Abstract
A newly developed Gamma Knife relocatable eXtend frame system has enabled the delivery of multi-session Gamma Knife radiosurgery without the use of skull pin fixation frame system. In this study, we investigate and report for the first time the whole procedural radiological accuracy for administering such treatments. To quantify the radiological alignment, the commonly used Winston-Lutz test was modified and used to determine the device accuracy of the eXtend frame system. Patient setup uncertainties relative to the device were further measured for a series of treatment sessions (n = 58), and then incorporated with the Winston-Lutz test results from individual patient-specific eXtend frame systems. The whole-procedure mean 3D radiological setup uncertainty was determined to be 0.69 ± 0.73 mm (1σ) from all the cases analyzed, and the mean 90% confidence level margins were found to be 0.55, 0.78 and 0.72 mm along the x-, y-, and z-axis, respectively. Our results therefore demonstrated that sub-millimetric radiological accuracy is clinically achievable for multi-session Gamma Knife radiosurgery treatments and a 1 mm margin along the major axes is sufficient for planning multi-session Gamma Knife radiosurgery treatments.
Keywords: Stereotactic radiosurgery, Gamma Knife, eXtend System, Relocatable frame, Accuracy
Introduction
A relocatable Gamma Knife frame system (Gamma Knife eXtend frame system, Elekta AB, Stockholm, Sweden) was recently developed and approved in North America (1) for administering multi-session Gamma Knife radiosurgery. The eXtend system takes advantage of technical advancements of the latest Gamma Knife Perfexion system (2-5), where automatic patient positioning enables multiple isocenters or shots to be delivered with a turnkey solution, and with only a single patient treatment setup for a majority of the cases. In addition, the accessible treatment space that allows the patient’s head to be positioned inside the Gamma Knife Perfexion unit has been significantly augmented by as much as 50% as compared to the previous Gamma Knife models. These advancements in the Perfexion model facilitated the developments of a relocatable frame system called the eXtend system.
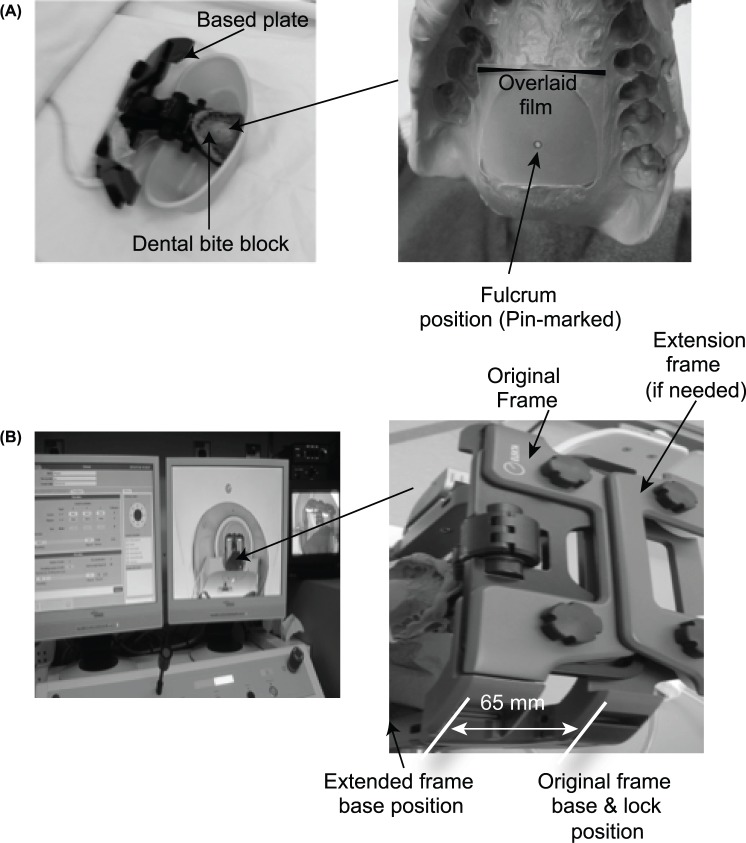
The technical components and operating details of the eXtend frame system have been recently reported (1, 6). In principle, the eXtend system relies on a head mold or cushion and a vacuum-assisted bite block to immobilize the patient’s head (Figures 1-2). Once the patient’s head is locked into position, the vacuum readings created at the interface between the base plate of the bite block (i.e., the fulcrum position) and the patient’s hard palate is monitored continuously throughout the treatment session to ensure setup accuracy and consistency. When carrying out a multisession treatment, a digital probe is then used to quantify any potential inter-session setup variations by measuring the distances (at multiple preset locations) from the patient’s head surface to the face of a cubic plastic helmet that is attached to the base plate of the bite block system. The readings from the digital probe allow one to determine relative shifts of the patient head along the major axes, i.e., anterior-posterior (AP), left-right (LAT) and superior-inferior (SI) directions, respectively.
Figure 1:
Device and experimental setup for performing the modified Winston-Lutz test on the patient-specific bite block device used for multi-session Gamma Knife radiosurgery. Right-side panels of the figure are the zoom-in view of the corresponding left-side panels: (A) shows the fulcrum position on the bite block and (B) shows the extend frame holding the bite block in the beam irradiation position.
Figure 2:
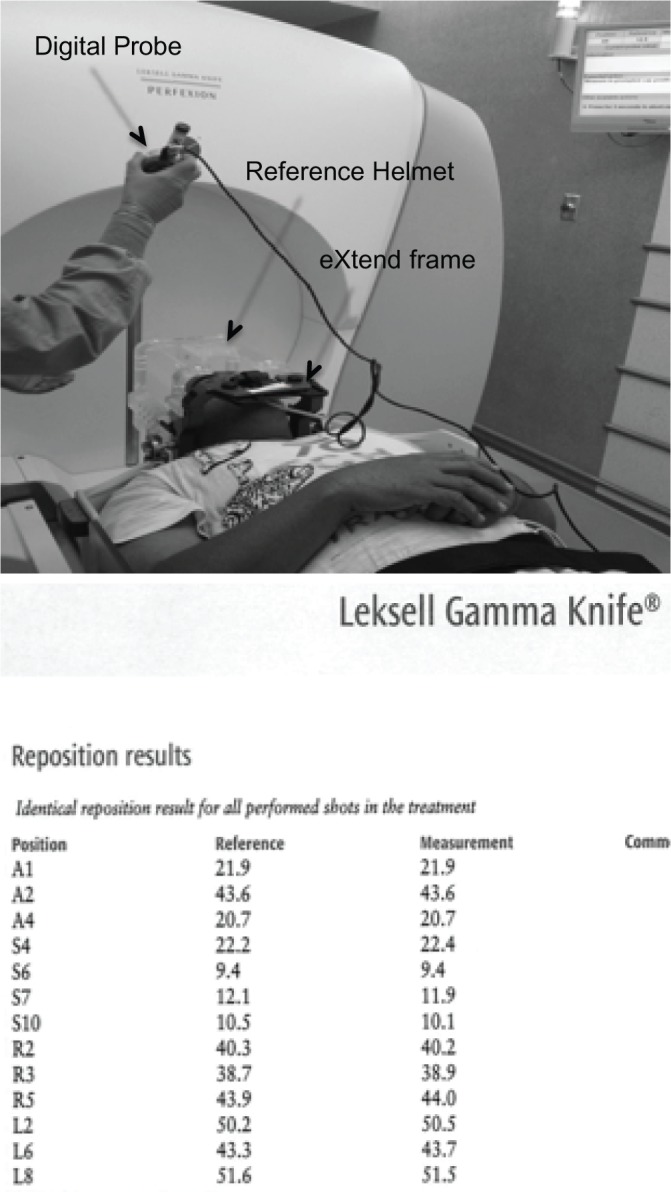
Illustration of an actual patient treatment setup process with the online digital probe measurement results for one treatment session. The reference measurement values are obtained during the simulation CT.
Because the base plate of the eXtend system is mechanically calibrated against the reference center of the Gamma Knife Perfexion system, the overall radiological accuracy of a patient setup is governed by a two-step setup process, which involved the following accuracies: (1) patient’s head positioning accuracy against the base plate of the eXtend frame system, and (2) the alignment accuracy of the eXtend frame base plate against the radiological center (e.g. focal point of all the radiation beamlets) of the Gamma Knife unit. The question therefore arises as to whether the whole-procedural radiological margin should be applied for this system under these processes, and if so how much under the clinical settings.
Previous studies have investigated the composite accuracy for the traditional Leksell frame systems (4, 5, 7). In those systems a rigid frame is directly fixated onto the patient skull via a set of metal pins, and because of this, the patient’s head shift relative to the frame itself is generally assumed to be negligible. However, the composite radiological accuracy of a relocatable frame system for Gamma Knife radiosurgery, particularly for the new eXtend frame system, has not been fully quantified in terms of patient-specific device accuracy together with the online setup accuracy although previous studies have reported on the online setup accuracy via imaging or direct online measurements (1, 6, 8).
The whole-procedural radiological accuracy is an important issue as it directly impacts the clinical decision regarding whether it is necessary to add any margin to the planning target volume for the multi-session Gamma Knife procedure. This in turn affects the total prescription dose as well as the dose fractionation schemes due to normal brain tissue tolerance levels despite the sharp dose-fall off typical to Gamma Knife radiosurgery (9). For this study, the composite wholeprocedure set-up margins for was measured on a cohort of patient cases (n = 12) sequentially treated with the Gamma Knife eXtend system at our institution since its first implementation in January 2012. All cases were for five treatment fractions except for one case for which there were three treatment fractions. This resulted in a total of 58 treatment sessions for the 12 cases that were used for this study. The total prescription dose for these cases ranged from 24 to 30 Gy. These analyses were part of our quality assurance measures during the commissioning and implementation of the eXtend frame system into our clinical practice. Here we report for the first time the results of these analyses.
Materials and Methods
The experimental setup for our modified Winston-Lutz test (10) is illustrated in Figure 1. The procedure started by threading a metal wire through the vacuum line of the custom-made patient bite block. The tip of the metal wire was then marked and aligned with the radiochromic film (Gafchromic MD-V2-55) to denote the fulcrum position of the eXtend frame (Figure 1). Afterwards a CT scan of the entire system without the patient was obtained, using a CT protocol identical to that clinically used for Gamma Knife eXtend frame patients (e.g. full head scan with 1.5 mm slice thickness). The CT images were then imported into the Leksell Gamma Plan system (version 10.1), and a single 4 mm shot was centrally placed on the fulcrum location as identified by the metal wire tip position.
After beam irradiation of approximately 20 Gy to the shot center, the exposed film was analyzed via an in-house analysis software. Unlike the traditional Winston-Lutz test, a peripheral isodose dose band (e.g. from 30 to 60% of the beam penumbra profile) was extracted, and overlaid on the center of the pin-mark as identified on the film (Figure 3). The details of the film analysis procedure were described in an early publication (7). From these extracted images, the center-of-mass of the isodose band as well as the pin-mark position was precisely determined. The locations of these two center-of-mass points were then compared with each other to determine the absolute shifts between the radiological center from the narrow isodose band, and the fulcrum point of the vacuum-assisted bite block.
Figure 3:
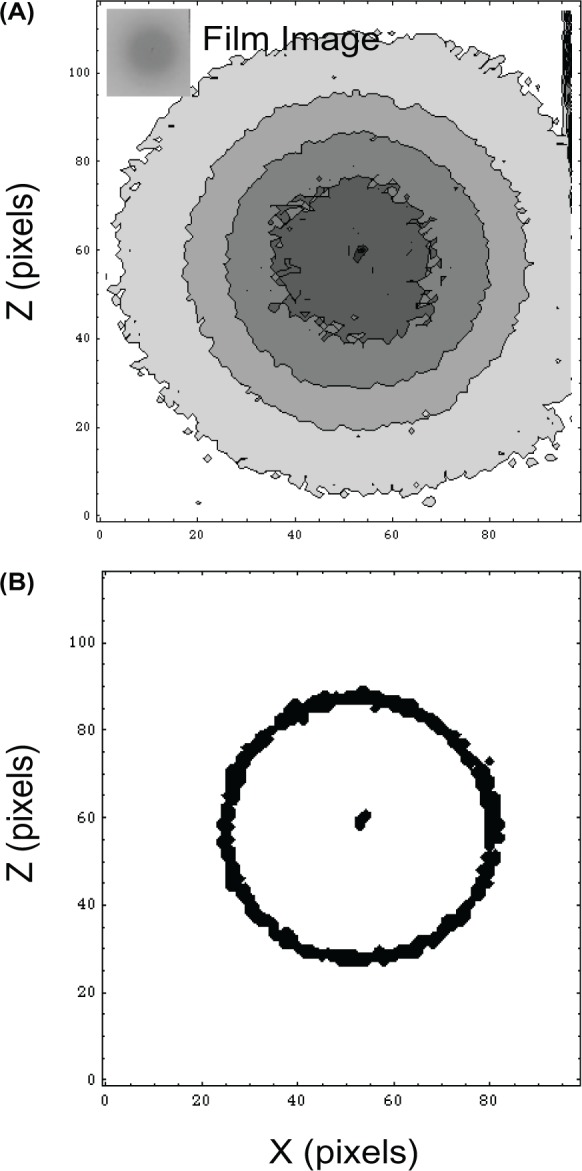
Illustration of an eXtend patient treatment case results showing (A) the original unfiltered film with the pin-mark at the center (B) the extracted isodose plot, and the peripheral isodose band (approximately 40-60% of the central dose) and the central pin-marked area. The scale of the plots is 0.2 mm. No smoothing and edge enhancing filters were used for this procedure. Instead, the mean center-of-mass (CM) position was determined for the central marking area and the peripheral isodose band. The discrepancy between the two CM positions was found to 0.36 ± 0.03 mm for repeated measurements. The result was insensitive to high background noise and the selection of the peripheral isodose band.
In addition to measuring the mechanical fulcrum alignment against the radiological center, individual patient setup shifts were also measured prior to each treatment. The overall patient setup uncertainty (Δ) was calculated as follows,
| 1 |
where <δx>, <δy>, <δz> are the mean mechanical patient setup shifts as measured via the digital probe in reference to the base plate or the fulcrum position (Figure 2) along the x-, y- and z-axes, representing the lateral, anterior-posterior, and longitudinal shifts, respectively. The digital probe was calibrated against a phantom and the precision of the probe was calibrated to be less than 0.005 mm as determined from repeat phantom measurements.
Combining the fulcrum shift (<δ0>) as determined by the aforementioned modified Winston-Lutz test with the patient setup uncertainty from Equation [1], the wholeprocedural shift vector (R) for each case was then calculated as follows
| 2 |
In Equation 2 above, we have assumed a non-correlative or random nature in the 3D shift vector from each measurement, despite the fact that the fulcrum film measurements were limited to 2D measurements along the surface of the bite block. In other words, we have assumed that the measured <δ0> is representative of the 3D shift vector length in the bite block alignment. This is a reasonable approximation as such a shift is relatively small as compared to the patient setup uncertainties of Equation [1].
Moreover, for certain patient cases for which the bite block fulcrum position falls outside of the current CT indexingbox for the beam irradiation (e.g. either due to the patient’s head geometry or due to the maximum range of the stereotactic coordinate along the axial direction), we added a fixed extension to the patient-specific bite block (Figure 1). This in effect extended the entire bite block and its fulcrum position superiorly by 65 mm, along the z-axis so that fulbrum point falls within the existing limit of the stereotactic coordinate values. The extension piece was an identical component of another extend frame except mounted reversely as shown in Figure 1. Because such an extension is a linear constant we applied the following relationship into Equation 1 (i.e., <δ(z+C)> = δz) for those cases, without affecting the generality of the derivations.
Results
Figure 2 shows an actual patient setup, and the patient positioning alignment measurements as determined via the digital probe prior to treatment delivery. The values shown are for measurements along the three major axes obtained prior to treatment delivery, and for the corresponding reference measurements obtained during the patient’s simulation CT scan. The root mean square value of the measured differences between these two values along the three major axes were <δx> = 0.22 ± 0.32 mm (1σ), <δy> = 0.06 ± 0.24 mm, and <δz> = 0.10 ± 0.34 mm, when averaging over all the treatment sessions (n = 5) for this case.
Figure 3 illustrates the exposed film and its analysis result for the fulcrum position measurement for the aforementioned patient case. As shown in Figure 3, a δ0 = 0.54 mm was obtained (note that the scale of the plot is 0.2 mm in grid size while the film scanning pixel resolution was 0.08 mm or 300 dpi). The obtained result was found to be insensitive to the selection of the peripheral isodose band. For example,
when enlarging or narrowing the peripheral isodose band by ±10%, the agreement between the marked pin position and the center-of-mass of the fulcrum position was found to be less than 0.07 mm. The results were consistent among all the film measurements demonstrating the insensitivity of the procedure to the background noise and to the selection of the narrow isodose band covering the peripheral isodose region. Substituting these values into Equation 2, the wholeprocedure radiological uncertainty for the entire treatment course was determined to be 0.59 ± 0.36 mm, for this particular case.
A summary of the whole-procedure uncertainties as measured from all the patient cases is given in Figure 4. All cases were for five treatment fractions except for one case (No. 6) for which there were three treatment fractions. This resulted in a total of 58 treatment sessions for the 12 cases that were used for this study. The total prescription dose for these cases ranged from 24 to 30 Gy. Based on the results shown in Figure 4, the mean setup uncertainty was found to be 0.69 ± 0.73 mm (1σ) when averaging over all these treatment sessions. Applying the Cartesian-based Van Herk formula (11) by assuming independence of individual setup measurements along the major axes and the validity of the formula for patient sample size (12), the 90% confidence level margins were determined to be 0.78 mm, 0.55 mm and 0.72 mm along the anterior-posterior, lateral, and superiorinferior directions, respectively.
Figure 4:
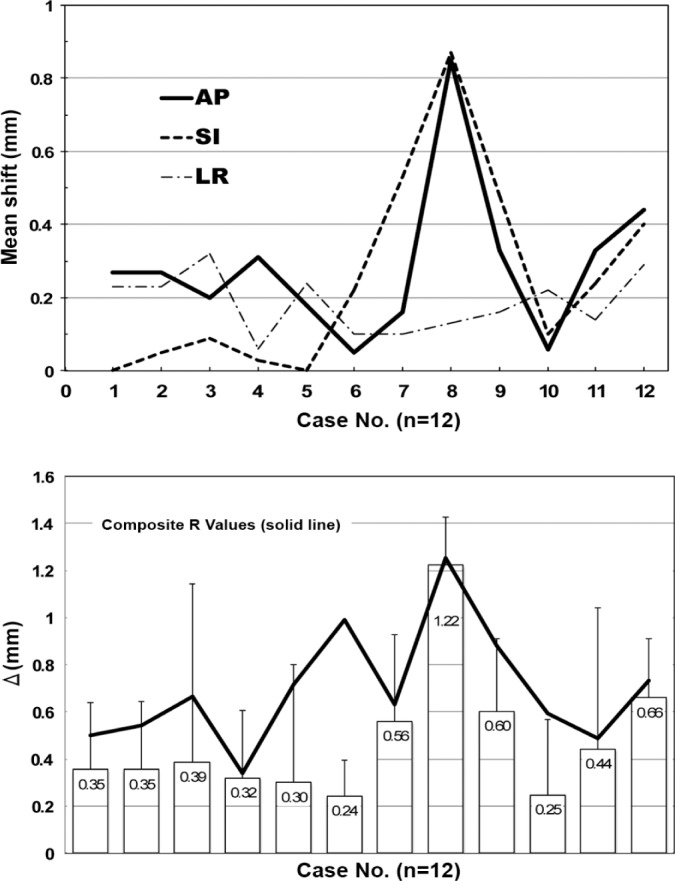
Summary of all the cases for the overall procedural accuracy. The errors bar shows a 1σ deviation from the mean value, and the solid line represents the composite Δ value obtained from Equation 2, for each case.
Discussion
This is the first study investigating the whole-procedure radiological margin required for delivering multi-session Gamma Knife treatments using a relocatable frame system. Based on a series of patient-specific treatment devices, and treatment delivery sessions, a sub-millimeter accuracy was found to be clinically achievable for a majority of the treatments, and a whole-procedural 1-mm margin was found to be sufficient to account for the majority of treatment-related setup uncertainties.
The technical uniqueness of our study stems from the adaptation of the well-known Winston-Lutz test to the relocatable eXtend frame system for multi-session Gamma Knife radiosurgery. The rationale for such an analysis was to overcome a common problem encountered in performing the traditional Winston-Lutz test where significant irregularities are created in a single isodose line due to the obscuring of the beam profile edge, because measured beam profiles may not be strictly circular in the shape, and because of noise from the low background dose such as that from the inside of a Gamma Knife unit (7, 10). For these reasons, line-smoothing software was often applied. The use of an isodose band solves the aforementioned problem and eliminates the need to precisely determine a specific peripheral isodose curve. The centers-of-mass as determined from our procedure were by definition the central position obtained via averaging all the dose points that fall within a band of isodose lines of the beam penumbra region.
Compared to the traditional Winston-Lutz test where alignment of the mechanical center versus the radiological center is measured for a preset circular geometry from fixed beam configuration such as that of a linear accelerator, the above method is adaptive to mechanical isocenter alignment for variable geometries where the exact field shape and field edge may not be known ahead of time, as in the case of the fulcrum alignment of a patient-specific bite block relative to the orientation of a symmetric 4-mm shot.
The advantages of such a technique are, (1) basing the mechanical center on relevant imaging that closely mimics clinical delivery, and (2) field edge detection via a band of peripheral isodose curves instead of a single isodose line. This renders the procedure highly robust to the measurement noise, and eliminates the need for curve smoothing as well as possible bias introduced by the smoothing software that is used.
However, a potential source of uncertainty for the current eXtend frame measurements is the rotation of the patient’s skull relative to the fulcrum of the bite block device. Since such rotations may affect the directional shift non-uniformly, it is practically impossible for the digital probe measurements to sample and precisely account for such rotations via a limited number of measurements along the major axes. Given complex and random nature of the problem, volumetric imaging such as online cone-beam CT is needed to quantify the nature and extent of such an uncertainty. As online imaging is currently unavailable for the Gamma Knife unit, such uncertainties were neglected for the analysis described in this study. Nonetheless, any radiological effects resulting from head rotations are expected to be small due to the 2π source arrangement in the Gamma Knife unit. Our ongoing studies will determine interplay between the source geometry related to rotational setup uncertainties, and ascertain their importance in determining the whole-procedure uncertainty for a multi-session eXtend frame Gamma Knife treatment.
In summary, one-millimeter planning target margin is demonstrated to be adequate for multi-session Gamma Knife radiosurgery treatments. Our conclusion is supported by the physical measurements of radiological isocenter alignments as well as patient-specific measurements from on-line treatment setups. Future online imageguided studies when they become available for the Gamma Knife unit, and more importantly clinical outcome studies would eventually determine whether a millimetric margin is a safe, and effective practice for multi-session Gamma Knife radiosurgery.
Acknowledgements
We acknowledge technical support from Elekta on the commissioning of the eXtend system.
References
- 1.Sayer FT, Sherman JH, Yen CP, Schlesinger DJ, Kersh R, Sheehan JP. Initial experience with the eXtend System: a relocatable frame system for multiple-session gamma knife radiosurgery. World Neurosurg 75, 665-672 (2011). DOI: 10.1016/j.wneu.2010.12.051 http://www.ncbi.nlm.nih.gov/pubmed/21704934 [DOI] [PubMed] [Google Scholar]
- 2.Lindquist C, Paddick I. The Leksell Gamma Knife Perfexion and comparisons with its predecessors. Neurosurgery 61, 130-140; discussion 140-131 (2007). DOI: 10.1227/01.neu.0000289726.35330. 8a00006123-200709001-00022 [pii] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17876243 [DOI] [PubMed] [Google Scholar]
- 3.Novotny J, Bhatnagar JP, Niranjan A, Quader MA, Huq MS, Bednarz G, Flickinger JC, Kondziolka D, Lunsford LD. Dosimetric comparison of the Leksell Gamma Knife perfexion and 4C. J Neurosurg 109 (Suppl), 8-14 (2008). DOI: 10.3171/JNS/2008/109/12/S3 http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=19123882 [DOI] [PubMed] [Google Scholar]
- 4.Regis J, Tamura M, Guillot C, Yomo S, Muraciolle X, Nagaje M, Arka Y, Porcheron D. Radiosurgery with the world's first fully robotized Leksell Gamma Knife Perfexion in clinical use: a 200-patient prospective, randomized, controlled comparison with the Gamma Knife 4C. Neurosurgery 64, 346-355; discussion 355-346 (2009). DOI: 10.1227/01.NEU.0000337578.00814.7500006123-200902000-00016 [pii] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=19190462 [DOI] [PubMed] [Google Scholar]
- 5.Sahgal A, Ma L, Chang E, Shiu A, Larson DA, Laperriere N, Yin FF, Tsao M, Menard C, Basran PS, Letourneau D, Heydarian M, Beachey D, Shukla V, Cusimano M, Hodaie M, Zadeh G, Bernstein M, Schwartz M. Advances in technology for intracranial stereotactic radiosurgery. Technol Cancer Res Treat 8, 271-280 (2009). DOI: d=3036&c=4291&p=17651&do=detail [pii] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=19645520 [DOI] [PubMed] [Google Scholar]
- 6.Ruschin M, Nayebi N, Carlsson P, Brown K, Tamerou M, Li W, Laperriere N, Sahgal A, Cho YB, Menard C, Jaffray D. Performance of a novel repositioning head frame for gamma knife perfexion and image-guided linac-based intracranial stereotactic radiotherapy. International Journal of Radiation Oncology, Biology, Physics 78, 306-313 (2010). DOI: 10.1016/j.ijrobp.2009.11.001 http://www.ncbi.nlm.nih.gov/pubmed/20385456 [DOI] [PubMed] [Google Scholar]
- 7.Ma L, Chuang C, Descovich M, Petti P, Smith V, Verhey L. Whole-procedure clinical accuracy of gamma knife treatments of large lesions. Med Phys 35, 5110-5114 (2008). DOI: 10.1118/1.2987669 http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=19070245 [DOI] [PubMed] [Google Scholar]
- 8.Schlesinger D, Xu Z, Taylor F, Yen CP, Sheehan J. Interfraction and intrafraction performance of the Gamma Knife Extend system for patient positioning and immobilization. Journal of Neurosurgery 117 (Suppl), 217-224 (2012). DOI: 10.3171/2012.6.GKS12989 http://www.ncbi.nlm.nih.gov/pubmed/23205813 [DOI] [PubMed] [Google Scholar]
- 9.Ma L, Sahgal A, Descovich M, Cho YB, Chuang C, Huang K, Laperriere NJ, Shrieve DC, Larson DA. Equivalence in dose fall-off for isocentric and nonisocentric intracranial treatment modalities and its impact on dose fractionation schemes. International Journal of Radiation Oncology, Biology, Physics 76, 943-948 (2010). DOI: 10.1016/j.ijrobp.2009.07.1721 http://www.ncbi.nlm.nih.gov/pubmed/20159366 [DOI] [PubMed] [Google Scholar]
- 10.Lutz W, Winston KR, Maleki N. A system for stereotactic radiosurgery with a linear accelerator. International Journal of Radiation Oncology, Biology, Physics 14, 373-381 (1988). DOI: 10.1016/03603016(88)90446-4 http://www.ncbi.nlm.nih.gov/pubmed/3276655 [DOI] [PubMed] [Google Scholar]
- 11.Yoda K, Nakagawa K. Technical note: extension of Van Herk's treatment margin model for anisotropic systematic positioning errors in cartesian coordinate systema. Medical Physics 38, 3913-3914 (2011). DOI: 10.1118/1.3596531 http://www.ncbi.nlm.nih.gov/pubmed/21858987 [DOI] [PubMed] [Google Scholar]
- 12.van Herk M. Errors and margins in radiotherapy. Seminars in Radiation Oncology 14, 52-64 (2004). DOI: 10.1053/j.semradonc.2003.10.003 http://www.ncbi.nlm.nih.gov/pubmed/14752733 [DOI] [PubMed] [Google Scholar]