Abstract
Imiquimod is a synthetic imidazoquinolone amine, which has potent immune response modifier activity, when topically used. This characteristic property of imiquimod has led to its use in a number of applications in dermatology, particularly in cutaneous malignancies, where it has been found to be effective and safe. Currently, additional mechanisms for its activity in actinic keratosis, basal cell carcinoma, and invasive squamous cell carcinoma have been elucidated. Its usage for cutaneous metastasis in breast cancer has been a further addition to its therapeutic armamentarium recently.
KEY WORDS: Cutaneous malignancies, imidazoquinolone, imiquimod
Introduction
Imiquimod is a synthetic compound which belongs to a new class of drugs referred to as imidazoquinolones. It acts as an immune response modifier in the body and has shown to have potent anti-viral and anti-tumor activity.[1] While screening drugs for anti-herpes virus activity, imiquimod's role as an immune response modifier was discovered. In 1999, the Food and Drug Administration (FDA) approved imiquimod for the treatment of external genital and perianal warts and in 2004, it was approved for treating actinic keratosis (AK) and superficial basal cell carcinoma (BCC). Recently, imiquimod has been found to be useful in a variety of dermatologic conditions. This article will review the clinical applications of 5% imiquimod cream in cutaneous premalignant and malignant conditions.
Mechanism of Action as Related to Cutaneous Malignancies
Imiquimod acts on the innate and the adaptive immune responses both directly and indirectly. Direct action is by binding to toll-like receptors (TLR) seven and eight of macrophages, monocytes, and dendritic cells[2] and by induction of apoptosis. Indirect action occurs by imiquimod inducing the release of immune modulatory cytokines. Imiquimod's effectiveness is also attributed by its action on Langerhans cells thereby stimulating its ability to present antigens[1] and enhancing its migration to the draining lymph nodes where antigens are presented to T cells, thus activating the body's adaptive immune response.
Direct Actions
Recent studies have thrown light on the possible direct effects of imiquimod on cutaneous malignancies. Induction of apoptosis in tumor cell lines has been postulated as the prime mechanism here. Imiquimod activates the workhorses of apoptosis, namely the caspase family of proteases.[2] There are two pathways that induce apoptosis, the extrinsic and the intrinsic pathway. It has been demonstrated that imiquimod brings about apoptosis by working on the intrinsic pathway which converge at the mitochondria. On activation of the intrinsic apoptotic pathway, pro-apoptotic molecules such as apoptosis-inducing factor, smac, HtrA2, cytochrome C, and endonuclease G are released.[3] These molecules then stimulate caspase-9 in a multimeric complex called the apoptosome or bring about the destruction of malignant cells in an independent manner. The independent manner by which imiquimod brings about apoptosis of tumor cell lines is by up-regulating pro-apoptotic proteins of the Bcl-2 family of proteins namely Bax and Bak, and the BH3-only proteins such as Bim, Bid, Bmf, Noxa, and Puma. Hence, we see that there is an increased expression of pro-apoptotic proteins and a down-regulation of anti-apoptotic proteins.[3]
Indirect Actions
Indirect actions of imiquimod occur by inducing the release of various cytokines. These cytokines stimulate a cell-mediated immune response, and this may be of value in the drug's anti-tumor activity.[4] The main cytokines induced include IL-12, tumor necrosis factor-alpha (TNF-alpha), and interferon (INF)-gamma. These in turn increase the levels of cytotoxic T cells and natural killer cells in the local milieu by inducing 2’5’oligoadenylate synthetase and blocking angiogenesis.[2] Further increase in IL-12 down-regulates IL-10 and thus stimulates anti-tumor T cells.[4]
Pharmacokinetics
Following the topical application of 5% imiquimod cream, there is minimal systemic absorption. Less than 0.9% of the drug is excreted by the urinary and the gastrointestinal system.[5]
Uses of Imiquimod in Cutaneous Premalignant and Malignant Conditions
Actinic Keratosis
Actinic keratosis are premalignant skin lesions seen mainly in fair-skinned individuals with a risk of transformation to invasive squamous cell carcinoma (SCC), and, therefore, this needs to be adequately dealt with. Imiquimod as a 5% cream was first approved by the FDA as a therapeutic agent for AK in 2004 and has shown exceedingly promising results for the same. Recently, imiquimod cream in a 3.75% strength has also become available with similar efficacy as the 5% cream and fewer cutaneous adverse effects. Apart from this advantage, an added advantage witnessed with the 3.75% preparation of imiquimod was the shorter duration of treatment and a wider surface area of application (i.e., 200 cm2 as compared to 25 cm2 for the 5% preparation of imiquimod).[6]
Newer mechanisms of imiquimod action postulated for actinic keratosis
Apart from the usual immunomodulatory role of imiquimod explained earlier, in AK, imiquimod additionally stimulated expression of E-selectin on tumor blood vessels, thereby promoting CD8+ cytotoxic T cells to occupy the tumor site, subsequently bringing about tumor regression clinically and histologically[7]
Following imiquimod usage, there is the development of T cell memory that further diminishes the risk of AK development.[8]
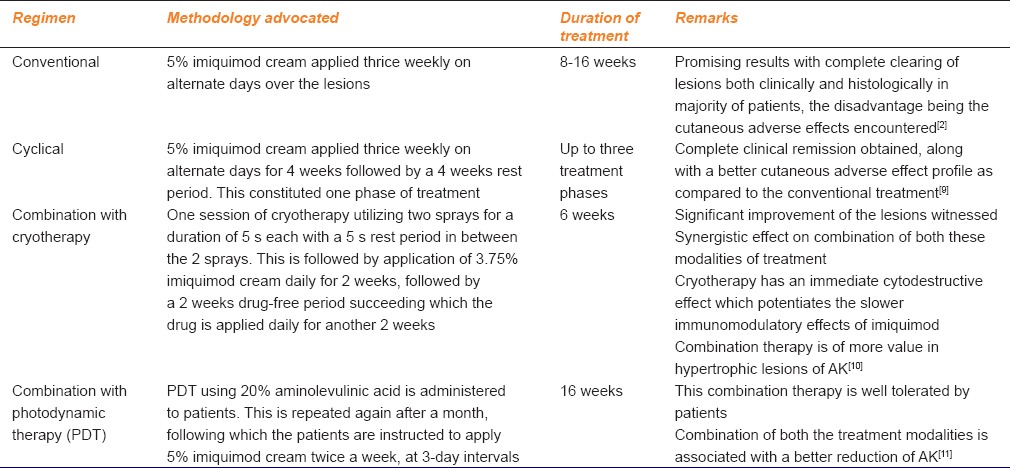
Treatment regimens using imiquimod for actinic keratosis [Table 1]
Table 1.
Treatment regimens using imiquimod for actinic keratosis
Newer and potent imiquimod analog
A sister drug of imiquimod, resiquimod whose potency has been found to be 10–100 times greater than imiquimod. A European phase II study demonstrated a 40–74.2% lesion clearance postapplication of resiquimod on AK lesions thrice weekly for a period of 4 weeks.[7]
Superficial Basal Cell Carcinoma
BCC is a common cutaneous neoplasm that very rarely metastasizes. However, if neglected, it can have a locally aggressive course with the destruction of the underlying tissues.
Newer mechanism of imiquimod action postulated for basal cell carcinoma
Apart from the mechanism of action mentioned above, in cases of BCC, imiquimod has an additional mechanism in antagonizing tumorigenesis. Imiquimod blocks the activation of the Hedgehog (HH)/glioma-associated oncogene (GLI) signaling pathway.[12] It has been suggested that an aberrant activation of this pathway plays an important role in the pathogenesis of BCC. Imiquimod acts in a direct, nonclassical manner, independent of its agonistic activity on the TLR-MyD88 complex in antagonizing the activity of the HH/GLI signaling pathway.[13] Imiquimod binds to the adenosine receptors and activates protein kinase A, which in turn phosphorylates GLI, heralding down-regulation of GLI 1 mRNA and protein levels in BCC cells. Because of this, there is a negative effect on the HH/GLI signaling pathway thereby thwarting its oncogenic potential.[14]
The first study using 5% imiquimod cream for treating superficial BCC was published in 1999. In the study, 35 patients were randomized to several dosing regimens of imiquimod, 5% cream, at one end of the spectrum and a vehicle cream at the other end. Treatment was given for a period of 16 weeks. In case of localized reactions to the cream, patients were given a drug-free period of 7 days. Patients who were given a twice daily, once daily, and thrice a week dosing of the drug showed 100% clearance based on histology. Sixty percentage of patients who were dosed twice weekly with imiquimod showed the complete clearance. Those patients who received imiquimod only once a week, 50% of them only showed complete remission. For the twice daily group treatment lasted for 10 weeks, 13 weeks for the once daily group and 14.5 weeks for the thrice weekly treatment group.[4]
Key points
Imiquimod, 5% cream, has been found effective in treating small superficial BCCs (maximum size of 2 cm in diameter) as demonstrated by several controlled trials and one systematic review[15]
Imiquimod has also been tried in a case series for the treatment of large superficial BCC of size >2 cm by Lacarrubba et al.[16] with promising results. However, more such studies are warranted for using imiquimod for the same
Multiple BCCs seen in Gorlin syndrome and xeroderma pigmentosum have also demonstrated a favorable outcome following application of 5% imiquimod[17,18]
However, though imiquimod has been employed in BCC, it may be appropriate only for selected primary low-risk lesions as a therapeutic modality. Surgical methods like Mohs micrographic surgery still remain the gold standard with a superior treatment outcome.[19,20]
Nodular Basal Cell Carcinoma
Imiquimod, 5% cream, can be used as an alternative in patients with small nodular BCCs who are poor candidates for surgery. Phase II clinical trials demonstrating the efficacy of imiquimod for nodular BCC have been seen in a 6-week trial in Australia and New Zealand and a 12-week trial in the United States. After 6 weeks of treatment, complete histologic clearance was seen in 71% of the cases in the 6 weeks once daily regimen and in 76% of the cases in the 12 weeks trial group.[2]
Sclerodermiform Basal Cell Carcinoma
In literature, a case report showing successful treatment of sclerodermiform BCC has been demonstrated. A thrice-weekly application of 5% imiquimod cream for 16 weeks showed complete clearance histologically with only scar tissue remnants. The patient was followed up for a period of 9 months post therapy, with observation of no recurrence.[2]
Squamous Cell Carcinoma in situ or Bowen's Disease
SCC in situ may involve the skin and mucosal surfaces. Of particular importance, is the involvement of the genital mucosa with Bowen's disease. These lesions generally are associated with human papilloma virus (HPV) infection, in particular, HPV type 16 which has the potential of diminishing the activity of tumor suppressor proteins p53 and Rb.[21]
Newer activity of imiquimod for genital Bowen's disease
It has been clearly demonstrated for SCC in situ of the vulva and the anal region, imiquimod apart from its anti-neoplastic effects, has shown to possess anti-viral activity against HPV and therefore, this action may potentiate imiquimod's effect for the above indication because elimination of HPV is a must to ensure the drugs therapeutic efficacy.[22]
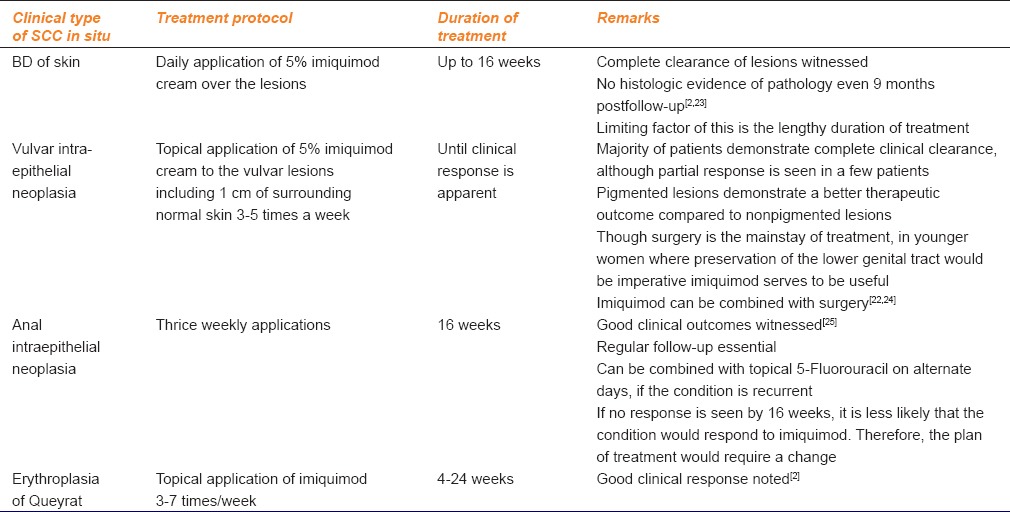
Salient features of imiquimod for squamous cell carcinoma in situ [Table 2]
Table 2.
Salient features of imiquimod for squamous cell carcinoma in situ
Invasive Squamous Cell Carcinoma
Five percentage imiquimod cream has shown efficacy even in invasive SCC.
Additional new mechanism of action of imiquimod for the above indication
Imiquimod in SCC additionally acts by down-regulating an anti-apoptotic regulator A20, thereby stimulating the nuclear factor kappa-beta signaling pathway in keratinocytes, eventually leading to apoptosis and tumor regression.[26]
Two immune-suppressed patients with renal transplant and having invasive SCC, one over the temple and the other over the sternum, were administered imiquimod 3 times a week for 12 weeks and imiquimod 3 times a week for 5 weeks and twice weekly for 7 weeks, respectively. Both patients when followed up at 6 and 8 months, respectively, had no evidence of residual tumor.[2]
Lentigo Maligna
Lentigo maligna (LM) is an in situ melanoma. The progression of LM to invasive melanoma is slow, owing to the sluggish radial growth phase and is estimated to be 5%.[27] The first reported successful treatment of LM was for an elderly patient who had LM on the scalp and was reluctant for surgery. Treatment was given for 7 months with various drug regimens and drug-free periods owing to localized reactions. There was complete clinical and histologic remission with no recurrence post 9 months of follow-up.[2] Ly et al.[28] and Powell et al.[29] have done a clinicopathologic evaluation of LM regression post 5% imiquimod cream usage and have demonstrated complete clearance in 53–75% of the treated patients. However, the major drawback for most of these studies was a follow-up for a maximum of period of only 1-year, which may be highly inadequate given the extremely slow radial growth phase seen in LM.
Key points
Long-term treatment with imiquimod is mandated for the above indication
May be combined with destructive therapies like CO2 laser
Even postclearance of lesions histologically, it is mandated to continue imiquimod application for a year.
Metastatic Melanoma
Several recent published studies have shown imiquimod to have promise in the treatment of metastatic melanoma (MM). Imiquimod was first used in a female patient who had lesions on the breast which were too extensive for surgery or radiotherapy. Imiquimod was applied thrice weekly along with systemic dacarbazine. By 12 weeks, the lesions treated with imiquimod completely resolved. Histopathology at 18 weeks showed apoptotic melanocytes surrounded by a dense lymphocytic infiltrate.[2]
Recent postulates in imiquimod's role for metastatic melanoma
Recently, the role of imiquimod in inhibiting melanoma has been further elaborated. Once imiquimod activates TLR7, plasmacytoid dendritic cells are stimulated, and are recruited to the site of the tumor and also the sentinel lymph nodes. There, they express TNF-related apoptosis inducing ligand, granzyme B, lysozyme, INF alpha, and other angiogenic inhibitors. A vascular endothelial growth factor is considered to be the prominent angiogenic factor in melanoma that promotes tumor growth. When these substances are released following imiquimod application, there is a block in tumor vascularization, which is an integral step necessary for the growth and invasiveness of the tumor, thereby halting tumor growth.[30,31]
Key points
Long-term treatment with imiquimod is required for this condition
May be combined with other with other therapies such as radiotherapy and CO2 laser
Though imiquimod may eradicate the cutaneous metastasis of MM, lymphatic spread of the tumor cannot be prevented by imiquimod.
Mycosis Fungoides
Imiquimod has been of help especially in the management of early mycosis fungoides (MF). The role in MF may be due to IFN alpha, a cytokine induced by imiquimod.[32]
Key points
For MF, imiquimod is an alternative treatment for localized plaques, that do not respond to conventional treatment modalities
Duration of treatment extends from 4 months to 2 years
Can be combined with systemic INFs in recalcitrant cases.[32]
Keratoacanthoma
Keratoacanthoma has been successfully treated with imiquimod applied daily for 4–12 weeks. Clinical regression was evident after 4–6 weeks. No recurrence was seen in the 4–6 months follow-up period.[2]
Extramammary Paget's Disease
Extramammary Paget's disease (EMPD) is a clinical condition simulating Paget's disease of the breast histologically and is clinically characterized by moist eczematous and erythematous plaques. Imiquimod acts by its immunomodulatory effect by stimulating synthesis of pro-inflammatory cytokines and inducing apoptosis of malignant cells. Successful treatment of EMPD has been seen following topical imiquimod usage. In a retrospective study by Luyten et al.,[33] it was shown that imiquimod produced a high rate of clinical clearance when used as a first-time treatment modality, and also for recurrent cases. A response rate of >80% was observed following the usage of 5% imiquimod cream. Sanderson et al.[34] documented 29 cases of vulvar EMPD that demonstrated 50% of clinical resolution for primary cases of EMPD and in 73% of patients with recurrent disease. In some cases though, 5% imiquimod may not achieve complete clearance of lesions. However, even partial reduction in the lesion size is profitable for both the patient and the treating physician, because once lesions reduce in size a more conservative surgical approach can be carried out, helping in achieving a better cosmetic and functional outcome.[35]
Infantile Hemangioma
Imiquimod acts here by its anti-angiogenic properties. Hu et al.[36] have demonstrated the efficacy of 5% imiquimod in superficial infantile hemangioma.
Merkel Cell Carcinoma
Merkel cell carcinoma (MCC) is a rare neuroendocrine tumor with an exorbitant malignant potential. Though MCC is a chemosensitive tumor, till date, no broadly accepted treatment protocol exists for the same.[37] Balducci et al.[38] have reported a case of MCC that showed complete remission posttopical application of 5% imiquimod combined with radiotherapy.
Kaposi's Sarcoma
Kaposi's sarcoma (KS) is a vascular neoplasm characterized by reddish-brown nodules and papules. Imiquimod acts by activating cytokines that have an antagonistic role in angiogenesis, pro-angiogenic factor down-regulation and induction of apoptosis in endothelial cells.[39] Goiriz et al.[40] reported a successful treatment outcome using 5% imiquimod cream in an 87-year-old man with widespread nodules of classical KS on both his lower limbs. Another patient with successful outcome following the usage of 5% imiquimod cream in a thrice weekly schedule for localized KS under occlusion for 8 h for a period of 3 months has been reported by Bernardini et al.[41]
Key point
In localized forms of KS imiquimod may have a role as monotherapy.
Cutaneous Metastasis Secondary to Carcinoma Breast
Breast cancer is a frequently diagnosed malignancy among women with an increased potential for cutaneous metastasis.
Role of imiquimod for this indication
The exact mechanism of imiquimod's role in breast cancer is unknown. However, it has been hypothesized that by binding to TLR7, imiquimod stimulates dendritic cells and macrophages releasing inflammatory cytokines which enable apoptosis of tumor cells.[42]
Adams et al.[43] and Dewan et al.[44] have elucidated the beneficial role of imiquimod in treating skin metastasis secondary to breast cancer. Henriques et al.[45] have further substantiated the beneficial role of imiquimod in metastatic breast cancer. Here, imiquimod applications were instituted 3 times a week following which there was an associated decrease in lesion thickness, intensity and pain score. In this report along with imiquimod, even chemotherapy was employed.
Adverse Effects
The most frequent adverse effects include itching, burning pain, and soreness at the application site. Other localized reactions include erythema, erosions, flaking, stinging, crusting, and vesiculation. Less frequent side effects include vitiligo such as hypopigmentation, hyperkeratosis, rhinitis, upper respiratory tract infections, myalgia, and headache. Rarely fatigue, dyspepsia, alopecia, chills, diarrhea, fever, and angioedema have been reported.[5]
Conclusions
Imiquimod, 5% cream, has shown to have promise in a variety of cutaneous oncological conditions. Unfortunately, however, the dermatologic work on imiquimod has mainly been in the form of case reports or small open trials. Very few double-blind cross-over trials have been done for the same. Hence, there is a need for larger multicentric studies which would be of more help for clinicians in successfully employing the immune response modifier activity of imiquimod for other off-label applications in dermatology.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
References
- 1.Sauder DN. Immunomodulatory and pharmacologic properties of imiquimod. J Am Acad Dermatol. 2000;43:S6–11. doi: 10.1067/mjd.2000.107808. [DOI] [PubMed] [Google Scholar]
- 2.Navi D, Huntley A. Imiquimod 5 percent cream and the treatment of cutaneous malignancy. Dermatol Online J. 2004;10:4. [PubMed] [Google Scholar]
- 3.Leverkus M. Imiquimod: Unexpected killer. J Invest Dermatol. 2004;122:XV–XVI. doi: 10.1111/j.0022-202X.2004.22537.x. [DOI] [PubMed] [Google Scholar]
- 4.Beutner KR, Geisse JK, Helman D, Fox TL, Ginkel A, Owens ML. Therapeutic response of basal cell carcinoma to the immune response modifier imiquimod 5% cream. J Am Acad Dermatol. 1999;41:1002–7. doi: 10.1016/s0190-9622(99)70261-6. [DOI] [PubMed] [Google Scholar]
- 5.Jobanputra KS, Rajpal AV, Nagpur NG. Imiquimod. Indian J Dermatol Venereol Leprol. 2006;72:466–9. doi: 10.4103/0378-6323.29352. [DOI] [PubMed] [Google Scholar]
- 6.Gupta AK, Cooper EA, Abramovits W. Zyclara (imiquimod) cream, 3.75% Skinmed. 2010;8:227–9. [PubMed] [Google Scholar]
- 7.Dodds A, Chia A, Shumack S. Actinic keratosis: Rationale and management. Dermatol Ther (Heidelb) 2014;4:11–31. doi: 10.1007/s13555-014-0049-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ulrich C, Bichel J, Euvrard S, Guidi B, Proby CM, van de Kerkhof PC, et al. Topical immunomodulation under systemic immunosuppression: Results of a multicentre, randomized, placebo-controlled safety and efficacy study of imiquimod 5% cream for the treatment of actinic keratoses in kidney, heart, and liver transplant patients. Br J Dermatol. 2007;157(Suppl 2):25–31. doi: 10.1111/j.1365-2133.2007.08269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Salasche SJ, Levine N, Morrison L. Cycle therapy of actinic keratoses of the face and scalp with 5% topical imiquimod cream: An open-label trial. J Am Acad Dermatol. 2002;47:571–7. doi: 10.1067/mjd.2002.126257. [DOI] [PubMed] [Google Scholar]
- 10.Goldenberg G, Linkner RV, Singer G, Frankel A. An investigator-initiated study to assess the safety and efficacy of imiquimod 3.75% cream when used after cryotherapy in the treatment of hypertrophic actinic keratoses on dorsal hands and forearms. J Clin Aesthet Dermatol. 2013;6:36–43. [PMC free article] [PubMed] [Google Scholar]
- 11.Shaffelburg M. Treatment of actinic keratoses with sequential use of photodynamic therapy; and imiquimod 5% cream. J Drugs Dermatol. 2009;8:35–9. [PubMed] [Google Scholar]
- 12.Wolff F, Loipetzberger A, Gruber W, Esterbauer H, Aberger F, Frischauf AM. Imiquimod directly inhibits Hedgehog signalling by stimulating adenosine receptor/protein kinase A-mediated GLI phosphorylation. Oncogene. 2013;32:5574–81. doi: 10.1038/onc.2013.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gruber W, Frischauf AM, Aberger F. An old friend with new skills: Imiquimod as novel inhibitor of Hedgehog signaling in basal cell carcinoma. Oncoscience. 2014;1:567–73. doi: 10.18632/oncoscience.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mondal BC, Mukherjee T, Mandal L, Evans CJ, Sinenko SA, Martinez-Agosto JA, et al. Interaction between differentiating cell- and niche-derived signals in hematopoietic progenitor maintenance. Cell. 2011;147:1589–600. doi: 10.1016/j.cell.2011.11.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roozeboom MH, Arits AH, Nelemans PJ, Kelleners-Smeets NW. Overall treatment success after treatment of primary superficial basal cell carcinoma: A systematic review and meta-analysis of randomized and nonrandomized trials. Br J Dermatol. 2012;167:733–56. doi: 10.1111/j.1365-2133.2012.11061.x. [DOI] [PubMed] [Google Scholar]
- 16.Lacarrubba F, Potenza MC, Gurgone S, Micali G. Successful treatment and management of large superficial basal cell carcinomas with topical imiquimod 5% cream: A case series and review. J Dermatolog Treat. 2011;22:353–8. doi: 10.3109/09546634.2010.548503. [DOI] [PubMed] [Google Scholar]
- 17.Yang JQ, Chen XY, Engle MY, Wang JY. Multiple facial basal cell carcinomas in xeroderma pigmentosum treated with topical imiquimod 5% cream. [Last accessed on Apr 25];Dermatol Ther. 2015 doi: 10.1111/dth.12217. [DOI] [PubMed] [Google Scholar]
- 18.Micali G, Lacarrubba F, Nasca MR, De Pasquale R. The use of imiquimod 5% cream for the treatment of basal cell carcinoma as observed in Gorlin's syndrome. Clin Exp Dermatol. 2003;28(Suppl 1):19–23. doi: 10.1046/j.1365-2230.28.s1.7.x. [DOI] [PubMed] [Google Scholar]
- 19.Clark CM, Furniss M, Mackay-Wiggan JM. Basal cell carcinoma: An evidence-based treatment update. Am J Clin Dermatol. 2014;15:197–216. doi: 10.1007/s40257-014-0070-z. [DOI] [PubMed] [Google Scholar]
- 20.Bath-Hextall F, Ozolins M, Armstrong SJ, Colver GB, Perkins W, Miller PS, et al. Surgical excision versus imiquimod 5% cream for nodular and superficial basal-cell carcinoma (SINS): A multicentre, non-inferiority, randomised controlled trial. Lancet Oncol. 2014;15:96–105. doi: 10.1016/S1470-2045(13)70530-8. [DOI] [PubMed] [Google Scholar]
- 21.Tristram A, Hurt CN, Madden T, Powell N, Man S, Hibbitts S, et al. Activity, safety, and feasibility of cidofovir and imiquimod for treatment of vulval intraepithelial neoplasia (RT3 VIN): A multicentre, open-label, randomised, phase 2 trial. Lancet Oncol. 2014;15:1361–8. doi: 10.1016/S1470-2045(14)70456-5. [DOI] [PubMed] [Google Scholar]
- 22.Kim JM, Lee HJ, Kim SH, Kim HS, Ko HC, Kim BS, et al. Efficacy of 5% imiquimod cream on vulvar intraepithelial neoplasia in Korea: Pilot study. Ann Dermatol. 2015;27:66–70. doi: 10.5021/ad.2015.27.1.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lacarrubba F, Nasca MR, Micali G. Advances in the use of topical imiquimod to treat dermatologic disorders. Ther Clin Risk Manag. 2008;4:87–97. doi: 10.2147/tcrm.s1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Frega A, Sesti F, Sopracordevole F, Biamonti A, Scirpa P, Milazzo GN, et al. Imiquimod 5% cream versus cold knife excision for treatment of VIN 2/3: A five-year follow-up. Eur Rev Med Pharmacol Sci. 2013;17:936–40. [PubMed] [Google Scholar]
- 25.Fox PA, Nathan M, Francis N, Singh N, Weir J, Dixon G, et al. A double-blind, randomized controlled trial of the use of imiquimod cream for the treatment of anal canal high-grade anal intraepithelial neoplasia in HIV-positive MSM on HAART, with long-term follow-up data including the use of open-label imiquimod. AIDS. 2010;24:2331–5. doi: 10.1097/QAD.0b013e32833d466c. [DOI] [PubMed] [Google Scholar]
- 26.Sohn KC, Li ZJ, Choi DK, Zhang T, Lim JW, Chang IK, et al. Imiquimod induces apoptosis of squamous cell carcinoma (SCC) cells via regulation of A20. PLoS One. 2014;9:e95337. doi: 10.1371/journal.pone.0095337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Erickson C, Miller SJ. Treatment options in melanoma in situ: Topical and radiation therapy, excision and Mohs surgery. Int J Dermatol. 2010;49:482–91. doi: 10.1111/j.1365-4632.2010.04423.x. [DOI] [PubMed] [Google Scholar]
- 28.Ly L, Kelly JW, O’Keefe R, Sutton T, Dowling JP, Swain S, et al. Efficacy of imiquimod cream, 5%, for lentigo maligna after complete excision: A study of 43 patients. Arch Dermatol. 2011;147:1191–5. doi: 10.1001/archdermatol.2011.260. [DOI] [PubMed] [Google Scholar]
- 29.Powell AM, Robson AM, Russell-Jones R, Barlow RJ. Imiquimod and lentigo maligna: A search for prognostic features in a clinicopathological study with long-term follow-up. Br J Dermatol. 2009;160:994–8. doi: 10.1111/j.1365-2133.2009.09032.x. [DOI] [PubMed] [Google Scholar]
- 30.Holcmann M, Drobits B, Sibilia M. How imiquimod licenses plasmacytoid dendritic cells to kill tumors. Oncoimmunology. 2012;1:1661–3. doi: 10.4161/onci.22033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Aspord C, Tramcourt L, Leloup C, Molens JP, Leccia MT, Charles J, et al. Imiquimod inhibits melanoma development by promoting pDC cytotoxic functions and impeding tumor vascularization. J Invest Dermatol. 2014;134:2551–61. doi: 10.1038/jid.2014.194. [DOI] [PubMed] [Google Scholar]
- 32.Fernandez-Guarino M. Emerging treatment options for early mycosis fungoides. Clin Cosmet Investig Dermatol. 2013;6:61–9. doi: 10.2147/CCID.S27482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Luyten A, Sörgel P, Clad A, Gieseking F, Maass-Poppenhusen K, Lellé RJ, et al. Treatment of extramammary Paget disease of the vulva with imiquimod: A retrospective, multicenter study by the German Colposcopy Network. J Am Acad Dermatol. 2014;70:644–50. doi: 10.1016/j.jaad.2013.12.008. [DOI] [PubMed] [Google Scholar]
- 34.Sanderson P, Innamaa A, Palmer J, Tidy J. Imiquimod therapy for extramammary Paget's disease of the vulva: A viable non-surgical alternative. J Obstet Gynaecol. 2013;33:479–83. doi: 10.3109/01443615.2013.790348. [DOI] [PubMed] [Google Scholar]
- 35.Toledo F, Silvestre JF, Cuesta L, Ballester I, Latorre N, Monteagudo A. Sequential use with imiquimod and surgery in extramammary Paget's disease. Dermatol Ther. 2012;25:82–5. doi: 10.1111/j.1529-8019.2012.01428.x. [DOI] [PubMed] [Google Scholar]
- 36.Hu L, Huang HZ, Li X, Lin XX, Li W. Open-label nonrandomized left-right comparison of imiquimod 5% ointment and timolol maleate 0.5% eye drops in the treatment of proliferating superficial infantile hemangioma. Dermatology. 2015;230:150–5. doi: 10.1159/000369164. [DOI] [PubMed] [Google Scholar]
- 37.Schrama D, Ugurel S, Becker JC. Merkel cell carcinoma: Recent insights and new treatment options. Curr Opin Oncol. 2012;24:141–9. doi: 10.1097/CCO.0b013e32834fc9fe. [DOI] [PubMed] [Google Scholar]
- 38.Balducci M, De Bari B, Manfrida S, D’Agostino GR, Valentini V. Treatment of Merkel cell carcinoma with radiotherapy and imiquimod (Aldara): A case report. Tumori. 2010;96:508–11. doi: 10.1177/030089161009600324. [DOI] [PubMed] [Google Scholar]
- 39.Gündüz K, Günay U, Inanir I, Gençoglan G, Temiz P. Efficacy of 5% imiquimod cream in a patient with classic Kaposi sarcoma. J Dermatol Case Rep. 2012;6:52–3. doi: 10.3315/jdcr.2012.1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Goiriz R, Ríos-Buceta L, De Arriba AG, Aragüés M, García-Diez A. Treatment of classic Kaposi's sarcoma with topical imiquimod. Dermatol Surg. 2009;35:147–9. doi: 10.1111/j.1524-4725.2008.34397.x. [DOI] [PubMed] [Google Scholar]
- 41.Bernardini B, Faggion D, Calabró L, Oro E, Alaibac M. Imiquimod for the treatment of classical Kaposi's sarcoma. Acta Derm Venereol. 2010;90:417–8. doi: 10.2340/00015555-0850. [DOI] [PubMed] [Google Scholar]
- 42.Kohrt H. Breast cancer treatment with imiquimod: Applying an old lotion to a new disease. Clin Cancer Res. 2012;18:6571–3. doi: 10.1158/1078-0432.CCR-12-3138. [DOI] [PubMed] [Google Scholar]
- 43.Adams S, Kozhaya L, Martiniuk F, Meng TC, Chiriboga L, Liebes L, et al. Topical TLR7 agonist imiquimod can induce immune-mediated rejection of skin metastases in patients with breast cancer. Clin Cancer Res. 2012;18:6748–57. doi: 10.1158/1078-0432.CCR-12-1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dewan MZ, Vanpouille-Box C, Kawashima N, DiNapoli S, Babb JS, Formenti SC, et al. Synergy of topical toll-like receptor 7 agonist with radiation and low-dose cyclophosphamide in a mouse model of cutaneous breast cancer. Clin Cancer Res. 2012;18:6668–78. doi: 10.1158/1078-0432.CCR-12-0984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Henriques L, Palumbo M, Guay MP, Bahoric B, Basik M, Kavan P, et al. Imiquimod in the treatment of breast cancer skin metastasis. J Clin Oncol. 2014;32:e22–5. doi: 10.1200/JCO.2012.46.4883. [DOI] [PubMed] [Google Scholar]


