Abstract
Background
The ‘Sunshine Soul Park’ is a network of social welfare institutions that provides communitybased rehabilitation services for individuals with mental illness.
Aims
Assess the effectiveness of the rehabilitation services provided at the ‘Sunshine Soul Park’ on the psychotic symptoms and social functioning of individuals with schizophrenia and, based on these findings, provide a theoretical model of community-based rehabilitation.
Methods
Sixty individuals with schizophrenia in the Huangpu District of Shanghai volunteered for the rehabilitation training program provided at six ‘Sunshine Soul Park’ community centers that involves day treatment, medication monitoring, biweekly rehabilitation training, and other recreational, social, and intellectual activities. A matched control group was recruited from individuals with schizophrenia registered on the Huangpu District registry of the ‘Severe Mental Illness Prevention and Rehabilitation System’. All participants continued their medication without change for the full year of follow-up. Both groups were assessed at baseline, and 3, 6, and 12 months after enrollment using the Insight and Treatment Attitude Questionnaire (ITAQ), Social Disability Screening Schedule (SDSS), Generic Quality of Life Inventory-74 (GQOLI-74), and Positive and Negative Syndrome Scale (PANSS).
Results
In the intervention group the ITAQ, SDSS, GQOLI-74, and PANSS scores showed statistically significant improvement compared to baseline at each follow-up assessment. Moreover, the trend in improvement in the interventions group is significantly faster than that in the control group.
Conclusions
The ‘Sunshine Soul Park’ rehabilitation training program enhances patients’ knowledge about their disorder and improves their social functioning and quality of life. Further studies to assess methods for up-scaling this intervention to other areas of China are warranted.
Keywords: schizophrenia, community rehabilitation, ‘Sunshine Soul Garden’, characteristic path length, quality of life, China
Abstract
背景
“阳光心园”是社会福利机构网络,为精神疾 病患者提供以社区为基础的康复服务。
目的
评估“阳光心园”针对精神分裂症患者的精神 病性症状和社会功能提供的康复服务的有效性,并根 据这些发现得出基于社区的康复服务的理论模型。
方法
上海市黄浦区的60 名精神分裂症患者自愿在 六个“阳光心园”社区参加了由其社区中心提供的康 复训练计划,涉及日间治疗、用药监测、每两周一次 的康复训练、以及其它休闲、社交和智力活动。从黄 浦区“重性精神疾病预防与康复系统” 中登记注册的 精神分裂症患者中招募相匹配的对照组。所有的参与 者在随访的一年内保持原先的用药,不做更改。在基 线和登记注册后的第3 个、第6 个和第12 个月分别对 两组使用自知力与治疗态度问卷(Insight and Treatment Attitude Questionnaire, ITAQ)、社会功能缺陷筛选量表 (Social Disability Screening Schedule, SDSS)、生活质量 综合评定问卷—74 (Generic Quality of Life Inventory-74, GQOLI-74)、和阳性和阴性症状量表(Positive and Negative Syndrome Scale, PANSS) 进行评估。
结果
在干预组中, 每次随访的ITAQ、SDSS、 GQOLI-74 和PANSS 评分都显著优于基线水平,有统计 学意义。此外,干预组的改善趋势显著快于对照组。
结论
“阳光心园”康复训练项目增进了患者对他们 疾病的了解,并提高他们的社会功能和生活质量。对 于这种方法,我们需要进一步研究,以评估是否必要 将这种方法推广至中国的其它地区。
中文全文
本文全文中文版从2015年08月06日起在http://dx.doi.org/10.11919/j.issn.1002-0829.215026可供免费阅览下载
1. Introduction
Schizophrenia is a severe mental illness with unclear etiology, an early age of onset, and high relapse rates. The disorder adversely affects both the cognitive and social functioning of affected individuals[1,2,3] resulting in a substantial reduction in the quality of their lives and that of their care givers.[4,5] The social recovery of patients with schizophrenia has primarily been the responsibility of families and community-based mental health services. Several models of community-based rehabilitation for persons with schizophrenia have been proposed; most focus on outpatient services that are able to reduce the severity of psychotic symptoms and,thus,result in lower rates of relapse and re-hospitalization.[6,7,8,9,10] Compared with patients who receive only pharmacological interventions, patients who receive combined pharmacological and rehabilitation services in outpatient clinics have better social functioning and insight. Starting in the 1980s China started adapting Western models of outpatient rehabilitation services to manage patients who had been discharged from psychiatric hospitals with a diagnosis of schizophrenia. Tang and colleagues[12] found that after seven years of follow-up 49% of discharged patients with schizophrenia who used outpatient rehabilitation services had returned to work; and Yu and colleagues[13] reported that persons with schizophrenia who utilized outpatient rehabilitation services had a reduction in negative symptoms, and improved social functioning and quality of life.
The ‘Sunshine Soul Park’ is a social welfare institution with centers in each urban sub-district (that is, ‘street’) of Shanghai that is operated by the China Disabled Persons Federation (a semi-governmental agency) and the Ministry of Civil Affairs in Shanghai. These centers, which vary in size depending on the population of the sub-district, provide multiplefaceted rehabilitation services for a subgroup of mentally disabled persons in the community (those who apply and are enrolled, often after a lengthy wait on a waitlist). These centers provide day care, psychological counseling, recreational rehabilitation, work rehabilitation, and social skills training to clinically stable patients with chronic mental disorders. Similar to psychiatric outpatient clinics, the ‘Sunshine Soul Park’ centers only provide rehabilitation services during the daytime; patients continue to live in their homes (usually with family members). Previous reports[14] have shown that the ‘Sunshine Soul Park’ rehabilitation program improves participants’ work skills and psychiatric symptoms; but these reports did not specifically focus on the effectiveness of the rehabilitation program among patients with schizophrenia.
The current study compares the functioning of community-dwelling individuals with schizophrenia who do or do not participate in the ‘Sunshine Soul Park’ rehabilitation program over a one-year follow-up period.
2. Methods
2.1. Sample
The enrollment process is shown in Figure 1. Starting in November 2010, all new enrollees at the six ‘Sunshine Soul Park’ community centers in the six sub-districts of Shanghai’s Huangpu District (population, 600,000) were invited to participate in the rehabilitation intervention. The first 60 individuals who met the following inclusion criteria were enrolled: a) between 18 to 50 years of age; b) diagnosed with schizophrenia according to the criteria of International Classification of Diseases (ICD-10)[15]; c) clinically stable (i.e., the positive subscale score of the Positive and Negative Syndrome Scale [PANSS][16] was less than 4); d) able to communicate clearly; e) had no alcohol or substance abuse problems, serious physical illnesses, or dementia; and f) both the patient and the guardian provided written informed consent to participate in the study.
Figure 1. Flowchart of the study.
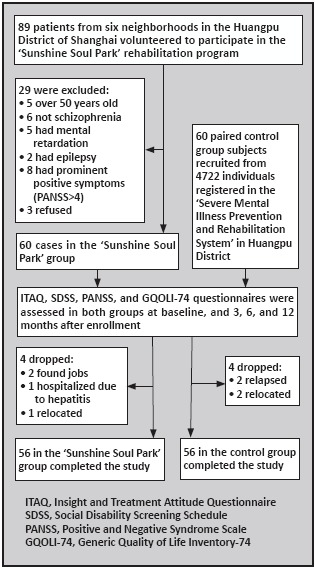
Sixty control subjects who met the inclusion criteria and were matched for gender, age (+ 3 years), and education to enrolled participants at the ‘Sunshine Soul Park’ community centers were recruited from the 4722 individuals registered in the ‘Severe Mental Illness Prevention and Rehabilitation System’ of Huangpu District. The control subjects and their guardians all signed the informed consent form before participating in the study.
2.2. Intervention
All the patients in the two groups continued their pharmacological treatment at the same dose throughout the one-year follow-up period. In the intervention (rehabilitation program) group medications were managed by psychiatrists who regularly visited the ‘Sunshine Soul Park’ community centers and the daily use of medication was jointly monitored by center staff (when the patient was at the center) and family members (when the patient was home). Patients in the control group were usually seen every three months by their treating clinician in the outpatient department of the psychiatric hospital in the Huangpu District or at one of the other psychiatric hospitals in Shanghai; their medication use was monitored by their family members.
Rehabilitation training for the intervention group was based on a model developed by Anding Hospital in Beijing and the disease control center at Shanghai Mental Health Center[17] that provided 24 biweekly sessions of 60-90 minutes over a 1-year period covering the following topics: a) training in how best to use and monitor the effects of antipsychotic medication; b) training in independent living; c) training in interpersonal communication; and d) career training. This training was provided by psychiatrists and psychiatric nurses. Individuals who missed three sessions in a row were dropped from the program (which was hard to get into), and those who appeared reluctant to continue at the center were actively encouraged to continue by both center staff and family members, so participation at each of the 24 sessions was over 90%. Participants in the rehabilitation group also attended other, less structured, activities at the centers on weekdays including social skills training using role-playing, hobby groups such as painting and calligraphy, and work skills groups such as computer competency and English language training. Occasionally, some of the intervention group subjects also received one-to-one counseling by a trained counsellor or volunteer social worker.
2.3. Assessment
Four questionnaires were administered to all participants in the study at baseline and at the end of the 3rd, 6th, and 12th month after enrollment: PANSS[16] (higher scores indicate more serious symptoms); Generic Quality of Life Inventory-74 (GQOLI-74)[16] (including 74 items and 20 factors to measure four dimensions of the quality of life - living conditions, physical functioning, psychological functioning, and social functioning); (c) Social Disability Screening Schedule (SDSS)[18] (assessing the degree of social disability within in the prior month; and the Insight and Treatment Attitude Questionnaire (ITAQ)[19] (with eleven items that assess knowledge about the illness and attitudes about using medication). For the current study GQOLI-74, SDSS, and ITAQ scores were considered primary outcomes and the PANSS score was considered as a secondary outcome. These instruments were administered by trained psychiatrists who did not participate in the clinical treatment or rehabilitation program of the patients. The evaluators were instructed not to ask the patients about their group assignment status; however, in some cases evaluators went to the ‘Sunshine Soul Park’ community centers to evaluate patients and, thus, learned of their group assignment, so the outcome evaluation was not completely ‘blind’.
2.4. Statistical analysis
The data was analyzed using SPSS 17.0 software. Independent t-tests, repeated measures ANOVA and two -way ANOVA were used to compare continuous outcomes within each group and between the two groups. Chi-squared tests were used to compare the frequency of categorical variables between two groups. Differences between groups were considered statistically significant when p<0.05.
3. Results
The characteristics of individuals in the intervention group (i.e., participants in the rehabilitation program at the ‘Sunshine Soul Park’ community centers) and control group are shown in Table1. Participants in the study were primarily patients with a chronic course of illness; the range in the duration of illness was 2 to 29 years in the intervention group and 2 to 28 years in the control group. There were no significant differences in the age, education, duration of illness, or other characteristics between the two groups.
Table 1.
Comparison of the characteristics of the intervention and control groups[n=60 in both groups]
| Characteristic | Intervention group | Control group | statistic | p-value |
| Male, n (%) | 31 (52%) | 31 (52%) | X2=0.00 | 1.000 |
| Age, mean (sd) | 39.2 (7.9) | 38.8 (7.5) | t=0.31 | 0.776 |
| Education, n (%) | ||||
| primary school or below | 8 (13%) | 5 (8%) | ||
| middle school and high school | 45 (75%) | 48 (80%) | X2=0.78 | 0.674 |
| college | 7 (12%) | 7 (12%) | ||
| Marital status, n (%) | ||||
| never married | 47 (78%) | 47 (78%) | ||
| currently married | 3 (5%) | 5 (8%) | X2=0.72 | 0.697 |
| separated or divorced | 10 (17%) | 8 (13%) | ||
| Years duration of illness, mean (sd) | 18.8 (7.6) | 19.0 (8.0) | t=0.31 | 0.888 |
| Number of episodes, mean (sd) | 2.3 (1.1) | 2.5 (1.4) | t=0.70 | 0.386 |
| Number of different antipsychotic medications used previously, mean (sd) | 2.7 (0.6) | 2.4 (1.4) | t=1.37 | 0.129 |
As shown in Figure 1, there were four dropouts over the one-year follow-up in each of the groups. In the intervention group, two individuals obtained regular employment and, thus, were unable to come to the community center, one developed hepatitis and required long-term medical care, and one moved to another location outside of the Huangpu District. In the control group two individuals relapsed and had to be rehospitalized and two moved to another location outside of the Huangpu District.
The results for ITAQ, SDSS, and PANSS are shown in Tables 2 and 3. The total ITAQ score, total SDSS score, total PANSS score, and negative symptoms PANSS subscales scores were all similar: there was no significant difference in the results between the groups at baseline; subsequently both groups showed steady improvement over baseline at the end of the 3rd, 6th, and 12th month; and the degree of improvement was significantly greater in the intervention group than in the control group at all three follow-up evaluations. The general psychopathology PANSS subscale score was significantly worse in the intervention group than in the control group at baseline but in all three follow-up assessments it was significantly better in the intervention group than in the control group. For all of these measures the repeated measures ANOVA showed that the trend in improvement in the intervention group was greater than that in the control group.
Table 2.
Comparison of mean (sd) scores between the two groups on the Insight and Treatment Attitude Questionnaire (ITAQ) and the Social Disability Screening Scale (SDSS)a [n=56 in both groups]
| time point | intervention group | control group | F | p | |
| ITAQ | baseline | 7.47 (3.57) | 7.39 (3.57) | 0.22 | 0.642 |
| end of 3rd month | 10.91 (3.84) | 8.32 (3.68) | 194.31 | <0.001 | |
| end of 6th month | 14.32 (3.71) | 8.53 (3.56) | 1035.41 | <0.001 | |
| end of 12th month | 16.71 (3.94) | 9.00 (3.51) | 1742.15 | <0.001 | |
| SDSS | baseline | 14.13 (2.68) | 14.25 (2.58) | 0.79 | 0.375 |
| end of 3rd month | 13.24 (2.67) | 14.20 (2.61) | 54.50 | <0.001 | |
| end of 6th month | 11.60 (2.78) | 14.02 (2.41) | 353.64 | <0.001 | |
| end of 12th month | 10.59 (3.21) | 13.88 (2.29) | 571.46 | <0.001 |
arepeated measures ANOVA indicate that the trend in improvement in the total scores in the intervention group was greater than that in the control group for both ITAQ (F=1996.40, p<0.001) and for SDSS (F=962.78, p<0.001)
Table 3.
Comparison of mean (sd) scores between the two groups on the Positive and Negative Syndrome Scale (PANSS)a [n=56 in both groups]
| time point | intervention group | control group | F | p | |
| positive symptoms | baseline | 12.34 (2.24) | 12.59 (2.32) | 5.10 | 0.024 |
| end of 3rd month | 11.77 (2.11) | 11.77 (2.01) | 0.00 | 0.992 | |
| end of 6th month | 11.03 (2.00) | 11.23 (2.42) | 3.49 | 0.062 | |
| end of 12th month | 10.44 (1.99) | 10.79 (2.85) | 8.56 | 0.003 | |
| negative symptoms | baseline | 19.25 (2.75) | 19.35 (2.64) | 0.52 | 0.467 |
| end of 3rd month | 17.25 (2.48) | 18.90 (2.58) | 182.59 | <0.001 | |
| end of 6th month | 15.12 (2.66) | 18.48 (2.55) | 675.77 | <0.001 | |
| end of 12th month | 13.64 (2.48) | 18.24 (2.53) | 1376.93 | <0.001 | |
| general psychopathology | baseline | 33.47 (3.58) | 33.03 (3.24) | 3.53 | <0.001 |
| end of 3rd month | 30.76 (2.99) | 31.97 (3.03) | 76.63 | <0.001 | |
| end of 6th month | 27.85 (3.08) | 31.26 (3.31) | 482.19 | <0.001 | |
| end of 12th month | 25.54 (3.11) | 30.69 (3.47) | 976.93 | <0.001 | |
| total score | baseline | 65.06 (5.24) | 64.98 (4.51) | 0.35 | 0.556 |
| end of 3rd month | 59.79 (4.76) | 62.7 (4.72) | 185.53 | <0.001 | |
| end of 6th month | 54.01 (5.00) | 60.99 (5.81) | 714.02 | <0.001 | |
| end of 12th month | 49.5 (5.65) | 59.74 (6.61) | 1095.57 | <0.001 |
arepeated measures ANOVA indicate that the trend in improvement in the PANSS positive symptoms subscale score was not significantly different between the groups (F=9.45, p=0.729) but the trend in improvement was greater in the intervention group than the control group for the negative symptoms subscale score (F=662.38, p<0.001), the general psychopathology subscale score (F=137.52, p<0.001), and the PANSS total score (F=428.43, p<0.001)
The positive symptom subscale of PANSS was significantly greater in the control group than in the intervention group at baseline and slightly lower than the control group; both groups showed gradual improvement over time but there was no significant difference in the rate of improvement between the groups.
The results for the GQOLI-74 are shown in Table 4. The overall quality of life score was significantly greater (i.e., higher quality of life) at baseline in the control group than in the intervention group but at the end of the 6th month and 12th month quality of life was significantly better in the intervention group, so the trend in improvement was significantly greater in the intervention group. Both the social functioning and psychological functioning subscale scores of GQOLI-74 show a significantly stronger trend for improvement in the intervention group than in the control group over the 1-year study. However, the living condition subscale score did not show any difference between groups at any point in the study and the physical functioning subscale score showed no significant difference in the trend over time in the two groups.
Table 4.
Comparison of mean (sd) scores between the two groups on the 74-item Generic Quality of Life Inventory (GQOLI-74)a [n=56 in both groups]
| time point | intervention group | control group | F | p | |
| physical functioning | baseline | 55.77 (10.59) | 57.07 (10.93) | 5.99 | 0.014 |
| end of 3rd month | 55.22 (8.72) | 56.62 (9.98) | 9.14 | 0.003 | |
| end of 6th month | 64.48 (8.42) | 63.79 (8.31) | 2.81 | 0.943 | |
| end of 12th month | 62.01 (8.00) | 56.63 (9.27) | 157.11 | <0.001 | |
| psychological functioning | baseline | 55.28 (7.90) | 55.94 (8.10) | 2.73 | 0.098 |
| end of 3rd month | 53.58 (7.69) | 54.34 (8.75) | 3.44 | 0.064 | |
| end of 6th month | 59.37 (8.84) | 59.91 (10.62) | 1.26 | 0.262 | |
| end of 12th month | 64.24 (8.08) | 60.41 (10.65) | 66.69 | <0.001 | |
| social functioning | baseline | 45.84 (9.84) | 46.44 (10.32) | 4.04 | 0.229 |
| end of 3rd month | 48.78 (9.54) | 46.16 (10.34) | 19.86 | <0.001 | |
| end of 6th month | 51.19 (9.13) | 44.56 (9.71) | 172.82 | <0.001 | |
| end of 12th month | 54.48 (9.36) | 44.11 (9.68) | 466.03 | <0.001 | |
| living conditions | baseline | 46.71 (12.91) | 47.06 (13.51) | 0.28 | 0.596 |
| end of 3rd month | 42.48 (13.61) | 42.96 (11.74) | 0.59 | 0.441 | |
| end of 6th month | 43.22 (11.96) | 42.79 (11.16) | 0.56 | 0.455 | |
| end of 12th month | 47.67 (14.43) | 46.83 (13.08) | 1.52 | 0.219 | |
| overall quality of life | baseline | 50.60 (7.46) | 51.28 (7.56) | 4.13 | <0.042 |
| end of 3rd month | 49.95 (6.58) | 49.88 (7.56) | 0.05 | 0.838 | |
| end of 6th month | 54.82 (6.65) | 52.64 (7.26) | 35.84 | <0.001 | |
| end of 12th month | 57.35 (7.10) | 51.71 (7.46) | 225.54 | <0.001 |
a repeated measures ANOVA indicate no significant differences in the trend over time between the two groups for the physical functioning subscale (F=23.96, p=0.086) and living conditions subscale (F=64.99, p=0.671), but there was a significant advantage for the treatment group in the psychological functioning subscale (F=857.57, p<0.001) the social functioning subscale (F=2225.21, p<0.001), and the overall quality of life score (F=1185.78, p<0.001)
4. Discussion
4.1. Main findings
This one-year follow up study found that compared to patients in a ‘treatment as usual’ control group those in the ‘Sunshine Soul Park’ rehabilitation program group show significantly greater increase in ITAQ scores, significant greater reduction in SDSS and PANSS scores, and an increase in the GQOLI-74 overall score and social functioning and psychological functioning subscale scores. These results indicate that the ‘Sunshine Soul Park’ rehabilitation intervention is effective in improving the social functioning of patients with schizophrenia and in helping them understand and manage their illness. Previous studies in China have obtained similar results.[20,21,22] Taken together, these studies demonstrate that a supportive social atmosphere promotes the rehabilitation of Chinese patients with chronic schizophrenia, a finding that is consistent with findings from similar studies in high-income countries.[23] Developing appropriate community-based rehabilitation programs is a promising way to slow or reverse the decline in patients’ social functioning, increase the proportion that can become fully functioning members of society, and, thus, substantially reduce the burden of the disease.
4.2. Limitations
Several issues need to be considered when evaluating these results. Participants in the rehabilitation program at the ‘Sunshine Soul Park’ community centers spent most of their time at the centers participating in activities that were not specifically part of the biweekly training sessions, so it cannot be stated with certainty that the improvement seen in the interventions group was specifically due to the 24 biweekly training sessions they attended. Participants in the program had applied to attend the community center’s activities, an opportunity that is only available to a minority of individuals with chronic schizophrenia in the community, so they (or their family members) may have been more strongly motivated (and, thus, have a better outcome) than patients who did not apply to go to the community center. The evaluation of the outcome was not blind (all patients and some of the evaluators knew the group assignment) so this may have introduced bias in the evaluation. Finally, the one-year duration of the intervention is quite long, but the benefit of the intervention my fall off after stopping the biweekly sessions, so its unsure whether or not this needs to be an ongoing or intermittent intervention.
4.3. Implications
This report confirms previous findings about the benefits of active, community-based rehabilitation programs for patients with chronic schizophrenia who are clinically stable on routine doses of antipsychotic medication; this type of intervention has better clinical, social, and quality of life outcomes than routine outpatient followup, than chronic inpatient care, and than community day-care that is limited to the monitoring of patients.[24,25,26,27,28,29,30]
There are, however, several issues that need to be resolved before moving to up-scale this type of community-based intervention in China and other lowand middle-income countries. First, the results need to be confirmed with a fully blinded study that isolates the different components (i.e., biweekly training, daily monitoring of medication by a care worker, other activities at the day-care center) to determine which component or which combination of components is effective. Second, the sample in our study was rather narrow - motivated patients with stable symptoms from motivated families - so the acceptability of the intervention to an unrestricted group of patients with schizophrenia needs to be evaluated. Third, the most effective duration and frequency of the training component of the intervention needs to be determined (does it need to be continuous or will intermittent ‘booster sessions’ be sufficient to maintain the effect?). Finally, the intervention requires substantial professional staff time, so scaling up the intervention may not be feasible until a large cadre of community mental health workers are trained and available - a task that will be particularly difficult to accomplish in rural communities that are already resource-poor. Creative ways must be developed to identify, train, and fund this new cadre of providers.
Biography
Ying Zhou graduated from Tongji University in 2000 with a Bachelor’s degree in clinical medicine. Since 2000, he has worked at the Mental Health Center of Huangpu District, Shanghai, as a chief psychiatrist and director of the rehabilitation department. His research interest is in the community rehabilitation of schizophrenia.
Funding Statement
This study was funded by the Shanghai Huangpu district key scientific and technical program: (2010) HGG—R12.
Conflict of interest: The authors declared no conflict of interest related to this manuscript.
Ethics approval: This study was approved by the Ethics Committee of the Huangpu Mental Health Center (Shanghai, China).
Informed consent: All the patients (or their guardians) provided written informed consent to participate in this study.
References
- 1.Bustillo J, Lauriello J, Horan W, Keith S. The psychosocial treatment of schizophrenia: an update. Am J Psychiatry. 2001;158(2):163–175. doi: 10.1176/appi.ajp.158.2.163. [DOI] [PubMed] [Google Scholar]
- 2.Kopelowicz A, Liberman RP, Mintz J, Zarate R. Comparison of efficacy of social skills training for deficit and non deficit negative symptoms in schizophrenia. Am J Psychiatry. 1997;154(3): 424–425. doi: 10.1176/ajp.154.3.424. [DOI] [PubMed] [Google Scholar]
- 3.Heinssen RK, Liberman RP, Kopelowicz A. Psychosocial skills training for schizophrenia: lessons from the laboratory. Schizophre bull. 2000;26(1): 21–46. doi: 10.1093/oxfordjournals.schbul.a033441. [DOI] [PubMed] [Google Scholar]
- 4.Yang YL, Lin XJ. [A primary retrospective study on recidivism among patients with schizophrenia] Zhongguo Jian Kang Xin Li Xue Za Zhi. 2014;22(11):1603–1605. doi: 10.13342/j.cnki.cjhp.2014.11.002. Chinese. [DOI] [Google Scholar]
- 5.Liu TL, Song XM, Chen G, Zheng XY. [Violent behavior in people with schizophrenia: a review] Zhong Hua Liu Xing Bing Xue Za Zhi. 2013;34(3):297–300. doi: 10.3760/cma.j.issn.0254-6450.2013.03.021. Chinese. [DOI] [PubMed] [Google Scholar]
- 6.Liberman RP, Mueser KT, Wallace CJ. Social skills training for schizophrenic individuals at risk for relapse. Am J Psychiatry. 1986;143(4): 523–526. doi: 10.1176/ajp.143.4.523. [DOI] [PubMed] [Google Scholar]
- 7.Shek E, Stein AT, Shansis FM, Marshall M, Crowther R, Tyrer P. Day hospital versus outpatient care for people with schizophrenia. Cochrane Database Syst Rev. 2009;7(4) doi: 10.1002/14651858.CD003240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pazvantoglu O, Simsek OF, Aydemir O, Sarisoy G, Korkmaz IZ, Mor S, et al. Reliability and validity of subjective well-being under neuroleptics scale-short form-turkish version. Bull ClinPsychopharmacol. 2012;22(3): 235–243. doi: 10.5455/bcp.20120731082335. [DOI] [Google Scholar]
- 9.Yildiz M, Yazici A , Unal S, Aker T. [Schizophrenia literature social skills training in social care: a multicenter an application of turkey in symptom management and medication management] TUrkPsikiyatrDerg-Turkish J Psychiatry. 2002;13(1): 41–47. Turkish. [PubMed] [Google Scholar]
- 10.Yazici A, Cos kun S. [BRSHH Day Hospital and rehabilitation center patient profile andwork program] Anadolu Psikiyatr Derg-Anatolian J Psychiatry. 2008;9(Suppl 1): 21–23. Anatolian. [Google Scholar]
- 11.Arslan M, Kurt E, Eryildiz D, Yazici A, Can A, Emul M. Effects of a psychosocial rehabilitation program in addition to medication in schizophrenic patients: a controlled study. KlinikPsikofarmakolojiBulteni. 2014;24(4): 360–367. doi: 10.5455/bcp.20140701074403. [DOI] [Google Scholar]
- 12.Tang WZ, Yuan YC. [Rehabilitation of schizophrenia through Day-hospital: A 7 year follow-up] Xian Dai Kang Fu. 2000;4(4): 552–553. Chinese. [Google Scholar]
- 13.Yu YY, Yu SJ, Yang X, Zhang ZW. [Affect of the day hospital workshop for the patients with schizophrenia in functional recovery] Sichuan Jing Shen Wei Sheng. 2010;23(2): 102–105. doi: 10.3969/j.issn.1007-3256.2010.02.012. Chinese. [DOI] [Google Scholar]
- 14.Yang XD, Zhang QG. [Evaluation of “Sunshine Heart Park” on the patients’rehabilitation with mental health disorder] She Qu Wei Sheng Bao Jian. 2011;10(4): 303–304. Chinese. [Google Scholar]
- 15.World Health Organization. International Statistical Classification of Disease and Related Health Problems, 10th Revision. Geneva: World Health Organization; 1992. [Google Scholar]
- 16. Wang XD, Wang XL. [Mental Health Rating Scale Manual (updated version)]. Beijing: Chinese Mental Health Journal; 1999263-275. [Google Scholar]
- 17.Zhou Y, Zhou RS, Lin YQ, Chen J. [The effects of the stylized training on community insight and social functioning of patients with schizophrenia] Yi Yao Qian Yan. 2014;4(24): 216. Chinese. [Google Scholar]
- 18. Zhang MY. [Psychiatric Rating Scale Manual] Changsha: Hunan Science and Technology Press; 199381-168Chinese [Google Scholar]
- 19.Liu HQ, Zhang PY. [Schizophrenia insight: The application of "questionnaire about insight and treatment attitude"] Shanghai Arch Psychiatry. 1995;3: 158. Chinese. [Google Scholar]
- 20.Chang YL, Li WY, Xiang YT, Xie L, Gao L, Chen GL. [Effect of whole-period psychiatric rehabilitation on outpatients with schizophrenia] Zhongguo Kang Fu Li Lun Yu Shi Jian. 2004;10(4): 198–199. doi: 10.3969/j.issn.1006-9771.2004.04.003. Chinese. [DOI] [Google Scholar]
- 21.Zhang WB, Zhang GF, Shen WL, Zhou Q, Zhao J, Su YL, et al. [Effects of social skills training for schizophrenic patients in the community] Zhongguo Jian Kang Xin Li Xue Za Zhi. 2011;19(10): 1153–1154. Chinese. [Google Scholar]
- 22.Sun XZ, Li YQ, Fang H. [Effects of community rehabilitation intervention for schizophrenia] Zhongguo Jian Kang Xin Li Xue Za Zhi. 2013;21(1): 54–55. Chinese. [Google Scholar]
- 23.Anthony WA Baltimore MD. The Principles of Psychiatric Rehabilitation. California: University Park Press; 1980. [Google Scholar]
- 24.Brooker C. A new role for the community psychiatric nurse in working with families caring for a relative with schizophrenia. Int J soc Psychiatry. 1990;36: 216–224. doi: 10.1177/002076409003600307. [DOI] [PubMed] [Google Scholar]
- 25.Holmberg G. Treatment, care and rehabilitation of the chronic mentally ill in Sweden. Hosp Community Psychiatry. 1998;39: 190–194. doi: 10.1176/ps.39.2.190. [DOI] [PubMed] [Google Scholar]
- 26.Cheng YM, Yan BP, Yu LY, Fu XG, Cui W, Di YQ , et al. [Investigation on mental disabilities and related factors of 210 patients with schizophrenia] Zhongguo Jian Kang Xin Li Xue Za Zhi. 2012;20(8): 1136–1139. Chinese. [Google Scholar]
- 27.Li WX. [The effect of comprehensive intervention on rehabilitation of patients with first-epsiode schizophrenia] Zhongguo Jian Kang Xin Li Xue Za Zhi. 2013;21(3): 403–405. Chinese. [Google Scholar]
- 28.Jiang MX, Ji YW, Zhou LJ, Ji WD, Tang WZ. [Study on correlation between social support and health state of community schizophrenia patients] Zhongguo Jian Kang Xin Li Xue Za Zhi. 2011;19(11): 1298–1301. Chinese. [Google Scholar]
- 29.Xiang YQ, Weng YZ, Hou YZ, Wang CY, Chen L. [A preliminary study of mediation management and symptom management skills-training for preventing] Zhong Hua Jing Shen Ke Za Zhi. 2001;34(3): 153–156. doi: 10.3760/j:issn:1006-7884.2001.03.008. Chinese. [DOI] [Google Scholar]
- 30.Zhen H, Chen SL, Tang AD, Zhou LJ, Ji WD. [Study on intervention effects of comprehensive community service team for schizophrenia in community] Zhongguo Jian Kang Xin Li Xue Za Zhi. 2012;20(11): 1615–1617. Chinese. [Google Scholar]


