Abstract
Context
Identifying neuromuscular screening factors for anterior cruciate ligament (ACL) injury is a critical step toward large-scale deployment of effective ACL injury-prevention programs. The Landing Error Scoring System (LESS) is a valid and reliable clinical assessment of jump-landing biomechanics.
Objective
To investigate the ability of the LESS to identify individuals at risk for ACL injury in an elite-youth soccer population.
Design
Cohort study.
Setting
Field-based functional movement screening performed at soccer practice facilities.
Patients or Other Participants
A total of 829 elite-youth soccer athletes (348 boys, 481 girls; age = 13.9 ± 1.8 years, age range = 11 to 18 years), of whom 25% (n = 207) were less than 13 years of age.
Intervention(s)
Baseline preseason testing for all participants consisted of a jump-landing task (3 trials). Participants were followed prospectively throughout their soccer seasons for diagnosis of ACL injuries (1217 athlete-seasons of follow-up).
Main Outcome Measure(s)
Landings were scored for “errors” in technique using the LESS. We used receiver operator characteristic curves to determine a cutpoint on the LESS. Sensitivity and specificity of the LESS in predicting ACL injury were assessed.
Results
Seven participants sustained ACL injuries during the follow-up period; the mechanism of injury was noncontact or indirect contact for all injuries. Uninjured participants had lower LESS scores (4.43 ± 1.71) than injured participants (6.24 ± 1.75; t1215 = −2.784, P = .005). The receiver operator characteristic curve analyses suggested that 5 was the optimal cutpoint for the LESS, generating a sensitivity of 86% and a specificity of 64%.
Conclusions
Despite sample-size limitations, the LESS showed potential as a screening tool to determine ACL injury risk in elite-youth soccer athletes.
Key Words: children, knee, biomechanics, movement patterns
Key Points
The Landing Error Scoring System (LESS) score may effectively identify elite-youth soccer athletes at higher risk of sustaining anterior cruciate ligament (ACL) injuries.
Elite-youth soccer athletes with LESS scores of 5 or more were at higher risk of sustaining ACL injuries than athletes with LESS scores less than 5.
Individuals with LESS scores of 5 or more may be targeted for ACL injury-prevention exercise programs.
Soccer is the most popular sport in the world, with more than 265 million participants. It is also one of the sports most commonly associated with athletic injury, such as to the anterior cruciate ligament (ACL). More than 25% of individuals with ACL injuries do not return to previous activity levels even after successful surgery and rehabilitation.1 Within 7 years after an ACL injury, 65% of individuals no longer play soccer.1 More than one-third of skeletally immature children also face challenges returning to sports such as soccer within 2 years of an ACL injury.2 Regardless of treatment, patients also have reported moderate to severe disability with walking (31%) and activities of daily living (44%).3,4 Adolescent female soccer players appear to be at greatest risk for negative long-term consequences, with more than 22% of these athletes undergoing either surgery to the contralateral knee or revision surgery during the 5-year period after the index surgery.5 Given that surgery and rehabilitation do not prevent long-term morbidity, the need to prevent ACL injuries in youth soccer athletes is great.
For effective injury prevention, prospective risk factors for injury should be established before preventive measures are introduced.6 Most theorized risk factors for ACL injury, such as sex, hormonal changes, notch width, and static postural alignment, are not modifiable through prevention efforts. Abnormal lower extremity biomechanics, however, are modifiable and are critical factors for study because they produce abnormal knee loading. Specifically, 3-dimensional knee loading, including knee-extension moment, proximal anterior tibial shear force, knee valgus-varus moment, and knee internal-external–rotation moment, often is implicated in ACL injury7,8 and imposes the greatest strain on the ACL.9,10 Data regarding ACL loading and injury mechanisms help clinicians understand what occurs at the time of injury.11 Prospective risk factors, however, provide information for identifying individuals at risk for sustaining injuries, potentially years before injury.11
Only a small body of evidence exists on prospective biomechanical risk factors for ACL injury. A limitation of these studies is the use of laboratory-based instrumentation and testing procedures.12,13 Whereas these instruments are the criterion standard for biomechanical measures, they are impractical in time and cost for large-scale mass screenings on the athletic field. To be feasible, a field-assessment tool for high-risk biomechanics should be brief; use minimal or inexpensive equipment; facilitate large-scale, field-based screening; and provide a valid and reliable measure of the biomechanics that predict injury.
The Landing Error Scoring System (LESS) is a field-assessment tool for identifying potentially high-risk movement patterns (“errors”) during a jump-landing maneuver. Padua et al14 demonstrated that the LESS has concurrent validity using 3-dimensional motion analysis and that good interrater and intrarater reliability can be obtained. However, few researchers15 have investigated the LESS as a prospective screening tool. Therefore, the purpose of our study was to examine the validity of the LESS (total score and individual items) in identifying individuals at risk for ACL injury in elite-youth soccer athletes. We hypothesized that higher LESS scores, representing a greater number of movement errors, would predict ACL injury in this population.
METHODS
Design and Participants
We used a prospective cohort design to evaluate the LESS as a predictor of ACL injury in elite-youth soccer athletes. Two soccer leagues (1 from North Carolina, 1 from Maryland) with under-11 to under-18 age divisions agreed to participate in the study. The 2 leagues competed in similar levels of competition and always on natural grass. All teams were simultaneously performing an injury-prevention program warm-up during this study.
A total of 829 participants (348 [42%] boys, 481 [58%] girls; age = 13.9 ± 1.8 years) were enrolled in this study: 565 (68%) from North Carolina (261 [46%] boys, 304 [54%] girls) and 264 (32%) from Maryland (87 [33%] boys, 177 [67%] girls). Of these participants, 207 (24.9%) were from 11 to 12 years of age. The group accumulated 1217 athlete-seasons of observation. At the initial test session, all participants were free from any injury or illness that prohibited competitive soccer activity. Participants and their legal guardians provided written informed assent and consent, respectively, before the initial test session. All procedures were approved by the Biomedical Institutional Review Board of the University of North Carolina at Chapel Hill.
Procedures
Each participant completed a baseline questionnaire and movement assessment at the beginning of each soccer season between August 2006 and January 2009. A brief baseline questionnaire addressed demographics and sport-related injury history. The movement assessment consisted of a jump-landing task that was graded using the LESS by video review at a later date. Returning athletes were retested at the start of their returning seasons using identical procedures.
All participants were monitored prospectively for ACL injury from the date of their enrollment (August 2006 through May 2009). A member of the research team visited each soccer team weekly during the monitoring period to record injuries that participants sustained. Coaches and participants were instructed to identify any participant who missed a soccer-related activity during the previous week due to an injury or an unknown reason. The research team member followed up with all participants with suspected injuries. All participants with reported ACL injuries completed a specific questionnaire to verify the injury and obtain information about the circumstances of injury. All reported ACL injuries were verified during surgical reconstruction and indicated on this self-reported questionnaire. Noncontact and indirect-contact ACL injuries were defined operationally as injuries that occurred without direct contact to the lower extremity from an external source at the time of injury. We defined noncontact mechanism of injury as an injury that did not involve contact with the participant. We defined indirect-contact mechanism of injury as an injury due to contact with a body part other than the knee (ie, trunk).
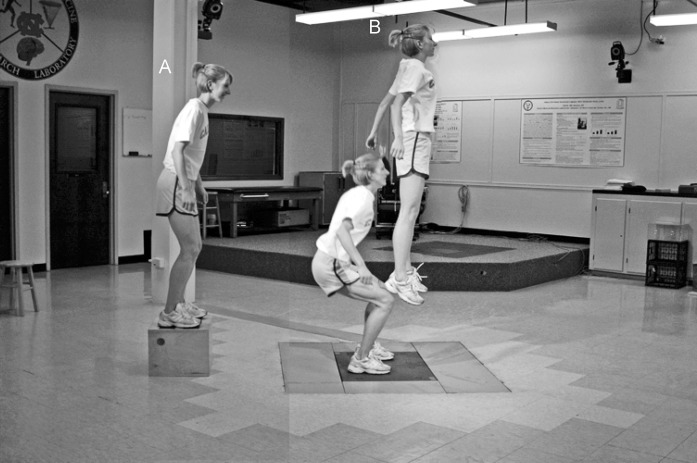
Jump-Landing Task
Participants performed 3 trials of a standardized jump-landing task during each test session on a soccer field before practice (Figure 1). The participant began the task standing on a 30-cm-high box placed at a distance of half the body height away from a landing area, which was marked by a line on the ground. Participants were instructed to jump forward so that both limbs left the box simultaneously, to land just past the line, and to jump for maximal height immediately after landing. They practiced until they were comfortable with the task and performed it correctly. Trials were excluded and repeated if the participants jumped vertically from the box or if they did not jump for maximal height upon landing. Two digital video cameras (model DCR-HC30; Sony Corporation of America, Park Ridge, NJ) were placed 10 ft (3 m) in front of and to the right of the participants to capture frontal and sagittal images of all jump-landing trials.14,16
Figure 1.
The standardized jump-landing task consists of 2 segments: A, participant jumps down from box and lands on ground; B, participant immediately jumps vertically as high as possible.
Data Reduction
Two research assistants (L.J.D., M.J.D.), who were blinded to injury status, graded the digital videos of all participants using the LESS and free computer software (QuickTime; Apple, Inc, Cupertino, CA). The LESS is a valid and reliable (interrater reliability: intraclass correlation coefficient [2,1] = 0.84, standard error of the mean = 0.71) clinical movement-analysis tool that evaluates specific jump-landing characteristics.14 Movements were analyzed at the initial contact frame, which was defined as the frame immediately before the foot was flat on the ground, and between initial contact and maximal knee flexion (Table 1). The LESS primarily uses a dichotomous scoring rubric to identify obvious movement errors, such as limited knee flexion or excessive medial knee displacement. Therefore, a 1-point differential in the total LESS score can be associated with moderate to large differences in certain biomechanical variables.14 A higher LESS score indicates a greater number of landing errors and consequently poorer jump-landing technique. The average LESS score from the 3 trials at each testing session was used for data analyses.
Table 1.
Operational Definitions for Individual Landing Error Scoring System Items
| Landing Error Scoring System Item |
Operational Definition of Error |
Scoring |
| Knee flexion: initial contact | The knee is flexed less than 30° at initial contact. | 0 = Absent |
| 1 = Present | ||
| Hip flexion: initial contact | The thigh is in line with the trunk at initial contact. | 0 = Absent |
| 1 = Present | ||
| Trunk flexion: initial contact | The trunk is vertical or extended on the hips at initial contact. | 0 = Absent |
| 1 = Present | ||
| Ankle plantar flexion: initial contact | The foot lands heel to toe or with a flat foot at initial contact. | 0 = Absent |
| 1 = Present | ||
| Medial knee position: initial contact | The center of the patella is medial to the midfoot at initial contact. | 0 = Absent |
| 1 = Present | ||
| Lateral trunk flexion: initial contact | The midline of the trunk is flexed to the left or the right side of the body at initial contact. | 0 = Absent |
| 1 = Present | ||
| Stance width: wide | The feet are positioned greater than shoulder width apart (acromion processes) at initial contact. | 0 = Absent |
| 1 = Present | ||
| Stance width: narrow | The feet are positioned less than shoulder width apart (acromion processes) at initial contact. | 0 = Absent |
| 1 = Present | ||
| Foot position: external rotation | The foot is externally rotated more than 30° between initial contact and maximum knee flexion. | 0 = Absent |
| 1 = Present | ||
| Foot position: internal rotation | The foot is internally rotated more than 30° between initial contact and maximum knee flexion. | 0 = Absent |
| 1 = Present | ||
| Symmetric initial foot contact: initial contact | One foot lands before the other foot or 1 foot lands heel to toe and the other foot lands toe to heel. | 0 = Absent |
| 1 = Present | ||
| Knee-flexion displacement | The knee flexes less than 45° between initial contact and maximum knee flexion. | 0 = Absent |
| 1 = Present | ||
| Hip-flexion displacement | The thigh does not flex more on the trunk between initial contact and maximum knee flexion. | 0 = Absent |
| 1 = Present | ||
| Trunk-flexion displacement | The trunk does not flex more between initial contact and maximum knee flexion. | 0 = Absent |
| 1 = Present | ||
| Medial-knee displacement | At the point of maximum medial knee position, the center of the patella is medial to the midfoot. | 0 = Absent |
| 1 = Present | ||
| Joint displacement | Soft: the participant demonstrates a large amount of trunk, hip, and knee displacement. | 0 = Soft |
| Average: the participant has some, but not a large amount of, trunk, hip, and knee displacement. | 1 = Average | |
| Stiff: the participant goes through very little, if any, trunk, hip, and knee displacement. | 2 = Stiff | |
| Overall impression | Excellent: the participant displays a soft landing with no frontal-plane or transverse-plane motion. | 0 = Excellent |
| Average: all other landings. | 1 = Average | |
| Poor: the participant displays large frontal-plane or transverse-plane motion, or the participant displays a stiff landing with some frontal-plane or transverse-plane motion. | 2 = Poor |
Statistical Analyses
Standard statistics for screening tests were used and included receiver operator characteristic curve analyses to select a test cutpoint, followed by computation of sensitivity and specificity. We compared mean LESS scores in the injured and uninjured participants using t tests. The 1-season risk of ACL injury in athletes whose screening was positive was divided by the 1-season risk of ACL injury in athletes whose screening was negative to compute the injury risk ratio. We used SPSS software (version 16.0; SPSS Inc, Chicago, IL) and SAS software (version 9.2; SAS Institute, Cary, NC) to analyze the data. Returning athletes contributed more than 1 season to the analysis, and multiple seasons were treated as statistically independent. Exact methods, such as the Fisher test, were used for analyses and confidence intervals (CIs). The α level was set at .05.
RESULTS
Seven participants sustained ACL injuries during follow-up (1 boy, 6 girls; age = 14.9 ± 0.7 years; age range, 13 to 17 years; Table 2). The mechanism of injury was indirect contact for 3 injuries and noncontact for 4 injuries. All injuries occurred during games. No participant who sustained an ACL injury had reported a previous lower extremity injury on the preseason baseline questionnaire.
Table 2.
Descriptive Characteristics of Participants Sustaining Anterior Cruciate Ligament Injury After Baseline Landing Error Scoring System Testing
| Characteristic |
Group |
||||||||
| Injured Participants (n = 7) |
Uninjured Participants (n = 820) |
||||||||
| Individual Participant |
Total |
||||||||
| Age, y | 15 | 17 | 14 | 17 | 15 | 13 | 13 | 14.9 ± 7.0a | 13.9 ± 1.8a |
| Sex | Female | Female | Female | Female | Male | Female | Female | 1 male, 6 females | 347 males, 475 females |
| Mechanism of injury | Indirect contact | Indirect contact | Noncontact | Noncontact | Noncontact | Indirect contact | Noncontact | 3 indirect contact, 4 noncontact | NA |
| Event | Game | Game | Game | Game | Game | Game | Game | Game | NA |
| Injured Landing Error Scoring System score | 5 | 9 | 3 | 5 | 7 | 7 | 8 | 6.24 ± 1.75 (4.62, 7.86)b | 4.43 ± 1.71 (4.34, 4.53)b |
| Previous Landing Error Scoring System score | NA | NA | 6 | NA | NA | 6 | NA | NA | NA |
Abbreviation: NA, not applicable.
Mean ± SD.
Mean ± SD (95% confidence interval).
Receiver Operator Characteristic Curve
The receiver operator characteristic analysis identified a LESS cutpoint of 5.17 as having optimal screening properties: 86% sensitivity and 71% specificity (Figure 2). The area under the curve was 0.78 (95% CI = 0.61, 0.95). The LESS is scored as a continuous variable; however, we do not consider that the LESS can be reliably and reproducibly scored to 1 decimal place in a clinical setting. Therefore, we selected the nearest whole number (5.00) as a clinically meaningful cutpoint. Use of the 5.00 cutpoint yielded the same sensitivity (86%; 95% CI = 42%, 99%) but reduced the specificity to 64% (95% CI = 62%, 67%). Given the very low incidence of ACL injury, the positive predictive value (PPV) was low (1.4%; 95% CI = 0.6%, 3.1%), whereas the negative predictive value (NPV) was high (99.8%; 95% CI = 99.1%, 99.9%).
Figure 2.
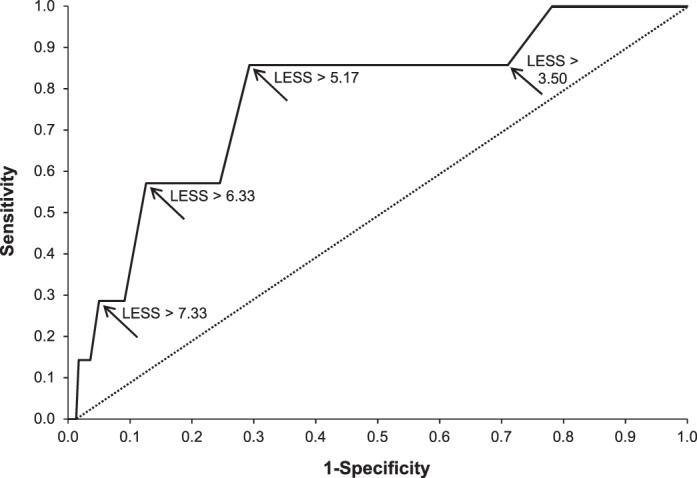
Receiver operator characteristic curve derived for the total Landing Error Scoring System (LESS) score and anterior cruciate ligament injury using different cutpoints. Using a LESS cutpoint of 5.17 revealed a sensitivity of 86% and a specificity of 71%. The area under the receiver operator characteristic curve was 0.78 (95% confidence interval = 0.61, 0.95).
The ACL Injury Risk
The 1-season risk of ACL injury in the overall sample was 0.58% (95% CI = 0.23%, 1.18%). The 1-season risk was 1.37% (95% CI = 0.50%, 2.96%) in athletes with preseason LESS scores of 5 or more and 0.13% (95% CI = 0.01%, 0.71%) in athletes with preseason LESS scores less than 5. Thus, the 1-season risk difference between a LESS score of 5 or more and less than 5 was 1.24% (95% CI = 0.12%, 2.36%; P = .01). The risk ratio for a LESS score of 5 or more compared with a score of less than 5 was 10.7. A greater LESS score was associated monotonically with a greater 1-season risk of ACL injury in elite-youth soccer (Table 3).
Table 3.
Preseason Landing Error Scoring System Score by In-Season Incidence of Anterior Cruciate Ligament Injurya
| Preseason Landing Error Scoring System Score |
In-Season Incidence |
Average 1-Season Risk per 100 Athletes, % |
||
| No. (% of Athletes) |
Total (n = 1217) |
|||
| No Injury (n = 1210) |
Anterior Cruciate Ligament Injury (n = 7) |
|||
| 0.0–2.9 | 182 (15) | 0 (0) | 182 | 0.00 |
| 3.0–4.9 | 596 (49) | 1 (14) | 597 | 0.17 |
| 5.0–7.9 | 389 (32) | 5 (71) | 394 | 1.27 |
| 8.0+ | 43 (5) | 1 (14) | 44 | 2.27 |
Test for trend: Z = −2.54, P = .01.
The LESS Score by Injury Status
The mean LESS score was higher in athletes who sustained ACL injuries (6.24 ± 1.75; 95% CI = 4.62, 7.86) than in athletes who did not sustain ACL injuries (4.43 ± 1.71; 95% CI = 4.34, 4.53) (t1215 = −2.784, P < .005). We compared the item errors on the LESS scale between injured and uninjured participants to determine the individual items driving the difference in mean LESS scores. The most predictive items were trunk-flexion displacement, hip-flexion displacement, joint displacement, trunk flexion: initial contact, foot position: external rotation, and knee-flexion displacement (Table 4).
Table 4.
Preseason Landing Error Scoring System Errors by In-Season Incidence of Anterior Cruciate Ligament Injury
| Landing Error Scoring System Item |
In-Season Incidence |
||
| No.a (% of Athletes) |
P Valueb |
||
| No Injury (n = 1210) |
Anterior Cruciate Ligament Injury (n = 7) |
||
| Knee flexion: initial contact | 798 (66) | 6 (86) | .43 |
| Hip flexion: initial contact | 5 (<1) | 0 (0) | >.99 |
| Trunk flexion: initial contact | 368 (30) | 4 (57) | .21 |
| Ankle plantar flexion: initial contact | 140 (12) | 0 (0) | >.99 |
| Medial knee position: initial contact | 171 (14) | 0 (0) | .60 |
| Lateral trunk flexion: initial contact | 394 (33) | 3 (43) | .69 |
| Stance width: wide | 77 (6) | 1 (14) | .37 |
| Stance width: narrow | 757 (63) | 5 (71) | >.99 |
| Foot position: external rotation | 653 (54) | 6 (86) | .13 |
| Foot position: internal rotation | 44 (4) | 0 (0) | >.99 |
| Symmetric initial-foot contact: initial contact | 148 (12) | 0 (0) | >.99 |
| Knee-flexion displacement | 120 (10) | 2 (29) | .15 |
| Hip-flexion displacement | 31 (3) | 1 (14) | .17 |
| Trunk-flexion displacement | 406 (34) | 6 (86) | .007 |
| Medial-knee displacement | 870 (72) | 5 (71) | >.99 |
| Joint displacement | |||
| Excellent (soft) | 678 (56) | 1 (14) | |
| Average | 456 (38) | 6 (86) | .04 |
| Stiff | 76 (6) | 0 (0) | |
| Overall impression | |||
| Excellent | 51 (4) | 0 (0) | |
| Average | 904 (75) | 5 (71) | .74 |
| Poor | 255 (21) | 2 (29) | |
Number of individuals displaying the specified movement error.
P values reflect the t or F values.
DISCUSSION
Validating field screening tools for identifying high-risk individuals for noncontact and indirect-contact ACL injuries is an important step in preventing these injuries in youth soccer players. We examined the predictive ability of a field-expedient assessment of movement quality during a jump landing. Our most important finding was that elite-level youth soccer athletes with LESS scores of 5 or more were at greater risk (1.2% risk difference) of sustaining noncontact or indirect-contact ACL injuries than their counterparts with LESS scores below 5.
Almost no literature exists regarding prospective biomechanical screening for ACL injury. Increased external-knee abduction (valgus) moment during a drop landing has been reported as a prospective risk factor for ACL injury, with a sensitivity and specificity of 78% and 67%, respectively.13 Our observations agreed with this research by demonstrating that movement quality is also a biomechanical risk factor predictive of noncontact or indirect-contact ACL injury, with very similar levels of sensitivity (86%) and specificity (64%). Confirmation in subsequent reports that the field-based LESS has a predictive capacity similar to that of laboratory instrumentation would be a major step forward in ACL injury-prevention screening. Using laboratory equipment is expensive, demands technical expertise, and is time consuming. In contrast, the LESS requires approximately $300 to $400 to be spent on equipment, a few hours of administration training, 1 to 2 minutes of athlete time per individual screened, and fewer than 5 minutes per athlete to grade the LESS. This time may be reduced by scoring the LESS in real time, which has been shown to be reliable.16 However, no research exists regarding the injury-prediction validity of the LESS in real time.
Our preliminary study showed that the LESS is not a perfect screening tool. Its PPV of 1.4% at first glance seems unacceptable. However, the PPV of any ACL screening test will always be low because the rate of ACL injury is very low, even in reportedly high-risk populations. For instance, assuming an ACL incidence of 1 per 1000 athletes, a screening test with 99% sensitivity and 99% specificity would have a PPV of only 10% simply due to the low incidence of the injury. Similarly, the NPV for a screening test of a low-incidence condition will always be mathematically very favorable. For instance, in our population of elite-youth soccer athletes, a LESS score below 5.0 had an NPV of 99.9%. Given that PPV and NPV are highly dependent on incidence, the best measures of screening efficacy are sensitivity and specificity, which are not influenced by injury incidence.
Most researchers have shown that ACL injury-prevention programs pose no risk to participants. In relation to our results, these programs have also been shown to specifically reduce LESS scores below the cutpoint threshold that we detected for injury-risk susceptibility.17,18 However, these programs require large investments of athlete time, and most successful programs involve professional supervision, which results in substantial logistical constraints and monetary cost. The LESS can be performed quickly with minimal expense and minimal technical expertise. Given that ACL injury-prevention programs are not harmful, one would always want to maximize sensitivity over specificity in designing a tool for screening youth athletes to focus limited injury-prevention resources on the portion of the population (roughly one-third in our study) at high risk for ACL injury. The ability to focus injury-prevention resources would represent an important step forward for injury-prevention efforts in large populations with substantial time and resource constraints, such as youth athletic leagues, public school systems, and military training populations.
The LESS score is quantified as the sum of 17 possible individual movement errors during a jump-landing task. A limitation of the LESS score is that all identified movement errors are grouped into a single overall score, which could comprise any combination of individual specific movement errors. In our study, the most predictive individual items for ACL injury were limited trunk-flexion displacement and average lower extremity (hip, knee, and ankle) joint displacement. However, these results should be interpreted with caution because they are based on a small number of injured athletes in a specific population. Furthermore, the LESS score is affected by age and sex. We caution that use of a single cutpoint (ie, 5) may not be appropriate for all ages and sexes. Additional studies with larger sample sizes are needed to explore whether age-specific or sex-specific cutpoints would be appropriate and would enhance the predictive capacity of the LESS.
Our observations are not consistent with those reported in a well-designed case-control study conducted by Smith et al,15 who screened high school (n = 2910) and collegiate (n = 966) athletes with the LESS. Twenty-eight of these individuals sustained noncontact ACL injuries (9 males, 19 females), and 64 matched control participants were included in the final data analysis, which showed no relationship between ACL injury risk and LESS score. Whereas these researchers did not report any associations, 2 observations suggested a relationship. Athletes with LESS scores of 6 or more tended to be at higher risk than athletes with LESS scores of 4 or below (males: P = .08, females: P = .06).
Some differences between our study and the study of Smith et al15 may account for the lack of agreement between studies. We focused on youth soccer athletes (age = 13.9 ± 1.8 years; 25% from 11 to 12 years of age), whereas Smith et al15 studied a diverse multisport group that included both high school and college-aged athletes (age = 18.3 ± 2 years). The LESS was not predictive of ACL injury when the sample was limited to high school athletes; however, the average age of the high-school athletes was 16.9 ± 1.1 years,15 which was greater than the average age of athletes in our study. The natural decline of LESS scores in older athletes was likely an effect of maturation or “selection effect” in competitive sports and might have limited the ability of the LESS to predict ACL injury in an older population. Smith et al15 also removed individuals with histories of ACL injury from the analysis. Previously, ACL-injured individuals were known to be at high risk for ACL injury19–21 and to have faulty movement patterns.22–24 Removing these athletes may have further limited the predictive ability of the LESS in this population because many individuals who could have been detected by the LESS might have been filtered from the source population.
Another factor to consider when comparing our observations and those of Smith et al15 is differences in sport or athlete type between studies. We examined only soccer athletes, whereas Smith et al15 included basketball, field hockey, football, gymnastics, lacrosse, rugby, soccer, and volleyball athletes. The ACL injury rates are higher in soccer than in sports such as field hockey, gymnastics, lacrosse, and volleyball.25 In addition, direct-contact ACL injuries are more common in sports such as rugby and American football than in soccer. Predicting ACL-injury risk in sports with lower injury rates or more direct-contact injuries may influence the ability to predict ACL injury using the LESS. By focusing on a high-risk group for ACL injury, we eliminated the potential confounding factors of age and sport type. Finally, the differences in the 2 datasets may simply reflect random variation due to the small numbers of ACL injuries (28, Smith et al15; and 7, current study) observed in these 2 studies.
CONCLUSIONS
Our results suggest that the LESS may have screening potential for ACL injury in elite-youth soccer athletes. These observations may have implications for ACL injury-prevention efforts in youth soccer because the LESS is a field assessment of movement quality that requires no laboratory-based instrumentation. Ideally, one would want to use movement screening programs that identify individuals at risk for ACL injury as young as possible to allow time for preventive training to correct high-risk movement patterns before the peak ages for ACL injury risk (age range, 15 to 18 years). Whereas a high LESS score may lack precision in identifying which athlete will sustain an ACL injury, the LESS score may be effective in separating athletes into high-risk and low-risk subgroups. These data should be interpreted with caution due to the small number of ACL injury cases in this analysis. However, given the devastating consequences of ACL injury, the paucity of other ACL screening tests, the favorable feasibility profile of the LESS, and the costs associated with large-scale ACL injury-prevention efforts, the screening value of the LESS needs further investigation in youth-sport populations.
REFERENCES
- 1.Brophy RH, Schmitz L, Wright RW, et al. Return to play and future ACL injury risk after ACL reconstruction in soccer athletes from the Multicenter Orthopaedic Outcomes Network (MOON) group. Am J Sports Med. 2012;40(11):2517–2522. doi: 10.1177/0363546512459476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moksnes H, Engebretsen L, Eitzen I, Risberg MA. Functional outcomes following a non-operative treatment algorithm for anterior cruciate ligament injuries in skeletally immature children 12 years and younger: a prospective cohort with 2 years follow-up. Br J Sports Med. 2013;47(8):488–494. doi: 10.1136/bjsports-2012-092066. [DOI] [PubMed] [Google Scholar]
- 3.Noyes FR, Mooar PA, Matthews DS, Butler DL. The symptomatic anterior cruciate-deficient knee: part I. The long-term functional disability in athletically active individuals. J Bone Joint Surg Am. 1983;65(2):154–162. doi: 10.2106/00004623-198365020-00003. [DOI] [PubMed] [Google Scholar]
- 4.Noyes FR, Matthews DS, Mooar PA, Grood ES. The symptomatic anterior cruciate-deficient knee: part II. The results of rehabilitation, activity modification, and counseling on functional disability. J Bone Joint Surg Am. 1983;65(2):163–174. doi: 10.2106/00004623-198365020-00004. [DOI] [PubMed] [Google Scholar]
- 5.Ahldén M, Samuelsson K, Sernert N, Forssblad M, Karlsson J, Kartus J. The Swedish National Anterior Cruciate Ligament Register: a report on baseline variables and outcomes of surgery for almost 18,000 patients. Am J Sports Med. 2012;40(10):2230–2235. doi: 10.1177/0363546512457348. [DOI] [PubMed] [Google Scholar]
- 6.van Mechelen W, Hlobil H, Kemper HC. Incidence, severity, aetiology and prevention of sports injuries: a review of concepts. Sports Med. 1992;14(2):82–99. doi: 10.2165/00007256-199214020-00002. [DOI] [PubMed] [Google Scholar]
- 7.Boden BP, Torg JS, Knowles SB, Hewett TE. Video analysis of anterior cruciate ligament injury: abnormalities in hip and ankle kinematics. Am J Sports Med. 2009;37(2):252–259. doi: 10.1177/0363546508328107. [DOI] [PubMed] [Google Scholar]
- 8.Krosshaug T, Nakamae A, Boden BP, et al. Mechanisms of anterior cruciate ligament injury in basketball: video analysis of 39 cases. Am J Sports Med. 2007;35(3):359–367. doi: 10.1177/0363546506293899. [DOI] [PubMed] [Google Scholar]
- 9.Markolf KL, Burchfield DM, Shapiro MM, Shepard MF, Finerman GA, Slauterbeck JL. Combined knee loading states that generate high anterior cruciate ligament forces. J Orthop Res. 1995;13(6):930–935. doi: 10.1002/jor.1100130618. [DOI] [PubMed] [Google Scholar]
- 10.Withrow TJ, Huston LJ, Wojtys EM, Ashton-Miller JA. The effect of an impulsive knee valgus moment on in vitro relative ACL strain during a simulated jump landing. Clin Biomech (Bristol, Avon) 2006;21(9):977–983. doi: 10.1016/j.clinbiomech.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 11.Padua DA. Executing a collaborative prospective risk-factor study: findings, successes, and challenges. J Athl Train. 2010;45(5):519–521. doi: 10.4085/1062-6050-45.5.519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zazulak BT, Hewett TE, Reeves NP, Goldberg B, Cholewicki J. Deficits in neuromuscular control of the trunk predict knee injury risk: a prospective biomechanical-epidemiologic study. Am J Sports Med. 2007;35(7):1123–1130. doi: 10.1177/0363546507301585. [DOI] [PubMed] [Google Scholar]
- 13.Hewett TE, Myer GD, Ford KR. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492–501. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 14.Padua DA, Marshall SW, Boling MC, Thigpen CA, Garrett WE, Beutler AI. The Landing Error Scoring System (LESS) is a valid and reliable clinical assessment tool of jump-landing biomechanics: the JUMP-ACL study. Am J Sports Med. 2009;37(10):1996–2002. doi: 10.1177/0363546509343200. [DOI] [PubMed] [Google Scholar]
- 15.Smith HC, Johnson RJ, Shultz SJ, et al. A prospective evaluation of the Landing Error Scoring System (LESS) as a screening tool for anterior cruciate ligament injury risk. Am J Sports Med. 2012;40(3):521–526. doi: 10.1177/0363546511429776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Padua DA, Boling MC, DiStefano LJ, Onate JA, Beutler AI, Marshall SW. Reliability of the Landing Error Scoring System-real time, a clinical assessment tool of jump-landing biomechanics. J Sport Rehabil. 2011;20(2):145–156. doi: 10.1123/jsr.20.2.145. [DOI] [PubMed] [Google Scholar]
- 17.DiStefano LJ, Padua DA, DiStefano MJ, Marshall SW. Influence of age, sex, technique, and exercise program on movement patterns after an anterior cruciate ligament injury prevention program in youth soccer players. Am J Sports Med. 2009;37(3):495–505. doi: 10.1177/0363546508327542. [DOI] [PubMed] [Google Scholar]
- 18.Padua DA, DiStefano LJ, Marshall SW, Beutler AI, de la Motte SJ, DiStefano MJ. Retention of movement pattern changes after a lower extremity injury prevention program is affected by program duration. Am J Sports Med. 2012;40(2):300–306. doi: 10.1177/0363546511425474. [DOI] [PubMed] [Google Scholar]
- 19.Laboute E, Savalli L, Puig P, et al. Analysis of return to competition and repeat rupture for 298 anterior cruciate ligament reconstructions with patellar or hamstring tendon autograft in sportspeople. Ann Phys Rehabil Med. 2010;53(10):598–614. doi: 10.1016/j.rehab.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 20.Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2009;37(2):246–251. doi: 10.1177/0363546508325665. [DOI] [PubMed] [Google Scholar]
- 21.Pinczewski LA, Lyman J, Salmon LJ, Russell VJ, Roe J, Linklater J. A. 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. Am J Sports Med. 2007;35(4):564–574. doi: 10.1177/0363546506296042. [DOI] [PubMed] [Google Scholar]
- 22.Gokeler A, Hof AL, Arnold MP, Dijkstra PU, Postema K, Otten E. Abnormal landing strategies after ACL reconstruction. Scand J Med Sci Sports. 2010;20(1):E12–E19. doi: 10.1111/j.1600-0838.2008.00873.x. [DOI] [PubMed] [Google Scholar]
- 23.Butler RJ, Minick KI, Ferber R, Underwood F. Gait mechanics after ACL reconstruction: implications for the early onset of knee osteoarthritis. Br J Sports Med. 2009;43(5):366–370. doi: 10.1136/bjsm.2008.052522. [DOI] [PubMed] [Google Scholar]
- 24.Oberländer KD, Brüggemann GP, Höher J, Karamanidis K. Altered landing mechanics in ACL-reconstructed patients. Med Sci Sports Exerc. 2013;45(3):506–513. doi: 10.1249/MSS.0b013e3182752ae3. [DOI] [PubMed] [Google Scholar]
- 25.Marshall SW, Padua DA, McGrath M. Incidence of ACL injury. In: TE Hewett, Shultz SJ, Griffin LY., editors. Understanding and Preventing Noncontact ACL Injuries. Champaign, IL: Human Kinetics;; 2007. pp. 5–29. In. eds. [Google Scholar]