Abstract
Background
Childhood lead poisoning is a public health problem gained widely attention for the health damage caused by lead exposure. Pediatrics defines lead poisoning as BLL of or higher than 10 μg/dL, which leads to harmful effects in nervous system, hematological system and urinary system. This study investigates the percentage of 0–18 year old Chinese population with blood lead level (BLL) ≥10 μg/dL during 1990–2012 by searching epidemiologic studies from electronic database focused on BLL in mainland China.
Methods
Epidemiologic studies about BLL in China mainland between January 1990 and October 2012 were searched from electronic databases including CNKI, CBM disc, Wanfang Data, Pubmed and Medline. Data extraction, data analysis and risk of bias assessments were performed.
Results
Fifty-five articles were included in analysis containing 200,002 subjects, covering 19 provinces, autonomous regions and municipalities. The corrected pooled rate by trim and fill method under random effect model was 9 % (95 CI: 6 %, 12 %). The corrected pooled lead poisoning rate by trim and fill method was 28.1 % (95 % CI: 21.6 %, 34.6 %) from data published during 1990–2000, much higher than the rate during 2001–2005 (10.5 %, 95 % CI: 6.4 %, 14.5 %) and the rate during 2006–2012 (5.3 %, 95 % CI: 3.7 %, 7 %). The corrected pooled lead poisoning percentage in eastern zone (4.3 %, 95 % CI: 2 %, 6.6 %) was slightly lower than that in western zone (5.8 %, 95 % CI: 3.2 %, 8.5 %) and much lower than in central zone (8.5 %, 95 % CI: 4.9 %, 12.1 %). The corrected pooled rate of population living around mining area (70 %, 95 % CI: 62.7 %, 77.3 %) was much higher than that of population in urban area (9.6 %, 95 % CI: 7.1 %, 12.1 %), suburban area (23.6 %, 95 % CI: 17 %, 30.3 %), rural area (23.8 %, 95 % CI: 6.7 %, 40.9 %) and industrial area (57.5 %, 95 % CI: 28 %, 86.9 %). In male population, the corrected pooled rate (10 %, 95 % CI: 7 %, 13 %) was slightly higher than that in female population (7.7 %, 95 % CI: 5 %, 10.4 %). Considering different age groups, the lead poisoning prevalence gradually rose with the increase of age and reached peak level at preschool age, then declined slightly with age.
Conclusion
This meta-analysis revealed lead exposure situation of Chinese population in recent decades which provide robust evidence for policy making.
Background
Lead is a toxic heavy metal and can cause damage to human organs and tissues, particularly to the development of central nervous system. Lead exposure in children might cause permanent learning and behavior disorders [1, 2]. Diagnosis of lead exposure is based on blood lead level (BLL) [3]. The American Academy of Pediatrics defines lead poisoning as BLL of or higher than 10 μg/dL [4]. Thus, the U.S. Centers for Disease Control and Prevention and World Health Organization stated that a BLL of 10 μg/dL or above needs to be concerned. However, lead exposure may have harmful effects on multiple organs even at lower levels [5, 6].
Data from National Health and Nutrition Examination Survey (NHANES) in USA indicated that an estimated percentage of BLL ≥10 μg/dL in children aged 1–5 years was 88 % during 1976–1980, then fell sharply to 4.4 % during 1991–1994, to 1.6 % during 1999–2002, and to 0.8 % during 2007–2010 [7–10]. In developed countries, children living in poor families with lower educational level are at higher risk of elevated BLL [8–11]. The situation is similar in the developing countries. Among Central and South American children, the percentage of children with BLL ≥10 μg/dL is 33 ~ 34 % [12]. The world disease burden from lead poisoning in Western Pacific accounts for about one fifth, and in Southeast Asia accounts for another fifth [12].
The Chinese government has begun to pay attention to childhood lead poisoning since 1990s, and at mean time Chinese scholars have conducted a couple of epidemiological studies to investigate childhood lead poisoning in local areas of China. To provide convincing evidence for policy making regarding children lead poisoning prevention, this study investigated the national trend of lead poisoning rate in the 0–18 year old of Chinese population during 1990–2012 by analyzing the published data.
Methods
Literature searching strategy
We searched epidemiologic studies about BLL in China mainland from electronic databases, CNKI, CBM disc, Wanfang Data, Pubmed and Medline between January 1990 and October 2012. The searching strategy was “blood lead level” OR “lead poisoning” in Chinese and English language. Two authors firstly screened articles by reading the titles and abstracts, and then reviewed the full text of the eligible publications.
Literature quality assessment
The assessing criteria based on the standard recommended by Agency for Healthcare Research and Quality (AHRQ) containing nine items was used to evaluate literature quality [13]. The principals of literature quality assessment were described in Table 1. Two authors evaluated each eligible article independently. The discrepancy between two authors was solved through discussion.
Table 1.
Assessment of observing study quality based on the standard recommended by AHRQ
| Assessing principala | |
|---|---|
| Study question clearly focused | |
| Sampling of Study Population (Random, Convenient, Self-selected) | |
| Clear definition of including or excluding criteria | |
| Clear definition of research time | |
| Assessment of confounding effects of various factors (for example, age of the patients, patient sex) | |
| Appropriate measure of precision | |
| Clear description of response rate | |
| Clear description of dealing with missing data | |
| Conclusions supported by results with possible bias and limitations taken into consideration |
ascoring method: yes = 1; no or not mentioned = 0
Inclusion criteria
1. Study subjects were not the specific lead exposure population; 2. Sample size should be not less than 100 (for neonatal, not less than 50); 3. BLL detection was under strict quality control; 4. Results must comprise the number of the subjects and number of lead poisoning subjects. Lead poisoning is defined as BLL ≥ 10 μg/dL in the studies included.
Data extraction
Two authors did data entry independently and cross-checked. The following details were recorded: authors, title, study year, study site, sample type, testing method, sample size, age range, gender, number of the subjects and number of lead poisoning subjects.
Data analysis
Heterogeneity was assessed by Cochran chi-square (χ2) and quantified with the I2 statistic, which was low when I2 was less than 25 %, moderate when between 25 % ~ 50 %, high when more than 50 % [14]. Considering heterogeneity across studies, a random-effects model was used to calculate pooled lead poisoning rate and 95 % confidence intervals (CIs). DerSimonian and Laird method might be a robust approach to combine weighted effect size under random-effects model. Subgroup analysis was used to deal with heterogeneity. Publication bias was evaluated by Begg’s Test and Egger’s test [15]. Significance was set at a P value less than 0.05. Stata version 12.0 (StataCorp, College Station, Texas, USA) was used for all statistical calculations.
Results
Searching result
Four hundred eighty-three articles were retrieved after searching the medical databases illustrated above. One hundred twenty-eight articles were excluded due to no English abstract. Two hundred thirty-nine articles were excluded due to lack of strict quality control of BLL test method. Atomic absorption spectrometry (AAS), inductively coupled plasma mass spectrometry (ICP-MS) and anodic stripping voltammetry (ASV) were acceptable BLL test methods in this study. Strict quality control (QC) should be performed in sample collection to avoid contamination. A daily QC procedure of library should be performed and at least two controls of low (<10 ug/dL) and high lead (>20 ug/dL) levels should be tested to ensure the validity of test results. The acceptable range for detecting accuracy should not be greater than ±4 ug/dL or ±10 %. For testing precision, the relative standard deviation (RSD) should not be more than 15 % when blood lead level between 2 to 10 ug/dL, and not be more than 10 % when level above 10 ug/dL. The libraries were participated in the external quality assessment (EQA) of the national center for clinical laboratory. Four articles did not mention BLL test method. Eight articles were repeated publication. Two articles were ineligible due to insufficient sample size. The remaining 102 articles were assessed of study quality by evaluation standard, which was recommended by Agency for Healthcare Research and Quality (AHRQ) [13]. Mean evaluated score of study quality was about four. The 55 articles above or equal to four scores were included in this study (Fig. 1, Table 2). All the included studies contained 200,002 subjects, covering 19 provinces, autonomous regions and municipalities. The characteristics of included studies were showed in Table 3 [16–70].
Fig. 1.
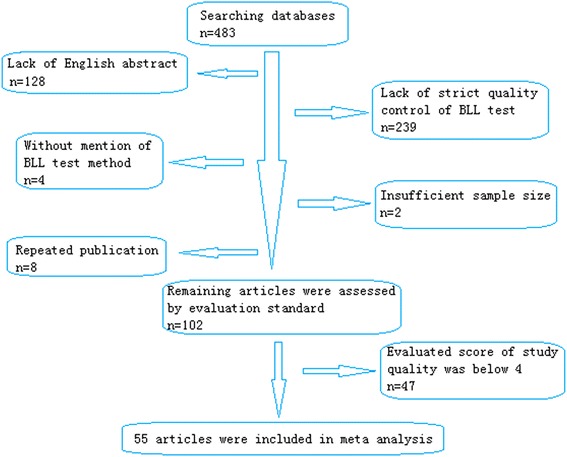
Flow diagram of the study selection process
Table 2.
Characteristics of included studies, by researching regions
| Eastern zone18–50 | Central zone51–56 | Western zone57–68 | National wide69–72 | |
|---|---|---|---|---|
| Number of studies | 33 | 6 | 12 | 4 |
| Published year | ||||
| 1990–2000 | 9 | 1 | 5 | 0 |
| 2001–2005 | 15 | 4 | 3 | 4 |
| 2006–2012 | 9 | 1 | 4 | 0 |
| Sample size | ||||
| <500 | 8 | 2 | 7 | 0 |
| 500–1499 | 15 | 3 | 3 | 0 |
| 1500–2999 | 8 | 1 | 1 | 0 |
| ≥3000 | 2 | 0 | 1 | 4 |
Table 3.
Information and data extracted from 55 publications in China
| Survey time | Sites | Testing methoda | Sample size | Districs (Sample size) | Age range |
|---|---|---|---|---|---|
| 2010 | Guangdong province | 1 | 1517 | 0–14 years | |
| 2003 | Foshan | 2 | 5175 | 3–6 years | |
| 2003 | Henan province | 2 | 527 | urban (251) | 3–5 years |
| industrial (276) | |||||
| 2003 | Foshan | 2 | 588 | urban (346) | newborn |
| suburban (242) | |||||
| 2006 | Nanjing | 1 | 404 | urban (404) | 9–12 years |
| 2008 | Ya’an | 1 | 703 | 0–12 years | |
| 2001 | Henan province | 1 | 585 | 0–6 years | |
| 2005 | Tai’an | 1 | 1200 | 7–12 years | |
| 2004 | Xuzhou | 1 | 1070 | 0–6 years | |
| 1997 | Guangxi province | 1 | 1508 | urban (1508) | newborn |
| 1993 | Shanghai | 1 | 348 | urban (348) | newborn |
| 1997 | Zhejiang province | 1 | 1320 | Urban (1024) | 0–6 years |
| suburban (296) | |||||
| 1997 | Beijing | 1 | 270 | urban (270) | 0–18 months |
| 2006 | Hohhot | 1 | 585 | 7–12 years | |
| 2005 | Urumqi | 1 | 987 | urban (987) | 6–10 years |
| 2004 | linyi | 1 | 1228 | urban (1228) | 2–6 years |
| 2004 | Guangzhou | 1 | 1215 | urban (1215) | 0–6 years |
| 2008 | Nanjing | 1 | 1258 | urban (1258) | 3–6 years |
| 2004–2006 | China | 1 | 44,045 | urban (44,045) | 0–6 years |
| 2005 | China | 1 | 17,141 | urban (17,141) | 0–6 years |
| 2010 | Guangzhou | 1 | 2464 | urban (2464) | 0–6 years |
| 2005 | Lishui | 1 | 2369 | urban (2369) | 3–6 years |
| 2006 | Anshan | 1 | 408 | urban (408) | 3–6 years |
| 2002 | Foshan | 2 | 152 | newborn | |
| 2002 | Guangzhou | 2 | 653 | urban (653) | 0–6 years |
| 2003 | Wuhu | 2 | 300 | urban (193) | 3–5 years |
| suburban (47) | |||||
| industrial (56) | |||||
| 2002 | Guangzhou | 2 | 1905 | urban (1518) | 3–14 years |
| rural (387) | |||||
| 2002 | Anshan | 1 | 913 | urban (150) | 0–6 years |
| suburban (150) | |||||
| industrial (300) | |||||
| mining (150) | |||||
| 2001 | Beijing | 1 | 2262 | 0–6 years | |
| 2004 | Jinchang | 1 | 256 | 2–7 years | |
| 2002 | Lanzhou | 1 | 262 | 0–3 years | |
| 1998 | Lanzhou | 1 | 103 | urban (103) | newborn |
| 2000 | Urumqi | 1 | 138 | newborn | |
| 2001 | Taiyuan | 1 | 395 | 4–6 years | |
| 1998 | Lanzhou | 1 | 160 | 3–6 years | |
| 1997 | Wuxi | 1 | 1249 | 0–5 years | |
| 2010 | Nanjing | 1 | 1113 | urban (1113) | 7–12 years |
| 2010 | Hunan province | 1 | 2044 | Urban (2044) | 2–6 years |
| 2011 | Kunming | 1 | 100 | newborn | |
| 2004 | Zhejiang province | 1 | 240 | 3–6 years | |
| 2008 | Shanghai | 1 | 1652 | newborn | |
| 2007 | Guangzhou and Shenzhen | 2 | 761 | urban (430) | 2–12 years |
| suburban (257) | |||||
| rural (74) | |||||
| 2011 | Guangzhou | 2 | 1570 | 6–14 years | |
| 2000 | Guiyang | 1 | 366 | 9–11 years | |
| 2004 | Jintan | 1 | 1344 | urban (933) | 3–5 years |
| suburban (187) | |||||
| rural (150) | |||||
| 1999 | Ningbo | 1 | 1018 | urban (1018) | 2–6 years |
| 1997–1999 | Shanghai | 1 | 5933 | 1–6 years | |
| 2008 | Chengdu | 1 | 4436 | 0–7 years | |
| 2004–2008 | China | 1 | 69,968 | urban (69,968) | 0–6 years |
| 2002 | China | 2 | 6502 | urban (6502) | 3–5 years |
| 1997 | Wuxi | 1 | 1117 | urban (589) | 1–5 years |
| suburban (528) | |||||
| 2004–2008 | Beijing | 1 | 5018 | urban (5018) | 0–6 years |
| 1993 | Shanghai | 1 | 132 | urban (132) | newborn |
| 1993 | Beijing | 1 | 141 | urban (141) | newborn |
| 2000 | Nanchang | 1 | 883 | urban (883) | 2–8 years |
a1-AAS;2-ICPMS
Pooled analysis of lead poisoning rate in Chinese population from data published during 1990–2012
Fifty-five studies were included in pooled analysis of unadjusted lead poisoning rate. Homogeneity test showed high heterogeneity between studies (χ2 = 17151.45, p = 0.000, I2 = 99.7 %). Under random effect-model, combined lead poisoning rate in the 0–18 year old Chinese population from data published during 1990–2012 was 25 % (95 % CI: 23 %, 28 %) (Fig. 2). Begg’s Test and Egger’s test showed the existence of publication bias (p < 0.05). Trim and fill method was used to provide an estimate of the number of missing studies and adjusted the pooled effect size for the publication bias [71]. In this article, 24 studies with the lead poisoning rates from 10 to 66 % were filled and used in the following analyses based on Trim and fill method. An adjusted intervention effect under random effect model was 9 % (95 CI: 6 %, 12 %) when 24 studies were supplemented.
Fig. 2.
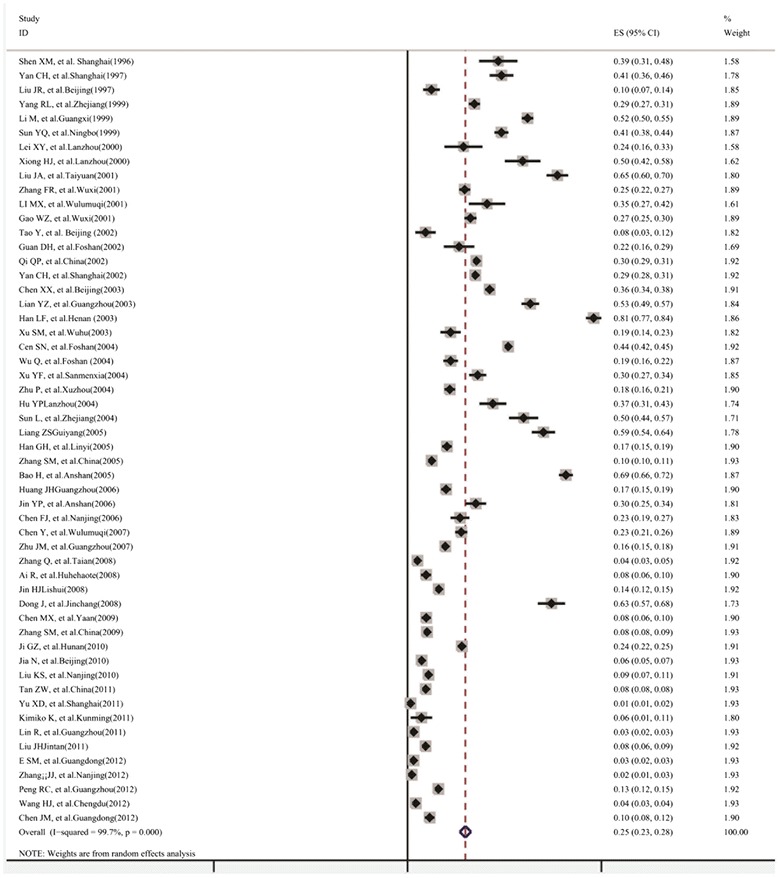
Forest plot of pooled analysis of lead poisoning rate in the 0–18 year old Chinese population during 1990–2012
The high heterogeneity might be associated with discrepancy of time, study sites, gender and age ranges of included studies. To deal with heterogeneity, subgroup analysis was used which was based on study year ranges, different economic zones, gender and different age ranges. Table 4 described pooled lead poisoning rates which corrected by trim and fill method due to publication bias in different subgroups, such as different published year ranges, economic zones, gender and age ranges groups respectively.
Table 4.
Lead poisoning rate according to published year, different economic zones, gender and different age ranges
| Subgroup | Pooled rate (95 % CI) (%) | Sample size | Heterogeneity test | P | I2 |
|---|---|---|---|---|---|
| Published year | |||||
| 1990–2000 | 28.1 % (21.6 %, 34.6 %) | 13,804 | 845.98 | <0.05 | 98.2 % |
| 2001–2005 | 10.5 % (6.4 %, 14.5 %) | 111,663 | 9525 | <0.05 | 99.7 % |
| 2006–2012 | 5.3 % (3.7 %, 7 %) | 73,629 | 1560.91 | <0.05 | 98.7 % |
| Economical zones | |||||
| Eastern zone | 4.3 % (2 %, 6.6 %) | 99,896 | 14819.93 | <0.05 | 99.5 % |
| Central zone | 8.5 % (4.8 %, 12.1 %) | 50,543 | 4572.20 | <0.05 | 99.3 % |
| Western zone | 5.8 % (3.2 %, 8.5 %) | 48,393 | 3956.12 | <0.05 | 99.1 % |
| Districs | |||||
| Urban area | 9.6 % (7.1 %, 12.1 %) | 167,058 | 6980.4 | <0.05 | 99.5 % |
| Suburban area | 23.6 % (17 %, 30.3 %) | 2555 | 114.22 | <0.05 | 93.9 % |
| Rural area | 23.8 % (6.7 %, 40.9 %) | 1416 | 184.99 | <0.05 | 98.4 % |
| Industrial area | 57.5 % (28 %, 86.9 %) | 937 | 403.16 | <0.05 | 99.3 % |
| Mining area | 70 %a (62.7 %, 77.3 %) | 150 | 0 | <0.05 | |
| Sex | |||||
| Male | 10 % (7 %, 13 %) | 100,036 | 3676.19 | <0.05 | 99.4 % |
| Female | 7.7 % (5 %, 10.4 %) | 82,754 | 2947.68 | <0.05 | 99.2 % |
| Age range | |||||
| Newborn (born-1 month) | 3.3 % (0, 14.8 %) | 4978 | 1970.40 | <0.05 | 99.5 % |
| Infant(1 month–1 year old) | 4.7 % (2.8 %, 6.7 %) | 11,551 | 125.12 | <0.05 | 90.4 % |
| Toddler (1–3 years old) | 7.4 % (4.8 %, 10 %) | 28,324 | 1532.99 | <0.05 | 97.7 % |
| Pre-school age (3–6 year old) | 9.5 % (7.8 %, 11.2 %) | 99,735 | 3623.39 | <0.05 | 98.2 % |
| school age (6–12 years old) | 6.7 % (4.7 %, 8.6 %) | 20,873 | 825.25 | <0.05 | 95.6 % |
| Adolescence (>12 years old) | 7 % (0, 13 %) | 435 | 17.99 | <0.05 | 88.9 % |
aThe data is a constant for only one literature included
The factor of time
The corrected pooled lead poisoning rate by trim and fill method was 28.1 % (95 % CI: 21.6 %, 34.6 %) from data published during 1990–2000, much higher than the rate during 2001–2005 (10.5 %, 95 % CI: 6.4 %, 14.5 %) and the rate during 2006–2012 (5.3 %, 95 % CI: 3.7 %, 7 %). Figure 3 showed an overall decreasing temporal trend of lead poisoning rate with study year through analysis tool of moving average line. The tendency of lead poisoning rate showed that the rate increased gradually in the 1990s, and dropped slowly during 2000–2003, then decreased rapidly after 2003.
Fig. 3.
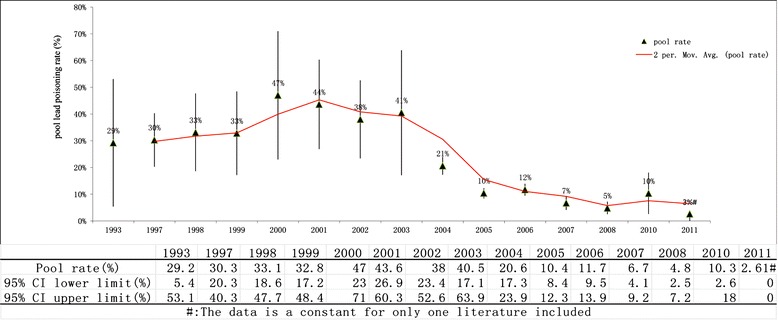
The temporal trend of lead poisoning rate in the 0–18 year old Chinese population during 1990–2012
The factor of different economic zones
According to economic level and geographic area, the provinces, autonomous regions and municipalities in mainland China are categorized into three zones: eastern, central and western. 1). The eastern zone includes Beijing, Tianjin, Hebei, Shanghai, Jiangsu, Zhejiang, Fujian, Shandong, Guangdong, Hainan and Liaoning. 2). The central zone includes Shanxi, Anhui, Jiangxi, Henan, Hubei, Hunan, Jilin and Heilongjiang. 3). The western zone includes Inner Mongolia, Guangxi, Chongqing, Sichuan, Guizhou, Yunan, Tibet, Shanxxi, Gansu, Qinghai, Ningxia and Xinjiang [72]. The corrected pooled lead poisoning percentage in eastern zone (4.3 %, 95 % CI: 2 %, 6.6 %) was slightly lower than that in western zone (5.8 %, 95 % CI: 3.2 %, 8.5 %) and much lower than in central zone (8.5 %, 95 % CI: 4.9 %, 12.1 %). An interact effect between economic zones and study year ranges on rate of BLL ≥ 10 μg/dL was noted when analyzing variance model with weighed least squares method (WLS) by sample size of included studies was applied (p < 0.05). When considering the effect of economic level on rate of BLL ≥ 10 μg/dL, all temporal tendencies of the rate were decreasing among three economic zones as showed in Fig. 4. But it should be highlighted that the relatively slower declining tendency in central zone compared to those in western zone and eastern zone.
Fig. 4.
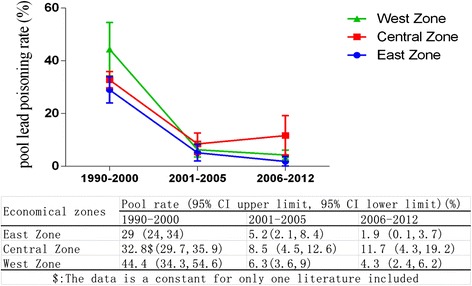
The temporal trend of lead poisoning rates among three economic zones in China main land
The factor of living districts
Only one literature reported that the lead poisoning rate among population living around mining area was 70 % (95 % CI: 62.7 %, 77.3 %) which was much higher than the corrected pooled rates in urban area (9.6 %, 95 % CI: 7.1 %, 12.1 %), suburban area (23.6 %, 95 % CI: 17 %, 30.3 %), rural area (23.8 %, 95 % CI: 6.7 %, 40.9 %) and industrial area (57.5 %, 95 % CI: 28 %, 86.9 %) from data published during 1990–2000. Figure 5 showed lead poisoning rates among different districts.
Fig. 5.
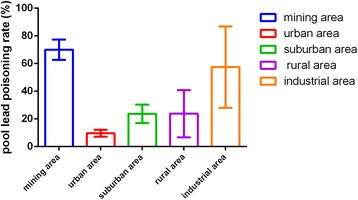
The pooled lead poisoning rates among different districts
The factor of gender
Gender information was available in 21 studies. The corrected pooled lead poisoning rate by trim and fill method of male population aged 0–18 year old in China (10 %, 95 % CI: 7 %, 13 %) was slightly higher than that of female (7.7 %, 95 % CI: 5 %, 10.4 %).
The factor of age range
The corrected lead poisoning rate by trim and fill method of preschool children between 3 to 6 years old (9.5 %, 95 % CI: 7.8 %, 11.2 %) was higher than that of other age ranges including newborn (3.3 %, 95 % CI: 0 %, 14.8 %), infant (4.7 %, 95 % CI: 2.8 %, 6.7 %), toddler under 3 years old (7.4 %, 95 % CI: 4.8 %, 10 %), school age between 6 to 12 years old (6.7 %, 95 % CI: 4.7 %, 8.6 %) and adolescence (7 %, 95 % CI: 0, 13 %). The lead poisoning rate of population aged 0–18 year old indicated lead exposure level. Figure 6 presented that the lead poisoning rate gradually rose with the increase of age and reached peak level at preschool age, then declined slightly with age. The temporal trends of lead poisoning rate in different age groups showed that the downward trend of prevalence with year was more obvious in population above 3 years old compared to population under 3 years old (Fig. 7).
Fig. 6.
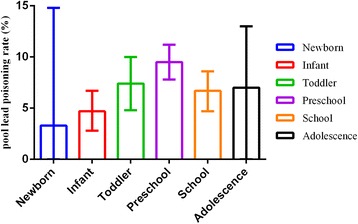
The pooled lead poisoning rate with different age ranges
Fig. 7.
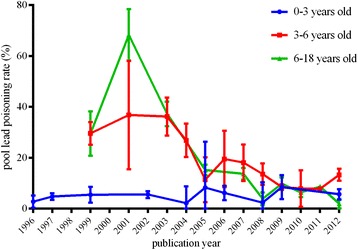
The pooled lead poisoning rate in different age group over the years
Discussion
With increasing number of epidemiological studies about BLL in China in recent years, it is now possible to obtain direct evidence of lead poisoning situation of Chinese population aged 0–18 years old. Based on strict inclusion criteria, eliminated relative low-quality studies by quality assessment of cross-sectional study, we identified 55 articles in this meta-analysis including 200,002 subjects, covering 19 provinces, autonomous regions and municipalities, thus the large population guaranteed the reliability of this study.
In this study, pooled rate of BLL ≥10 μg/dL in the 0–18 year old Chinese population during 1990–2012 was 25.1 % and corrected pooled rate under trim and fill method was 9 %, both much higher than all levels during 1991–1994 (4.4 %), 1999–2002 (1.6 %) and 2007–2010 (0.8 %) in US [8–10].
Considering high heterogeneity, subgroup analysis of different study year ranges showed overall decreasing trend of the rate with time. The decline appears to be attributed to government efforts of controlling lead pollution, including the phasing out of leaded gasoline, converting household fuel from coal to natural gas or other clean energy alternatives, and shutting down heavily polluted enterprises. But this study revealed that during 1993–2000 of survey time when leaded gasoline was not prohibited in China mainland and China had been undergoing rapid and drastic industrial development, tendency of lead poisoning rate was slightly increasing with time [43]. After early 21 century when leaded gasoline was gradually phased out in China mainland, the results showed steadily decreasing trend of the rate with time [73]. This result was consistent with studies conducted in USA which revealed the close correlation between the decreasing use of gasoline with lead and sharply declining BLL simultaneously [74, 75]. In the age of leaded gasoline, the lead dust mainly attributed to the exhaust of leaded gasoline and diesel fuel, while the lead-free gasoline brought down the atmosphere lead concentration [76–78].
Although the Chinese government and researchers continued to pay efforts to lead poisoning control and take preventative measurements for several decades, the study found that the declining tendency of lead poisoning rate was slow in the short term during 2000–2003. Several factors contributed to that as below. Though atmospheric lead emission from vehicle exhaust was decreasing rapidly in short period of time after unleaded gasoline application in China, it was hard to eliminate the lead accumulated in the soil in short time, which caused environmental pollution and potential lead exposure to high risk population, such as children and women [79, 80]. After 2003 of survey time, the rate was decreasing rapidly from about 40 to 2.61 % in 2011. Although the rate of BLL ≥10 μg/dL gradually declined with time, in this study pooled rate was 8 % from data published during 2006–2012, still much higher than that (0.8 %) observed in the surveys conducted in USA from 2007 to 2010 [10]. One of the key factors contributed to this observation in China might be the increasing lead discharge from the industrial emission [81]. The data showed that coal consumption, as the most important contributing factor of the lead discharge, continued to rise in recent decades in China [81].
When considering the factor of economic level, we found that pooled rate of BLL ≥10 μg/dL in eastern zone was slightly higher than that in the other two zones and still presented a sharp decreasing tendency since 2000. It is well known that low family income was a statistically significant independent predictor of elevated children’s BLL [8]. According to the data of Chinese statistical inspection, the annual per-capita income of people in eastern China was much higher than that in western China [82]. However, the slightly increasing tendency of lead poisoning rate in central zone since 2000 should be explained cautiously for a small quantity of epidemiological data. During 2006–2010, only five studies were included in this meta-analysis and rate of BLL ≥10 μg/dL in Hunan province was 24 % which accounted for a relatively large weight in pooled analysis [52].
Pooled lead poisoning rate of male population aged 0–18 years old (24.9 %) was slightly higher than that of female, which was similar to what was observed in the third National Health and Nutrition Examination Surveys (NHANES III) during 1999–2004 in USA [8]. It might be associated with more outdoor activity for male population, which leads to higher risk of lead exposure. As for age factor, the lead poisoning percentage peaked at pre-school age (3–6 year old) and then declined with age, similar to the result of analogical study in Chinese population, but not consistent with the result of previous studies in which the percentage of BLL ≥10 μg/dL was higher in children aged 1 to 2 years old than 3–5 years old, which needs to be explored further [8, 82].
There were several limitations needed to be classified: (a) for the coverage of evidence base, adequate epidemiological surveys encompassing the geographical, racial, economic, cultural, social diversity of nation as a whole were required. In this meta-analysis, the number of national wide surveys was small and data was missing during the periods of 1990–2000 and 2006–2012. The data from poor rural areas was limited, and this might cause underestimation of the pooled rate; (b) homogeneity test showed high heterogeneity between studies. The heterogeneity was still high within subgroups, which might be influenced by other factors, such as geographical distribution, living environment, living habits and ethnicities [83, 84]; (c) in this meta-analysis, publication bias still exists, which might be caused by investigator’s loss of interest in the topics with null (negative or inconclusive) results, editor’s preference to articles with positive results, etc. [85, 86]. The publication bias in this study might lead to overestimation of the rate of BLL ≥10 μg/dL. Thus, trim and fill method should be applied to correct the pooled effect size by supplementing 24 studies [71].
Conclusions
In conclusion, the overall rate of BLL ≥10 μg/dL in Chinese population aged 0–18 years old during 1990–2012 presented persistent declining trend along with time. Pooled percentage was slightly lower in eastern zone than other two economic zones. The rate was slightly higher in male population than in female population. The lead poisoning rate of Chinese population during postnatal period climbed from infancy, peaked at pre-school age and then declined with age. This meta-analysis revealed lead exposure situation of Chinese population in recent decades which provide robust evidence for policy making.
Acknowledgments
This work was supported by the National Basic Research Program of China (“973”Program, 2012CB525001), Public Welfare Project of the Chinese Ministry of Health (201002001, 201002006). We thank Prof. S.L. Tong and Prof. F.X. Ouyang for help with data analysis and revised the manuscript.
Abbreviation
- CI
Confidence interval
- BLL
Blood lead level
- NHANES
National Health and Nutrition Examination Survey
- AHRQ
Agency for Healthcare Research and Quality
- WLS
Weighed least squares
- AAS
Atomic absorption spectrometry
- ICPMS
Inductively coupled plasma mass spectrometry
Footnotes
Min-ming Li and Jia Cao contributed equally to this work.
Competing interests
The authors declare that they have no competing interests. All the authors have no financial relationships relevant to this article to disclose.
Authors’ contributions
ML: developed the protocol and search strategy, screened all records, extracted data, carried out the data analysis, interpreted results, and prepared the manuscript draft; JC: extracted data, screened all records, reviewed and revised the manuscript. ZG: extracted data, reviewed and revised the manuscript. XS: supervised the study, reviewed and revised the manuscript. CY: supervised the study, screened all records for eligibility, provided arbitration, reviewed and revised the manuscript. All authors read and approved the final manuscript.
Contributor Information
Min-ming Li, Email: minmingli@126.com.
Jia Cao, Email: cjhanru@163.com.
Zhen-yan Gao, Email: milijingling@163.com.
Xiao-ming Shen, Email: xmshen@shsmu.edu.cn.
Chong-huai Yan, Phone: +86-021-25078857, Email: yanch@shkeylab-ceh.org.
References
- 1.Lanphear BP, Hornung R, Khoury J, et al. Low-level environmental lead exposure and children’s intellectual function: an international pooled analysis. Environ Health Perspect. 2005;113(7):894–899. doi: 10.1289/ehp.7688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Landrigan PJ, Schechter CB, Lipton JM, Fahs MC, Schwartz J. Environmental pollutants and disease in American children. Environ Health Perspect. 2002;110(7):721–728. doi: 10.1289/ehp.02110721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pearson HA, Schonfeld DJ. Lead. In Rudolph CD: Rudolph’s Pediatrics (21st ed.). McGraw-Hill Professional. 2003. ISBN 0-8385-8285-0
- 4.Ragan P, Turner T. Working to prevent lead poisoning in children: getting the lead out. JAAPA. 2009;22(7):40–45. doi: 10.1097/01720610-200907000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Rossi E. Low level environmental lead exposure: a continuing challenge. Clin Biochem Rev. 2008;29(2):63–70. [PMC free article] [PubMed] [Google Scholar]
- 6.Barbosa JF, Tanus-Santos JE, Gerlach RF, Parsons PJ. A Critical Review of Biomarkers Used for Monitoring Human Exposure to Lead: Advantages, Limitations, and Future Needs. Environ Health Perspect. 2005;113(12):1669–1674. doi: 10.1289/ehp.7917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pirkle JL, Brody DJ, Gunter EW, et al. The decline of blood lead levels in the United States: the National Health and Nutrition Examination Surveys (NHANES) JAMA. 1994;272:284–291. doi: 10.1001/jama.1994.03520040046039. [DOI] [PubMed] [Google Scholar]
- 8.Jones RL, Homa DM, Meyer PA, et al. Trends in blood lead levels and blood lead testing among US children aged 1 to 5 years, 1988–2004. Pediatrics. 2009;123:376–385. doi: 10.1542/peds.2007-3608. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention (CDC) Blood lead levels—United States, 1999–2002. MMWR. 2005;54:513–516. [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention (CDC) Blood Lead Levels in Children Aged 1–5 Years-United States, 1999–2010. MMWR. 2013;62(13):245–248. [PMC free article] [PubMed] [Google Scholar]
- 11.Pokras MA, Kneeland MR. Lead poisoning: using transdisciplinary approaches to solve an ancient problem. Ecohealth. 2008;5(3):379–385. doi: 10.1007/s10393-008-0177-x. [DOI] [PubMed] [Google Scholar]
- 12.Payne M. Lead in drinking water. Can Med Assoc J. 2008;179(3):253–254. doi: 10.1503/cmaj.071483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kane RL, Shamliyan T, Mueller C, Duval S, Wilt T. Nursing Staffing and Quality of Patient Care. Evidence Report/Technology Assessment No. 151 (Prepared by the Minnesota Evidence based Practice Center under Contract No. 290-02-0009.) AHRQ Publication No.07-E005. Rockville, MD: Agency for Healthcare Research and Quality.; 2007. [Google Scholar]
- 14.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta analysis. Sta Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 15.Rothstcin HR, Sutton AJ, Borenstcin M. Publication Bias in Meta-Analysis: Prevention, Assessment and Adjustments. [M] ©2005 John Wiley& Sons, Ltd, October 2005, Online ISBN: 9780470870167, doi:10.1002/0470870168.
- 16.Chen XX, Teng HH, Wang FZ, et al. Blood Lead Level and Related Risk Factors Among Children Aged 0–6 Aears in Beijing. Chin J Epidemiol. 2003;24(10):868–871. [PubMed] [Google Scholar]
- 17.Jia N, Dai YH, Xie XY, Tan ZW. A surveillance of children’s blood lead levels in Beijing in 2004–2006 Chinese Journal of Woman and Child. Health Research. 2010;21(6):719–722. [Google Scholar]
- 18.Tao Y, Bai XT, Zhang HQ, Liu JR, Wang YL, Dong B. Variety Trend and Affect Factors Analysis on Blood Lead Level of Pregnant Women and Infants. China Public Health. 2002;18(1):58–60. [Google Scholar]
- 19.Liu JR, Qin XY, Bai XT, et al. Dynamic Study on Blood Lead Levels of Pregnant Women and Infants in a District of Beijing. [in Chinese] Journal of Hygiene Research. 1997;26(1):38–40. [PubMed] [Google Scholar]
- 20.Er SM, Chen C, Zeng JM, Hu GC. (2012) Blood Lead Levels of Children under 14 Years of Age from a Physical Examination in a Hospital in Guangzhou. J Environ Occup Med. 2012;29(7):441–442. [Google Scholar]
- 21.Wu Q, Cen SN, Guan DH, Guo XL. Blood Lead Level of Pregnant Women and Newborn. Maternal and Child Health Care of China. 2004;19(8):109–110. [Google Scholar]
- 22.Cen SN, Ou TF, Guan DH. The Relationship of Blood Lead Level of Preschool Children and Microelement. Chinese Journal of Practical Pediatrics. 2004;19(5):288–290. [Google Scholar]
- 23.Guan DH, Liu JA, Li FZ. Analysis on the Maternal and Umbilical Cord Blood Lead Levels in Foshan Area and Their Relative Factors. Guangdong Trace Elements Science. 2002;9(11):40–43. [Google Scholar]
- 24.Zhu JM, Ma WJ, Liang XX, Xu YH, Lian XW, Du DA. Blood Lead Level of Children aged 3–14 year old in Guangdong Province. Journal of Environment and Health. 2007;24(7):510–511. [Google Scholar]
- 25.Peng RC, Rao SQ, Wu RQ, Liu Y. Blood Lead Level and Influencing Factors among Children of 0–6 Years in Liwan District of Guangzhou. Medical Recapitulate. 2012;18(5):789–791. [Google Scholar]
- 26.Lian YZ, Chen DL, Lin LJ, Dai RD, Shi FY, Ou HQ. Investigation on Serum Pb of Children Aged 0 ~ 6Years Old from Dongshan District of Guangzhou. Guangdong Trace Elements Science. 2003;10(8):59–62. [Google Scholar]
- 27.Chen JM, Tong YP, Xu JZ. Environmental lead pollution threatens the children living in the Pearl River Delta region, China. Environ Sci Pollut Res. 2012;19:3268–3275. doi: 10.1007/s11356-012-0837-9. [DOI] [PubMed] [Google Scholar]
- 28.Huang JH. Investigation on blood lead level of children aged 0 ~ 6 yeas old from Guangzhou. Guangdong Trace Elements Science. 2006;13(3):35–38. [Google Scholar]
- 29.Lin R, Lin GZ, Wu JG, Lin L, Du L, Liu YY. Investigation on Blood Lead Levelamong school-aged children in Guangzhou. Chin J Sch Health. 2011;32(1):59–60. [Google Scholar]
- 30.Liu JH, Ai YX, McCauley L, et al. Blood lead levels and associated socio-demographic factors among preschool children in the South Eastern region of China. Paediatr Perinat Epidemiol. 2012;26:61–69. doi: 10.1111/j.1365-3016.2011.01234.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu KS, Hao JH, Gu PQ, Chen J. Detection of Blood Lead and Blood Cadmium Levels Among Pre-school Aged Children in Nanjing. J Prev Med Inf. 2010;26(10):773–774. [Google Scholar]
- 32.Chen FJ, Zhou ZX, Chi H, et al. Study on the relationship between the abnormal behavior and blood lead level of the children in Nanjing. Jiangsu Prev Med. 2006;17(3):10–11. [Google Scholar]
- 33.Zhang JJ, Ji LL, Zhou L, He YX, Chen LS, Chen XD. Investigation on blood lead level of children aged 7–12 years in Nanjing city. Jiangsu J Prev Med. 2012;23(4):19–20. [Google Scholar]
- 34.Gao WZ, Li Z, Kaufmann RB. Blood Lead Levels among Children Aged 1 to 5 Years in Wuxi City, China. Environmental Research Section A. 2001;87:11–19. doi: 10.1006/enrs.2001.4281. [DOI] [PubMed] [Google Scholar]
- 35.Zhang FR, Chen YF, Jiang XY, Zhu H, Yin YX. A study on relationship between blood lead level in children and fetal umbilical cord. Chin J Prev Med. 2001;35(1):42–43. [PubMed] [Google Scholar]
- 36.Zhu P, Li R, Tian LJ, Zhu M, Wen C. Study on blood lead and related factors in children of Xuzhou. Acta Academiae Medicinae Xuzhou. 2004;24(6):521–523. [Google Scholar]
- 37.Jin YP, Liao YJ, Lu CW. Health effects in children aged 3–6 years induced by environmental lead exposure. Ecotoxicol Environ Saf. 2006;63:313–317. doi: 10.1016/j.ecoenv.2005.05.011. [DOI] [PubMed] [Google Scholar]
- 38.Bao H, Meng J, Qu R, Zhao LY. Investigation on the level of blood lead and its influence factors for 0–6 children in Anshan Area. Strait J Prev Med. 2005;11(1):16–18. [Google Scholar]
- 39.Han GH, Lu L, Lu SL. A Survey On Blood Lead Level Of Pre-school Children in Linyi Urban District. Journal of Linyi Medical College. 2005;27(1):35–36. [Google Scholar]
- 40.Zhang Q, Xu YP. Blood lead level of preschool children and impact of lead exposure on children’s health. Journal of Taishan Medical College. 2008;29(10):792–794. [Google Scholar]
- 41.Yan CH, Shen XM, Ao LM, et al. Lead exposure level in cord blood and its related factors. Chin J Prev Med. 1997;31(1):9–12. [PubMed] [Google Scholar]
- 42.Yu XD, Yan CH, Shen XM. Prenatal exposure to multiple toxic heavy metals and neonatal neurobehavioral development in Shanghai. China Neurotoxicol Teratol. 2011;33:437–443. doi: 10.1016/j.ntt.2011.05.010. [DOI] [PubMed] [Google Scholar]
- 43.Shen XM, Yan CH, Zhou JD, et al. Relationship between lead content in umbilical blood and neurobehavioral development in infants. Chin J Prev Med. 1996;30(2):68–70. [PubMed] [Google Scholar]
- 44.Yan CH, Wu SH, Shen XM, et al. The trends of changes in children’s blood lead levels since the introduction of lead free gasoline in Shanghai. Chinese Journal of Epidemiology. 2002;23(3):172–174. [PubMed] [Google Scholar]
- 45.Sun L, Zhao ZY, Li L. Preschool children’s lead levels in rural communities of Zhejiang province. China Int J Hyg Environ Health. 2004;207:437–440. doi: 10.1078/1438-4639-00312. [DOI] [PubMed] [Google Scholar]
- 46.Yang RL, Zhao ZY, Chen CX, Li LT, Chen HY, Zhang RZ. Analysis of lead levels in 1320 pre-school children of Zhejiang Province. Journal of Zhejiang University. 1999;28(4):160–161. [Google Scholar]
- 47.Jin HJ. Exploration of relationship between blood lead level and height and weight of children aged 3 to 6 in Lishui city. Maternal and Child Health Care of China. 2008;23(4):557–558. [Google Scholar]
- 48.Sun YQ, Qian YY, Zhang YX, et al. Investigation on blood level and high-risk factors of children aged 2–6 in Ningbo. Ningbo Medical. 1999;11:101–102. [Google Scholar]
- 49.Xu SM, Chen K, Xia CS, et al. Blood lead level of children and influence factors of lead pollution in Wuhu. Chin J Dis Control Prev. 2003;7(5):414–415. [Google Scholar]
- 50.Han LF, Zhu G, Zhang BP, Wu HY, Li HB, Guo BC. Investigation on Children’s Blood Lead Level in Urban Areas of Henan Province. China Public Health. 2003;19(9):1098–1099. [Google Scholar]
- 51.Xu YF, Qiao YN, Cao HZ, et al. Epidemiological survey on lead content of blood for children aged0 ~ 6 years in western Henan province and its affecting factors. Chinese Journal of Child Health Care. 2004;12(2):133–137. [Google Scholar]
- 52.Ji GZ, Deng FM, Wu XY, et al. An epidemiologic survey on blood lead levels in preschool children living in towns of Hunan Province. Chin J Contemp Pediatr. 2010;12(8):645–648. [PubMed] [Google Scholar]
- 53.You ZH, Hu XG, Chao MX, et al. An investigation on blood lead level and affacting factors of 883 children in Nanchang City. Studies of Trace Elements and Health. 2001;18(2):53–55. [Google Scholar]
- 54.Liu JA, Liu DH, Jing J, Yi HQ, Huang ML, Chen XB. Blood lead levels of 395 preschool children in a residential district of Taiyuan city. Chin J School Health. 2001;22(1):7–8. [Google Scholar]
- 55.Dong J, Liu ZH, Xiong HJ. Study of the levels of lead and eight trace elements among preschool children in Jinchang. J Clin Pediatr. 2008;26(12):1063–1066. [Google Scholar]
- 56.Hu YP. A study on blood lead levels and affecting factors for lead poisoning of infants. Chinese Journal of Reproductive Health. 2004;15(1):15–17. [Google Scholar]
- 57.Xiong HJ, Lei XY, Zhao YF, Yuan BS, Li R, Niu JP. A study on the relationship between blood lead level and intelligence quotient in children. Chinese Journal of Practical Pediatrics. 2000;15(12):731–732. [Google Scholar]
- 58.Lei XY, Xiong HJ. Higher blood lead levels of neonates are associated with environmental factors. Chin J Pediatr. 2000;38(6):373–376. [Google Scholar]
- 59.Li M, Yang XQ, Chen SM, et al. Lead Exposure level in umbilical cord blood and its related factors. Journal of Guangxi Medical University. 1999;16(6):885–887. [Google Scholar]
- 60.Liang ZS. An epidemiological study on lead poison of children aged 9–11 years old in Guiyang. Henan J Prev Med. 2005;16(6):324–327. [Google Scholar]
- 61.Ai R, Yun X, Su YL, Zhu H, Li Z, Yang Y. A research of blood lead level and its effect about electrophysiology of brain in school-age children. Maternal and Child Health Care of China. 2008;23(18):2522–2523. [Google Scholar]
- 62.Wang HJ, Shi H, Chang L. Association of blood lead with calcium, iron, zinc and hemoglobin in children aged 0–7 years: a large population-based study. Biol Trace Elem Res. 2012;149:143–147. doi: 10.1007/s12011-012-9413-x. [DOI] [PubMed] [Google Scholar]
- 63.Chen MX, Qiu P, Zhao XS. Investigation and relevant factor analysis on the lead level of children aged 0 ~ 12 in Ya’an. Studies of Trace Elements and Health. 2009;26(2):17–18. [Google Scholar]
- 64.Li MX, Li WC, Guo YF, Zhu YP. The maternal and umbilical cord blood lead levels in Han and Uygur and analysis of its relative factors. Guangdong Trace Elements Science. 2001;8(10):19–23. [Google Scholar]
- 65.Chen Y, Li L, Cui J, Wang PD, Ar SY, Zhu Y. Blood lead level and the influencing factors between Uygur and Han children in Urumqi. Chin J Sch Health. 2007;28(4):344–345. [Google Scholar]
- 66.Kawata K, Yan L, Hao L, Zhang XQ, Ushijima H. Specific factors for prenatal lead exposure in the border area of China. Int J Hyg Environ Health. 2006;209:377–383. doi: 10.1016/j.ijheh.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 67.Zhang SM, Dai YH, Xie XH. Surveillance of childhood blood lead levels in 14 cities of China in 2004–2006. Biomed Environ Sci. 2009;22:288–296. doi: 10.1016/S0895-3988(09)60058-1. [DOI] [PubMed] [Google Scholar]
- 68.Tan ZW, Dai YH, Xie XY, Zhang SM, Fan CY, Jia N. Blood lead status and influencing factors among preschooI children in urban areas of China. Chin J Pediatr. 2011;49(4):294–300. [PubMed] [Google Scholar]
- 69.Qi QP, Yang YW, Yao XY, et al. Blood lead level of children in the urban areas in China. Chin J Epidemiol. 2002;23(3):162–166. [PubMed] [Google Scholar]
- 70.Zhang SM, Dai YH, Xie XH, Fan ZY, Tan ZW. Study on Blood Lead Level and Related Risk Factors Among Children Aged 0–6 years in 15 cities in China. Chin J Epidem. 2005;26(9):651–54. [PubMed] [Google Scholar]
- 71.Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455–463. doi: 10.1111/j.0006-341X.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 72.Zhang ZY, Liu AY, Yao SJ. Convergence of China’s regional incomes: 1952–1997 Convergence of China’s regional incomes: 1952–1997. China Econ Rev. 2001;12(2–3):243–258. doi: 10.1016/S1043-951X(01)00053-0. [DOI] [Google Scholar]
- 73.Yang GX. Mandatory national standard of automobile free-lead gasoline. China Standards Review. 2000;4:13–16. [Google Scholar]
- 74.Annest JL, Pirkle JL, Makuc D, Neese JW, Bayse DD, Kovar MG. Chronological trend in blood lead levels between 1976 and 1980. N Engl J Med. 1983;308(23):1373–1377. doi: 10.1056/NEJM198306093082301. [DOI] [PubMed] [Google Scholar]
- 75.U.S. EPA (Environmental Protection Agency) Costs and Benefits of Reducing Lead in Gasoline: Final Regulatory Impact Analysis. Washington, D.C: EPA-230-05-85-006. Office of Policy Analysis; 1985. [Google Scholar]
- 76.Chiaradia M, Gulson BL, James M, Jameson CW, Johnson D. Identification of secondary lead sources in the air of an urban environment. Atmos Environ. 1997;31(21):3511–3521. doi: 10.1016/S1352-2310(97)00218-5. [DOI] [Google Scholar]
- 77.Zhu BQ, Chen YW, Peng JH. Lead isotope geochemistry of the urban environment in the Pearl River Delta. Appl Geochem. 2001;16:409–417. doi: 10.1016/S0883-2927(01)00047-6. [DOI] [Google Scholar]
- 78.Zhang GL, Tan MG, Li XL, et al. Comprehensive Study of Lead Pollution in Atmospheric. Aerosol of Shanghai Environmental Science. 2006;27:831–836. [PubMed] [Google Scholar]
- 79.Zhang GL, Tan MG, Li XL, et al. Comprehensive Study of Lead Pollution in Atmospheric Aerosol of Shanghai. Environ Sci Technol. 2006;27(5):831–836. [PubMed] [Google Scholar]
- 80.Chen TB, Zheng YM, Chen H, Zheng GD. Background Concentrations of Soil Heavy Metals in Beijing. Environ Sci Technol. 2004;25(1):117–122. [PubMed] [Google Scholar]
- 81.Department of Industry and Transport Statistics, National Bureau of Statistics, Energy Bureau, National Development and Reform Commission. China Energy Statistical Yearbook. Beijing, China: China Statistics Press; 2007:83–124. [in Chinese].
- 82.National Bureau of Statistics of the People’s Republic of China. China Statistical Yearbook 2012, China Statistics Press. ISBN 978-7-5037-6693-0/C•2752 available: www.stats.gov.cn/tjsj/ndsj/.
- 83.Wang SQ, Zhang JL. Blood lead levels in children. China Environmental Research. 2006;101:412–418. doi: 10.1016/j.envres.2005.11.007. [DOI] [PubMed] [Google Scholar]
- 84.He K, Wang SQ, Zhang JL. Blood lead levels of children and its trend in China. Sci Total Environ. 2009;407:3986–3993. doi: 10.1016/j.scitotenv.2009.03.018. [DOI] [PubMed] [Google Scholar]
- 85.Easterbrook PJ, Berlin JA, Gopalan R, Matthews DR. Publication bias in clinical research. Lancet. 1991;337(8746):867–872. doi: 10.1016/0140-6736(91)90201-Y. [DOI] [PubMed] [Google Scholar]
- 86.Sackett DL. Bias in analytic research. J Chronic Dis. 1979;32(1–2):51–63. doi: 10.1016/0021-9681(79)90012-2. [DOI] [PubMed] [Google Scholar]


