has been established in rats to evaluate different hernia repair meshes for infection prevention [10]. While these meshes were not applied in their anatomically-intended defect (across a tear in the fascia), the model still allows for biomaterial evaluation in an in vivo soft tissue environment with a relatively simple surgery in an inexpensive model. Although these physiologic models can generate preliminary data for tissue engineering strategies, animal models which reflect the correct anatomic defects ultimately need to be utilized before translation [11]. Attention to detail in surgical protocol design is necessary. Seemingly minor decisions can alter infection in an animal model- for example, the choice of local anesthetic can impact the course of infection [12]. External drugs may need to be delivered to create metabolic imbalances [13] or immune suppression [14, 15]. After deciding on the appropriate defect for the animal model, the inoculum (pathogen, dose, and vehicle of infection) can be chosen.
2.2 Inoculum
The species of microorganism chosen for an infected animal model is specific to the human disease being studied. In very broad strokes, the most common aerobic pathogens can be classified as gram positive or gram negative (based on cellular wall staining) [16]. In addition, the role of anaerobic species in wound infection is becoming increasingly recognized [17]. These fastidious species present challenges in their culture and inoculation due to sensitivity to atmospheric oxygen, but due to their role in chronic wounds and multi-pathogen infection, infected animal models are more frequently incorporating anaerobic species [18]. Out of these three general classes (gram positive, gram negative, and anaerobic), the specific organism is chosen based on prevalence in human disease. For example, bone infection (osteomyelitis) in humans is most often caused by Staphylococcus aureus [2]. Therefore, the majority of established animal models of infected bone defects involve S. aureus as the primary pathogen. For infected tissue defects in which there is no clear most prevalent pathogen, multiple groups with different organisms are often utilized, such as a representative gram positive, gram negative, and anaerobic microbe [15, 19].
In addition to species, the pathogen strain chosen can have a significant impact on the animal model. While strains can be obtained locally from clinical isolates, it is recommended that they are purchased from a commercial source such as the American Tissue Culture Collection (ATCC) for standardization. Many commercially-offered strains have information available regarding the source of the pathogen. Different strains within the same species demonstrate different virulence factors, antibacterial resistance patterns, and rates of biofilm production [20]. Biofilm, the extracellular matrix produced by microbes, inhibits the local immune response [21] and increases antibiotic resistance [22]. As many foreign body infections are caused by biofilm-producing pathogens [23], tissue engineering strategies which incorporate cell scaffolds may be particularly vulnerable to biofilm-associated infection. As new therapies specific to biofilm-associated infections are being developed [3], animal models of infected tissue defects with emphasis on biofilm formation have been established and continue to be improved [24–27].
Regarding the inoculum, the concentration of pathogens and delivery vehicle must be considered in selecting or designing an animal model. If establishing a new model or a new pathogen within an existing model, often the optimal concentration must be evaluated in a pilot study where pathogen concentrations are increased logarithmically [28, 29]. In most defects relevant to tissue engineering, a sublethal infection is desired. Therefore, a concentration must be high enough to generate a self-sustaining infection but low enough so that the infection is localized and does not result in systemic disease or sepsis. While inoculum is most frequently delivered by injection of media into the wound, delivering bacteria in a physical vehicle increases virulence. Vehicles in the literature include a pathogen-seeded collagen sponge [28], infected dextran beads [30], or a pre-formed biofilm [24, 31]. While hematogenous bacterial seeding of implanted materials has been attempted, this approach was unsuccessful in a rat model [32].
While the majority of animal models of infected tissue defects challenge wounds with one pathogen species at a time, human chronic wounds such as diabetic ulcers most frequently feature polymicrobial communities [18, 33]. In addition, multiple species have been demonstrated to show synergistic effects and alter bacterial phenotype in animal wound models [34]. Efforts continue to develop animal models of infection with polymicrobial populations that remain stable over time [31].
2.3 Infection Evaluation
A critical consideration in designing or choosing an infected animal model to gauge a tissue engineering strategy is the method by which the infection and healing are evaluated. For the sake of discussion, these methods have been divided into three categories: clinical signs, terminal analysis, and real-time analysis. The most basic method of evaluating infection progression is observing clinical signs of infection (such as wound exudate, weight loss, and survival time). While these markers are valuable and should be noted when displayed, they are often observed under severe disease conditions which may not reflect the sublethal, localized infections in which tissue engineering strategies may be useful. In addition, in infections of deep tissues such as osteomyelitis, it may be impossible to observe any signs of local disease progression.
The next method of evaluation is analysis of infection at a terminal time point at time of euthanasia. This can be performed by techniques such as counting colony-forming units (CFUs) within the infected tissue, histologic staining, and quantitative polymerase chain reaction (qPCR) detection of bacterial DNA. For CFU counting, the infected tissue is harvested and microorganisms are removed (often by homogenization or sonication) into media and plated after serial dilution [35]. This gives an estimate of the quantitative concentration of bacteria in the wound at the time of euthanasia. While inexpensive and frequently utilized, the CFU counting technique is user dependent and known to be variable [35, 36]. Histologic staining of defect tissue is another technique that can be performed after euthanasia. While staining can indicate presence or absence of bacteria in response to a therapy, it is difficult to accurately quantitate these histological results. After excision and sonication of infected tissue, DNA can be removed and purified for qPCR using pathogen-specific primers. The results can be normalized to host animal DNA to compare across groups for a quantitative marker of bacterial presence [25, 37]. By using primers unique to different pathogenic species, qPCR can quantitate the ratios of different bacteria in relation to one another in polymicrobial infections [31]. A weakness of all of the terminal analysis techniques is inability to track infection over time in individual animals and necessity of additional groups at each time point to evaluate the course of disease.
To minimize number of animals needed and gain the capability of tracking infection in an individual animal over time, techniques to monitor disease over real-time have been developed. Perhaps the simplest form of real-time monitoring is a refinement of CFU counting. In the irrigation technique, saline is used to gently wash an infected wound and can then be collected and plated for a bacterial count which can be approximately correlated with infection of the wound [38]. The irrigation technique is limited to infected defects that can be irrigated without surgery (such as infected cutaneous wounds) as well as the previous weaknesses discussed regarding CFU counting. In the cases of animal models of osteomyelitis, radiographic techniques such as x-ray systems and microcomputed tomography can be used to track disease progression in real-time [25]. However, the most broadly impactful development in real-time monitoring of infection in animal models is bioluminescent bacteria. By infecting wounds with these bioluminescent strains, in vivo imaging can be used to quantify luminescence and correlate it with bacterial load. Depending on the strain, this can be done successfully in cutaneous wounds [39], subcutaneous wounds [40], deep soft tissue wounds [41], and even orthopedic defects [25, 42].
2.4 Summary of Considerations
A summary of several factors that should be taken into consideration when selecting an infected animal model to evaluate tissue engineering strategies is presented in Table 1. These are not meant to be a complete list, but a guide when beginning to design a study with infected animal models. To demonstrate how some of these factors have been implemented in the literature, the remainder of this review will explore infected animal models using cutaneous, fascial, and orthopedic defects as examples. Because ethical, regulatory, financial, and translational considerations are often dominant drivers in choosing a particular animal model, the infection models presented here are arranged by species.
Table 1.
Summary of several key considerations in choosing or developing infected animal models for evaluation of tissue engineering-based strategies
| Considerations for Infected Models in Tissue Engineering | |
|---|---|
| Host Animal | |
| Size | |
| Strain | |
| Species | |
| Defect | |
| Size | |
| Anatomical location | |
| Accompanying systemic metabolic/immunologic deficiencies | |
| Inoculum | |
| Species | |
| Strain | |
| Concentration | |
| Vehicle | |
| Evaluation | |
| Clinical signs | |
| Terminal analyses (CFU counting, histology) | |
| Real-time analyses (irrigation, radiography, bioluminescent imaging) | |
3.0 Infected Cutaneous Defects
The skin is often viewed as the first line of defense against a hostile environment. Therefore, it is unsurprising that damage to the skin frequently results in infection. While these infections are trivial in a healthy host, local or systemic immune suppression can result in significant morbidity and even lead to lethality. Acute infected skin defects relevant to tissue engineering include burns, trauma, and infection of surgical sites. Chronic infected skin defects include diabetic ulcers- these ulcers occur in up to 25% of diabetic patients (22.3 million Americans were estimated to have diabetes as of 2012) and become frequently infected, greatly increasing treatment costs and patient morbidity [43–45]. Based on these disease states, there has been great interest within the tissue engineering community to create strategies to regenerate cutaneous wounds [46]. In addition to modeling human disease, infected cutaneous wound models are useful due to their ease of surgery (compared to internal tissues) and often used to test new antimicrobial biomaterials and strategies. In addition, due to their easy access, infected cutaneous wounds are have been used to visualize response of infection to therapeutics in real-time [39] as well as evaluate the efficacy of photodynamic treatments that may not otherwise penetrate to deep layers [40].
Infected cutaneous defects range in severity from superficial infections of the epidermis [47] to full thickness wounds that can result in lethality under the correct conditions (such as high inoculum concentration) [29, 48]. A wide variety of pathogens have been studied in cutaneous wounds, including gram positives and negatives, anaerobes and polymicrobial infections [31, 34], and even fungi [49]. While dozens of papers have been published with different models, several variations commonly occurring in the literature will be discussed.
3.1 Small Animal Models
A plethora of small animals have been used to model infected cutaneous defects, including mice, rats, guinea pigs, and rabbits. While mice and rats are the most common species selected, there is some controversy surrounding the differences in human and rodent cutaneous healing. Specifically, wound contracture, rather than re-epithelialization or new tissue deposition, dominates the healing process in rodents. Specific models have been developed that inhibit wound contracture by splinting in order to more faithfully recapitulate human healing [50]. However, as wound contracture is delayed in rodents during infection [51], the necessity of splinting in infected models is unclear. One of the earliest infected cutaneous defect models was the infected mouse dorsal burn wound, as established by Stieritz et al. [29]. In this model, approximately 30% of the total body surface area of a mouse was burned by exposure to a flame for 10 s followed by inoculation with Pseudomonas aeruginosa. This procedure was modified by Rumbaugh et al. and others to create a burn wound by use of scalding water (90°C) rather than open flame [52] and also applied to rats [53]. The dorsal cutaneous burn wound models have been used to explore pathogen quorum sensing [52], bacterial migration and development of sepsis from infected burn wounds [29], and different therapies [54–56]. Infected surgical excision sites have also been widely explored in small animal models (infected incisional models are not as relevant to tissue engineering due to the small size of the defect). These excisions are typically created by a scalpel, surgical scissors, or punch biopsy in the dorsum (and sometimes include splinting to prevent healing by contraction [50]), followed by inoculation. In addition to splinting, Lundberg et al. developed an infected rat model [57] where a sterile chamber with a window was placed over the wound for observation of granulation tissue throughout the course of infection [39]. In certain cases of localized cutaneous infection, multiple excision sites in the dorsum can be created and infected to act as different groups, such as different localized therapy arms [58]. While the majority of infected burn models utilize P. aeruginosa as the pathogen of choice, excisional wound models have explored a wider variety of pathogens including S. aureus [8, 9, 15, 19, 31, 40], P. aeruginosa [15, 19, 31], Escherichia coli [39, 58], Enterococcus faecalis [31], Acinetobacter baumanii [19], Proteus mirabilis [15], Finegoldia magna [31], and Clostridium perfringens [19]. There have also been efforts to emulate the chronic polymicrobial cutaneous wounds observed in diabetic patients with small animal models. For example, the infected excisional cutaneous wound model has also been studied in diabetic mice [8]. Due to the polymicrobial nature of infected diabetic ulcers, a murine model was established that allows for inoculation with up to four species (gram positive, gram negative, and anaerobic) and maintains infection with all species for at least 12 days [31].
3.2 Large Animal Models
There is a relative dearth of large animal models of infected cutaneous wounds currently in the literature. As porcine skin shares many similarities to human skin [59, 60], pigs are the most common large animal model for infected cutaneous wounds. Due to their large size, numerous excisions can be made per animal as either full thickness [13, 61] or partial thickness wounds [26], limiting the total number of animals needed for study. As in the small animal models, pigs can be rendered diabetic and wounds can be fitted with chambers for observation of healing (as well as irrigation CFU counts) [13]. The porcine dorsal excisional model has been utilized to study biofilm production in cutaneous wounds [26], polymicrobial infection [61], different wound dressing therapies [61], and infection progression and healing in diabetic versus metabolically-normal hosts [13].
4.0 Infected Fascial Defects
A hernia develops when a congenital or acquired defect in the internal wall surrounding an organ leads to regions of absence or weakness in the fascia. This defect allows internal organs to protrude through the fascia, causing swelling and discomfort beneath the skin. Though there are many different types of hernias, the most common occur through the abdominal wall and include inguinal, femoral, groin, incisional, and hiatal hernias [62]. Due to factors such as infection and foreign body reaction, hernias have a relatively high reoccurrence rate (46%). As such, there is a clinical need for effective and reliable biomaterials to improve surgical outcomes [63].
Though there is no single gold standard for hernia repair, most surgical techniques today use synthetic mesh held in place by a small number of sutures to repair and reinforce the abdominal wall [64]. Synthetic meshes are effective at reducing infection, pain, and hernia reoccurrence after surgery. The first synthetic meshes commonly used for hernia repair were composed of non-absorbable polymers, including polyester, polypropylene, and polytetrafluoroethylene. In recent years, newer meshes made out of absorbable and/or non-synthetic materials, such as poly(glycolic acid), polyglactin, and porcine dermis, have been developed [65]. However, most meshes still result in at least a 5% postoperative infection rate, which often requires surgical revision. Therefore, the development of infection resistant meshes for hernia repair is becoming increasingly important to the field [66]. Accordingly, animal models have been developed to study hernia mesh infection, giving special consideration to the wide variety of biomaterials that are currently being used in clinical repair. To date, rodents, rabbits, pigs, and primates have all been used as models for investigation of hernia repair [67].
4.1 Small Animal Models
Due to their small size, rodents are most often used to test the capabilities of mesh to prevent infection through subcutaneous pouches, a defect created immediately underneath the skin in which a biomaterial can be incubated. While this model does not reflect repair and is not under mechanical duress, as the mesh is not sutured over a fascial defect, it can reflect infection in an in vivo environment and compare different antimicrobial strategies. For instance, a rat subcutaneous pouch model was utilized to determine the efficacy of coating polypropylene mesh grafts with gold and palladium particles for clearance of Staphylococcus epidermidis infection over 8 days [10]. This model has also been used to compare infection rates between polypropylene monofilament and polypropylene/polyglactin multifilament meshes after inoculating these meshes with S. aureus and examining the amount of bacterial adherence to these meshes after 7 days [68].
Though many studies utilize rodents for subcutaneous mesh incubation, some studies have also examined the properties of mesh when used for hernia repair. For example, a rat ventral hernia repair model compared the infection rates between four different biological grafts. These grafts were inoculated with Green Fluorescent Protein (GFP) labeled S. aureus and evaluated 30 days after ventral hernia repair with fluorescence imaging to determine the amount of bacterial clearance from the grafts [69]. In addition to labeling bacteria with GFP, bacteria expressing bioluminescence have also been utilized in surgical mesh models to monitor in vivo infection in real-time with non-invasive imaging in a mouse model [70].
Though not used as frequently as the rat model, rabbit models have also served as viable options to model mesh repair of hernias. While the subcutaneous pouch model has also been implemented in rabbits (for example, to examine the infection mitigation of gelatin-coated polymer meshes impregnated with antibiotics [71]), rabbits are large enough that more robust models featuring repair of abdominal wall defects have been created. Milburn et al. compared the ability of acellular dermal matrix grafts and synthetic grafts to resist infection for in vitro hernia repair of the ventral central abdominal wall [72]. This study took place over a period of 1 to 3 weeks and examined meshes that were inoculated with S. aureus. Due to the repair method, this study was also able to determine the extent to which acellular dermal matrices could vascularize the site of repair, an important factor in infection clearance [72]. Other studies also examined the ability of meshes to integrate the mesh into the repair site and to minimize foreign body reactions. For example, Greenawalt et al. evaluated adhesion formation, tissue integration, and overall cellular response to an implanted mesh in the cecum wall after 28 days of implantation in a rabbit model [73].
4.3 Large Animal Models
While small animal models have proven useful for evaluating the antimicrobial properties of meshes for use in hernia repair, their ability to model the performance of the material in a surgical setting is limited due to the small size of the animals used. Therefore, further studies have utilized larger animal models to produce more anatomically-accurate platforms for evaluating infection clearance and integration with host tissue.
Porcine models are advantageous because they allow researchers to more accurately measure how various meshes will react in physiologically realistic hernia repair. The study of adhesion formation, a frequent sign of infection, is one way to evaluate the effectiveness of a biomaterial for hernia repair [74]. For example, Duffy et al. utilized a porcine model to examine differences between adhesion and ingrowth in two types of mesh (a collagen-coated polyester mesh and polytetrafluoroethylene-polypropylene composite mesh) during sutureless laparoscopic ventral hernia repair [75]. This laparoscopic procedure would be difficult to perform on a smaller animal. In another porcine laparoscopic repair model, Borrazzo et al. implanted prosthetic meshes coated with a bioresorbable adhesion barrier versus plain polypropylene meshes and polytetrafluoroethylene meshes and compared the meshes after 28 days for evaluation of adhesion formation to the periosteum [76].
While several large animal studies have been done in porcine models, even fewer studies have been done in primate models. Though primates physiologically resemble humans to a great extent, their large cost and time required for upkeep provide a substantial barrier to their use. However, Xu et al. successfully used a primate model (Caribbean vervets) of ventral hernia repair to function as a surrogate for a clinical study to examine the use of human acellullar dermal matrix as a replacement for common synthetic meshes [77]. In this study, defects in adult male monkeys were repaired with acellular dermal matrix and after 10, 20, 35, and 120 days the graft and surrounding tissue were excised and evaluated for healing strength, angiogenesis, cell repopulation and the presence of T- and B-lymphocytes, and macrophages. Additionally, immunohistochemical analysis was performed on the sample to determine cytokine and antibody presence. This study showed promising results for the use of the Caribbean vervet in future studies of the immunologic response of a host to biologic materials [77].
5.0 Infected Orthopedic Defects
Acute and chronic osteomyelitis is a pressing concern within the fields of orthopedics and orthopedic biomaterials. Osteomyelitis following trauma or routine joint repair surgery has devastating consequences, including weeks to months of potentially toxic systemic antibiotic therapy, repeat surgeries for debridement or removal of hardware, and in severe cases, amputation. Bone injuries are particularly susceptible to infection because they often require implantation of fixation hardware that can act as a substrate for bacteria to adhere and proliferate upon. Research in the orthopedic biomaterials field has sought to improve the treatment of musculoskeletal infections through the use of local delivery applications, and many models that have been developed are particularly well suited toward the evaluation of biomaterials designed to simultaneously treat infections and stimulate bone regeneration. Stringent and clinically relevant animal models are necessary to evaluate biological responses to infection, the efficacy of experimental treatments, and functional repair of infected defects. The majority of animal models of osteomyelitis are infected with S. aureus since the most common cause of long bone infection following trauma and surgical implantation of hardware [2, 78, 79]. Coagulase-negative S. aureus, P. aeruginosa, and methicillin-resistant S. aureus are also implicated in osteomyelitis [2, 78], though there are only a few models that address these organisms.
5.1 Small Animal Models
One of the most common mouse models of infection is for S. aureus post-arthroplasty infection. Bernthal et al. established a S. aureus infection in the knee joint by inserting 0.6 mm Kirschner into the femoral intramedullary canal with 1 mm left protruding into the joint space and pipetting the inoculum into the joint space [80]. Both Bernthal et al. and Pribaz et al. performed this post-arthroplasty S. aureus infection model with LysEGFP mice, which are genetically engineered to express green fluorescent myeloid cells, to evaluate the degree of inflammation present in infected knee joints [80, 81]. Pribaz et al. found that, of four luminescent bacterial strains tested, Xen36 induced the least amount of inflammation [81]. In addition, Xen29 and Xen36 had a shorter duration of inflammation at 14 days compared to Xen40 and ALC2906 at 21 days. Niska et al. have further characterized how this post-arthroplasty infection model using LysEGFP mice can facilitate longitudinally monitoring through bioluminescent imaging for S. aureus Xen29, fluorescence imaging for neutrophils, and radiographic and histologic assessment [82]. Furthermore, by combining the data obtained through all imaging modalities, the effects of inflammation and infection on the development of osteolytic lesions could be evaluated.
Rat models of osteomyelitis are extremely well described in the literature. Like mice, rats are extremely cost-effective, and since rat models have also been extensively characterized, historical controls and many modifications of the various types of rat models exist. The infected rat segmental femoral defect is one of the most common models used to evaluate the efficacy of systemic and local antibiotic delivery vehicles, as well as regenerative strategies in the presence of infection. A key advantage of the rat femoral defect is that extensive model development has established that the inoculating dose needed to produce a S. aureus infection in the presence of hardware is as low as 102 CFU, though many studies use 105 CFU for stringent evaluation of treatment methods [28, 83–85]. Brown et al. demonstrated that early debridement in conjunction with local delivery of antibiotics via poly(methylmethacrylate) beads was more effective in reducing S. aureus bacterial counts than debridement alone after 2 weeks [84]. The efficacy of local antibiotic delivery from a variety of non-degradable and degradable polymer vehicles including PMMA [86] and polyurethane [87] have been evaluated in the rat femoral defect. Sanchez et al. investigated the use of biofilm dispersal agents against a variety of S. aureus strains in a contaminated rat femoral defect, finding that D-amino acids may potentially aid in the reduction of infection by dispersing biofilms on implanted biomaterials [85]. Chen et al. performed a study to evaluate bone regeneration induced by osteopontin-1 in a S. aureus-contaminated rat femoral defect without antibiotic treatment, and found that osteopontin was able to facilitate significantly more bone regeneration even without direct treatment of the infection or the presence of a bone scaffold [88]. More recent efforts have attempted to promote the regeneration of infected defects by concomitantly delivering an osteoinductive drug and an antibiotic. Guelcher et al. delivered BMP-2 with vancomycin from an injectable polyurethane scaffold in a S. aureus infected femoral defect, which resulted in significantly greater bone formation than delivery of BMP-2 alone [89].
The infected rat tibial defect model is another popular infection model with a variety of methods of defect creation and induction of infection. The creation of this defect is simple: exposure of the tibia, creation of a hole in the bone to expose the marrow, injection of bacteria into the marrow, and sealing of the hole with bone wax [90, 91]. Sclerosing agents can be used to facilitate infection, but are not widely used in the literature. While the bone wax can serve as a foreign body to facilitate the infection, often other foreign bodies such as Kirschner wires are deliberately implanted in order to mimic the fixation hardware used clinically. The tibial defect model can be used to evaluate therapeutic strategies. Lucke et al. demonstrated that local delivery of gentamicin from implanted polymer-coated Kirschner wires reduced the bacterial load in S. aureus-infected tibiae [92]. There are few rat osteomyelitis models that do not use S. aureus as the infecting organism, so Nelson et al. has expanded the infected tibial defect model to include infection with P. aeruginosa, a less common but also virulent and difficult to eradicate organism [93].
Rabbit models of long bone osteomyelitis can be more varied due to their larger size, and studies have been published using different long bone sites and different infecting organisms [94–96]. Building upon a preliminary report of acute rabbit tibial osteomyelitis by Scheman et al. in 1941 [97], Norden et al. described the development of a chronic rabbit tibial osteomyelitis model using a clinical isolate of S. aureus in conjunction with a sclerosing agent [98]. Using two strains of S. aureus and one strain of P. mirabilis, Norden et al. showed that 1) the use of a sclerosing agent facilitated the establishment of infection, 2) the clinical isolate S. aureus SMH was able to establish clinical infection while S. aureus 209P was not able to, and 3) P. mirabilis can establish an osteomyelitis in the rabbit tibia, though with less frequency than S. aureus SMH [98]. Andriole et al. further developed the chronic osteomyelitis model by introducing stain steel pins into the defect, mimicking the presence of fixation hardware [99]. Since then, tibial models of osteomyelitis have been widely used to evaluate treatment with various treatment modalities [79]. In addition to the tibial defect model, radial defect models have also been developed [95]. Ambrose et al. used a S. aureus-infected radial defect model to test tobramycin-releasing poly(lactic-co-glycolic acid) microparticles and showed that the infection rate decreased from 64% in rabbits with control implants to 0% in rabbits with tobramycin microparticles [100].
While models of S. aureus osteomyelitis dominate the literature, there is a wider variety of infecting organisms in rabbit models than in murine models. Norden et al. published a model of P. aeruginosa osteomyelitis in the rabbit tibia in which 91–94% of rabbits have positive cultures after 70 days without treatment [94, 101]. The authors found that combination therapy with sisomicin and carbenicillin for 4 weeks is more effective at treating P. aeruginosa tibial osteomyelitis in the rabbit than either drug alone [94]. In a subsequent study using the same model, they show that the use of ciprofloxacin is more effective than tobramycin for the treatment of osteomyelitis caused by P. aeruginosa [101]. Xie et al. have also described a model in which tibial defects are infected with E. coli and showed that gentamicin-loaded borate bioactive glass improved bone regeneration compared to gentamicin with pure bioactive glass and bioactive glass with no gentamicin [102].
5.3 Large Animal Models
Large animal models are desirable because it is possible to more closely replicate the size of clinical defects and implanted materials in goat and sheep models. However, model development is relatively limited because of the increased cost associated with large animals, and some published models have too low a sample size to make definitive conclusions [103]. In addition, there are relatively few goat and sheep osteomyelitis studies in the literature compared to lower order species, so it can be difficult to find an established infection model that has shown success with multiple investigators.
Goats have been used to evaluate experimental treatments in variety of locations, with and without associated orthopedic hardware. Voos et al. implanted pins into the iliac crests of goats in order to investigate whether tobramycin-loaded PMMA pin sleeves could prevent pin-tract infection by S. aureus on a short time scale of 16 days [104]. Another series of goat studies utilized a unicortical 12-mm circular tibial defect infected with S. aureus [105, 106]. Both Thomas et al. and Beardmore et al. performed infected non-treated control groups in order to show that an infection could be established [105, 106]. Lalliss et al. developed a complex tibial defect goat model involving the removal of 10 mm of the medial cortex of the tibia, removal of 13–15 g of anterior compartment muscle, and thermal injury to remaining musculature of the anterior compartment [107]. The defects were inoculated with either P. aeuruginosa (lux) or S. aureus (lux) [107].
Sheep long bone osteomyelitis models described in the literature have used a tibial osteotomy [108, 109] or a medial femoral condyle defect [110] inoculated with S. aureus. Control groups in these studies also indicate that it is possible to induce a S. aureus infection in the tibia of sheep, making them an acceptable large animal for osteomyelitis studies.
6.0 Concluding Remarks
The development of reproducible and clinically-relevant infection animal models will continue to be important in the fields of tissue engineering and biomaterials, especially since in vitro assays and computational modeling are unable to realistically account for the complex interactions between pathogen, native tissue, and patient comorbidities. While small animal models of infection have proliferated in the literature, leading to a wealth of information and experience in the evaluation of experimental treatments of infection in mice, rats, and rabbits, there is a distinct lack of well-established large animal models of infection. While small animal models are excellent for preliminary model development, evaluating experimental treatments and investigating underlying mechanisms of infection, large animal models provide more anatomically relevant information for eventual translation into humans. Because of ethical concerns with the number of small animals needed for statistical power and the use of large animal models in research, further development of non-destructive evaluation methods will be critical to expanding the development of animal models for infection research in an ethical and practical manner. The importance of the distinction between biofilm-producing and non-biofilm-producing strains of bacteria has been increasingly recognized, and more recent animal models are adapting to this new paradigm of infection. Finally, as culture techniques and analytical capabilities improve, the role of anaerobic bacteria and polymicrobial infection is becoming more prominent, and future models are likely to expand upon single aerobic organism models to include anaerobes and multiple cultures at a single site. Despite the incredible advances being made in tissue engineering and biomaterials, infection remains one of the most damaging complications. As new strategies are developed to combat infection, animal models of infection will be instrumental in translating therapies to the clinic.
Highlights.
Important considerations for selecting or designing infected animal models to evaluate tissue engineering-based strategies are underscored
Established models of infection for cutaneous, fascial, and orthopedic defects are reviewed
Areas that require further model development are discussed
Acknowledgments
This work was supported by the Army, Navy, NIH, Air Force, VA and Health Affairs to support the AFIRM II effort, under Award No. W81XWH-14-2-0004. The U.S. Army Medical Research Acquisition Activity, 820 Chandler Street, Fort Detrick MD 21702-5014 is the awarding and administering acquisition office. Opinions, interpretations, conclusions and recommendations are those of the author and are not necessarily endorsed by the Department of Defense. In addition, A.M.T. and S.R.S. would like to thank the Baylor College of Medicine Medical Scientist Training Program (NIH T32 GM007330) and A.M.T. would like to thank the Barrow Scholars Program.
Abbreviations
- ATCC
American Tissue Culture Collection
- BMP-2
Bone morphogenetic protein 2
- CFU
Colony-forming unit
- qPCR
Quantitative polymerase chain reaction
Footnotes
There are no conflicts of interest to report in this work.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
8.0 References
- 1.Martin P, Leibovich SJ. Trends Cell Biol. 2005;15:599–607. doi: 10.1016/j.tcb.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 2.Darouiche RO. N Engl J Med. 2004;350:1422–1429. doi: 10.1056/NEJMra035415. [DOI] [PubMed] [Google Scholar]
- 3.Shah SR, Tatara AM, D’Souza RN, Mikos AG, Kasper FK. Materials Today. 2013;16:177–182. [Google Scholar]
- 4.Carter TG, Brar PS, Tolas A, Beirne OR. J Oral Maxillofac Surg. 2008;66:1417–1425. doi: 10.1016/j.joms.2008.01.058. [DOI] [PubMed] [Google Scholar]
- 5.Lee MH, Arcidiacono JA, Bilek AM, Wille JJ, Hamill CA, Wonnacott KM, Wells MA, Oh SS. Tissue Eng Part B Rev. 2009;16:41–54. doi: 10.1089/ten.TEB.2009.0449. [DOI] [PubMed] [Google Scholar]
- 6.Sellers RS, Clifford CB, Treuting PM, Brayton C. Vet Pathol. 2012;49:32–43. doi: 10.1177/0300985811429314. [DOI] [PubMed] [Google Scholar]
- 7.McLoughlin RM, Solinga RM, Rich J, Zaleski KJ, Cocchiaro JL, Risley A, Tzianabos AO, Lee JC. Proc Natl Acad Sci U S A. 2006;103:10408–10413. doi: 10.1073/pnas.0508961103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shi CM, Nakao H, Yamazaki M, Tsuboi R, Ogawa H. Arch Dermatol Res. 2007;299:449–456. doi: 10.1007/s00403-007-0776-3. [DOI] [PubMed] [Google Scholar]
- 9.Kim MH, Liu W, Borjesson DL, Curry FR, Miller LS, Cheung AL, Liu FT, Isseroff RR, Simon SI. J Invest Dermatol. 2008;128:1812–1820. doi: 10.1038/sj.jid.5701223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Saygun O, Agalar C, Aydinuraz K, Agalar F, Daphan C, Saygun M, Ceken S, Akkus A, Denkbas EB. J Surg Res. 2006;131:73–79. doi: 10.1016/j.jss.2005.06.020. [DOI] [PubMed] [Google Scholar]
- 11.Hollister SJ, Murphy WL. Tissue Eng Part B Rev. 2011;17:459–474. doi: 10.1089/ten.teb.2011.0251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stratford AF, Zoutman DE, Davidson JS. Plast Reconstr Surg. 2002;110:1275–1279. doi: 10.1097/01.PRS.0000025427.86301.8A. [DOI] [PubMed] [Google Scholar]
- 13.Hirsch T, Spielmann M, Zuhaili B, Koehler T, Fossum M, Steinau HU, Yao F, Steinstraesser L, Onderdonk AB, Eriksson E. BMC Surg. 2008;8:5. doi: 10.1186/1471-2482-8-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lin L, Ibrahim AS, Xu X, Farber JM, Avanesian V, Baquir B, Fu Y, French SW, Edwards JE, Jr, Spellberg B. PLoS Pathog. 2009;5:e1000703. doi: 10.1371/journal.ppat.1000703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Burkatovskaya M, Tegos GP, Swietlik E, Demidova TN, PCA, Hamblin MR. Biomaterials. 2006;27:4157–4164. doi: 10.1016/j.biomaterials.2006.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Madison BM. Biotech Histochem. 2001;76:119–125. [PubMed] [Google Scholar]
- 17.Dowd SE, Sun Y, Secor PR, Rhoads DD, Wolcott BM, James GA, Wolcott RD. BMC Microbiol. 2008;8:43. doi: 10.1186/1471-2180-8-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bertesteanu S, Triaridis S, Stankovic M, Lazar V, Chifiriuc MC, Vlad M, Grigore R. Int J Pharm. 2014;463:119–126. doi: 10.1016/j.ijpharm.2013.12.012. [DOI] [PubMed] [Google Scholar]
- 19.Yates CC, Whaley D, Babu R, Zhang J, Krishna P, Beckman E, Pasculle AW, Wells A. Biomaterials. 2007;28:3977–3986. doi: 10.1016/j.biomaterials.2007.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gill SR, Fouts DE, Archer GL, Mongodin EF, Deboy RT, Ravel J, Paulsen IT, Kolonay JF, Brinkac L, Beanan M, Dodson RJ, Daugherty SC, Madupu R, Angiuoli SV, Durkin AS, Haft DH, Vamathevan J, Khouri H, Utterback T, Lee C, Dimitrov G, Jiang L, Qin H, Weidman J, Tran K, Kang K, Hance IR, Nelson KE, Fraser CM. J Bacteriol. 2005;187:2426–2438. doi: 10.1128/JB.187.7.2426-2438.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Parsek MR, Singh PK. Annu Rev Microbiol. 2003;57:677–701. doi: 10.1146/annurev.micro.57.030502.090720. [DOI] [PubMed] [Google Scholar]
- 22.Amorena B, Gracia E, Monzon M, Leiva J, Oteiza C, Perez M, Alabart JL, Hernandez-Yago J. J Antimicrob Chemother. 1999;44:43–55. doi: 10.1093/jac/44.1.43. [DOI] [PubMed] [Google Scholar]
- 23.Costerton JW, Montanaro L, Arciola CR. Int J Artif Organs. 2005;28:1062–1068. doi: 10.1177/039139880502801103. [DOI] [PubMed] [Google Scholar]
- 24.Schierle CF, De la Garza M, Mustoe TA, Galiano RD. Wound Repair Regen. 2009;17:354–359. doi: 10.1111/j.1524-475X.2009.00489.x. [DOI] [PubMed] [Google Scholar]
- 25.Li D, Gromov K, Soballe K, Puzas JE, O’Keefe RJ, Awad H, Drissi H, Schwarz EM. J Orthop Res. 2008;26:96–105. doi: 10.1002/jor.20452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Davis SC, Ricotti C, Cazzaniga A, Welsh E, Eaglstein WH, Mertz PM. Wound Repair Regen. 2008;16:23–29. doi: 10.1111/j.1524-475X.2007.00303.x. [DOI] [PubMed] [Google Scholar]
- 27.Schaber JA, Triffo WJ, Suh SJ, Oliver JW, Hastert MC, Griswold JA, Auer M, Hamood AN, Rumbaugh KP. Infect Immun. 2007;75:3715–3721. doi: 10.1128/IAI.00586-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen X, Tsukayama DT, Kidder LS, Bourgeault CA, Schmidt AH, Lew WD. J Orthop Res. 2005;23:816–823. doi: 10.1016/j.orthres.2005.01.009. [DOI] [PubMed] [Google Scholar]
- 29.Stieritz DD, Holder IA. J Infect Dis. 1975;131:688–691. doi: 10.1093/infdis/131.6.688. [DOI] [PubMed] [Google Scholar]
- 30.Bunce C, Wheeler L, Reed G, Musser J, Barg N. Infect Immun. 1992;60:2636–2640. doi: 10.1128/iai.60.7.2636-2640.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dalton T, Dowd SE, Wolcott RD, Sun Y, Watters C, Griswold JA, Rumbaugh KP. PLoS One. 2011;6:e27317. doi: 10.1371/journal.pone.0027317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gottenbos B, Klatter F, Van Der Mei HC, Busscher HJ, Nieuwenhuis P. Clin Diagn Lab Immunol. 2001;8:980–983. doi: 10.1128/CDLI.8.5.980-983.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dowd SE, Wolcott RD, Sun Y, McKeehan T, Smith E, Rhoads D. PLoS One. 2008;3:e3326. doi: 10.1371/journal.pone.0003326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kelly MJ. Ann R Coll Surg Engl. 1980;62:52–59. [PMC free article] [PubMed] [Google Scholar]
- 35.Sutton S. Journal of validation technology. 2011;3:42–46. [Google Scholar]
- 36.Niederman MS. Clin Infect Dis. 2010;51(Suppl 1):S93–99. doi: 10.1086/653055. [DOI] [PubMed] [Google Scholar]
- 37.Hein I, Lehner A, Rieck P, Klein K, Brandl E, Wagner M. Appl Environ Microbiol. 2001;67:3122–3126. doi: 10.1128/AEM.67.7.3122-3126.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Saymen DG, Nathan P, Holder IA, Hill EO, Macmillan BG. Appl Microbiol. 1972;23:509–514. doi: 10.1128/am.23.3.509-514.1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jawhara S, Mordon S. Antimicrob Agents Chemother. 2004;48:3436–3441. doi: 10.1128/AAC.48.9.3436-3441.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gad F, Zahra T, Francis KP, Hasan T, Hamblin MR. Photochem Photobiol Sci. 2004;3:451–458. doi: 10.1039/b311901g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kuklin NA, Pancari GD, Tobery TW, Cope L, Jackson J, Gill C, Overbye K, Francis KP, Yu J, Montgomery D, Anderson AS, McClements W, Jansen KU. Antimicrob Agents Chemother. 2003;47:2740–2748. doi: 10.1128/AAC.47.9.2740-2748.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Funao H, Ishii K, Nagai S, Sasaki A, Hoshikawa T, Aizawa M, Okada Y, Chiba K, Koyasu S, Toyama Y, Matsumoto M. Infect Immun. 2012;80:733–741. doi: 10.1128/IAI.06166-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Singh N, Armstrong DG, Lipsky BA. JAMA. 2005;293:217–228. doi: 10.1001/jama.293.2.217. [DOI] [PubMed] [Google Scholar]
- 44.Association AD. Diabetes Care. 2013;36:1033–1046. [Google Scholar]
- 45.Prompers L, Huijberts M, Schaper N, Apelqvist J, Bakker K, Edmonds M, Holstein P, Jude E, Jirkovska A, Mauricio D, Piaggesi A, Reike H, Spraul M, Van Acker K, Van Baal S, Van Merode F, Uccioli L, Urbancic V, Tennvall G Ragnarson. Diabetologia. 2008;51:1826–1834. doi: 10.1007/s00125-008-1089-6. [DOI] [PubMed] [Google Scholar]
- 46.Clark RA, Ghosh K, Tonnesen MG. J Invest Dermatol. 2007;127:1018–1029. doi: 10.1038/sj.jid.5700715. [DOI] [PubMed] [Google Scholar]
- 47.Kugelberg E, Norstrom T, Petersen TK, Duvold T, Andersson DI, Hughes D. Antimicrob Agents Chemother. 2005;49:3435–3441. doi: 10.1128/AAC.49.8.3435-3441.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hamblin MR, Zahra T, Contag CH, McManus AT, Hasan T. J Infect Dis. 2003;187:1717–1725. doi: 10.1086/375244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ben-Ami R, Kontoyiannis DP. Methods Mol Biol. 2012;845:569–582. doi: 10.1007/978-1-61779-539-8_42. [DOI] [PubMed] [Google Scholar]
- 50.Galiano RD, Michaels Jt, Dobryansky M, Levine JP, Gurtner GC. Wound Repair Regen. 2004;12:485–492. doi: 10.1111/j.1067-1927.2004.12404.x. [DOI] [PubMed] [Google Scholar]
- 51.Robson M, Kucukcelebi A, Carp SS, Hayward PG, Hui PS, Cowan WT, Ko F, Cooper DM. Eur J Clin Microbiol Infect Dis. 1994;13(Suppl 2):S41–46. doi: 10.1007/BF01973601. [DOI] [PubMed] [Google Scholar]
- 52.Rumbaugh KP, Griswold JA, Iglewski BH, Hamood AN. Infect Immun. 1999;67:5854–5862. doi: 10.1128/iai.67.11.5854-5862.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yalcin O, Soybir G, Koksoy F, Kose H, Ozturk R, Cokneseli B. Surg Today. 1997;27:154–158. doi: 10.1007/BF02385906. [DOI] [PubMed] [Google Scholar]
- 54.Nakae H, Inaba H. J Trauma. 2000;49:511–514. doi: 10.1097/00005373-200009000-00020. [DOI] [PubMed] [Google Scholar]
- 55.Toklu HZ, Sener G, Jahovic N, Uslu B, Arbak S, Yegen BC. Int Immunopharmacol. 2006;6:156–169. doi: 10.1016/j.intimp.2005.07.016. [DOI] [PubMed] [Google Scholar]
- 56.Huang Q, Shao L, He M, Chen H, Liu D, Luo Y, Dai Y. Burns. 2005;31:637–642. doi: 10.1016/j.burns.2005.02.006. [DOI] [PubMed] [Google Scholar]
- 57.Lundberg C, Campbell D, Agerup B, Ulfendahl H. Scand J Plast Reconstr Surg. 1982;16:123–131. doi: 10.3109/02844318209006580. [DOI] [PubMed] [Google Scholar]
- 58.Hamblin MR, O’Donnell DA, Murthy N, Contag CH, Hasan T. Photochem Photobiol. 2002;75:51–57. doi: 10.1562/0031-8655(2002)075<0051:rcowib>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 59.Middelkoop E, van den Bogaerdt AJ, Lamme EN, Hoekstra MJ, Brandsma K, Ulrich MM. Biomaterials. 2004;25:1559–1567. doi: 10.1016/s0142-9612(03)00502-7. [DOI] [PubMed] [Google Scholar]
- 60.Sullivan TP, Eaglstein WH, Davis SC, Mertz P. Wound Repair Regen. 2001;9:66–76. doi: 10.1046/j.1524-475x.2001.00066.x. [DOI] [PubMed] [Google Scholar]
- 61.Wright JB, Lam K, Buret AG, Olson ME, Burrell RE. Wound Repair Regen. 2002;10:141–151. doi: 10.1046/j.1524-475x.2002.10308.x. [DOI] [PubMed] [Google Scholar]
- 62.Millikan KW, Deziel DJ. Surg Clin North Am. 1996;76:105–116. doi: 10.1016/s0039-6109(05)70425-4. [DOI] [PubMed] [Google Scholar]
- 63.Dabbas N, Adams K, Pearson K, Royle G. JRSM Short Rep. 2011;2:5. doi: 10.1258/shorts.2010.010071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Brown CN, Finch JG. Ann R Coll Surg Engl. 2010;92:272–278. doi: 10.1308/003588410X12664192076296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Falagas ME, Kasiakou SK. Clin Microbiol Infect. 2005;11:3–8. doi: 10.1111/j.1469-0691.2004.01014.x. [DOI] [PubMed] [Google Scholar]
- 66.Daghighi S, Sjollema J, van der Mei HC, Busscher HJ, Rochford ET. Biomaterials. 2013;34:8013–8017. doi: 10.1016/j.biomaterials.2013.07.044. [DOI] [PubMed] [Google Scholar]
- 67.Bringman S, Conze J, Cuccurullo D, Deprest J, Junge K, Klosterhalfen B, Parra-Davila E, Ramshaw B, Schumpelick V. Hernia. 2010;14:81–87. doi: 10.1007/s10029-009-0587-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Klinge U, Junge K, Spellerberg B, Piroth C, Klosterhalfen B, Schumpelick V. J Biomed Mater Res. 2002;63:765–771. doi: 10.1002/jbm.10449. [DOI] [PubMed] [Google Scholar]
- 69.Harth KC, Broome AM, Jacobs MR, Blatnik JA, Zeinali F, Bajaksouzian S, Rosen MJ. Surg Endosc. 2011;25:2224–2229. doi: 10.1007/s00464-010-1534-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Engelsman AF, van der Mei HC, Francis KP, Busscher HJ, Ploeg RJ, van Dam GM. J Biomed Mater Res B Appl Biomater. 2009;88:123–129. doi: 10.1002/jbm.b.31158. [DOI] [PubMed] [Google Scholar]
- 71.Goeau-Brissonniere O, Leflon V, Letort M, Nicolas MH. Biomaterials. 1999;20:229–232. doi: 10.1016/s0142-9612(98)00164-1. [DOI] [PubMed] [Google Scholar]
- 72.Milburn ML, Holton LH, Chung TL, Li EN, Bochicchio GV, Goldberg NH, Silverman RP. Surg Infect (Larchmt) 2008;9:433–442. doi: 10.1089/sur.2007.044. [DOI] [PubMed] [Google Scholar]
- 73.Greenawalt KE, Butler TJ, Rowe EA, Finneral AC, Garlick DS, Burns JW. J Surg Res. 2000;94:92–98. doi: 10.1006/jsre.2000.6020. [DOI] [PubMed] [Google Scholar]
- 74.Rodgers KE. Sepsis. 1999;3:317–325. [Google Scholar]
- 75.Duffy AJ, Hogle NJ, LaPerle KM, Fowler DL. Hernia. 2004;8:358–364. doi: 10.1007/s10029-004-0258-x. [DOI] [PubMed] [Google Scholar]
- 76.Borrazzo EC, Belmont MF, Boffa D, Fowler DL. Hernia. 2004;8:108–112. doi: 10.1007/s10029-003-0181-6. [DOI] [PubMed] [Google Scholar]
- 77.Xu H, Wan H, Sandor M, Qi S, Ervin F, Harper JR, Silverman RP, McQuillan DJ. Tissue Eng Part A. 2008;14:2009–2019. doi: 10.1089/ten.tea.2007.0316. [DOI] [PubMed] [Google Scholar]
- 78.Calhoun JH, Manring MM, Shirtliff M. Semin Plast Surg. 2009;23:59–72. doi: 10.1055/s-0029-1214158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Reizner W, Hunter JG, O’Malley NT, Southgate RD, Schwarz EM, Kates SL. Eur Cell Mater. 2014;27:196–212. doi: 10.22203/ecm.v027a15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bernthal NM, Stavrakis AI, Billi F, Cho JS, Kremen TJ, Simon SI, Cheung AL, Finerman GA, Lieberman JR, Adams JS, Miller LS. PLoS One. 2010;5:e12580. doi: 10.1371/journal.pone.0012580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Pribaz JR, Bernthal NM, Billi F, Cho JS, Ramos RI, Guo Y, Cheung AL, Francis KP, Miller LS. J Orthop Res. 2012;30:335–340. doi: 10.1002/jor.21519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Niska JA, Meganck JA, Pribaz JR, Shahbazian JH, Lim E, Zhang N, Rice BW, Akin A, Ramos RI, Bernthal NM, Francis KP, Miller LS. PLoS One. 2012;7:e47397. doi: 10.1371/journal.pone.0047397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Penn-Barwell JG, Rand BC, Brown KV, Wenke JC. Bone Joint Res. 2014;3:187–192. doi: 10.1302/2046-3758.36.2000293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Brown KV, Walker JA, Cortez DS, Murray CK, Wenke JC. J Surg Orthop Adv. 2010;19:18–22. [PubMed] [Google Scholar]
- 85.Sanchez CJ, Jr, Prieto EM, Krueger CA, Zienkiewicz KJ, Romano DR, Ward CL, Akers KS, Guelcher SA, Wenke JC. Biomaterials. 2013;34:7533–7543. doi: 10.1016/j.biomaterials.2013.06.026. [DOI] [PubMed] [Google Scholar]
- 86.Penn-Barwell JG, Murray CK, Wenke JC. J Orthop Trauma. 2014;28:370–375. doi: 10.1097/BOT.0b013e3182a7739e. [DOI] [PubMed] [Google Scholar]
- 87.Li B, Brown KV, Wenke JC, Guelcher SA. J Control Release. 2010;145:221–230. doi: 10.1016/j.jconrel.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 88.Chen X, Kidder LS, Lew WD. J Orthop Res. 2002;20:142–150. doi: 10.1016/S0736-0266(01)00060-2. [DOI] [PubMed] [Google Scholar]
- 89.Guelcher SA, Brown KV, Li B, Guda T, Lee BH, Wenke JC. J Orthop Trauma. 2011;25:477–482. doi: 10.1097/BOT.0b013e31821f624c. [DOI] [PubMed] [Google Scholar]
- 90.Rissing JP, Buxton TB, Weinstein RS, Shockley RK. Infect Immun. 1985;47:581–586. doi: 10.1128/iai.47.3.581-586.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Power ME, Olson ME, Domingue PA, Costerton JW. J Med Microbiol. 1990;33:189–198. doi: 10.1099/00222615-33-3-189. [DOI] [PubMed] [Google Scholar]
- 92.Lucke M, Schmidmaier G, Sadoni S, Wildemann B, Schiller R, Haas NP, Raschke M. Bone. 2003;32:521–531. doi: 10.1016/s8756-3282(03)00050-4. [DOI] [PubMed] [Google Scholar]
- 93.Nelson DR, Buxton TB, Luu QN, Rissing JP. Infection. 1990;18:246–248. doi: 10.1007/BF01643399. [DOI] [PubMed] [Google Scholar]
- 94.Norden CW, Keleti E. J Infect Dis. 1980;141:71–75. doi: 10.1093/infdis/141.1.71. [DOI] [PubMed] [Google Scholar]
- 95.Smeltzer MS, Thomas JR, Hickmon SG, Skinner RA, Nelson CL, Griffith D, Parr TR, Jr, Evans RP. J Orthop Res. 1997;15:414–421. doi: 10.1002/jor.1100150314. [DOI] [PubMed] [Google Scholar]
- 96.Ambrose CG, Clyburn TA, Louden K, Joseph J, Wright J, Gulati P, Gogola GR, Mikos AG. Clin Orthop Relat Res. 2004:293–299. doi: 10.1097/01.blo.0000126303.41711.a2. [DOI] [PubMed] [Google Scholar]
- 97.Scheman L, Janota M, Lewin P. Journal of the American Medical Association. 1941;117:1525–1529. [Google Scholar]
- 98.Norden CW. J Infect Dis. 1970;122:410–418. doi: 10.1093/infdis/122.5.410. [DOI] [PubMed] [Google Scholar]
- 99.Andriole VT, Nagel DA, Southwick WO. Yale J Biol Med. 1974;47:33–39. [PMC free article] [PubMed] [Google Scholar]
- 100.Ambrose CG, Clyburn TA, Mika J, Gogola GR, Kaplan HB, Wanger A, Mikos AG. J Bone Joint Surg Am. 2014;96:128–134. doi: 10.2106/JBJS.L.01750. [DOI] [PubMed] [Google Scholar]
- 101.Norden CW, Shinners E. J Infect Dis. 1985;151:291–294. doi: 10.1093/infdis/151.2.291. [DOI] [PubMed] [Google Scholar]
- 102.Xie Z, Cui X, Zhao C, Huang W, Wang J, Zhang C. Antimicrob Agents Chemother. 2013;57:3293–3298. doi: 10.1128/AAC.00284-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Tran N, Tran PA, Jarrell JD, Engiles JB, Thomas NP, Young MD, Hayda RA, Born CT. Biomed Res Int. 2013;2013:674378. doi: 10.1155/2013/674378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Voos K, Rosenberg B, Fagrhi M, Seligson D. J Orthop Trauma. 1999;13:98–101. doi: 10.1097/00005131-199902000-00005. [DOI] [PubMed] [Google Scholar]
- 105.Thomas DB, Brooks DE, Bice TG, DeJong ES, Lonergan KT, Wenke JC. Clin Orthop Relat Res. 2005;441:366–371. doi: 10.1097/01.blo.0000181144.01306.b0. [DOI] [PubMed] [Google Scholar]
- 106.Beardmore AA, Brooks DE, Wenke JC, Thomas DB. J Bone Joint Surg Am. 2005;87:107–112. doi: 10.2106/JBJS.C.01670. [DOI] [PubMed] [Google Scholar]
- 107.Lalliss SJ, Stinner DJ, Waterman SM, Branstetter JG, Masini BD, Wenke JC. J Orthop Trauma. 2010;24:598–602. doi: 10.1097/BOT.0b013e3181ec45ba. [DOI] [PubMed] [Google Scholar]
- 108.Stewart S, Barr S, Engiles J, Hickok NJ, Shapiro IM, Richardson DW, Parvizi J, Schaer TP. J Bone Joint Surg Am. 2012;94:1406–1415. doi: 10.2106/JBJS.K.00886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Schaer TP, Stewart S, Hsu BB, Klibanov AM. Biomaterials. 2012;33:1245–1254. doi: 10.1016/j.biomaterials.2011.10.038. [DOI] [PubMed] [Google Scholar]
- 110.McLaren JS, White LJ, Cox HC, Ashraf W, Rahman CV, Blunn GW, Goodship AE, Quirk RA, Shakesheff KM, Bayston R, Scammell BE. Eur Cell Mater. 2014;27:332–349. doi: 10.22203/ecm.v027a24. [DOI] [PubMed] [Google Scholar]


