Abstract
Background
Recently it was suggested that high myopia macular holes (HMMH) and macular holes accompanied by retinal detachment occur in the advanced stages of myopia traction maculopathy (MTM), while macular retinoschisis, shallow retinal detachment without holes, and lamellar macular holes occur in the early stages of MTM. Complete vitreous cortex removal associated with internal limiting membrane peeling is now widely used to treat HMMH. However, it remains uncertain at what HMMH stage patients would benefit most from surgical intervention. Our study was aimed to evaluate the postoperative anatomical changes and functional outcomes of high myopia macular holes (HMMH).
Methods
Patients were retrospectively collected between March 2009 and August 2011. Before and 1st, 3rd, and 9th month after 23G pars plana vitrectomy, all patients underwent a complete ophthalmologic examination, spectral domain optical coherence tomography (SD-OCT) and MP-1. At each follow-up, best-corrected visual acuity (BCVA), photoreceptor inner and outer segments (IS/OS) defects, and retinal sensitivity (RS) were investigated. According to different preoperative macular hole morphologies, patients were divided into three groups: Group 1, macular hole with epiretinal membrane (ERM) traction and macular retinoschisis; Group 2, full-thickness macular hole (FTMH); Group 3, FTMH with subretinal fluid.
Results
43 eyes from 43 patients met the inclusion criteria. The mean age was 60 years. BCVA and RS were significantly improved after vitrectomy; the mean IS/OS defect was significantly reduced. At 9 postoperative months, 11 of 43 (25.6 %) eyes achieved IS/OS junction integrity; 9 of these 11 (81.8 %) eyes belonged to Group 1, 2 (18.2 %) belonged to Group 2.
Conclusions
Pars plana vitrectomy combined with ILM peeling and gas tamponade results in limited functional outcomes in patients with HMMH. The appearance of subretinal fluid indicates a worse prognosis for surgical intervention.
Background
Retinopathy in pathological myopia is a major cause of visual impairment, and long axial lengths and posterior staphyloma eventually lead to myopia traction maculopathy (MTM) [1]. The term MTM was first used in 2004 to describe a series of posterior pole pathologies in cases of high myopia, such as macular retinoschisis, shallow retinal detachment without retinal holes, lamellar macular holes, and macular holes, with or without retinal detachment. In 1999, Takano and Kishi speculated that the formation of high myopia macular holes (HMMH) resulted from macular retinoschisis or shallow retinal detachment without holes [2]. Panozzo and Mercanti [3] supported this notion and suggested that HMMH and macular holes accompanied by retinal detachment occur in the advanced stages of MTM, while macular retinoschisis, shallow retinal detachment without holes, and lamellar macular holes occur in the early stages of MTM. This hypothesis has been confirmed by several other groups [4–8].
Complete vitreous cortex removal associated with internal limiting membrane peeling is now widely used to treat HMMH. However, it remains uncertain at what HMMH stage patients would benefit most from surgical intervention.
In this study, we used spectral domain optical coherence tomography (SD-OCT) and microperimetry pre- and postoperatively in patients diagnosed with HMMH to observe and analyze the retinal microstructure and functional recovery.
Materials and methods
Data collection
Patients with a diagnosis of HMMH were retrospectively collected from the Department of Ophthalmology at Shanghai First People’s Hospital, Shanghai Jiaotong University between March 2009 and August 2011. All patients underwent a standard ophthalmologic examination preoperatively and at 1 month, 3 months, and 9 months after pars plana vitrectomy, including volume OCT scanning with an SD-OCT (Spectralis, Heidelberg Engineering, Heidelberg, Germany) and the MP-1 microperimeter (Nidek Technologies, Padua, Italy). The imaging protocols used are described below. Patient information, such as age, sex, lens status, axial length, history of ophthalmic diseases or surgeries, and ophthalmic diagnoses, was also collected. The following inclusion criteria were applied: subjective visual symptoms; high myopia (> − 6.00 diopters), with an axial length >26.00 mm; and a full-thickness macular hole (FTMH) as confirmed and documented by OCT examination. Patients with diabetes, hypertension, eye surgery within 1 year, one or several peripheral retinal holes or retinal detachment were excluded. Best-corrected visual acuity (BCVA) was measured using E-VA charts, and the results were converted to logMAR units. Approval for data collection and analysis was obtained from the institutional review board of the Shanghai First People’s Hospital. Written consent was obtained from all patients. The research adhered to the tenets set forth in the Declaration of Helsinki.
SD-OCT
All OCT scans were performed with the Spectralis OCT (Heidelberg Engineering, Germany). The scan protocol consisted of 19-line scans centered on the fovea covering 30° radial, with a line spacing of 350 μm between the scans. Active eye tracking and line averaging of 10 scans per line (ART 10) were used. The IS/OS defect was measured by OCT. Only gradable records were used in the study. Two graders (Q.S., Y.F.) independently evaluated each OCT image set (Fig. 1).
Fig. 1.
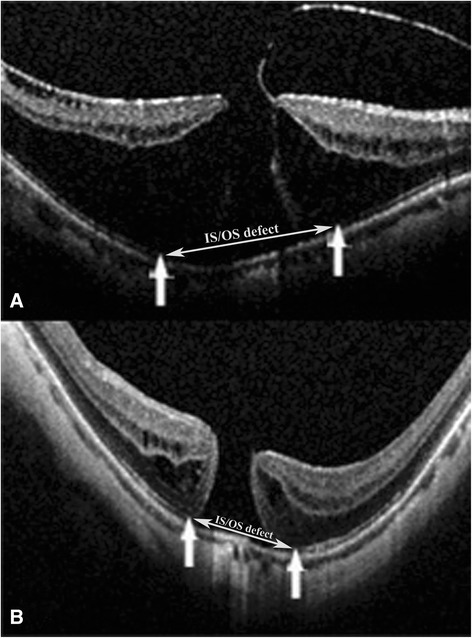
a and b: Measurements of foveal microstructure on SD-OCT images. The distance between two one-way arrows was measured as IS/OS defect (see two-way arrow). a is a preoperative image from Group 1, which showed a macular hole with ERM traction, macular retinoschisis; b is FTMH image before surgery in Group 2
Microperimetry
The retinal sensitivity was measured using the MP1 (Nidek technology, Padua, Italy).
The eye-tracking system corrected eye movements automatically and obtained images with an infrared camera. The test area comprised the macular 10° and 40 stimulus locations within this field. A white background, with a red single cross as a fixation target and Goldmann III white spot stimuli, were used. The luminance range was 0–20 dB. The maximum brightness was 127 cd/m [2], the minimum brightness was 1.27 cd/m [2], and the stimulus duration was 200 ms. A staircase strategy of the 4-2-1 pattern was used. The retinal sensitivity threshold map was automatically registered to the color fundus photo, and the overall average retinal sensitivity was calculated (Fig. 2).
Fig. 2.
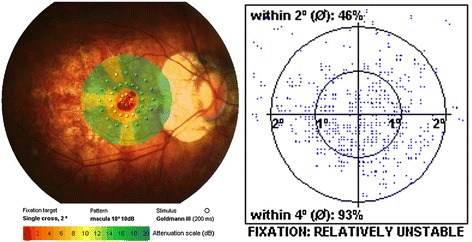
A macular retinal sensitivity map overlaid a fundus color photo which was measured by MP1. The test area was macular 10 degrees. 40 stimulate points were recorded. The luminance range was 0–20 dB. The maximum brightness was 127 cd/m2, minimum brightness was 1.27 cd/m2, and stimulus duration was 200 ms. A staircase strategy of 4-2-1 pattern was used. The average of 40 points retinal sensitivity was calculated
Groupings
Based on the OCT images, the patients were divided into three groups: [9, 10] Group 1, macular hole with epiretinal membrane (ERM) traction, macular retinoschisis; Group 2, FTMH without ERM and subretinal fluid; and Group 3, FTMH with subretinal fluid, with or without ERM (Fig. 3).
Fig. 3.
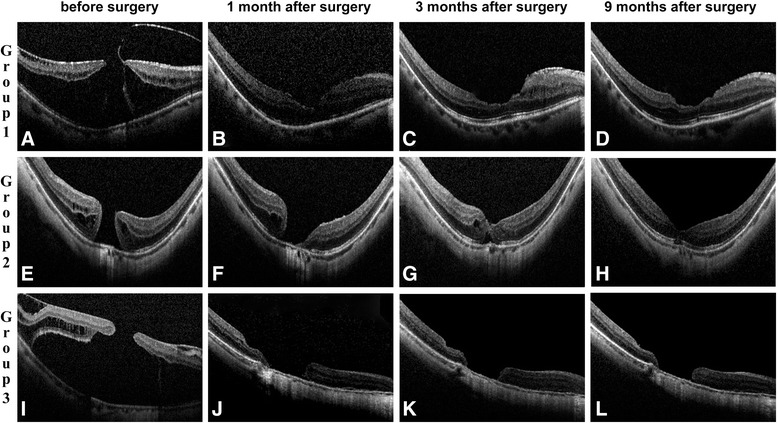
a-l: Macular microstructures on SD-OCT B-scans before and 1 month, 3 months, 9 months after surgery. a-d: OCT B-scans from the right eye of a 58 year-old woman in Group 1 before and 1 month, 3 months, 9 months after surgery. The IS/OS defect before and 1 month, 3 months, 9 months after surgery were 1717, 1364, 0, 0 μm, the BCVA were 0.70, 0.52, 0.30, 0.22 logMAR, and the RS were 15.7, 16.8, 17.3, 18.1 dB. e-h: OCT B-scans from the left eye of a 55 year-old woman in Group 2 before and 1 month, 3 months, 9 months after surgery. The IS/OS defect before and 1 month, 3 months, 9 months after surgery were 1329, 1129, 871, 94 μm, the BCVA were 1, 0.52, 0.30, 0.30 logMAR, and the RS were 10.8, 12.5, 13.5, 15.1 dB. i-l: OCT B-scans from the right eye of a 54 year-old woman in Group 3 before and 1 month, 3 months, 9 months after surgery. The IS/OS defect before and 1 month, 3 months, 9 months after surgery were 4011, 2635, 2363, 2388 μm, the BCVA were 1.52, 1, 1, 1 logMAR, and the RS were 10.4, 12.6, 12.9, 12.7 dB
Surgical approach
All patients underwent transconjunctival 23G pars plana vitrectomy. The procedures for 7 eyes were combined with phacoemulsification and intraocular lens implantation in the same surgery. All surgeries were performed by a single surgeon (Y.F.). To stain the internal limiting membrane (ILM), 0.05 % indocyanine green (ICG) was applied. A 15 % perfluoropropane (C3F8) gas tamponade was used at the completion of vitrectomy. The patients were required to maintain a prone position for 7 to 15 days. Eyes with silicone oil tamponade were not included.
Statistical methods
Data were analyzed using frequency and descriptive statistics. Shapiro-Wilk test was used to assess the normal distribution of the quantitative parameters in this study. To compare differences in pre- and postoperative IS/OS defect, BCVA and RS in each group, Student paired t-test was used. Multiple linear regression analysis was used to evaluate correlation between IS/OS defect before surgery and BCVA, RS before and after surgery. Statistical analysis was performed using commercially available SPSS software (Version 19.0, SPSS Inc., Chicago, IL, USA). A two-sided p value of <0.05 was considered to be statistically significant.
Results
Demographic characteristics
A total of 48 eyes from 48 patients met the inclusion criteria. Because 5 eyes were lost to follow-up, a total of 43 eyes were included in this study. At month 1, 43 eyes were included. No eyes underwent a second surgery. Twelve eyes were pseudophakic before entering the study, and 7 eyes underwent combined procedures with phacoemulsification and intraocular lens implantation at the initial surgery. The between-group differences regarding age, eye, gender, axial length and cataract surgery were not significant (Table 1). The preoperative parameters regarding age, eye, gender, axial length and cataract surgery had no significant effect in the surgical outcomes (Table 3).
Table 1.
Comparison of Demographic Characteristics of Each Group
| Group1 | Group2 | Group3 | p value | |
|---|---|---|---|---|
| Number of eyes | 17 | 12 | 14 | -- |
| Age (mean ± SD), years | 60.24 ± 6.04 | 59.33 ± 7.66 | 60.29 ± 9.24 | 0.72* |
| Eye (right) | 8 | 5 | 10 | 0.25a |
| Gender (women) | 12 | 11 | 10 | 0.35a |
| Axial length, mm | 28.03 ± 0.85 | 27.95 ± 1.11 | 28.30 ± 1.30 | 0.85* |
| Cataract surgery | ||||
| Before the initial surgery | 5 | 3 | 4 | 0.96a |
| At the initial surgery | 3 | 2 | 2 | 0.95a |
| Pseudophakic eyes | ||||
| 1 month after surgery | 8(47 %) | 5(42 %) | 6(43 %) | 0.33a |
| 3 months after surgery | 8(47 %) | 6(50 %) | 9(64 %) | 0.27a |
| 9 months after surgery | 12(71 %) | 8(67 %) | 11(79 %) | 0.24a |
| Preoperative parameters | ||||
| IS/OS defect, μm | 986.16 ± 823.47 | 2225.49 ± 758.38 | 4689.08 ± 978.69 | <0.0001* |
| BCVA, LogMAR | 0.71 ± 0.33 | 0.97 ± 0.21 | 1.65 ± 0.44 | <0.0001* |
| RS, dB | 16.27 ± 1.17 | 13.78 ± 2.67 | 9.07 ± 2.07 | <0.0001* |
IS/OS photoreceptor inner segment and outer segment, BCVA best-corrected visual acuity, logMAR logarithm of minimal angle of resolution, RS retinal sensitivity. P value represents the difference between groups. P < 0.05 was considered statistically significant. *Kruskal-Wallis test. aFisher’s exact probability test
Table 3.
Regression Analysis Between IS/OS Defect Before Surgery and BCVA, RS Before and After Surgery
| Outcomes Parameters | BCVA (logMAR) before and after surgery | Retinal Sensitivity (dB) before and after surgery | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Before | 1 month | 3 months | 9 months | Before | 1 month | 3 months | 9 months | |||||||||
| r, p value | r, p value* | r, p value* | r, p value* | r, p value* | r, p value* | r, p value* | r, p value* | |||||||||
| IS/OS defect (μm) before surgery | 0.89 | <0.0001 | 0.74 | <0.0001 | 0.79 | <0.0001 | 0.73 | <0.0001 | 0.70 | <0.0001 | 0.48 | <0.0001 | 0.44 | <0.0001 | 0.43 | <0.0001 |
| Age | 0.76 | 0.28 | 0.88 | 0.77 | 0.85 | 0.85 | 0.76 | 0.69 | ||||||||
| Gender | 0.82 | 0.49 | 0.23 | 0.25 | 0.35 | 0.18 | 0.11 | 0.13 | ||||||||
| Eye | 0.11 | 0.95 | 0.56 | 0.26 | 0.53 | 0.79 | 0.52 | 0.63 | ||||||||
| Cataract surgery | 0.33 | 0.94 | 0.38 | 0.49 | 0.23 | 0.43 | 0.46 | 0.38 | ||||||||
| Axial length | 0.56 | 0.21 | 0.42 | 0.82 | 0.35 | 0.81 | 0.62 | 0.52 | ||||||||
BCVA best-corrected visual acuity, IS/OS photoreceptor inner segment and outer segment, logMAR logarithm of minimal angle of resolution, RS retinal sensitivity. *Multiple linear regression analysis was used to evaluate correlation between IS/OS defect before surgery and BCVA, RS before and after surgery, adjusted with age, gender, eye, cataract surgery and axial length. r value represents adjusted R square. P < 0.05 was considered statistically significant
Anatomical results
The mean IS/OS defect of all patients measured by OCT was 2537.62 ± 279.75 μm before surgery and 1120.11 ± 167.60 μm at 9 months after surgery (p < 0.0001). Moreover, the mean IS/OS defect after surgery decreased significantly from follow-up to follow-up in each group. The mean IS/OS defect of Group 1 before surgery was 986.16 ± 823.47 μm, and this value decreased to 318.34 ± 481.72 μm at 9 months after surgery (p < 0.0001). In Group 2, the IS/OS defects before surgery and 9 months after surgery were 2225.49 ± 758.38 μm and 811.76 ± 465.70 μm (p < 0.0001), respectively. The means for Group 3 were 4689.08 ± 978.69 μm before surgery and 2357.98 ± 924.54 μm 9 months after surgery (p < 0.0001) (Table 2).
Table 2.
IS/OS defect, BCVA and RS Outcomes of 3 Groups Before and After Surgery
| Outcomes Parameter | Before surgery | 1 month after surgery | 3 months after surgery | 9 months after surgery | |||
|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | t, p Value* | Mean ± SD | t, p Value* | Mean ± SD | t, p Value* | |
| Group1 (17 eyes) | |||||||
| IS/OS defect (μm) | 986.16 ± 823.47 | 593.08 ± 697.79 | 5.02, < 0.0001 | 415.23 ± 561.58 | 5.25, < 0.0001 | 318.34 ± 481.72 | 5.08, < 0.0001 |
| BCVA (logMAR) | 0.71 ± 0.33 | 0.49 ± 0.25 | 4.41, 0.0004 | 0.45 ± 0.25 | 5.47, < 0.0001 | 0.43 ± 0.24 | 5.76, < 0.0001 |
| RS (dB) | 16.27 ± 1.17 | 17.23 ± 1.09 | 8.35, < 0.0001 | 17.47 ± 1.12 | 8.68, < 0.0001 | 17.62 ± 1.17 | 8.95, < 0.0001 |
| Group2 (12 eyes) | |||||||
| IS/OS defect (μm) | 2225.49 ± 758.38 | 1484.31 ± 423.94 | 5.99, < 0.0001 | 1097.06 ± 450.65 | 9.56, < 0.0001 | 811.76 ± 465.70 | 10.83, < 0.0001 |
| BCVA (LogMAR) | 0.97 ± 0.21 | 0.85 ± 0.16 | 2.36, 0.38 | 0.77 ± 0.23 | 5.87, 0.0001 | 0.71 ± 0.19 | 5.33, 0.0002 |
| RS (dB) | 13.78 ± 2.67 | 15.08 ± 2.32 | 5.95, < 0.0001 | 15.42 ± 2.19 | 6.17, < 0.0001 | 15.51 ± 2.27 | 6.34, < 0.0001 |
| Group3 (14 eyes) | |||||||
| IS/OS defect (μm) | 4689.08 ± 978.69 | 3257.98 ± 892.75 | 4.64, 0.0005 | 2671.43 ± 985.54 | 6.15, < 0.0001 | 2357.98 ± 924.54 | 7.07, < 0.0001 |
| BCVA (LogMAR) | 1.65 ± 0.44 | 1.29 ± 0.39 | 2.75, 0. 17 | 1.05 ± 0.23 | 5.10, 0.0002 | 0.91 ± 0.20 | 6.57, < 0.0001 |
| RS (dB) | 9.07 ± 2.07 | 11.59 ± 2.45 | 3.96, 0.002 | 12.46 ± 2.45 | 5.21, 0.0002 | 12.69 ± 2.46 | 5.47, 0.0001 |
BCVA best-corrected visual acuity, IS/OS photoreceptor inner segment and outer segment, logMAR logarithm of minimal angle of resolution, RS retinal sensitivity. *Student paired t-test; p value represents the difference between after and before surgery. P < 0.05 was considered statistically significant
Functional results
The mean logMAR BCVA of all patients was 1.09 ± 0.53 before surgery and 0.67 ± 0.29 at 9 months after surgery (p < 0.0001). Moreover, the mean BCVA improved significantly after surgery at all follow-ups in each group. The mean BVCA in Group 1 was 0.71 ± 0.33 before surgery and 0.43 ± 0.24 at 9 months after surgery (p < 0.0001). Before surgery, the mean BCVA of Group 2 was 0.97 ± 0.21, whereas this value 9 months after surgery was 0.71 ± 0.19 (p = 0.0002). In Group 3, the mean BCVA values before surgery and 9 months after surgery were 1.65 ± 0.44 and 0.91 ± 0.20 (p < 0.0001), respectively.
The mean RS of all patients was 13.23 ± 3.65 before surgery and 15.43 ± 2.86 at 9 months after surgery (p < 0.0001). The mean RS of Group 1 was 16.27 ± 1.17 dB before surgery and 17.62 ± 1.17 dB at 9 months after surgery (p < 0.0001). Before surgery, the mean RS of Group 2 was 13.78 ± 2.67 dB, whereas at 9 months after surgery, this value was 15.51 ± 2.27 (p < 0.0001). In Group 3, before surgery and 9 months after surgery, the mean RS values were 9.07 ± 2.07 and 12.69 ± 2.46 (p < 0.0001), respectively, and this difference was statistically significant (Table 2).
Closure Rates
At 9 months after surgery, 11 of 43 (25.6 %) eyes achieved IS/OS junction integrity; 9 (81.8 %) of these 11 eyes belonged to Group 1, 2 (18.2 %) belonged to Group 2. The closure rates were 52.9 % (9 of 17 eyes) in Group 1, 16.7 % (2 of 12 eyes) in Group 2 and 0 in Group 3.
Correlation between preoperative anatomy and postoperative function
The preoperative IS/OS defect was significantly correlated with the postoperative BCVA and retinal sensitivity at 1 month after surgery (r = 0.71, p < 0.0001). The same result was also observed at 3 and 9 months after surgery (Table 3).
Discussion
OCT has recently made it possible to explore changes in ocular layers as axial progresses and the globe is stretched. These findings consist of dehiscence of retinal layers known as retinoschisis, tractional ILM detachment, macular holes (lamellar and full thickness), posterior retinal detachment and choroidal neovascular membranes [10]. According to these OCT findings, patients in this study were separated into 3 groups.
This study showed that HMMH eyes without subretinal fluid (Groups 1 and 2) obtained better postoperative anatomical and functional outcomes than eyes with subretinal fluid (Group 3). In addition, the HMMH patients with ERM traction, retinoschisis (Group 1) regained more visual function than patients with full-thickness macular holes (Group 2). This result suggests that subretinal fluid represents an advanced damage stage. Other research groups have also reported this observation [4–8]. In our study, Group 1 through 3 approximated HMMH at varying severities stage in its natural course. Indeed, preoperative IS/OS defects, BCVA and RS all differed significantly among the three groups, providing clinical significance for the grouping of patients performed in our study.
The integrity of inner and outer segments of photoreceptors (IS/OS) is closely related to visual recovery after successful MH closure surgery [11–15]. Visual acuity is generally used as a gold standard to indicate visual function, although it represents only one aspect. In this study, microperimetry was applied to quantify foveal and perifoveal retinal sensitivity and correlate these results to the microstructural findings in HMMH [16, 17]. Specifically, we used the IS/OS defect as an anatomical parameter and BCVA and retinal sensitivity (RS) as functional parameters to evaluate the relationship between microstructure and function in the HMMH eyes that underwent surgery.
We found that in all 3 groups, the IS/OS defect decreased significantly as time progressed, indicating a potential regeneration of photoreceptors. Similarly, BCVA and RS measurements gradually reached significant improvement after surgery. Interestingly, the preoperative IS/OS defect was significantly correlated with both the preoperative and postoperative BCVA and RS values (Table 3). Although great care must be taken with small patient cohorts, our study revealed the potential prognostic value of the size of the IS/OS defect in conjunction with other known factors (e.g., retinal or RPE atrophy) and the preoperative diameters of macular holes.
Furthermore, 52.9 % (9 of 17 eyes) eyes in Group 1 approached postoperative closure, only 16.7 % (2 of 12 eyes) in Group 2 and 0 in Group 3 at 9 months after surgery. The minimum preoperative diameter of IS/OS defect in each group was 305.88 μm in Group 1, 1258.82 μm in Group 2, and 2317.64 μm in Group 3. As this parameter has showed a potential prognostic value, this result explained the significant differences in postoperative closure rates between groups.
Subretinal fluid is a generally regarded as a negatively prognostic complication of HMMH, because, in theory, chronic fluid may aggravate damage to photoreceptors. Assuming that subretinal fluid is a severity-dependent complication in the evolution of HMMH, it is even more important to perform effective surgery at a less damage stage for optimal postoperative functional recovery and restoration. Our study suggests that the appearance of ERM traction and consequent retinoschisis without subretinal fluid in HMMH, indicates a better prognosis for surgical intervention. Although some patients may show no subjective symptoms for years at this stage [18–20], visual acuity impairment should indicate surgery in the affected eye.
Based on its low complication rate, transconjunctival 23-gauge (23G) pars plana vitrectomy, as performed in our cases, was an effective treatment for HMMH. Nonetheless, our study lacks long-term results exceeding 9 months. Indeed, vitrectomy in myopic cases is associated with a postoperative risk for retinal detachment and subsequent visual loss [21], which we fortunately did not observe within these 9 months. Generally, MH closure is less frequently observed following vitrectomy in HMMH compared to emmetropic cases [22]. These less favorable results may be explained by the presence of persistent macular traction because of continued elongation and staphyloma formation in pathologic myopia. Based on this hypothesis, other groups have suggested that an additional procedure, such as an episcleral macular buckle, may be useful to counteract the posterior traction [21, 23]. Although a variety of procedures are available for HMMH, there is still no unified standard treatment method. Therefore, additional longer-term studies are required.
ICG toxicity and damage to the retina has been reported in in vitro and in vivo studies, and following macular surgery. Toxic effects can occur to retinal glial cells, to the nerve fiber layer, to retinal ganglion cells, and to the optic nerve. ICG at concentrations higher than 1.25 % or application of the dye in air are very likely causing retinal damage [24]. In this study, a concentration of was applied in every case with a less than 30 seconds dyeing time to minimize the ICG toxicity as far as possible.
Our study has a number of limitations. First, none of the eyes in Group 3 and very few in Group 2 closed, whereas the postoperative BCVA were all significantly improved. This may result from the underestimation of the preoperative visual acuity due to cataract. The improved paracentral vision thanks to the regeneration of IS/OS structure as time progressed could also be a part of the explanation. Second, ICG toxicity and damage to the retina has been reported in in vitro and in vivo studies, and following macular surgery. Toxic effects can occur to retinal glial cells, to the nerve fiber layer, to retinal ganglion cells, and to the optic nerve. ICG at concentrations higher than 1.25 % or application of the dye in air are very likely causing retinal damage [24]. In this study, a concentration of was applied in every case with a less than 30 seconds dyeing time to minimize the ICG toxicity as far as possible. Third, this study lacks long-term results exceeding 9 months. Further prospective, long-term study would be needed for detection of further anatomical and functional changes.
Conclusions
In conclusion, pars plana vitrectomy combined with ILM peeling and gas tamponade results in limited functional outcomes in patients with HMMH. In HMMH, the appearance of subretinal fluid indicates a worse prognosis for surgical intervention.
Abbreviations
- BCVA
best-corrected visual acuity
- HMMH
high myopia macular hole
- ICG
Indocyanine green
- ILM
internal limiting membrane
- IS/OS
photoreceptor inner and outer segments
- MTM
myopic traction maculopathy
- MP1
Microperimetry 1
- OCT
optical coherence tomography
- RS
retinal sensitivity
- FTMH
full-thickness macular hole
- SD-OCT
spectral domain OCT
- ERM
epiretinal membrane
Footnotes
Competing interests
Dr. Ying Fan receives research support from the National Basic Research Program of China (973 Program) 2011CB707500. All authors declare that they have no competing interests.
Authors’ contributions
QS carried out the collection, analysis and interpretation of data; participated in drafting the manuscript. HX was involved in data collection, analysis and revision of the draft. FH and XS participated in its design and coordination and helped to revise the draft. YF was responsible for the preliminary thoughts and analyses, original study design, coordination and revision of the manuscript. All authors read and approved the final manuscript.
Contributor Information
Qing Shao, Email: qshao87@hotmail.com.
Huijuan Xia, Email: huijuanxia2015@sina.com.
Florian M. A. Heussen, Email: florian.heussen@gmail.com
Yanling Ouyang, Email: yanlingyouyang@gmail.com.
Xiaodong Sun, Email: xdsun@sjtu.edu.cn.
Ying Fan, Email: mdyingfan@gmail.com.
References
- 1.Panozzo G, Mercanti A. Optical coherence tomography findings in myopic traction maculopathy. Arch Ophthalmol. 2004;122:1455–1460. doi: 10.1001/archopht.122.10.1455. [DOI] [PubMed] [Google Scholar]
- 2.Takano M, Kishi S. Foveal Retinoschisis and Retinal Detachment in Severely Myopic Eyes With Posterior Staphyloma. Am J Ophthalmol. 1999;128:472–476. doi: 10.1016/S0002-9394(99)00186-5. [DOI] [PubMed] [Google Scholar]
- 3.Panozzo G, Mercanti A. Vitrectomy for myopic traction maculopathy. Arch Ophthalmol. 2007;125:767–772. doi: 10.1001/archopht.125.6.767. [DOI] [PubMed] [Google Scholar]
- 4.Smiddy WE, Kim SS, Lujan BJ, Gregori G. Myopic traction maculopathy: spectral domain optical coherence tomographic imaging and a hypothesized mechanism. Ophthalmic Surg Lasers Imaging. 2009;40:169–173. doi: 10.3928/15428877-20090301-21. [DOI] [PubMed] [Google Scholar]
- 5.Gaucher D, Haouchine B, Tadayoni R, Massin P, Erginay A. Long-term follow-up of high myopic foveoschisis: natural course and surgical outcome. Am J Ophthalmol. 2007;143:455–462. doi: 10.1016/j.ajo.2006.10.053. [DOI] [PubMed] [Google Scholar]
- 6.Ikuno Y, Tano Y. Early macular holes with retinoschisis in highly myopic eyes. Am J Ophthalmol. 2003;136:741–800. doi: 10.1016/S0002-9394(03)00319-2. [DOI] [PubMed] [Google Scholar]
- 7.Shimada N, Ohno-Matsui K, Baba T, Futagami S, Tokoro T. Natural course of macular retinoschisis in highly myopic eyes without macular hole or retinal detachment. Am J Ophthalmol. 2006;142:497–500. doi: 10.1016/j.ajo.2006.03.048. [DOI] [PubMed] [Google Scholar]
- 8.Matsumura N, Ikuno Y, Tano Y. Posterior vitreous detachment and macular hole formation in myopic foveoschisis. Am J Ophthalmol. 2004;138:1071–1073. doi: 10.1016/j.ajo.2004.06.064. [DOI] [PubMed] [Google Scholar]
- 9.Hayashi K, Ohno-Matsui K, Shimada N, Moriyama M, Kojima A. Long-term pattern of progression of myopic maculopathy: a natural history study. Ophthalmology. 2010;117:1595–1611. doi: 10.1016/j.ophtha.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 10.Hooshang F, Fedra H, Mohammad RE. Optical coherence tomographic findings in highly myopic eyes. J Ophthalmic Vis Res. 2010;5:110–121. [PMC free article] [PubMed] [Google Scholar]
- 11.Inoue M, Watanabe Y, Arakawa A, Sato S, Kobayashi S. Spectral-domain optical coherence tomography images of inner/outer segment junctions and macular hole surgery outcomes. Graefes Arch Clin Exp Ophthalmol. 2009;247:325–330. doi: 10.1007/s00417-008-0999-9. [DOI] [PubMed] [Google Scholar]
- 12.Sano M, Shimoda Y, Hashimoto H, Kishi S. Restored photoreceptor outer segment and visual recovery after macular hole closure. Am J Ophthalmol. 2009;147:313–318. doi: 10.1016/j.ajo.2008.08.002. [DOI] [PubMed] [Google Scholar]
- 13.Wakabayashi T, Fujiwara M, Sakaguchi H, Kusaka S, Oshima Y. Foveal microstructure and visual acuity in surgically closed macular holes: spectral-domain optical coherence tomographic analysis. Ophthalmology. 2010;117:1815–1824. doi: 10.1016/j.ophtha.2010.01.017. [DOI] [PubMed] [Google Scholar]
- 14.Oh J, Smiddy WE, Flynn HW, Jr, Gregori G, Lujan B. Photoreceptor inner/outer segment defect imaging by spectral domain OCT and visual prognosis after macular hole surgery. Invest Ophthalmol Vis Sci. 2010;51:1651–1658. doi: 10.1167/iovs.09-4420. [DOI] [PubMed] [Google Scholar]
- 15.Fujimoto S, Ikuno Y, Nishida K. Postoperative optical coherence tomographic appearance and relation to visual acuity after vitrectomy for myopic foveoschisis. Am J Ophthalmol. 2013;156:968–973. doi: 10.1016/j.ajo.2013.06.011. [DOI] [PubMed] [Google Scholar]
- 16.Zaben A, Zapata MA, Garcia-Arumi J. Retinal sensitivity and choroidal thickness in high myopia. Retina. 2015;35:398–406. doi: 10.1097/IAE.0000000000000367. [DOI] [PubMed] [Google Scholar]
- 17.Chang LK, Koizumi H, Spaide RF. Disruption of the photoreceptor inner segment-outer segment junction in eyes with macular holes. Retina. 2008;28:969–975. doi: 10.1097/IAE.0b013e3181744165. [DOI] [PubMed] [Google Scholar]
- 18.Baba T, Ohno-Matsui K, Futagami S, Yoshida T, Yasuzumi K. Prevalence and characteristics of foveal retinal detachment without macular hole in high myopia. Am J Ophthalmol. 2003;135:338–342. doi: 10.1016/S0002-9394(02)01937-2. [DOI] [PubMed] [Google Scholar]
- 19.Coppé AM, Ripandelli G, Parisi V, Varano M, Stirpe M. Prevalence of asymptomatic macular holesin highly myopic eyes. Ophthalmology. 2005;112:2103–2109. doi: 10.1016/j.ophtha.2005.06.028. [DOI] [PubMed] [Google Scholar]
- 20.Ratiglia R, Osnaghi S, Bindella A, Pirondini C. Posterior traction retinal detachment in highly myopic eyes: clinical features and surgical outcome as evaluated by optical coherence tomography. Retina. 2005;25:473–478. doi: 10.1097/00006982-200506000-00013. [DOI] [PubMed] [Google Scholar]
- 21.Ando F, Ohba N, Touura K, Hirose H. Anatomical and visual outcomes after episcleral macular buckling compared with those after pars plana vitrectomy for retinal detachment caused by macular hole in highly myopic eyes. Retina. 2007;27:37–44. doi: 10.1097/01.iae.0000256660.48993.9e. [DOI] [PubMed] [Google Scholar]
- 22.Wu TT, Kung YH. Comparison of anatomical and visual outcomes of macular hole surgery in patients with high myopia vs. non-high myopia: a case–control study using optical coherence tomography. Graefes Arch Clin Exp Ophthalmol. 2012;250:327–331. doi: 10.1007/s00417-011-1821-7. [DOI] [PubMed] [Google Scholar]
- 23.Chen YP, Chen TL, Yang KR, Lee WH, Kuo YH. Treatment of retinal detachment resulting from posterior staphyloma-associated macular hole in highly myopic eyes. Retina. 2006;26:25–31. doi: 10.1097/00006982-200601000-00005. [DOI] [PubMed] [Google Scholar]
- 24.Gandorfer A, Haritoglou C, Kampik A. Toxicity of indocyanine green in vitreoretinal surgery. Dev Ophthalmol. 2008;42:69–81. doi: 10.1159/000138974. [DOI] [PubMed] [Google Scholar]


