Abstract
Background
Researchers have demonstrated moderate evidence for the use of exercise in the treatment of subacromial impingement syndrome (SAIS). Recent evidence also supports eccentric exercise for patients with lower extremity and wrist tendinopathies. However, only a few investigators have examined the effects of eccentric exercise on patients with rotator cuff tendinopathy.
Purpose
To compare the effectiveness of an eccentric progressive resistance exercise (PRE) intervention to a concentric PRE intervention in adults with SAIS.
Study Design
Randomized Clinical Trial
Methods
Thirty‐four participants with SAIS were randomized into concentric (n = 16, mean age: 48.6 ± 14.6 years) and eccentric (n = 18, mean age: 50.1 ± 16.9 years) exercise groups. Supervised rotator cuff and scapular PRE's were performed twice a week for eight weeks. A daily home program of shoulder stretching and active range of motion (AROM) exercises was performed by both groups. The outcome measures of the Disabilities of the Arm, Shoulder, and Hand (DASH) score, pain‐free arm scapular plane elevation AROM, pain‐free shoulder abduction and external rotation (ER) strength were assessed at baseline, week five, and week eight of the study.
Results
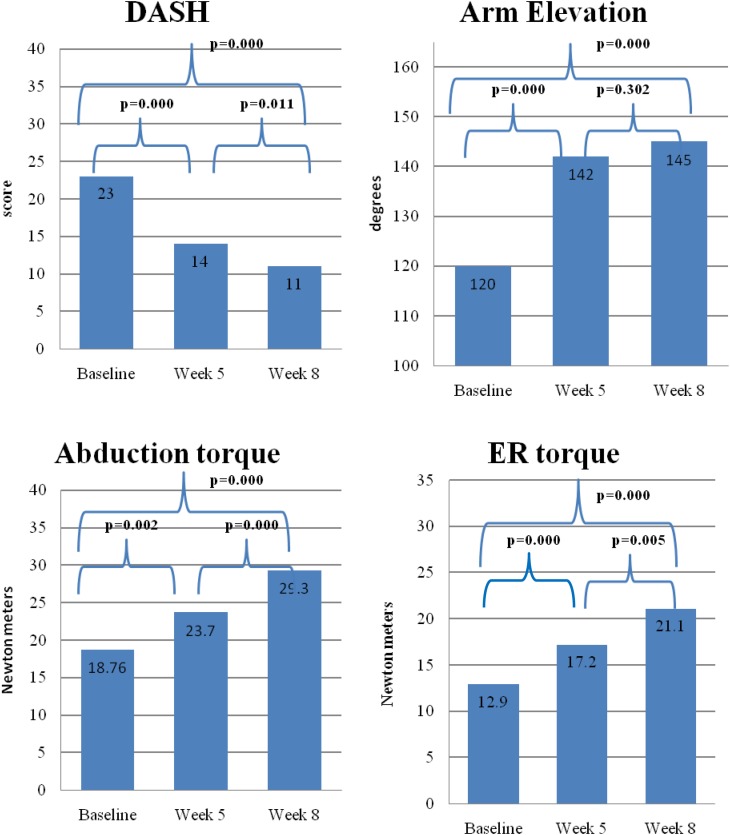
Four separate 2x3 ANOVAs with repeated measures showed no significant difference in any outcome measure between the two groups over time. However, all participants made significant improvements in all outcome measures from baseline to week five (p < 0.0125). Significant improvements also were found from week five to week eight (p < 0.0125) for all outcome measures except scapular plane elevation AROM.
Conclusion
Both eccentric and concentric PRE programs resulted in improved function, AROM, and strength in patients with SAIS. However, no difference was found between the two exercise modes, suggesting that therapists may use exercises that utilize either exercise mode in their treatment of SAIS.
Level of evidence
Therapy, level 1b
Keywords: Physical therapy, rotator cuff, shoulder, strengthening
INTRODUCTION
Disorders of the shoulder complex; which includes the clavicular, scapulothoracic, and glenohumeral articulations, have been suggested to be the third most common cause of musculoskeletal consultation in primary care with the most common shoulder diagnosis being subacromial impingement syndrome (SAIS).1-3 Moderate evidence supports the use of therapeutic exercise in the treatment of SAIS.4-8 More specifically, the results of exercise intervention studies targeting the rotator cuff and scapular muscles demonstrate significant pain reduction and functional improvement in the short term, as well as functional improvement in the long term in patients with SAIS.7,9,10 However, these studies of interventions for SAIS have used a wide variety of types and modes of exercises, mostly using concentric and eccentric contractions with elastic bands, machine weights, and free weights.11-16 Furthermore, the authors of those studies compared their exercise programs to other treatment modalities such as injections, surgery, and manual therapy or have compared supervised versus home exercises programs, but none compared types of resistive exercises to determine which is most effective in the treatment of SAIS.
Studies of rotator cuff and knee extensor muscles in asymptomatic individuals and rat tendons have demonstrated greater cross‐sectional area, increased fascicle length, greater neuromuscular activation, greater strength and peak torque, increased tendon collagen synthesis, and stabilization of angiogenesis with eccentric exercise.17-23 Based on these findings, clinicians are increasing their use of eccentric exercise in the treatment of tendinopathies. Recent studies by investigators who have used eccentric exercise in treatment of Achilles, patellar and wrist extensor tendinopathy have demonstrated greater pain reduction and improvement of function than concentric exercise.24-28
Three case series have been performed that examine the effect of eccentric exercise on patients with SAIS and have shown favorable outcomes, such as pain reduction and functional improvement when the eccentric exercises were included in the treatment plan.29-31 Furthermore, Maenhout et al found increased shoulder abduction strength when adding an eccentric full can exercise to concentric‐eccentric internal and external rotation (ER) exercises in a randomized clinical trial (RCT). However, no additional benefit was found for pain reduction or functional improvement.32 To the authors’ knowledge, no studies specifically have compared concentric and eccentric exercises in patients with SAIS. Therefore, the purpose of this study was to compare the effectiveness of an eccentric progressive resistance exercise (PRE) intervention to a concentric PRE interventions in adults with SAIS.
METHODS
Participants
An a‐priori power analysis was conducted using G*Power version 3.1.2 to estimate the sample size required to find statistically significant differences with a desired level of power set at 0.80 and an α‐level at 0.0125.33 Effect sizes of 0.55 to 1.06 were found in previous studies that investigated shoulder function using the Disabilities of the Arm, Shoulder, and Hand (DASH) as an outcome measure in persons with adhesive capsulitis, post acromioplasty, and impingement.34-36 However, a medium effect size of 0.25 was used for this study as a conservative estimate because the current study protocol included two exercise interventions and had no true control group which would likely result in a smaller effect size. An estimate of 38 participants, 19 participants per group, was required to ensure adequate power for an ANOVA with repeated measures.
Fifty‐five patients who were at least 18 years old and who had shoulder pain were recruited for this study from an urban, hospital‐based, outpatient rehabilitation center. Once patients agreed to participate in the study, they were asked to read and sign an informed consent in accordance with Institutional Review Board (IRB) requirements. Participants were excluded if they had a history of shoulder, cervical, or thoracic surgery, shoulder dislocation, fracture, labral tear, full‐thickness rotator cuff tear, adhesive capsulitis, rheumatic disease, pregnancy or medical condition that precluded them from performing resisted exercises. Participants who had pain level at or higher than 7/10 on the numeric pain rating scale (NPRS) were excluded from the study as this level of pain indicated a shoulder condition not likely to respond to exercise alone. Screening evaluation was performed by the primary investigator (PI), a licensed physical therapist and orthopaedic clinical specialist with over 22 years of experience. The screening evaluation included the Neer, Hawkins‐Kennedy, and coracoid (i.e. cross‐body) adduction impingement tests to confirm their impingement symptoms.37 The infraspinatus test, drop arm test, and “empty can” tests were used to rule out patients with a full thickness rotator cuff tear.37 Eligible participants were the patients who had at least one positive impingement test and one negative rotator cuff tear test. Participants with three positive rotator cuff tear tests were likely to have a full‐thickness rotator cuff tear, and were excluded from the study. After the screening examination, 38 out of 55 participants were eligible for the study.
Examiners and Treating Therapist
Seven examiners participated in the collection of outcome measurements. The examiners included four licensed physical therapists, two second‐year physical therapy doctoral students, and one licensed occupational therapist. The licensed clinicians averaged over 20 years of experience and included two certified hand therapists and two doctors of physical therapy. Prior to data collection, the PI met with the examiners and familiarized them with the testing protocol. The PI was the treating physical therapist for all participants.
Outcome Measures
Once participants were determined to be eligible for the study, they underwent a baseline outcome measure assessment. The baseline and follow‐up outcome measurements were assessed by an examiner who was blinded to the treatment group. The same examiner performed three testing sessions with each participant; at baseline, at week five, and at week eight. Participants were asked to stop taking pain medication four hours prior to their appointment on outcome assessment days to ensure accurate assessment of their pain‐free range of motion and strength. However, participants could take their pain medications as prescribed by their physician at all other times during the study. Each participant completed a baseline NPRS rating and the DASH functional outcome measure. As shown in Figure 1, participants also were assessed for pain‐free AROM of arm elevation in the scapular plane using a digital inclinometer in sitting following the method described by Kolber et al.38 Two trials of AROM measurements were recorded and the mean value of the two measurements was used for data analysis.
Figure 1.
Arm scapular elevation inclinometer measurement
Isometric strength for shoulder abduction and ER was assessed using an Accuforce Cadet hand‐held dynamometer (HHD) (Ametek Incorporated M & G Division, Largo, Florida). Both motions were tested in supine to minimize the effect of differing limb weight of participants. Abduction and ER were tested with the shoulder in 90 ° of abduction and 90 ° of elbow flexion.39 Resistance was applied perpendicular to the distal humerus just above the lateral epicondyle for abduction and perpendicular to the dorsal distal forearm one inch proximal to the ulnar styloid for ER (Figures 2 and 3). Participants held the aforementioned positions as the examiner applied force through the dynamometer using the “make” test procedure with the participant building up to maximal tension in one to two seconds and continuing to maintain the tension for four to five more seconds.39,40 Two measurements were taken for each of the two strength tests, with a 30‐second rest between the two measurements to allow for muscle recovery. The mean of the two measurements of each strength test was used for data analysis. The length of the limb from the lateral edge of the acromion to the lateral epicondyle and from one inch proximal to the ulnar styloid to the proximal olecranon was also recorded for calculating torque (N∙m). The four outcome measurements (DASH score, AROM of scapular plane elevation, shoulder abduction strength and shoulder ER strength) were performed again at the end of five and eight weeks of the supervised interventions.
Figure 2.
Abduction strength measurement with dynamometer
Figure 3.
External rotation strength measurement with dynamometer
Participant Allocation
Once the baseline outcome measurements were completed, participants were randomly assigned to one of the two intervention groups using pre‐prepared, sealed folders. Figure 4 illustrates the CONSORT diagram for participant recruitment, randomization and enrollment. One enrolled participant in the concentric group dropped out at three weeks due to an unrelated medical issue and was not included in the data analysis. Three additional participants in the concentric group withdrew after five weeks, one due to traveling out of state and two for financial and work conflict reasons. As a result, a total of 34 (91%) of the participants completed the 8‐week study and the final assessments, 16 in the concentric group and 18 in the eccentric group. An intention‐to‐treat analysis using the last observation carried forward method was performed for statistical analysis.
Figure 4.
The CONSORT diagram
Interventions
Both groups of participants completed a supervised PRE program two times a week for eight weeks. The first two weeks of the intervention involved both groups being familiarized with the exercise techniques and equipment, as well as a submaximal repetition maximum (RM) testing procedure in order to determine the resistance to be used during exercise sessions. Familiarization involved two sessions of instruction and performance of each exercise with a light resistance that did not cause pain and instruction by the PI in correct exercise technique in pain‐free ROM. The third week began the differentiation of treatment intervention of the eccentric and concentric intervention groups using the resistance predicted by the submaximal RM testing. Figure 5 illustrates the timing and flow of the exercise program and assessment sessions. Participants were instructed to perform only the exercises given as part of the study intervention and to avoid adding any new upper body activities until completion of the study. Participants also were informed that they were not to receive any other therapy or treatment for the involved shoulder during the study period.
Figure 5.
Procedure timing and exercise progression flow char
The exercises used in this study were chosen based on literature review of electromyographic (EMG) and biomechanical studies of exercises that optimize rotator cuff and scapular muscle recruitment.41-45 The exercises included the seated “full can”, sidelying internal rotation (IR), sidelying ER with towel roll, supine protraction, sidelying horizontal abduction, sidelying abduction, and prone shoulder extension in neutral rotation. All exercises (Appendix 1) were performed using a dumbbell, and were performed in the participant's pain‐free AROM. The eccentric exercise group performed the lowering portion of the exercises with the therapist repositioning the weight to the starting position to avoid resistance during the lifting (concentric) portion of each exercise. The concentric group performed the lifting portion of the exercises with the therapist repositioning the weight to the start position to avoid resistance in the lowering (eccentric) portion of the exercise. The PI was the treating physical therapist for all participants and was not involved in the outcome measure assessment in order to prevent bias of the results. Participant in both groups were given a home exercise program (HEP), consisting of pectoralis minor and posterior shoulder stretching, thoracic spine self‐mobilization into extension, and pain‐free AROM in flexion and abduction standing in front of a mirror to monitor for excessive scapular elevation. The primary purpose of the HEP was to address the soft tissue, joint, and capsular tightness commonly cited for contributing to poor scapular and glenohumeral biomechanics.46 Participants were asked to perform the HEP once daily on the days they did not exercise in the clinic, as well as part of the cool down exercises after clinic exercise sessions. In addition, participants were asked to keep an exercise log of their HEP performance, which was reviewed by the treating therapist at the end of each week to monitor compliance. This log was turned in at the completion of the study.
Repetition maximum assessment
The repetition maximum (RM) assessment was used to standardize the procedure for determining an appropriate weight for our participants’ shoulder exercises. Because the study participants had shoulder pain and pathology a submaximal 20RM testing procedure was used in order to minimize strain on the injured shoulder but still arrive at an appropriate exercise dosage using a standardized method. The commonly used 1 RM testing for healthy athletes would not be appropriate to use in patients with painful shoulders.47 Research has shown that the majority of injuries occur during the 1RM testing, not the PRE program itself.48 In order to reduce the risk of injury during RM testing, it has been suggested that the actual 1RM be predicted using an equation established from submaximal RM testing.47,49-51 In addition, it has been shown that older adults and novice exercisers require multiple assessments of the RM in order to obtain an accurate assessment.52-54 Therefore, participants in the current study underwent the 20RM testing procedure twice in week two. The better of the two 1RM predictions was used to determine the training resistance.
During the 20RM testing, the treating therapist initially selected a resistance that they anticipated would result in the participant's inability to lift with correct form or “fail” between 10 and 20 repetitions. This resistance selection was informed by the therapist's observation of the participant's exercise technique and muscle control during the familiarization sessions of week one. If the participant completed more than 20 repetitions at the chosen resistance, maintaining a speed of two to four seconds to lift and to lower, they rested for four minutes before trying again with a heavier resistance.47-55 The number of repetitions completed in the “failure” set was used in the Kemmler, Lauber, Wassermann (KLW) formula to predict the 1RM for each exercise.47 The KLW formula is (wi [0.988‐0.0000584 ri3 + 0.00190 ri2 + 0.0104 ri]) where wi is the load of measurement, and ri is the number of repetitions. This formula was shown to be an accurate predictor of 1RM across a number of repetitions up to 20.47 For each submaximal 20RM testing, a warm‐up consisting of five minutes on the UBE followed by one set of ten repetitions at 50% of the testing resistance was performed prior to the first testing trial for each exercise.
Exercise Progression
During the first session of week three, participants were instructed in the respective group exercises: either the concentric or eccentric portion of the training exercises. Both groups performed three sets of 12 repetitions of each of the seven intervention exercises at 70% of their newly predicted 1RM. Figure 5 illustrates the resistance training protocol and progression for each week of the study. If the training weight predicted by the formula fell between the dumbbell increments available in the clinic, the resistance was rounded down to the next closest dumbbell weight. Because the outcome assessments occurred again in the fifth and eighth week from enrollment, the submaximal 20RM testing was repeated at week four and at week six. Training resistance was adjusted in the sessions following the exercise testing sessions with participants performing three sets of 12 repetitions using resistance of 70% of the new predicted 1RM. In the week immediately prior to the next exercise testing session, the resistance was increased to 80% of the predicted 1RM.
STATISTICAL METHODS
The collected data was analyzed using SPSS Graduate Pack 22.0 (IBM Corp., Armonk, New York). Descriptive statistics were performed to illustrate the participant characteristics of gender, age, baseline DASH scores, baseline pain severity level, and duration of symptoms. Baseline age, DASH score, pain severity level, AROM, strength measurements and duration of symptoms were analyzed using t‐tests (p = 0.05) to determine if differences between the groups existed. Four separate 2x3 analyses of variance (ANOVA) with repeated measures were used to compare each of the four dependent variables between the groups at baseline, and after five weeks and eight weeks of exercise intervention. The α was set at 0.0125 after the adjustment for each ANOVA to minimize type I errors. Post hoc comparisons (p = 0.05) were performed when a significant difference was found.
RESULTS
Table 1 summarizes the characteristics of the participants in each group at baseline. The mean age for all participants was near 50 years with a range of 23 to 84 years. The mean symptom duration was just under two years. Baseline shoulder pain levels for all participants demonstrated a mean of 2.0 on the NPRS. Independent t‐tests performed on the baseline outcome measures, and the participants’ age and duration of symptoms data revealed no significant differences between the groups. The descriptive data for the outcome measures of DASH score, pain‐free scapular elevation AROM, pain‐free abduction torque, and pain‐free ER torque are presented in Table 2. The mean DASH score at baseline for all participants was 23.2 with the mean score improving in each of the subsequent time frames. Mean scaption AROM for all participants was 120 degrees indicating limited motion. The eight week mean improved to a functional 145 degrees. Abduction torque for all participants started at a mean of 18.7 N.m for all participants and increased to a mean of 29.2 N.m at the end of the eight week intervention. Similarly, the ER torque for all participants improved from a mean at baseline of 12.8 N.m to a mean of 21.2 N.m by the end of the intervention. The results of the ANOVAs showed no significant interaction of treatment group by time for all outcome measures: (a) DASH score (p = 0.890), (b) arm elevation AROM (p = 0.373), (c) abduction torque (p = 0.421), and (d) ER torque (p = 0.933). The main effect of time was significant for all four outcome measures (p < 0.001). Post‐hoc analyses revealed significant improvements for all of the outcome measures from baseline to week five (p < 0.05), regardless of group assignment. All outcome measures except arm elevation AROM (p = 0.302) continued to show significant improvement from week five to week eight (p < 0.05). Figure 6 illustrates the results collected at baseline, week five and week eight for each of the four outcome measures.
TABLE 1.
Participant Characteristics and Outcome Measurements at Baseline
| Concentric Exercise (n=16) | Eccentric Exercise (n=18) | All (n=34) | |
|---|---|---|---|
| Gender (M/F) | 6/10 | 8/10 | 14/20 |
| Age (years) | 48.6 ± 14.6 | 50.1 ± 16.9 | 49.4 ± 15.6 |
| Involved shoulder (R/L) | 7/9 | 11/7 | 18/16 |
| Duration of symptoms (months) | 20.6 ± 26.6 | 28.2 ± 23.6 | 22.7 ± 24.3 |
| NPRS score | 2.1 ± 1.6 | 2.0 ± 1.8 | 2.0 ± 1.7 |
| DASH score | 21.2 ± 6.5 | 25.0 ± 10.6 | 23.2 ± 9.0 |
| Arm elevation AROM (°) | 125.0 ± 35.8 | 114.8 ± 37.5 | 119.6 ± 36.5 |
| Shoulder abduction torque (N∙m) | 17.9 ± 11.7 | 19.5 ± 12.4 | 18.7 ± 11.9 |
| Shoulder ER torque (N∙m) | 11.1 ± 10.3 | 14.4 ± 11.0 | 12.8 ± 10.6 |
Abbreviations: M = male; F = female; NPRS = Numeric Pain Rating Scale; DASH = Disabilities of the Arm, Shoulder, and Hand; AROM = active range of motion; ER,=external rotation
TABLE 2.
Outcome Measurements at Baseline, Week 5, and Week 8 assessments
| All (n = 34) | Concentric Exercise Group (n = 16) | Eccentric Exercise Group (n = 18) | |
|---|---|---|---|
| DASH | |||
| Baseline | 23.2 ± 9.0 | 21.2 ± 6.5 | 25.0 ± 10.6 |
| Week 5 | 13.8 ± 8.1 | 12.3 ± 7.1 | 15.1 ± 8.9 |
| Week 8 | 10.8 ± 9.8 | 9.3 ± 7.1 | 12.1 ± 11.7 |
| Arm elevation AROM (°) | |||
| Baseline | 119.6 ± 36.5 | 125.0 ± 35.8 | 114.8 ± 37.5 |
| Week 5 | 142.4 ± 23.5 | 142.9 ± 23.6 | 142.1 ± 24.1 |
| Week 8 | 145.0 ± 26.3 | 143.8 ± 30.4 | 146.2 ± 23.0 |
| Abduction torque (N∙m) | |||
| Baseline | 18.7 ± 11.9 | 17.9 ± 11.7 | 19.5 ± 12.4 |
| Week 5 | 23.8 ± 13.9 | 20.6 ± 12.5 | 26.5 ± 14.7 |
| Week 8 | 29.2 ± 17.2 | 27.0 ± 16.1 | 31.2 ± 18.3 |
| ER torque (N∙m) | |||
| Baseline | 12.8 ± 10.6 | 11.1 ± 10.3 | 14.4 ± 11.0 |
| Week 5 | 17.2 ± 12.5 | 15.0 ± 11.2 | 19.1 ± 13.5 |
| Week 8 | 21.2 ± 13.4 | 19.4 ± 13.6 | 22.7 ± 13.4 |
Abbreviations: DASH, Disabilities of the Arm, Shoulder, and Hand; AROM, active range of motion; ER, external rotation
Figure 6.
(Continued)
DISCUSSION
The results of this study revealed that there were no significant differences between the groups in strength, range of motion, or DASH scores, indicating that eccentric‐based exercises were not more effective than concentric‐based exercises for treating patients with SAIS. The results also revealed that the effect sizes were small for all four outcome measures: (a) DASH partial η2 = 0.002, (b) arm elevation ROM partial η2 = 0.024 (c) abduction torque partial η2 = 0.030 and (d) ER torque partial η2 = 0.003. These small values of effect size can be attributed to the lack of differences between the groups. These findings are contrary to the better outcomes that have been reported for eccentric exercise when eccentric exercise was used in the treatment of tendinopathy of the Achilles, patellar, and wrist extensor tendons.56-59 The aforementioned studies only assessed pain intensity and self‐reported functional level, but did not assess strength or ROM. In addition, the eccentric exercises in the Achilles and patellar tendon studies were performed daily into the painful ROM and using body weight resistance on a single limb. One wrist extensor study used isokinetic exercises and another released a twisted rubber bar. Therefore, a direct comparison could not be made as the exercise intensity, load, and frequency used in these studies were different from those used in the current study. Maenhout et al32 reported better shoulder abduction strength in the eccentric group after 12 weeks of intervention. However, similar to the findings of the current study, Maenhout et al32 did not find a significant difference in functional scores using the Shoulder Pain and Disability Index (SPADI). The difference in exercise resistance level and number of different eccentric exercises performed could account for the different findings in group strength differences between the current study and the Maenhout et al study.32
The resistance load and volume of exercise in the current study was the same for both groups in terms of percentage of predicted 1RM used and number of sets and repetitions performed. Submaximal eccentric resistance (70‐80% of predicted concentric 1RM) was used to lessen the possibility of pain or injury during exercise in the participants. As a result, the concentric group may have been challenged at a different intensity than the eccentric group, as 70% of the concentric 1RM could have been easier to lower than to lift. Eccentric exercise in the training of healthy adults often involves supramaximal resistance in order to elicit muscle strength and mass gains.23 Many studies of eccentric exercise effects in other tendinopathies have used resistance that placed participants above the pain threshold.31,57,60 This approach is thought to have a greater effect on tendon properties and healing. However, the use of exercise beyond the pain threshold and use of supramaximal resistance are not feasible or reasonable for patients who have painful shoulders. Investigators who have examined the effects of eccentric exercise on muscles and tendons most recently suggest that the changes in the tissues are mainly due to resistance training load and intensity rather than contraction type, thus challenging the clinical belief in the superiority of eccentric training over concentric training.61,62 Future studies should compare similar exercise loads and intensities of the same contraction type and match intensity levels of concentric and eccentric exercises more closely in order to obtain a better comparison.
The results of this study demonstrated a significant main effect of time on all four outcome measures, indicating that all participants (both groups) made significant improvements after eight weeks for all of the outcome measures. These findings agree with the findings of the other authors who used resistance exercise in the treatment of SAIS that resulted in improved function and improved strength.29-31 Post‐hoc analysis also revealed that all of the outcome measures demonstrated significant improvement from baseline to week five with the greatest change in scapular elevation AROM and function (DASH scores) occurring in that time frame. The mean improvement in the DASH scores exceeded the minimal clinically important difference (MCID) of 10 points by the week five assessment with only an additional three points improvement at week eight.34,35 From week five to week eight, all participants continued to make significant improvements in all outcome measures except scapular elevation AROM. The findings of this study suggest that significant ROM and functional improvements occurred primarily in the first five weeks of PRE treatment approaching normal limits in that time frame. Strength gains improved in that same five week time frame but continued to improve even after ROM and functional scores were no longer improving significantly. However, without a true control group, one cannot be certain if these improvements were due to our intervention or simply due to the normal course of the condition over time.
The use of a submaximal exercise testing protocol appears to be a safe method for selecting and progressing resistance for shoulder rehabilitation exercises. Many of the participants in this study were older adults who had no experience with resisted exercises. The inclusion of two sessions for exercise technique instruction and practice with light resistance prior to exercise testing resulted in no injury from exercise testing, indicating that submaximal RM testing could allow therapists to safely predict each individual's 1RM for each exercise. The prediction formula and procedures used in this study could provide a standardize approach for determining a starting resistance when patients with SAIS are ready for PRE exercises. In addition, this process of standardized exercise progression resulted in significant strength gains without increasing pain or causing injury. The methods used in the current study demonstrated appropriate exercise dosing to accomplish meaningful strength and functional gains in an efficient amount of time for patients with SAIS.
Limitations
There were several limitations in this study that may have impacted the findings. The use of dumbbell resistance as opposed to isokinetic resistance for the exercise intervention may have obscured significant differences in the outcome measures between the groups due to the inability to separate the concentric and eccentric phases as completely as one can with isokinetic exercise equipment. While the treating physical therapist in this study made every effort to isolate concentric or eccentric contractions performed by participants, it was not possible to completely prevent the participant from contracting their muscles or “helping” to perform the opposing contraction type during an isotonic free‐weight exercise. The intention of the current study was to develop an exercise program that can be used in any physical therapy clinic with equipment commonly found in the majority of facilities. Isokinetic equipment is more feasible for studies conducted in research facilities and is cost prohibitive for many small community physical therapy facilities. Several EMG studies have indicated that sidelying exercises actually showed greater recruitment of rotator cuff muscles with less recruitment of the deltoid and upper trapezius than prone lying exercises.42-44 The side‐lying position was used in this study for horizontal abduction and external rotation as a result of the findings of the EMG studies and because the older patient population in the current study had difficulty obtaining the prone position and stabilizing the trunk against a long resistance lever with prone exercises. The use of sidelying exercises for these motions may have impacted the recruitment of the midscapular and posterior rotator cuff muscles. Another limitation of this study was lack of a true control group that did not receive an intervention, thus it cannot be determined how much of the improvement in function, AROM, and strength of the shoulders in persons with SAIS was due to the natural course of the condition or due to the treatment interventions. Because the participants were referred to the clinic for treatment, it was not ethical to withhold treatment.
Conclusion
Both submaximal eccentric and concentric PREs resulted in improved function, AROM, and strength in patients with SAIS. However, no difference was found between the two exercise modes, suggesting that therapists may use exercises that utilize either exercise mode in their treatment of SAIS.
Appendix 1
Figures of Exercises used during interventions
REFERENCES
- 1.Dinnes J Loveman E McIntyre, et al. The effectiveness of diagnostic tests for the assessment of shoulder pain due to soft tissue disorders: A systematic review. Health Technol.Assess. 2003;7(29):iii‐1‐166. [DOI] [PubMed] [Google Scholar]
- 2.Pribicevic M Pollard H Bonello R. An epidemiologic survey of shoulder pain in chiropractic practice in australia. J. Manipulative Physiol. Ther. 2009;32(2):107‐117. [DOI] [PubMed] [Google Scholar]
- 3.van der Windt DA Koes BW De Jong BA, et al. Shoulder disorders in general practice: Incidence, patient characteristics, and management. Ann. Rheum Dis. 1995;54(12):959‐964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Green S Buchbinder R Hetrick S. Physiotherapy interventions for shoulder pain. Cochrane Database Syst. Rev. (Online). 2003;(2):CD004258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kelly SM Wrightson PA Meads CA. Clinical outcomes of exercise in the management of subacromial impingement syndrome: A systematic review. Clin Rehabil. 2010;24(2):99‐109. [DOI] [PubMed] [Google Scholar]
- 6.Kromer TO Tautenhahn UG de Bie RA, et al. Effects of physiotherapy in patients with shoulder impingement syndrome: A systematic review of the literature. J. Rehabil. Med.: Official Journal of the UEMS European Board of Physical and Rehabilitation Medicine. 2009;41(11):870‐880. [DOI] [PubMed] [Google Scholar]
- 7.Kuhn JE. Exercise in the treatment of rotator cuff impingement: A systematic review and a synthesized evidence‐based rehabilitation protocol. J. Shoulder Elbow Surg. 2009;18(1):138‐160. [DOI] [PubMed] [Google Scholar]
- 8.Trampas A Kitsios A. Exercise and manual therapy for the treatment of impingement syndrome of the shoulder: A systematic review. Physical Therapy Reviews. 2006;11(2):125‐142. [Google Scholar]
- 9.Hanratty CE McVeigh JG Kerr DP, et al. The effectiveness of physiotherapy exercises in subacromial impingement syndrome: A systematic review and meta‐analysis. Semin. Arthritis Rheum. 2012;42(3): 297‐316. [DOI] [PubMed] [Google Scholar]
- 10.Littlewood C Ashton J Chance‐Larsen K, et al. Exercise for rotator cuff tendinopathy: a systematic review. Physiotherapy. 2012;98(2): 101‐109. [DOI] [PubMed] [Google Scholar]
- 11.Bang MD, Deyle GD. Comparison of supervised exercise with and without manual physical therapy for patients with shoulder impingement syndrome. J. Orthop Sports Phys. Ther. 2000;30(3):126‐137. [DOI] [PubMed] [Google Scholar]
- 12.Bas¸kurt Z Bas¸kurt F. Gelecek N, et al. The effectiveness of scapular stabilization exercise in the patients with subacromial impingement syndrome. J.Back Musculoskelet. 2011;24(3):173‐179. [DOI] [PubMed] [Google Scholar]
- 13.Conroy DE Hayes KW. The effect of joint mobilization as a component of comprehensive treatment for primary shoulder impingement syndrome. J. Orthop Sports Phys. Ther. 1998;28(1): 3‐14. [DOI] [PubMed] [Google Scholar]
- 14.Lombardi I Jr Magri AG Fleury AM, et al. Progressive resistance training in patients with shoulder impingement syndrome: A randomized controlled trial. Arthritis Rheum. 2008;59(5):615‐622. [DOI] [PubMed] [Google Scholar]
- 15.Ludewig PM Borstad JD. Effects of a home exercise programme on shoulder pain and functional status in construction workers. Occup.Environ Med. 2003;60(11):841‐849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Senbursa G Baltaci G Atay A. Comparison of conservative treatment with and without manual physical therapy for patients with shoulder impingement syndrome: A prospective, randomized clinical trial. Knee Surg.Sports Traumatol. Arthrosc.: 2007;15(7):915‐921. [DOI] [PubMed] [Google Scholar]
- 17.Bast SC Vangsness CT Jr Takemura J, et al. The effects of concentric versus eccentric isokinetic strength training of the rotator cuff in the plane of the scapula at various speeds. Bulletin (Hospital for Joint Diseases (New York, N.Y.)), 1998;57(3):139‐144. [PubMed] [Google Scholar]
- 18.Guilhem G Cornu C Guevel A. Neuromuscular and muscle‐tendon system adaptations to isotonic and isokinetic eccentric exercise. Ann. Phys. Rehabil. Med., 2010;53(5):319‐341. [DOI] [PubMed] [Google Scholar]
- 19.Heinemeier KM Olesen JL Haddad F, et al. Expression of collagen and related growth factors in rat tendon and skeletal muscle in response to specific contraction types. J. Physiol., 2007;582(Pt 3):1303‐1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Higbie EJ Cureton KJ Warren GL 3rd, et al. Effects of concentric and eccentric training on muscle strength, cross‐sectional area, and neural activation. J. Appl.Physiol. (Bethesda, Md.: 1985), 1996;81(5):2173‐2181. [DOI] [PubMed] [Google Scholar]
- 21.Nakamura K Kitaoka K Tomita K. Effect of eccentric exercise on the healing process of injured patellar tendon in rats. J. Orthop. Sci., 2008;13(4): 371‐378. [DOI] [PubMed] [Google Scholar]
- 22.Reeves ND Maganaris CN Longo S, et al. Differential adaptations to eccentric versus conventional resistance training in older humans. Exp. Physiol., 2009;94(7):825‐833. [DOI] [PubMed] [Google Scholar]
- 23.Roig M O’Brien K. Kirk G, et al. The effects of eccentric versus concentric resistance training on muscle strength and mass in healthy adults: A systematic review with meta‐analysis. Brit J.Sport Med. 2009;43(8):556‐568. [DOI] [PubMed] [Google Scholar]
- 24.Andres BM Murrell GA. Treatment of tendinopathy: What works, what does not, and what is on the horizon. Clin. Orthop Relat. R. 2008;466(7):1539‐1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kingma JJ de Knikker R Wittink HM, et al. Eccentric overload training in patients with chronic achilles tendinopathy: A systematic review. Brit J.Sport Med. 2007;41(6):e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lorenzen J Kramer R Vogt PM, et al. Systematic review about eccentric training in chronic patella tendinopathy]. [Systematische Literaturanalyse uber exzentrisches Training bei chronischer Patellatendinopathie: Gibt es einen Standard?] Sportverletz. Sportsc. 2010; 24(4):198‐203. [DOI] [PubMed] [Google Scholar]
- 27.Malliaras P Maffulli N Garau G. Eccentric training programmes in the management of lateral elbow tendinopathy. Disabil.Rehabil. 2008;30(20‐22):1590‐1596. [DOI] [PubMed] [Google Scholar]
- 28.Woodley BL Newsham‐West RJ Baxter GD. Chronic tendinopathy: Effectiveness of eccentric exercise. Brit J.Sport Med. 2007;41(4):188‐98; discussion 199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bernhardsson S Klintberg IH Wendt GK. Evaluation of an exercise concept focusing on eccentric strength training of the rotator cuff for patients with subacromial impingement syndrome. Clin. Rehabil.. 2011;25(1):69‐78. [DOI] [PubMed] [Google Scholar]
- 30.Camargo PR Avila MA Alburquerque‐Sendin F, et al. Eccentric training for shoulder abductors improves pain, function and isokinetic performance in subjects with shoulder impingement syndrome: A case series. Rev. Bras. Fisioter. (Sao Carlos (Sao Paulo, Brazil. 2012;16(1):74‐83. [DOI] [PubMed] [Google Scholar]
- 31.Jonsson P Wahlstrom P Ohberg L, et al. Eccentric training in chronic painful impingement syndrome of the shoulder: Results of a pilot study. Knee Surg. Sport. Tr., A.:. 2006;14(1):76‐81. [DOI] [PubMed] [Google Scholar]
- 32.Maenhout AG Mahieu NN De Muynck M, et al. Does adding heavy load eccentric training to rehabilitation of patients with unilateral subacromial impingement result in better outcome? A randomized, clinical trial. Knee Surg. Sport. Tr., A. 2013:21(5):1158‐1167. [DOI] [PubMed] [Google Scholar]
- 33.Faul F Buchner A Erdfelder E, et al. G*Power (Version 3.1.2) [Computer software]. Universität Kiel, Germany; 2009.
- 34.Gummesson C Atroshi I Ekdahl C. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: Longitudinal construct validity and measuring self‐rated health change after surgery. BMC Musculoskelet Di. 2003;4:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Roy JS MacDermid JC Woodhouse LJ. Measuring shoulder function: a systematic review of four questionnaires. Arthritis Rheum. 2009; 61(5):623‐632. [DOI] [PubMed] [Google Scholar]
- 36.Staples MP Forbes A Green S, et al. Shoulder‐specific disability measures showed acceptable construct validity and responsiveness. J.Clin. Epidemiol, 2010;63(2):163‐170. [DOI] [PubMed] [Google Scholar]
- 37.Magee DJ. Orthopedic physical assessment. 5th Edition. St. Louis, MO: Saunders; 2008. [Google Scholar]
- 38.Kolber MJ Vega F Widmayer K, et al. The reliability and minimal detectable change of shoulder mobility measurements using a digital inclinometer. Physiother. Theory Prac. 2011;27(2):176‐184. [DOI] [PubMed] [Google Scholar]
- 39.Hayes K Walton JR Szomor ZL, et al. Reliability of 3 methods for assessing shoulder strength. J.Shoulder Elbow Surg. 2002; 11(1): 33‐39. [DOI] [PubMed] [Google Scholar]
- 40.Bohannon RW. Make tests and break tests of elbow flexor muscle strength. Phys Ther. 1988;68(2):193‐194. [DOI] [PubMed] [Google Scholar]
- 41.Moseley JB Jr Jobe FW Pink M, et al. EMG analysis of the scapular muscles during a shoulder rehabilitation program. Am. J.Sport. Med.. 1992;20(2):128‐134. [DOI] [PubMed] [Google Scholar]
- 42.Reinold MM Escamilla RF Wilk KE. Current concepts in the scientific and clinical rationale behind exercises for glenohumeral and scapulothoracic musculature. J. Orthop. Sports Phys Ther. 2009;39(2):105‐117. [DOI] [PubMed] [Google Scholar]
- 43.Reinold MM Macrina LC Wilk KE, et al. Electromyographic analysis of the supraspinatus and deltoid muscles during 3 common rehabilitation exercises. J.Ath. Training. 2007;42(4):464‐469. [PMC free article] [PubMed] [Google Scholar]
- 44.Reinold MM Wilk KE Fleisig GS, et al. Electromyographic analysis of the rotator cuff and deltoid musculature during common shoulder external rotation exercises. J. Orthop Sports Phys. Ther. 2004;34(7):385‐394. [DOI] [PubMed] [Google Scholar]
- 45.Townsend H Jobe FW Pink M, et al. Electromyographic analysis of the glenohumeral muscles during a baseball rehabilitation program. Am. J.Sport. Med. 1991;19(3):264‐272. [DOI] [PubMed] [Google Scholar]
- 46.Ludewig PM Reynolds JF. The association of scapular kinematics and glenohumeral joint pathologies. J. Orthop Sports Phys. Ther. 2009;39(2):90‐104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kemmler WK Lauber D Wassermann A, et al. Predicting maximal strength in trained postmenopausal woman. J.Strength Cond. Res. 2006; 20(4):838‐842. [DOI] [PubMed] [Google Scholar]
- 48.Pollock ML Carroll JF Graves JE, et al. Injuries and adherence to walk/jog and resistance training programs in the elderly. Med.Sci Sport.Exer. 1991;23(10):1194‐1200. [PubMed] [Google Scholar]
- 49.Mayhew JL Ball TE Arnold MD, et al. Relative muscular endurance performance as a predictor of bench press strength in college men and women. J.App Sport Sci Res. 1992;6(4): 200‐206. [Google Scholar]
- 50.Reynold JM Gordon TJ Robergs RA. Prediction of one repetition maximum strength from multiple repetition maximum testing and anthropometry. J.Strength Cond. Res 2006;20(3):584‐592. [DOI] [PubMed] [Google Scholar]
- 51.Wood TM Maddalozzo GF Harter RA. Accuracy of seven equations for predicting 1‐RM performance of apparently healthy, sedentary older adults. Meas. Phys. Educ.Exer. Sci.. 2002;6(2):67‐94. [Google Scholar]
- 52.Phillips WT Batterham AM Valenzuela JE, et al. Reliability of maximal strength testing in older adults. Arch.Phys. Med.Rehab. 2004;85(2):329‐334. [DOI] [PubMed] [Google Scholar]
- 53.Ploutz‐Snyder LL Giamis EL. Orientation and familiarization to 1RM strength testing in old and young women. J.Strength Cond. Res. 2001;15(4):519‐523. [PubMed] [Google Scholar]
- 54.DeBeliso M Harris C Spitzer‐Gibson T, et al. A comparison of periodised and fixed repetition training protocol on strength in older adults. J.Sci.Med. Sport. 2005; 8(2):190‐199. [DOI] [PubMed] [Google Scholar]
- 55.Wathen D. Load assignment. In T. R. Baechle (Ed.), Essentials of strength training and conditioning (pp. 435–446). Champaign, IL: Human Kinetics; 1994. [Google Scholar]
- 56.Croisier JL Foidart‐Dessalle M Tinant F, et al. An isokinetic eccentric programme for the management of chronic lateral epicondylar tendinopathy. Brit. J.Sports Med.. 2007;41(4):269‐275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jonsson P Alfredson H. Superior results with eccentric compared to concentric quadriceps training in patients with jumper's knee: A prospective randomised study. Brit. J.Sports Med. 2005;39(11): 847‐850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mafi N Lorentzon R Alfredson H. Superior short‐term results with eccentric calf muscle training compared to concentric training in a randomized prospective multicenter study on patients with chronic achilles tendinosis. Knee Surg.Sport Tr., A. 2001;9(1):42‐47. [DOI] [PubMed] [Google Scholar]
- 59.Tyler TF Thomas GC Nicholas SJ, et al. Addition of isolated wrist extensor eccentric exercise to standard treatment for chronic lateral epicondylosis: A prospective randomized trial. J.Shoulder Elbow Surg. 2010;19(6):917‐922. [DOI] [PubMed] [Google Scholar]
- 60.Alfredson H Pietila T Jonsson P, et al. Heavy‐load eccentric calf muscle training for the treatment of chronic achilles tendinosis. Am. J.Sports Med.. 1998;26(3):360‐366. [DOI] [PubMed] [Google Scholar]
- 61.Malliaras P Barton C Reeves N, et al. Achilles and patellar tendinopathy loading programmes. Sports Med.. 2013;43(4):267‐286. [DOI] [PubMed] [Google Scholar]
- 62.Malliaras P Kamal B Nowell A. et al. Patellar tendon adaptation in relation to load‐intensity and contraction type. J.Biomech. 2013;46(11):1893‐1899. [DOI] [PubMed] [Google Scholar]