Abstract
The liver is the most frequently injured intraperitoneal organ, despite its relatively protected location. The liver consisting of a relatively fragile parenchyma contained within the Glisson capsule, which is thin and does not provide it with great protection. The management of hepatic trauma has undergone a paradigm shift over the past several decades with significant improvement in outcomes. Shifting from mandatory operation to selective nonoperative treatment, and, presently, to nonoperative treatment with selective operation. Operative management emphasizes packing, damage control, and utilization of interventional radiology, such as angiography and embolization. Because of the high morbidity and mortality, liver resection seems to have a minimal role in the management of hepatic injury in many reports, but in a specialized referral center, like our institute, surgical treatment becomes, in many cases, the only life-saving treatment. Innovations in liver transplant surgery, living liver donation, and the growth of specialized liver surgery teams have changed the way that surgeons and hepatic resection are done.
Keywords: Hepatectomy, laceration of liver, blunt liver trauma, liver fixation
Case presentation
A 23-year-old male arrived to emergency room after being run over by a car. On his arrival, GCS 15, BP 136/90, HR 92, severe RUQ pain with large hematoma on the right chest and abdomen which was distended with localized peritonitis.
FAST—large amount of fluid in the abdominal cavity.
Chest X-ray—no signs of pneumothorax no ribs fractures.
-
Severe liver injury Gr 4, extravasation of contrast material—“Blash”;
Irregularity in the right hepatic vein close to the IVC junction—suspected RT hepatic vein laceration;
Large amount of blood in the abdominal cavity;
Stable fracture of the pelvis.
Figure 1.

CT before surgery—hemoperitoneum with laceration of the liver.
Figure 2.

CT before surgery—suspected tear of the right hepatic vein.
Due to the CT finding and hemodynamically instability with tachycardia above 100 and hypotension, the patient was rushed to the OR for exploratory laparotomy. Angiography with embolization was not done, because in case of severe liver injury with hemodynamically instability the right course of action is an immediate surgery.
Surgical technique
The operative findings were a large central liver laceration with active bleeding which was not controlled by packing alone. A “Pringle” was placed over the hepato-duodenal ligament which decreased the bleeding but did not stop it. A complex hepatic injury involving the liver parenchyma, the right hepatic pedicle and the right hepatic vein was diagnosed. As a result of right pedicle tear, the attempts to release the clamping failed and were accompanied by massive bleedings. Several attempts to control the right pedicle were not successful; we considered putting a caval balloon catheter if the total vascular exclusion (TVE) was not successful. TVE (Figure 3) was performed due to the retroperitoneal bleeding and enabled the displacement of the liver and the assessment of the IVC injury. After excluding the liver, exploration revealed that the liver was torn off from the IVC and the right hepatic vein was disconnected (Figure 4). A formal right hepatectomy was performed without dissection of the pedicle by an anterior approach. Due to bowel edema the abdomen could not be closed primarily and the remaining left lobe of the liver could not be fixed within the abdominal wall, a temporary closure of the abdomen with VAC PAK was done. The patient was transferred to the ICU hemodynamically stable for further resuscitation.
Figure 3.
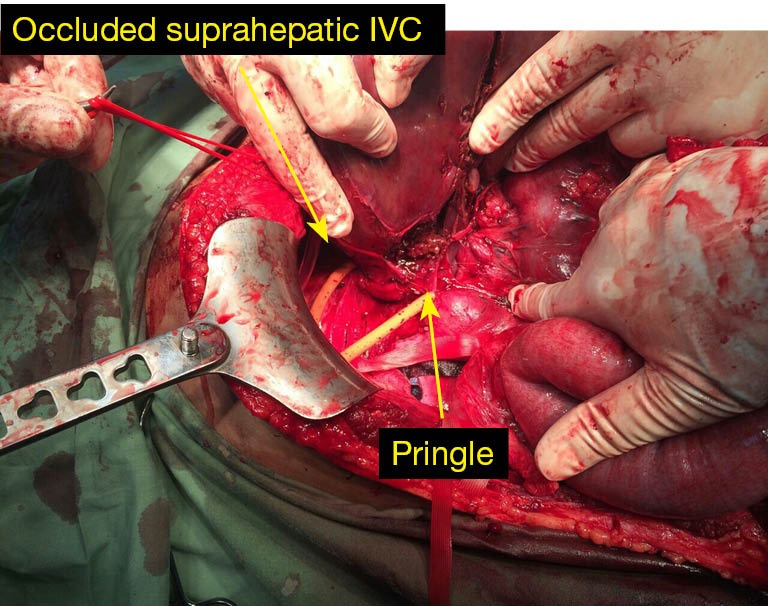
Total vascular exclusion before hepatectomy.
Figure 4.
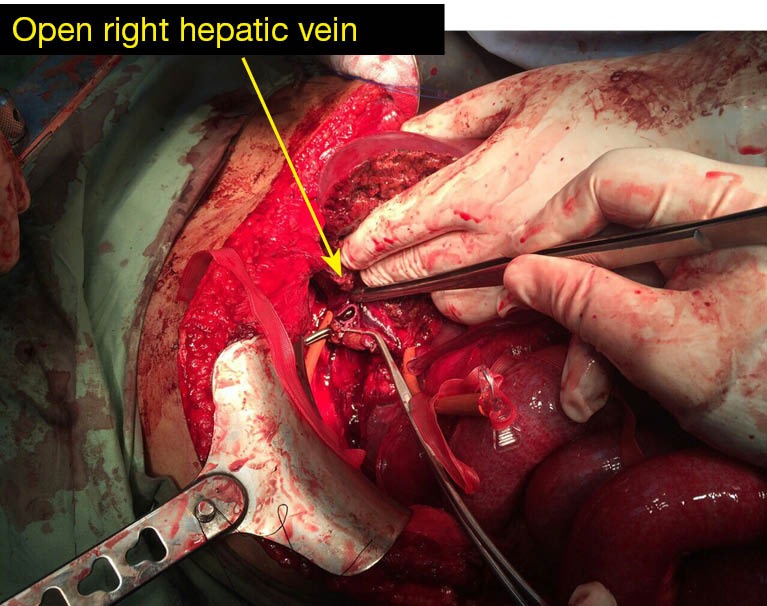
Torn right hepatic vein.
Post-operative course
During the next 2 weeks, the patient was operated three times and had an open abdomen that was kept closed with a VAC PAC.
Immediately after the first operation the patient remained intubated and kept his hemodynamically stability with noradrenaline. A biliary leak was observed and the bowels were less edematous. On post-operative day 6 the abdomen was opened to change the VAC in the ICU, the liver was found twisted to the right and very congested. An intraoperative US showed a severe narrowing of the left and mid hepatic veins with a reduced blood flow, corresponding to a partial Budd Chiari. After putting the liver in its anatomic position the hepatic veins looked normal with a normal flow. Acute Budd-Chiari syndrome (ABCS) after major hepatic resection is rare but potentially lethal (1,2). After extended right hepatectomy, the remnant liver can be affected by outflow obstruction due to torsion of the IVC or kinking of the left hepatic vein (2,3). Fixing left remnant liver in the anatomic position has been demonstrated to improve hepatic vein flow and reduce ABCS incidence after extended right liver resection (4). In addition, the usage of expenders filled with fluids is common in dual liver transplants, which are taken off after a period of time after surgery (5). Under this special circumstance that the left lobe of the liver could not be fixed anatomically due to the open abdomen, an innovative solution was chosen: putting a sterile 500 cc saline bag within the abdominal cavity, keeping the left lobe of the liver in place (Figure 5). In the next 10 days the saline bag was replaced every 3 days in the ICU. The patient was transfer to the trauma unit after 2 weeks in the ICU, he went through a prolonged rehabilitation process and he is recovering from his injuries (Figure 6).
Figure 5.

Saline bag for fixing the liver in place.
Figure 6.

Granulation tissue over the abdomen before skin graft.
The patient was released from the hospital after a month. He is programmed for a reconstruction of the abdominal wall.
Summary
The management of liver trauma underwent a significant shift over the past several decades with an impressive improvement in outcomes. Shifting from mandatory operation to selective non-operative treatment and presently, to non-operative treatment in selected patients (6-8). The non-operative management (NOM) such as angiography with embolization (reserved only for hemodynamically stable patients) or intra-aortic balloon occlusion (IABO) which is useful for proximal vascular control, by clamping the descending aorta, in traumatic haemorrhagic shock (there are limited clinical studies regarding its effectiveness) (9).
We described a unique and innovative treatment for a complicated liver trauma, where the surgeons chose the unconventional trauma treatment due to an uncontrolled massive bleeding of patient.
The operation was executed by a well-experienced hepato-biliary team of surgeons, and took place in a tertiary trauma center. Procedures such as the one described here, have good success rates and low mortality rates when performed by an experienced team. In this case, the experienced and highly skilled team was also forced to exhibit creative thinking and unorthodox measures to save the patient’s live.
Acknowledgements
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Poon RT, Chan J, Fan ST. Left hepatic vein kinking after right trisegmentectomy: a potential cause of postoperative liver failure. Hepatogastroenterology 1998;45:508-9. [PubMed] [Google Scholar]
- 2.Wang JK, Truty MJ, Donohue JH. Remnant torsion causing Budd-Chiari syndrome after right hepatectomy. J Gastrointest Surg 2010;14:910-2. [DOI] [PubMed] [Google Scholar]
- 3.Di Domenico S, Rossini A, Petrocelli F, et al. Recurrent acute Budd-Chiari syndrome after right hepatectomy: US color-Doppler vascular pattern and left hepatic vein stenting for treatment. Abdom Imaging 2013;38:320-3. [DOI] [PubMed] [Google Scholar]
- 4.Ogata S, Kianmanesh R, Belghiti J. Doppler assessment after right hepatectomy confirms the need to fix the remnant left liver in the anatomical position. Br J Surg 2005;92:592-5. [DOI] [PubMed] [Google Scholar]
- 5.Inomata Y, Tanaka K, Egawa H, et al. Application of a tissue expander for stabilizing graft position in living-related liver transplantation. Clin Transplant 1997;11:56-9. [PubMed] [Google Scholar]
- 6.Ochiai T, Igari K, Yagi M, et al. Treatment strategy for blunt hepatic trauma: analysis of 183 consecutive cases. Hepatogastroenterology 2011;58:1312-5. [DOI] [PubMed] [Google Scholar]
- 7.Morrison JJ, Bramley KE, Rizzo AG. Liver trauma--operative management. J R Army Med Corps 2011;157:136-44. [DOI] [PubMed] [Google Scholar]
- 8.Kozar RA, Feliciano DV, Moore EE, et al. Western Trauma Association/critical decisions in trauma: operative management of adult blunt hepatic trauma. J Trauma 2011;71:1-5. [DOI] [PubMed] [Google Scholar]
- 9.Irahara T, Sato N, Moroe Y, et al. Retrospective study of the effectiveness of Intra-Aortic Balloon Occlusion (IABO) for traumatic haemorrhagic shock. World J Emerg Surg 2015;10:1. [DOI] [PMC free article] [PubMed] [Google Scholar]


