Abstract
Research indicates stress, craving and menstrual phase may play a role in relapse to smoking. It remains unknown how these factors may interact during cessation. This study describes the relationship between craving and cortisol concentrations by menstrual phase during ad libitum smoking and investigates the impact of this relationship on time to relapse. Five assessments of cortisol concentrations and craving levels were collected the day before smoking cessation in female smokers (n=38) during either the follicular (n=21; F) or luteal (n=17; L) phase. Craving at wake-up was significantly greater in the F phase than the L phase (2.5±1.9 vs. 1.1±1.4; p=0.018; respectively). Decreased levels of morning cortisol concentrations and a greater decline from morning to the nadir levels in cortisol were associated with increased craving at bedtime in the L (r=−0.68, p=0.002; r=−0.67, p=0.003; respectively), but not in the F phase. Craving at wake-up was a significant predictor of time to relapse (p=0.008). Our results indicate that menstrual phase may play a role in the relationship among craving, cortisol concentrations, and risk for relapse.
Keywords: Smoking Cessation, Menstrual Cycle, Craving, Cortisol, Female
1.0 Introduction
Gender disparities have been identified in smoking behavior, such that women experience greater nicotine dependence and have a more difficult time quitting smoking compared to men (Perkins, 2001). Studies of tobacco abstinence on bio-behavioral systems and stress response to account for this gender difference are growing.
Although stress response studies have focused on both the autonomic nervous system response and the hypothalamic-pituitary-adrenal axis (HPAA), sex differences of the HPAA response has been more systematically studied. The stress response is dependent on the stressor used (al’Absi, Lovallo, McKey, & Pincomb, 1994; al’Absi & Lovallo, 1993) responses of both systems show marked and consistent differences according to sex, and hormonal changes in women (i.e. menstrual cycle, pregnancy, and menopause). Adult women between puberty and menopause usually show lower HPAA and autonomic responses than men of the same age. Enhanced HPAA responsiveness has been observed in the luteal phase of the menstrual cycle (Tersman, Collins & Eneroth, 1991; Kirshbaun, Kudiekla, Gaab, Schoomer & Hellhammer, 1999; Rohleder, Schommer, Helhammer, Engle & Kirschbaum, 2001, Wolf, Schommer, Hellhammer, McEwen, & Kirschbaum, 2001). Findings in menopausal women and those on hormone therapy show the HPAA response to be more inconsistent (Lindheim, Legro, Berstein, et al 1992; Seeman, Singer, Wilkinson & McEwen, 2001, Kudielka, Buske-Kirschbaum, Hellhammer & Kirschbaum, 2004). Taken together this body of literature suggests that sex hormones may play a role in the HPAA in women.
With regard to stress response in smoking cessation, cortisol, a physiological measure of stress released by the HPAA, has been shown to vary by sex and smoking status. Female smokers have been shown to have blunted cortisol response to stress when compared to both non-smoking women and men of smoking and non-smoking status (Back, Waldrop, Saladin, et al 2008). Research also suggests that in women the HPAA is more sensitive to the effects of chronic nicotine use (Back et al, 2008). Variance in cortisol levels in response to stress, have been linked to early smoking relapse (al’Absi, Hatsukami, & Davis 2005; Rasmusson, Wu, Paliwal, Anderson & Krishnan-Sarin, 2006). There appears to be a significant decrease in cortisol levels immediately after a quit attempt that is associated with withdrawal symptoms, stress and smoking urges (Ussher, West, Evans, et al, 2006). Differences in the initial cortisol drop may be more pronounced for women compared to men, but the current research yields mixed results on these findings (al’Absi, Hatsukami, Davis & Wittmers, 2004; Ussher et al, 2006). Changes in cortisol were found to be linked with both smoking relapse and changes in depressive symptoms in women, but showed no correlation to depressive symptoms in men (Rasmusson et al, 2006). Further, in women, changes in estrogen modulate changes in cortisol and memory (Andreano, Arjomandi, & Cahill 2008).
Current cortisol and smoking cessation research suggests there may be a link to sex hormones but this has not been fully explored (Back et al, 2008; Rasmusson et al 2006) If cortisol is a predictor of relapse and the menstrual cycle modulates cortisol levels, then specific timing of quit attempts by phase may improve outcomes. Under ad libitum smoking conditions, the current study aims are to investigate menstrual phase differences in (1) diurnal patterns in craving, (2) diurnal patterns in cortisol concentrations, (3) the relationship between craving and cortisol concentrations, and (4) the impact of craving and cortisol concentrations on time to relapse. We hypothesized that cortisol levels will be higher during the luteal phase, that the diurnal pattern will show the expected nadir low and that higher cortisol levels in luteal phase will correlate negatively with prediction of relapse.
2.0. Methods
2.1. Participants
Female smokers were recruited to participate in a randomized smoking cessation trial (Allen, Allen & Pomerleau, 2009; Allen, Bade, Center Finstand & Hatsukami, 2008) from the community via posted flyers, local papers, radio, and television advertisements. To be eligible the women had to: be between the ages of 18–40, be motivated to quit smoking (as indicated through a self-reported 7 or higher on a 10-point Likert-type scale), smoke ≥10 cigarettes per day for at least the past year, have regular menstrual cycles (between 24–36 day cycles), not be taking any hormonal contraception or psychotropic medications, and not using any other forms of tobacco. Eligibility was assessed by a phone screen and a clinic visit. The University of Minnesota’s Investigational Review Board approved this study.
2.2. Protocol
During the screening visit the participants completed the Fagerstrom Test of Nicotine Dependence (FTND; Heatherton, Kozlowski, Frecker & Fagerstrom, 1991), provided demographic information and received a randomly assigned quit date in either the F or L phase of the menstrual cycle. Participants completed weekly/biweekly clinic visits during the first month after their assigned quit date. During the clinic visits, participants also received smoking cessation behavioral counseling (for details regarding this intervention see Allen, et al 2008). No other cessation treatment was used. Smoking status was evaluated at each visit by Carbon Monoxide Breathlyzer (CO < 5ppm indicating abstinence). Daily smoking and menstrual cycle diaries, as well as measures of premenstrual symptoms, withdrawal and smoking urges were completed (data not shown).
2.3 Independent Measures
Menstrual Phase
Menstrual phase was determined using menstrual calendars and urine Luteininzing Hormone (LH) peaks as previously validated by the study authors (Allen, Hatsukami, Christianson, & Nelson, 1996; Allen, Hatsukami, Christianson, & Brown, 2000).
2.4 Dependent Measures
Cortisol
Approximately one week prior to their assigned quit date participants attended a baseline visit and were provided with materials and instruction for saliva sample collection. Cortisol samples were obtained on the day before their quit date, through self-administered Salviettes™ (saliva sample swabs) outside of the clinic at five designated times throughout the day. The subject produced approximately two mL of saliva by placing a cotton swab in their month then depositing it in a plastic tube. The times of collection were as follows: immediately after waking, 60 minutes after waking, 10:00 am, 8:00 pm and at bedtime (see Figure 1). These times were chosen to create a clear diurnal pattern of the cortisol and HPAA activity from the typical highest levels before waking and the nadir levels around 8pm. All samples were stored at −20°C until transferred for analysis. Salivary cortisol assays were conducted in duplicate using a time-resolved immunoassay with fluorometric end point detection. The assay has a minimum sensitivity of 0.4 nmol/L (Dressendorfer, Kirschbaum, Rohde, Stahl & Strasburger, 1992). Cortisol assays were conducted at the University of Dusseldorf (Germany).
Figure 1.
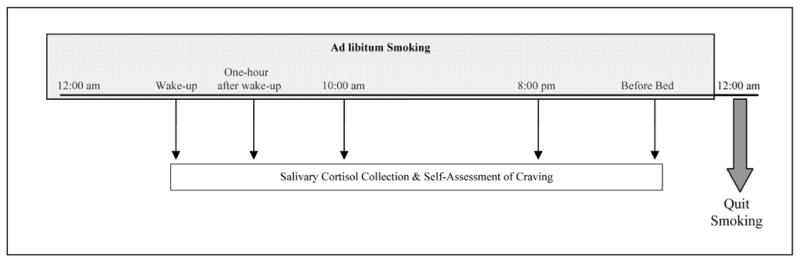
Schematic Diagram of Salivary Cortisol Collection & Self-Assessment of Craving on the Day Before Quit Day
Craving
Each time a cortisol sample was collected, participants assessed their level of craving (al’Absi, Lovallo, McKey, et al 1998; al’Absi Wittmers, Erickson, Hatsukami & Crouse, 2003), with the following item: “rate the degree to which desire to smoke applies to how you felt during the last 30 minutes.” The rating was completed on a likert-type scale ranging from 0 (‘not at all’) to 7 (‘very strong’).
Relapse
Time to relapse (defined as a puff or more from a lit cigarette) was determined retrospectively using daily smoking diaries, Time Line FollowBack (TLFB; Sobell & Sobell, 1991; Sobell & Sobell, 1996) and verified at each clinic visit with Carbon Monoxide breath analyzer (CO < 5ppm indicating abstinence).
2.3. Statistical Analysis
The difference between nadir and wake-up in cortisol concentration was computed by subtracting the cortisol value at 8:00 pm from the cortisol value at wake-up. Descriptive statistics were computed to describe demographics, smoking behavior, craving and cortisol concentrations. Demographic and smoking behavior differences by randomization group were assessed by t-tests and chi-square tests. Craving and cortisol concentrations were compared between the randomization groups by conducting independent t-tests. Craving and cortisol concentrations were further compared by computing Pearson correlations and Fisher z-Transformation by menstrual cycle phase and repeated measures ANOVAs controlling for FTND score. A multiple regression model, controlling for FTND score, used all five cortisol concentrations, all five craving items and menstrual phase to predict days to relapse. All analyses were completed using SAS 9.1.
3.0 Results
3.1. Demographics & Smoking Behavior
A total of 38 participants were enrolled into the study, 21 were randomized to F phase and 17 to L phase. Participants were, on average, 29.80 (Standard Deviation [S.D.] ± 6.40) years old with an average of 13.92 (S.D. ± 1.71) years of education. They smoked a mean of 14.61 (S.D. ± 4.00) cigarettes per day with an average FTND score of 3.53 (S.D. ± 1.83). Participants who were randomized to the F phase had significantly higher FTND scores compared to those randomized to the L phase (4.33±1.62 vs. ± 2.53±1.59, respectively; p-value=0.002). There were no other statistically significant differences between the randomization groups in terms of demographics or smoking behavior (Table 1).
Table 1.
Demographics & Smoking Behavior by Randomization Group (Mean ± Standard Deviation)
| All (n=38) | F Phase (n=21) | L Phase (n=17) | |
|---|---|---|---|
| Demographics | |||
| Age (years) | 29.80±6.40 | 28.76±6.37 | 31.06±6.39 |
| Education (years) | 13.92±1.71 | 13.76±1.79 | 14.12±1.65 |
| Smoking Behavior | |||
| CPD | 14.61±4.00 | 14.81±4.00 | 14.35±4.12 |
| Age Started (years) | 16.58±2.52 | 16.10±1.81 | 17.18±3.15 |
| FTND Score | 3.53±1.83 | 4.33±1.62 | 2.53±1.59 |
3.2. Diurnal Pattern of Craving by Menstrual Phase
Craving ranged from a low of 1.86 (S.D. ± 1.80) at wake-up to a high of 3.68 (S.D. ± 1.45) at 8:00 p.m. Those in the F phase reported significantly higher craving levels at wake-up compared to participants in the L phase (2.48±1.89 vs. 1.12±1.41, respectively; p-value=0.018). This significant relationship was reduced to a trend (F-value=3.90, p-value=0.056) when FTND score was controlled for. There were no other significant differences in craving by phase (Table 2).
Table 2.
Craving and Cortisol Concentration by Menstrual Phase (Mean ± Standard Deviation)
| All (n=38) | F Phase (n=21) | L Phase (n=17) | |
|---|---|---|---|
| Craving † | |||
| Wake-up | 1.86±1.80 | 2.48±1.89 | 1.12±1.41 |
| One hour after wake-up | 2.82±1.57 | 3.19±1.66 | 2.35±1.37 |
| 10:00 am | 3.32±1.69 | 3.14±1.82 | 3.53±1.55 |
| 8:00 pm | 3.68±1.45 | 3.80±1.40 | 3.53±1.55 |
| Bed time | 3.45±2.00 | 3.33±1.93 | 3.59±2.12 |
| Cortisol Concentration * | |||
| Wake-up | 10.98±6.23 | 11.13±5.00 | 10.81±7.65 |
| One hour after wake-up | 10.00±5.91 | 9.93±6.32 | 10.08±6.60 |
| 10:00 am | 5.59±3.52 | 4.87±2.17 | 6.47±4.62 |
| 8:00 pm (Nadir) | 2.19±1.71 | 2.37±2.01 | 1.95±1.27 |
| Bed time | 3.15±3.83 | 3.09±4.67 | 3.23±2.59 |
| Difference between Nadir and Wake-up | 12.06±5.84 | 8.75±5.83 | 8.85±7.33 |
Using a 8-point Likert Type Scale (range 0–7)
Reported in nanomol/Liter
3.3. Diurnal Pattern of Cortisol Concentrations by Menstrual Phase
Cortisol concentrations ranged from 10.98 (S.D. ±6.23) nmol/L at wake-up to 2.19 (S.D. ±1.71) nmol/L at the nadir level (8:00 pm). Cortisol concentrations were not significantly different by menstrual phase at any time point during the day (Table 2). This finding was confirmed in an analysis controlling for FTND score, which also indicated no significant differences in cortisol concentrations by phase (data not shown).
3.4. Correlation between Craving and Cortisol Concentration by Menstrual Phase
Increased craving at night was associated with greater cortisol concentrations at wake-up and greater decline from morning to the nadir levels in cortisol concentrations (r=−0.450, p-value=0.005; r=−0.481, p-value=0.002; respectively). When this association was investigated by menstrual phase, these findings were only significant in the L phase (r=−0.680, p-value=0.003; r=−0.674, p-value=0.003; respectively) and not in the F phase (r=−0.151, p-value=0.513, r=−0.280, p-value=0.219). There were no other significant correlations between craving and cortisol concentrations (data not shown).
3.5. Predictability of Craving, Cortisol Concentrations and Menstrual Phase on Time to Relapse
After controlling for FTND score, craving at wake-up was a significant predictor of time to relapse (p=0.008). There were no other significant predictors based on craving, cortisol concentrations or menstrual phase (data not shown).
4.0 Discussion
The results of this study indicate there may be a relationship between cortisol concentrations, craving, menstrual cycle phase and smoking cessation outcomes. While we did not observe any significant differences in cortisol concentrations by menstrual phase, we observed significantly higher levels of craving at wake up among women in the follicular phase as compared to women in the luteal phase. Craving at night was negatively correlated to both the morning and the diurnal pattern of cortisol concentrations. This relationship was significant in the luteal phase, but not the follicular phase. Finally, craving at wake-up significantly predicted time to relapse regardless of baseline level of dependence, cortisol concentrations and menstrual cycle phase. In addition our findings confirm expected diurnal cortisol fluctuations (Bailey & Heitkemper, 1991; Weitzman, Fukushima, Nogerire, Roffwarg, Gallagher, & Hellman, 1971).
These observations are particularly interesting in light of our recent findings in a randomized clinical smoking cessation trial (Allen et al, 2008b), which indicated that the luteal phase was associated with a more favorable smoking cessation outcome. While the mechanism for this observation remains unknown, we theorize that the results may be a function of an influence of ovarian hormones on subjective mood response or physiological and subjective effects of nicotine (or both). In contrast, retrospective clinical trials (Carpenter, Saladin, Leinbach, Larowe & Upadhyaya, 2008; Franklin, Napier, Ehrman, Hariti, O’Brien & Childress, 2004l) using pharmacotherapy found that women quitting in the follicular phase had more favorable outcomes. Further, recent research by Benowitz and colleagues (2006) indicated that women using combination birth control pills metabolized nicotine faster than both women using progesterone-only pills and men; suggesting that higher levels of estrogen may be associated with an increase in nicotine metabolism. These results taken together, however, suggest that ovarian hormones play a role in smoking cessation outcomes for women and need to be considered in treatment programs and clinical trials.
We also found that decreased levels of morning cortisol concentrations and a greater decline from morning to the nadir levels in cortisol were associated with increased craving. These results are consistent with previously reported findings indicating that the dysregulated HPAA activity in smokers is associated with enhanced withdrawal symptoms and risk for smoking relapse (Frederick, Reus, Ginsberg, et al, 1998; al’Absi, Amunrud, & Wittmers, 2002; al’Absi, 2006). It is possible that nicotine’s actions on the HPAA contribute to the reinforcing properties of smoking and enhance the benefits smokers draw from nicotine, and therefore reduced cortisol levels may be associated with increased craving. Specific mechanisms mediating these properties remain to be investigated. For example, it is possible that cortisol moderates functions of neuropeptides that mediate nicotine’s effects (Koob & Le Moal, 1997). Nevertheless, these findings suggest that craving may be increased by declined cortisol levels, although these findings need to be replicated in larger studies.
This study is among the first to prospectively investigate multiple risk factors of smoking relapse among female smokers with specific regard to the menstrual cycle. This study had a number of limitations including a relatively small, homogeneous sample size which may limiting the generalizability of our results and might account for the discrepant findings between our previous publication (Allen et al, 2008) and this study regarding the predictability of menstrual phase on time to relapse. Participants completed the cortisol saliva samples and craving item on their own time; thus, it may be possible that data was not collected as instructed. In addition, we are unable to comment on the potentially causal relationship between estrogen/progresterone and smoking cessation outcomes, as we did not measure hormone levels in this study.
In conclusion, the present study suggests there may be a complex relationship between menstrual cycle, craving and cortisol levels; and the possible impact of these items on smoking cessation outcomes. Future work is needed in larger studies to further define this relationship.
Acknowledgments
This study was funded by NIDA grant 2-R01-DA08075. We thank our research staff – Tracy Bade, Nicole Cordes and Roshan Paudal – for their help with study management, subject recruitment, data measurement and data entry.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Alicia M. Allen, Email: alle0299@umn.edu, University of Minnesota, Medical School, Department of Family Medicine & Community Health; 2701 University Avenue SE, Suite 201, Minneapolis, MN 55414, Phone: 612-627-1818, Fax: 612-627-4899
Sharon S. Allen, Email: allen001@umn.edu, University of Minnesota, Medical School, Department of Family Medicine & Community Health; 2701 University Avenue SE, Suite 201, Minneapolis, MN 55414, Phone: 612-624-2446, Fax: 612-625-0916
Jennifer Widenmier, Email: kings131@umn.edu, University of Minnesota, Medical School, Department of Family Medicine & Community Health; 2701 University Avenue SE, Suite 201, Minneapolis, MN 55414, Phone: 612-627-4902; Fax: 612-627-4899
Mustafa al’Absi, Email: malabsi@d.umn.edu, University of Minnesota Medical School, 1035 University Drive, Room 236 D601, Duluth, MN, Phone: 218-726-7144, Fax: 612-624-0727
References
- al’Absi M, Amunrud T, Wittmers LE. Psychophysiological effects of nicotine abstinence and behavioral challenges in habitual smokers. Pharmacology, Biochemistry & Behavior. 2002;72:707–716. doi: 10.1016/s0091-3057(02)00739-6. [DOI] [PubMed] [Google Scholar]
- al’Absi M, Hatsukami D, Davis GL, Wittmers LE. Prospective examination of effects of smoking abstinence on cortisol and withdrawal symptoms as predictors of early smoking relapse. Drug & Alcohol Dependence. 2004;73:267–278. doi: 10.1016/j.drugalcdep.2003.10.014. [DOI] [PubMed] [Google Scholar]
- al’Absi M, Hatsukami D, Davis GL. Attenuated androcorticotropic responses to psychological stress are associated with early smoking relapse. Psychopharmacology. 2005;181:107–117. doi: 10.1007/s00213-005-2225-3. [DOI] [PubMed] [Google Scholar]
- al’Absi M, Lovallo WR, McKey BS, Pincomb GA. Borderline hypertensives produce exaggerated adrencortical responses to mental stress. Psychosomatic Medicine. 1994;56:245–250. doi: 10.1097/00006842-199405000-00011. [DOI] [PubMed] [Google Scholar]
- al’Absi M, Lovallo WR. Cortisol concentrations of borderline hypertensive men exposed to a novel experimental setting. Psychoneuroendorinology. 1993;18:355–363. doi: 10.1016/0306-4530(93)90011-9. [DOI] [PubMed] [Google Scholar]
- al’Absi M, Lovallo WR, McKey B, Sung BH, Whitsett TL, Wilson MF. Hypothalamic-pituitary-adrenocortical responses to psychological stress and caffeine in men at high and low risk for hypertension. Psychosomatic Medicine. 1998;60:521–527. doi: 10.1097/00006842-199807000-00021. [DOI] [PubMed] [Google Scholar]
- al’Absi M, Wittmers LE, Erickson J, Hatsukami DK, Crouse B. Attenuated adrenocortical and blood pressure responses to psychological stress in ad libitum and abstinent smokers. Pharmacology, Biochemistry & Behavior. 2004;74:401–410. doi: 10.1016/s0091-3057(02)01011-0. [DOI] [PubMed] [Google Scholar]
- al’Absi M, Wittmers LE, Erickson J, Hatsukami DK, Crouse B. Attenuated adrenocortical and blood pressure responses to psychological stress in ad libitum and abstinent smokers. Pharmacology, Biochemistry & Behavior. 2003;74:401–410. doi: 10.1016/s0091-3057(02)01011-0. [DOI] [PubMed] [Google Scholar]
- al’Absi M. Hypothalamic-pituitary-adrenocortical responses to psychological stress and risk for smoking relapse. International Journal of Psychophysiology. 2006;59:218–227. doi: 10.1016/j.ijpsycho.2005.10.010. [DOI] [PubMed] [Google Scholar]
- Allen SS, Allen AM, Pomerleau CS. Influence of phase-related variability in premenstrual symptomatology, mood, smoking withdrawal and smoking behavior during ad libitum smoking, on smoking cessation outcome. Addictive Behaviors. 2009;37:107–111. doi: 10.1016/j.addbeh.2008.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen SS, Bade T, Center B, Finstad D, Hatsukami D. Menstrual Phase Effects on Smoking Relapse. Addiction. 2008;103:809–821. doi: 10.1111/j.1360-0443.2008.02146.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen SS, Hatsukami DK, Christianson D, Brown S. Effects of transdermal nicotine on craving, withdrawal and premenstrual symptomatology in short-term smoking abstinence during different phases of the menstrual cycle. Nicotine & Tobacco Research. 2000;2:231–241. doi: 10.1080/14622200050147493. [DOI] [PubMed] [Google Scholar]
- Allen SS, Hatsukami D, Christianson D, Nelson D. Symptomatology and energy intake during the menstrual cycle in smoking women. Journal of Substance Abuse. 1996;8:303–319. doi: 10.1016/s0899-3289(96)90170-4. [DOI] [PubMed] [Google Scholar]
- Andreano JM, Arjomandi H, Cahill L. Menstrual cycle modulation of the relationship between cortisol and long-term memory. Psychoneuroendocrinology. 2008;33:874–882. doi: 10.1016/j.psyneuen.2008.03.009. [DOI] [PubMed] [Google Scholar]
- Back SE, Waldrop AE, Saladin ME, Yeatts SD, Simpson A, McRae AL, Upadhyaya HP, Sisson RC, Spratt EG, Allen J, Kreek MJ, Brady LT. Effects of gender and cigarette smoking on reactivity of psychological and pharmacological stress provocation. Psychoneuroendocrinology. 2008;33:560–568. doi: 10.1016/j.psyneuen.2008.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey SL, Heitkemper MM. Morningness-eveningness and early morning salivary cortisol levels. Biological Psychology. 1991;32:181–192. doi: 10.1016/0301-0511(91)90009-6. [DOI] [PubMed] [Google Scholar]
- Benowitz NL, Lessov-Schlaggar CN, Swan GE, Jacob P. Female sex and oral contraceptive use accelerate nicotine metabolism. Clinical Pharmacology Therapy. 2006;79:480–488. doi: 10.1016/j.clpt.2006.01.008. [DOI] [PubMed] [Google Scholar]
- Carpenter MJ, Saladin ME, Leinbach AS, Larowe SD, Upadhyaya HP. Menstrual phase effects on smoking cessation: A pilot feasibility study. Journal of Womens Health. 2008;17:293–301. doi: 10.1089/jwh.2007.0415. [DOI] [PubMed] [Google Scholar]
- Dressendorfer RA, Kirschbaum C, Rohde W, Stahl F, Strasburger CJ. Synthesis of cortisol-biotin conjugate and evaluation as a tracer in am immunoassay for salivary cortisol measurement. The Journal of Steroid Biochemistry & Molecular Biology. 1992;43:683–692. doi: 10.1016/0960-0760(92)90294-s. [DOI] [PubMed] [Google Scholar]
- Franklin T, Napier K, Ehrman R, Gariti P, O’Brien C, Childress A. Retrospective study: Influence of menstrual cycle on cue-induced cigarette craving. Nicotine & Tobacco Research. 2004;6:171–175. doi: 10.1080/14622200310001656984. [DOI] [PubMed] [Google Scholar]
- Frederick SL, Reus VI, Ginsberg D, Hall SM, Munoz RF, Ellman G. Cortisol and response to dexamethasone as predictors of withdrawal distress and abstinence success in smokers. Biological Psychiatry. 1998;43:525–530. doi: 10.1016/S0006-3223(97)00423-X. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The fagerstrom test for nicotine dependence: A revision of the fagerstrom tolerance questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Kirshbaum C, Kudiekla BM, Gaab J, Schommer NC, Hellhammer DH. Impact of gender, menstrual cycle phase, and oral contraceptives on the activity of the hypothalamus-pituitary-adrenal axis. Psychosomatic Medicine. 1999;61:154–162. doi: 10.1097/00006842-199903000-00006. [DOI] [PubMed] [Google Scholar]
- Koob GF, Le Moal M. Drug abuse: hedonic homeostatic dysregulation. Science. 1997;278:52–58. doi: 10.1126/science.278.5335.52. [DOI] [PubMed] [Google Scholar]
- Kudielka BM, Buske-Kirschbaum A, Hellhammer DH, Kirschbaum C. HPA axis responses to laboratory psychosocial stress in healthy elderly adults, younger adults, and children: impact of age and gender. Psychoneuroendocrinology. 2004;29:83–89. doi: 10.1016/s0306-4530(02)00146-4. [DOI] [PubMed] [Google Scholar]
- Lindheim SR, Legro RS, Bernstein L, Stanczyk FZ, Vijod MA, Presser SC, Lobo RA. Behavioral stress responses in premenopausal and postmenopausal women and the effects of estrogen. American Journal of Obstetrics & Gynecology. 1992;167:1831–1836. doi: 10.1016/0002-9378(92)91783-7. [DOI] [PubMed] [Google Scholar]
- Perkins KA. Smoking cessation in women: Special considerations. CNS Drugs. 2001;5:391–411. doi: 10.2165/00023210-200115050-00005. [DOI] [PubMed] [Google Scholar]
- Rasmusson AM, Wu R, Paliwal P, Anderson GM, Krishnan-Sarin S. A decrease in plasma DHEA to cortisol ratio during smoking abstinence may predict relapse: A preliminary study. Psychopharmacology. 2006;186:473–480. doi: 10.1007/s00213-006-0367-6. [DOI] [PubMed] [Google Scholar]
- Rohleder N, Schommer NC, Hellhammer DH, Engle R, Kirschbaum C. Sex differences in glucocorticoid sensitivity of proinflammatory cytokine production after psychosocial stress. Psychosomatic Medicine. 2001;63:966–972. doi: 10.1097/00006842-200111000-00016. [DOI] [PubMed] [Google Scholar]
- Seeman TE, Singer B, Wilkinson CW, McEwen B. Gender differences in age-related changes in HPA axis reactivity. Psychoneuroendocrinology. 2001;26:225–240. doi: 10.1016/s0306-4530(00)00043-3. [DOI] [PubMed] [Google Scholar]
- Sobell L, Sobell MB. Timeline Follow-Back: A technique for assessing self-reported alcohol consumption. New Jersey: Humana Press; 1991. [Google Scholar]
- Sobell LC, Sobell MB. Timeline Follow-Back User’s Guide. Toronto, Canada: Addiction Research Foundation; 1996. [Google Scholar]
- Tersman Z, Collins A, Eneroth P. Cardiovascular responses to psychological and physiological stressors during the menstrual cycle. Psychosomatic Medicine. 1991;53:185–197. doi: 10.1097/00006842-199103000-00008. [DOI] [PubMed] [Google Scholar]
- Ussher M, West R, Evans P, Steptoe A, McEwan A, Clow A, Hucklebridge F. Reductin in cortisol among users of nicotine patches. Psychosomatic Medicine. 2006;68:229–306. doi: 10.1097/01.psy.0000204926.27215.a1. [DOI] [PubMed] [Google Scholar]
- Weitzman ED, Fukushima D, Nogerire C, Roffwarg H, Gallagher TF, Hellman L. Twenty-four hour pattern of the episodic secretion of cortisol of normal subjects. Journal of Clinical Endocrinology. 1971;33:14–21. doi: 10.1210/jcem-33-1-14. [DOI] [PubMed] [Google Scholar]
- Wolf OT, Schommer NC, Hellhammer DH, McEwen BS, Kirschbaum C. The relationship between stress induced cortisol levels and memory differs between men and women. Psychoneuroendocrinology. 2001;26:711–720. doi: 10.1016/s0306-4530(01)00025-7. [DOI] [PubMed] [Google Scholar]


