Abstract
There has been limited research that has examined the prevalence of depression and attitudes towards depression and mental health treatment in Arab-American adolescents; we sought to assess these in a predominantly Arab-American community in metro Detroit. A health survey of adolescents aged 12–17 years was conducted (n=98). Participants were recruited from two local community organizations in Dearborn, MI. Depression was assessed by the Patient Health Questionnaire-9 (PHQ-9) Depression Scale, and attitude towards depression and willingness to seek help for mental health conditions were assessed by the Self-Stigma of Depression Scale (SSDS). To assess whether attitudes might be affected by information about mental health treatment, adolescents were randomized to view either an educational video about mental health, or a control video before responding to questions about their willingness to seek help for mental health conditions. Overall, 14% of Arab-American adolescents in this study endorsed moderate or moderately severe depression (PHQ-9 ≥ 11), suggesting a need to increase awareness of and access to mental health services and screening for Arab-American youth.
Keywords: adolescents, arab-american, depression, mental health, stigma
Introduction
Depression is a costly and debilitating mental illness that can result in short-term disability and decreased productivity, and can adversely affect the course of common chronic conditions, such as arthritis, asthma, cardiovascular disease, cancer, diabetes, and obesity (Centers for Disease Control and Prevention, 2011). According to the World Health Organization (2009), depression is the leading cause of disability in the world, as well as the 4th leading contributor to the global burden of disease.
Depression affects approximately 1 in 10 adults in the United States (Centers for Disease Control and Prevention, 2011), however depression rates have been found to vary significantly by ethnic group. Since September 11, 2001, studies have shown that Arab-American adults in particular have been found to have high rates of depression. According to a post-9/11 online study among 601 adult Arab-Americans from 35 states, 50% of respondents reported scores that met criteria for depression, as assessed by the Center for Epidemiologic Studies-Depression Scale (CES-D) (Amer & Hovey, 2011).
Among Arabs in the Middle-East, both depression and seeking help for mental illness are issues that are heavily stigmatized. Stigma associated with mental health care may negatively affect a person’s decision to seek out psychological therapy and counselling (Corrigan, 2004). Studies have shown that the rate of depression in Lebanon, for example, is comparable to the rate of depression in Western Europe, while the percentage of patients with depression who actually seek treatment is much lower (Karam et al., 2006). Studies assessing stigma towards mental health among in Arabs living in America are limited, but there is some evidence to show that stigma consciousness is associated with greater severity of most symptoms in adult Arab-American mental health patients (Kira & Hammad, 2005).
Large public health database studies about Arab-American mental health are difficult to perform, as Arabs are considered to be an ‘invisible minority’ in the United States (Naber, 2000). People of Arab descent are categorized as ‘White’ or ‘Caucasian’ by the American government, thus making it unfeasible to extract group-specific data from public mental health databases (Amer & Hovey, 2011). Given these limitations, an even less studied group is Arab-American adolescents.
Despite a high prevalence of mental disorders among adolescents generally, this age group is one of the least likely to seek help (Kessler et al., 2005). Even further, it has been suggested that young people from cultural minority groups may be even less likely to voluntarily seek professional help when needed (Rickwood et al., 2007). Arab-American adolescents, in particular, face an increased risk for discrimination and acculturative stress (Ahmed et al., 2011).
The specific aims of this study were: to explore the rates of depression and the presence of other health issues in a sample of Arab-American adolescents from a community in metro Detroit; to compare levels of stigma associated with both depression and seeking psychological help between youth with and without depression; and to assess whether viewing an educational video about mental health stigma would decrease ratings of stigma towards depression and mental health help-seeking in adolescents.
Methods
Study Design
Participants were recruited using convenience sampling at two local community organizations in Dearborn, Michigan: the Arab Community Center for Economic & Social Services (ACCESS) Child & Adolescent Health Center and the Helping Youth Progress & Excel (HYPE) Recreation Center. The city of Dearborn has the largest proportion of Arab Americans in the United States, and the state of Michigan ranks second overall in the size of its Arab American population (Arab American Institute, 2013).
Recruitment took place over a span of six months from February to July, 2012. Inclusion criteria for adolescents included age between 12–17 years old, and self-identified as being of Arab descent. Of the 119 adolescents that completed the survey: 11 (9.2%) were excluded due to being outside the age range and 10 (8.4%) were excluded for not identifying as Arab.
Recruitment approach differed slightly by location. At the ACCESS Child & Adolescent Health Center, volunteers approached parents who were with children in the waiting room. At the HYPE Recreation Center, parents and adolescent volunteers signed up to take the survey at various events throughout the building. The study was also advertised at local high schools with flyers; interested students came to one of the two study locations to complete the survey.
Parental consent and adolescent assent were obtained. Each participant was provided with a $10 incentive for their participation in the study. Since the study was anonymous, at the end of the survey adolescents were provided with information for free follow-up counselling to discuss any issues brought up during the survey. The University of Michigan Institutional Review Board approved this study.
Survey Design
The online surveys were administered on computers at one of the two study locations. The surveys were hosted securely on SurveyGizmo.com. The youth survey included two YouTube® videos that were randomized to adolescents taking the survey.
Measures
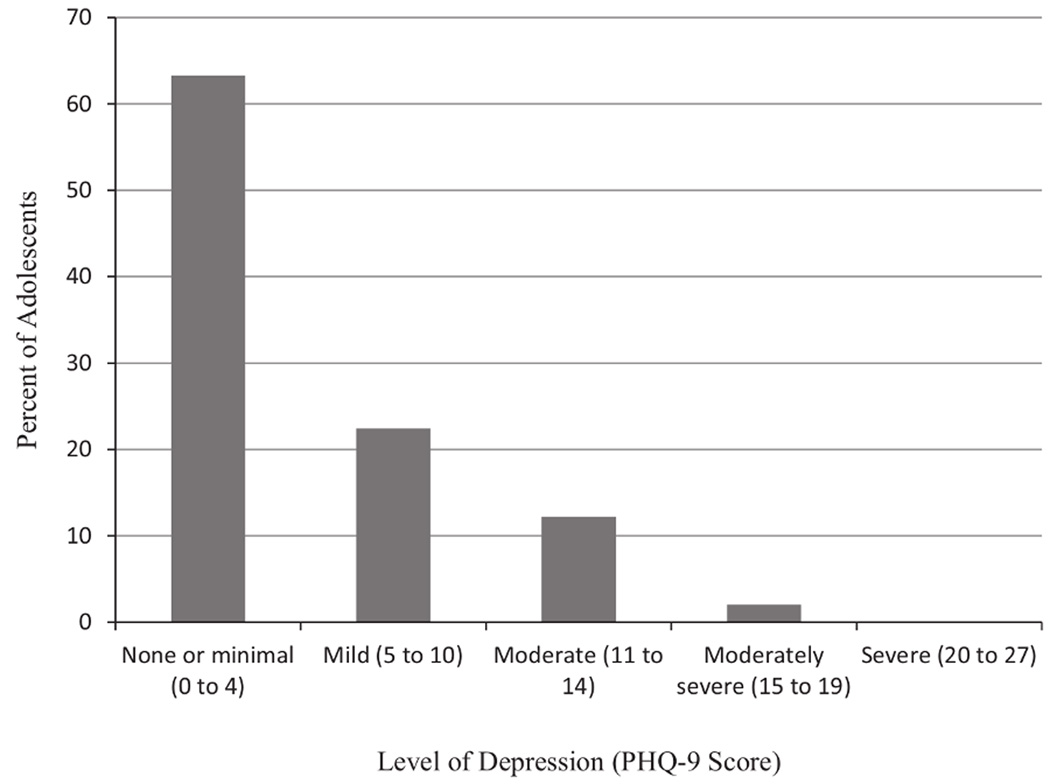
Depression among adolescents was measured by the Patient Health Questionnaire-9 (PHQ-9) Depression Scale. The PHQ-9 is a depression survey that scores each of the nine DSM-IV criteria over the preceding two weeks as present not at all (0) to nearly every day (3); scores range from 0 to 27 (Kroenke et al., 2001). PHQ-9 scores were separated into five tiers to indicate level of depression: 0–4: none or minimal; 5–10: mild; 11–14: moderate; 15–19: moderately-severe; 20+: severe. According to Richardson et al. (2010), a PHQ-9 score of 11 or more had a sensitivity of 89.5% and a specificity of 77.5% for detecting youth who met the DSM-IV criteria for major depression.
Stigma towards depression and willingness to seek help for mental health conditions were measured by the Self-Stigma of Depression Scale (SSDS). This scale is useful in understanding self-stigma and evaluating stigma interventions. Scores from the SSDS range from 16 to 80, with higher scores indicating higher levels of stigma. Although the SSDS has only been validated in adults, the authors suggest that it would be highly suitable for adolescents (Barney et al., 2010).
Prior to administration of the SSDS, the online survey automatically randomized the adolescents to watch one of two videos: a mental health awareness video (n=46) vs. a control video which discussed childhood obesity (n=42), with the remaining adolescents (n=10) unaccounted for due to a data collection error at the beginning of this study where the survey did not capture the video randomization variable. Each video was 4–5 minutes in length and was in the same format, with a health professional being interviewed in each (Christie Clinic, 2011; Cale, 2009). The mental health awareness video provided mental health education to youth within a short time frame. Due to the data collection error that did not record which video was assigned for the first 10 adolescents, these subjects were not included in analyses of the responses to the stigma questionnaire when comparing the association between stigma scores and video. However, we included all adolescent (n=98) SSDS scores for other calculations such as the average SSDS scores for all adolescents, and also when comparing the association between average SSDS scores and depression.
Statistical Analysis
For the results in this study, Chi-squared tests were performed to compare depression (PHQ-9 ≥ 11) with other study population characteristics. Independent samples t-tests were used to compare average PHQ scores among youth. A Pearson correlation was used to measure the association between SSDS scores and total PHQ-9 scores. All significance values reported are two tailed.
Results
The majority of adolescent participants were recruited at the ACCESS site (n=80), with the balance recruited at HYPE (n=18). Overall, the majority of the adolescent participants (82%) said that the main reason for their visit to the study location was ‘only to take this survey;’ however, the breakdown differed between locations. At the HYPE Recreation Center, 100% of the adolescents cited that the main reason for their visit to the study location was ‘only to take this survey;’ meanwhile, at the ACCESS Child & Adolescent Health Center, 22.5% of the adolescents cited a different reason for their visit to the site that day.
Table 1 summarizes the socio-demographic characteristics of the adolescent study population (n=98). There was a slightly higher ratio of males (57%) to females (43%). Ages ranged from 12 to 17 (M=15.4; SD=1.5). The majority of adolescents were second generation immigrants (69%), with 20% being first generation immigrants and 10% third generation immigrants. The study population was predominantly Muslim (93%). There was no difference in gender, age, depression scores, or SSDS stigma scores between participants who took the survey at ACCESS (n=80) compared to those who were recruited at HYPE (n=18).
Table 1.
Descriptive Characteristics for Arab-American Adolescents Recruited from Dearborn, MI, February to July, 2012 (n=98).
| N (%) (or Mean ± SD) | |
|---|---|
| Age | 15.4 ± 1.5 |
| Gender | |
| Male | 56 (57%) |
| Female | 42 (43%) |
| Education | |
| 5th to 6th grade | 7 (7%) |
| 7th to 8th grade | 7 (7%) |
| 9th grade | 19 (19%) |
| 10th grade | 30 (31%) |
| 11th grade | 15 (15%) |
| 12th grade | 20 (20%) |
| Country of Origin | |
| USA | 77 (79%) |
| Yemen | 5 (5%) |
| Saudi Arabia | 5 (5%) |
| Lebanon | 4 (4%) |
| Iraq | 4 (4%) |
| Other | 3 (3%) |
| Immigrant Generation | |
| Firsta | 20 (20%) |
| Secondb | 68 (69%) |
| Thirdc | 10 (10%) |
| Religion | |
| Muslim | 91 (93%) |
| Other | 7 (7%) |
| Hijab* (n=42) | |
| Yes | 29 (69%) |
| No | 13 (31%) |
| Recruitment Site | |
| ACCESS Child & Adolescent Health Center | 80 (82%) |
| HYPE Recreation Center | 18 (18%) |
| PHQ Depression Screen † | |
| None or minimal depression (0–4) | 62 (63%) |
| Mild depression (5–10) | 22 (23%) |
| Moderate depression (11–14) | 12 (12%) |
| Moderately severe depression (15–19) | 2 (2%) |
| Severe depression (20–27) | 0 (0%) |
| Self-Stigma of Depression Scale (SSDS) ‡ | |
| Mean | 54.3 ± 13.4 |
| Range | (20, 76) |
Immigrant youth who migrated to the U.S.
U.S.-born children of at least one foreign-born parent.
U.S.-born children of two U.S.-born parents, where at least one grandparent is foreign-born.
Hijab is a veil which covers the hair, and is worn by Muslim women particularly in the presence of non-related adult males. This question was on asked to individuals who identified themselves as female.
A total PHQ-9 score ≥11 has an optimal sensitivity and specificity for detecting major depression in adolescents.
SSDS: Minimum Score = 16, Maximum Score = 80.
The majority of the adolescents reported never having consumed an alcoholic drink (91%), smoked a cigarette (86%), or tried recreational drugs (93%). With regards to water pipes (hookahs), 33% of the adolescents reported smoking a water pipe at least once.
Overall, 14% of adolescents endorsed moderate or moderately severe depression (PHQ-9 ≥ 11). Only two percent of adolescents in this study reported that they were previously diagnosed with depression. Subjects who reported dissatisfaction with their current weight (34%) were more likely to also endorse significant levels of depression (p = 0.045). There were no other differences on any measure between those with PHQ-9 scores ≥ 11 vs. those with PHQ-9 < 11, and there was no statistically significant differences by gender for the PHQ-9 scores or other survey responses.
Five percent of the adolescents reported experiencing sexual activity against their will. Of these five participants, four (80%) reported that they did not tell anyone or seek help, and two (40%) endorsed moderate or moderately severe depression.
With regards to prior mental health help-seeking, 13% of adolescents reported previously talking with a health professional about a mental health issue. Of those who did not or were unsure (n=85), 35% of them said they would never consider talking to a health professional about any mental health issues.
With regards to the SSDS stigma score, there was no difference between adolescents who were randomized to the mental health awareness video (n=46) and those randomized to the control video (n=42); (56.2, SD=14.6 vs. 52.0, SD 12.9; p=0.16). Stigma scores did not vary significantly by gender, immigrant generation, or depression based on PHQ-9 cut-off score. There was a weak but statistically significant correlation between PHQ-9 score and SSDS score (r=0.23; p=0.024), suggesting that the PHQ-9 scores only explained approximately 5% of the variance of SSDS scores.
Discussion
Nearly one in seven (14%) Arab-American adolescents in this study exhibited moderate or moderately severe depression based on PHQ-9 scores. At the same time, only two percent of the adolescents in the study population reported a prior diagnosis of depression by a health professional. While the sampling methodology was not designed to collect a representative sample of the adolescent population in this community, the results suggest that the rate of depression among Arab-American adolescents may be higher than the national rate of major depression among American adolescents aged 12–17 (8.0%) (Federal Interagency Forum on Child and Family Statistics, 2012).
We recognize that the PHQ-9 is not a diagnostic assessment, and so reported depression prevalence is merely an estimate. At the same time, the number of adolescents endorsing moderate or moderately severe depression may be underreported in our data. Youth may often meet diagnostic criteria for major depressive disorder by presenting with irritability rather than depressed mood. Although the PHQ-9 was validated among adolescents, it does not include an item about irritability (Richardson et al., 2010).
A proposed method to decrease stigma towards mental health is through mental health awareness and education (Penn & Couture, 2002). In our study, we found that a brief mental health awareness video was not associated with decreased stigma scores or more positive views about seeking psychological help. This single, brief exposure to mental health education appeared to have little impact on stigma.
Limitations of this study included the use of convenience sampling. Although this method allowed us to reach our recruitment goals in a timely and cost-effective manner, it limits generalizability to the Arab-American adolescent population at large.
Given these limitations, this study still provides some insight into the adolescent population in this community, and it suggests a need to increase access to screening and mental health services for Arab-American youth.
Future research is needed to elucidate the causes for the high rate of depression in this sample. Since our study only focused on adolescents of Arab descent, future studies in this community can compare depression scores between Arab-American adolescents with adolescents of other races and ethnicities who live in the same community. Methods to recruit a broader, more representative sample should be considered. In addition, future research could strive to assess to what extent parents, the home, or the society might have had an effect on adolescent mental health.
If additional studies show high ratings of stigma towards mental health in the broader Arab-American adolescent population, then one would want to consider using other modalities of mental health education and awareness in order to decrease this stigma.
Figure 1.
Adolescent PHQ-9 Depression Screen: Level of Depression.
Acknowledgement
This study was carried out with funding from the University of Michigan Institute for Clinical & Health Research (MICHR) [2UL1TR000433]. A special thanks to the staff at the ACCESS Child & Adolescent Health Center, the staff at the HYPE Recreation Center, Ali Sayed, Ola Saad, Mountaha Eidy, and Hady Jaber for their support and assistance.
Footnotes
Notes on contributors
When this work was conducted, Reda Jaber was a medical student at the University of Michigan, in a combined MD/MBA/MSCR degree program. He graduated on May 16, 2014.
Mona Farroukh is the Program Coordinator for the Child & Adolescent Center and also the Director of the Domestic Violence Prevention Program at ACCESS.
Marriam Ismail is a Public Health Specialist at the ACCESS Community Health & Research Center, specialized in the coordination of the Substance Abuse Prevention Program.
Jehad Najda is a Medical Clinic Coordinator at the ACCESS Community Health & Research Center.
Heba Sobh is currently an undergraduate student at the University of Michigan-Dearborn pursuing her degree in Biochemistry with hopes to continue on to Pharmacy School.
Adnan Hammad is the Senior Director of the Community Health & Research Center at ACCESS and is the Chairman of the National and International Health Research Initiative.
Gregory Dalack is Associate Professor and Chair of the Department of Psychiatry at the University of Michigan.
References
- Ahmed SR, Kia-Keating M, Tsai KH. A Structural Model of racial Discrimination, Acculturative Stress, and Cultural Resources Among Arab American Adolescents. American Journal of Community Psychology. 2011 doi: 10.1007/s10464-011-9424-3. [DOI] [PubMed] [Google Scholar]
- Amer MM, Hovey JD. Anxiety and depression in a post-September 11 sample of Arabs in the USA. Social Psychiatry and Psychiatric Epidemiology. 2011 doi: 10.1007/s00127-011-0341-4. [DOI] [PubMed] [Google Scholar]
- Arab American Institute. National Arab American Demographics. [last accessed December 14, 2013];2013 Retrieved from < http://www.aaiusa.org/pages/demographics/>. [Google Scholar]
- Barney LJ, Griffiths KM, Christensen H, Jorm AF. The Self-Stigma of Depression Scale (SSDS): development and psychometric evaluation of a new instrument. International Journal of Methods in Psychiatric Research. 2010;19(4):243–254. doi: 10.1002/mpr.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cale R. Childhood Obesity Prevention [Video] [last accessed December 14, 2013];2009 Retrieved December 20, 2011, from < http://youtu.be/7ccrwb_s9Kg>. [Google Scholar]
- Centers for Disease Control and Prevention. [last accessed December 14, 2013];2011 Retrieved from < http://www.cdc.gov/Features/dsDepression/>.
- Christie Clinic. Mental Health Awareness Month [Video] [last accessed December 14, 2013];2011 Retrieved December 20, 2011, from < http://youtu.be/tRucxfKYgxE>. [Google Scholar]
- Corrigan PW. How stigma interferes with mental health care. American Psychologist. 2004;59:614–625. doi: 10.1037/0003-066X.59.7.614. [DOI] [PubMed] [Google Scholar]
- Federal Interagency Forum on Child and Family Statistics. [last accessed December 14, 2013];2012 Retrieved July 30, 2012, from < http://www.childstats.gov/americaschildren/tables/health4a.asp?popup=true>.
- Karam EG, Mneimneh ZN, Karam AN, Fayyed JA, Nasser SC, Chatterji S, Kessler RC. Prevalence and treatment of mental disorders in Lebanon: a national epidemiological survey. The Lancet. 2006;367:25–31. doi: 10.1016/S0140-6736(06)68427-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kira IA, Hammad A. The Effects of Stigma Consciousness on Mental Health. Ethnicity & Disease. 2005;15(1) Suppl 1:S1–S104. [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a Brief Depression Severity Measure. Journal of General Internal Medicine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naber N. Ambiguous insiders: an investigation of Arab American invisibility. Ethnic and Racial Studies. 2000;23:37–61. [Google Scholar]
- Penn DL, Couture SM. Strategies for reducing stigma toward persons with mental illness. World Psychiatry. 2002;1(1):20–21. [PMC free article] [PubMed] [Google Scholar]
- Richardson LP, McCauley E, Grossman DC, McCarty CA, Richards JR, Russo JE, Rockhill C, Katon W. Evaluation of the Patient Health Questionnaire-9 Item for Detecting Major Depression Among Adolescents. Pediatrics. 2010;126:1117. doi: 10.1542/peds.2010-0852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rickwood DJ, Deane FP, Wilson CJ. When and how do young people seek professional help for mental health problems? The Medical Journal of Australia. 2007;187:35–39. doi: 10.5694/j.1326-5377.2007.tb01334.x. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Global Health Risks: Mortality and burden of disease attributable to selected major risks. [last accessed December 14, 2013];2009 Retrieved from < http://www.who.int/healthinfo/global_burden_disease/GlobalHealthRisks_report_full.pdf>.