Abstract
As computers and smartphones continue to transform the doctor-patient relationship, it is essential that healthcare professionals understand how their patients wish to interact with these devices. The results from a satisfaction questionnaire of 225 Oncology patients treated in 2011 in Quebec, Canada provide insight into the manner in which patients have been and wish to communicate with their healthcare teams. The survey also addressed whether or not patients searched the Internet for supplementary information regarding their condition. Generally, patients were neutral regarding adopting greater usage of modern means of communication. The majority of patients did not want to be contacted via e-mail or SMS, nor did the patients want to make appointments or fill out surveys online. Forty four percent of patients used the Internet to learn more about their condition. Concerning the patients who were not provided with links to medically relevant websites, 44% wished their doctors had supplied them with such links. Though there was much overlap between the 44% of patients who went on the Internet to learn more about their condition and the 44% of the patients who wished their physicians provided them with such links, 14% of all the patients wished their medical teams had provided them with links, but did not independently search for medically relevant information about their condition. Using chi-square testing education level was found to be the best predictor of which patients searched the web for supplementary information about their conditions (p = 0.003). Contrary to findings in other studies, a comparable proportion of patients in each age-group used the Internet to research their condition. Given the wealth of web-resources available to cancer patients, it would be beneficial for both healthcare teams and their patients if physicians consistently offered a list of trustworthy websites to their patients.
Keywords: e-Patient, Patient
Introduction
As social networks and mobile devices enable people to become increasingly connected, it is important for health-care professionals to remain abreast of how their patients wish to communicate with their medical teams. In order to efficiently allocate resources, medical teams must be mindful of whether their patients wish to be able to phone, SMS, or e-mail them. Similarly, monitoring the manner in which patients utilize the Internet to learn about their medical conditions will enable physicians to provide more responsive and efficient health care.
E-Patients are those patients who utilize the Internet to learn about their condition and treatment (1). Though a variety of studies have previously examined e-Patient demographics, there is a dearth of data pertaining to e-Patients in Canada and especially in Quebec. Furthermore, the Internet is rapidly evolving and usage rates continue to increase both in Canada (2) and in Quebec (3). In a medical context, this translates into a growing number of e-Patients. Therefore, in order to better inform patients, it is important to track how they use the Internet and to determine what, if any guidance medical teams should supply to better assist these types of patients.
Internet usage was the primary focus of this study because encouraging patients to become e-Patients could efficiently empower patients to become better educated healthcare consumers. Research by Kim and Kwon has demonstrated that e-Patients turn most frequently to the web for information about their condition but are more trusting of information they receive from their health care teams (4). Therefore, in contrast to providing patients with a physician’s e-mail address or telephone number, providing patients with a series of links to reliable healthcare websites would be a time-efficient way of providing them with supplementary medical information that they can trust.
Materials and Methods
To measure patient attitudes towards modern means of communication, between August 28, 2011 and January 10, 2012, surveys were sent to 500 radiation oncology patients. This sample corresponds to approximately 10% of the total population of patients during the specified time interval. 225 patients, or 45% of the population sample, completed the survey.
The study was approved by the hospital directorate of information management and quality performance, the hospital cancer care program, and the health promotion committee of the department of radiation oncology.
The modern means of communication survey was composed of yes-no questions. The surveys were performed in French as the majority of the patients were French-speaking. The survey asked the following:
1: Do you have an e-mail address?
2: Do you have Internet access at home or elsewhere?
3: Would you like to be contacted by e-mail?
4: Do you have a cell phone?
5a: Did you receive an e-mail address to contact a member of your treatment team?
5b: If not, would you have liked to have one?
6: Did you go on the Internet to get information about your disease?
7a: Did we give you links to websites with information about your disease?
7b: If not, would you have wanted links to information about your disease?
8: Would you have liked to answer this survey online?
9: Would you like to make your appointments online?
10: Would you have liked to communicate with the hospital by SMS?
The demographic survey asked patients to select their gender, the language they speak most frequently at home, type of cancer, and their age group. Patients were also asked about their highest level of academic achievement. They could choose among the following options: none, high school, professional school, commercial college, general and vocational college (CEGEP), and University. In Quebec, CEGEP is an intermediary school between high school (which ends in 11th grade) and university, where both trade school courses and pre-university courses are offered. In order to assess overall patient satisfaction with their care, patients were given a Likert-type scale with options ranging from very unsatisfied to very satisfied. Patients were also asked whether or not they were assigned nurse navigators. At Montreal University Health Centre (CHUM) selected patients are assigned nurse navigators to assist them with coordinating their treatments and to serve as their primary point of contact with the hospital staff.
Due to an administrative error, the link between the demographic survey and the means of communication survey was lost for 161 out of 225 surveys. Descriptive statistics pertaining to the modern means of communication survey were performed using all 225 responses. In those surveys that could be linked, chi-square tests were used to assess statistical significance between categorical variables. Twotailed p values < 0.05 were considered significant.
Results
Demographics
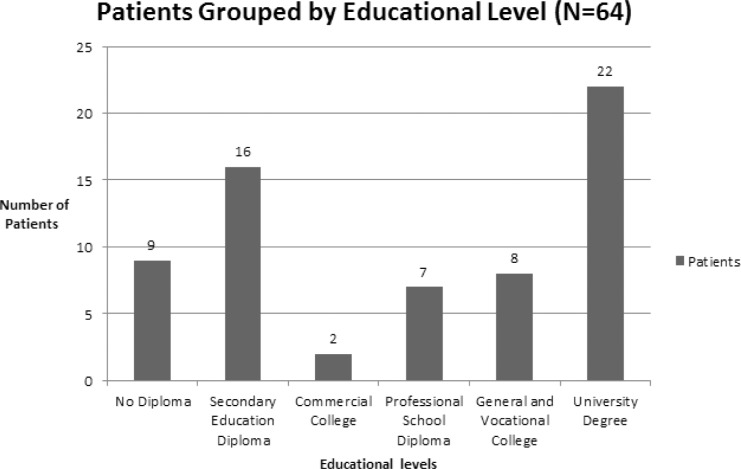
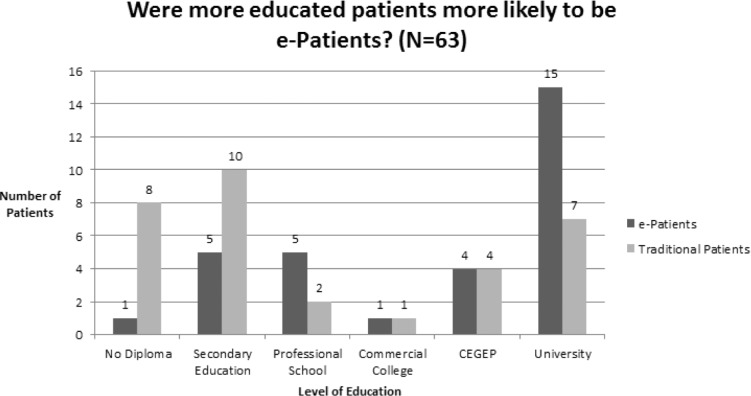
Of the 64 patients who had linked demographic surveys, the average age was 67.9. Forty one percent of the patients were in the 55-64 age group, which was the plurality. Fifty percent of the population was female. The three most common types of cancers affecting patients were Breast, Prostate, and Lung in decreasing order. The plurality (34%) of patients had university degrees (Figure 1). A bar graph differentiating patients by educational level is presented below in Figure 1. Ninety one percent of the population spoke French at home. Eighty four percent of the population was “very satisfied” with the information they received from their medical teams, while another 11% was “satisfied”.
Figure 1.
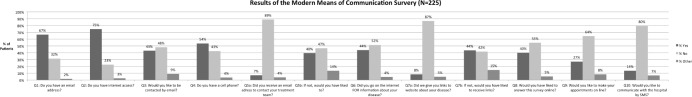
Modern Means of Communication
Of the 225 respondents, 150 had an e-mail address. One hundred sixty eight patients (74.7%) had Internet access at home or somewhere else. One hundred twenty one patients (53.8%) had a cell phone. Ninety seven patients (43.1%) would have liked to be contacted via e-mail. Sixteen patients (7.1%) received an e-mail address to contact a member of their medical team. Eighty nine patients (39.6%) would have liked to get one. Ninety nine patients (44.0%) went on the Internet to get information about their disease. Nineteen patients (8.4%) received links to get information about their disease. Ninety eight patients (43.6%) wished their physician’s provided them with links. Ninety patients (40.0%) would have liked to answer the survey online. Sixty one patients (27.1%) would have liked to be able to make appointments online. Thirty one patients (13.8%) would have liked to be able to communicate with the hospital by SMS. (The data is presented below in Figure 2.)
Figure 2.
Out of the 98 patients who answered yes to question 7b, indicating that they wished their medical teams provided them with links to websites containing information about their illness, 67% or 68%, answered yes to question 6 indicating that they acted as e-Patients, while, 31 patients, or 32%, answered no to question 6, indicating that they did not independently search for links. Sixteen patients, corresponding to 7% of the overall population acted as e-Patients but did not wish to receive links from their medical teams.
Chi-square Testing of Relationships between Demographic Information and Internet Usage
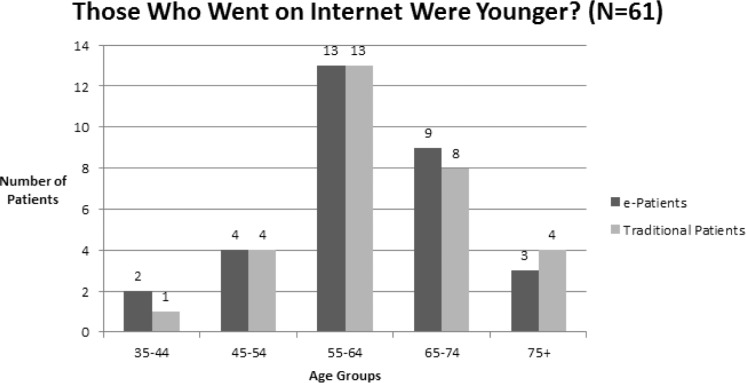
Chi-square testing was performed to detect a relationship between age-group and patients responses to question 6 (“Did you use the Internet to find out more information about your illness?”). The association was not significant (p = 0.97). (The data is presented below in Figure 3.)
Figure 3.
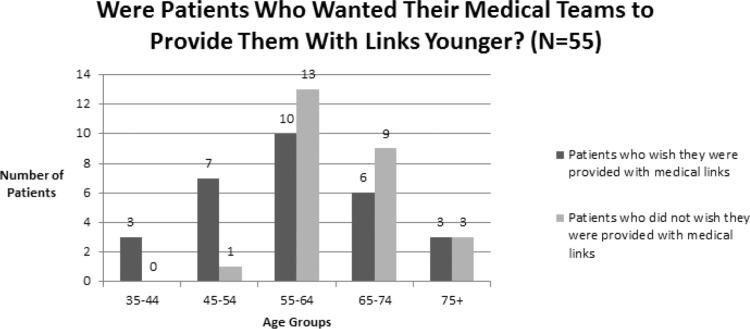
Chi-square testing was also performed to test for a relationship between age-group and the results of question 7b, did patients wish their medical teams provided them with relevant links. The association was not significant (p = 0.079). (The data is presented below in Figure 4.)
Figure 4.
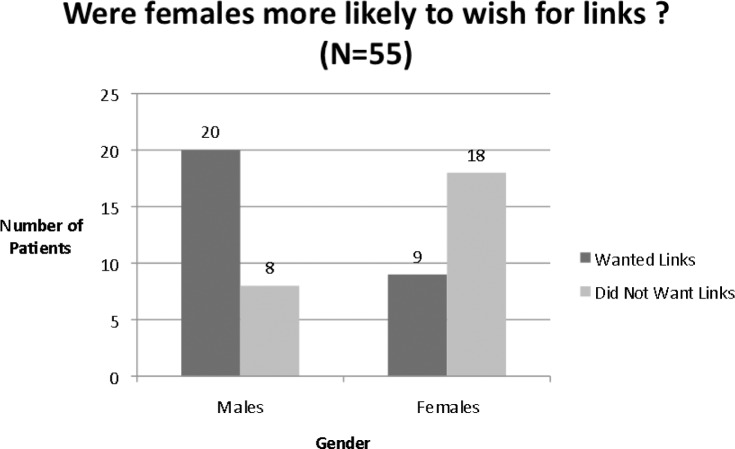
Gender had no significant relationship regarding how one answered question 6 (p = 0.6995). However, regarding question 7b, did patients wish their medical teams provided them with relevant links, men were significantly more likely to wish their medical teams provided them with links (p = 0.0047). (The data is presented below in Figure 5.)
Figure 5.
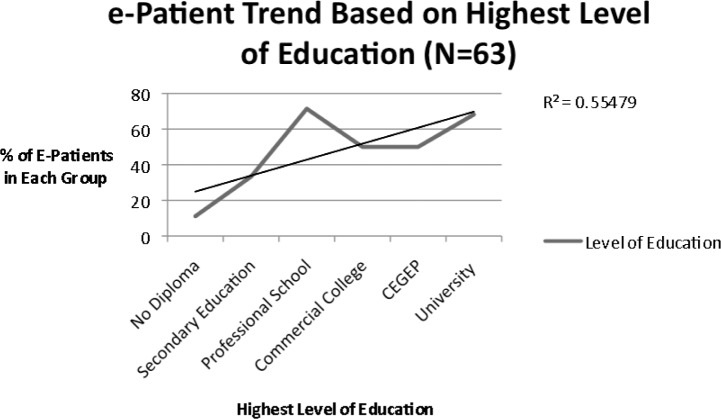
When patient were grouped by those who had selected no diploma, high school, professional school, commercial college, CEGEP, and university, more educated patients were more likely to be e-Patients (p = 0.046 ). The data is present below in Figure 6. The trend line is presented below with an R2 = 0.55. (The data is presented below in Figure 7.)
Figure 6.
Figure 7.
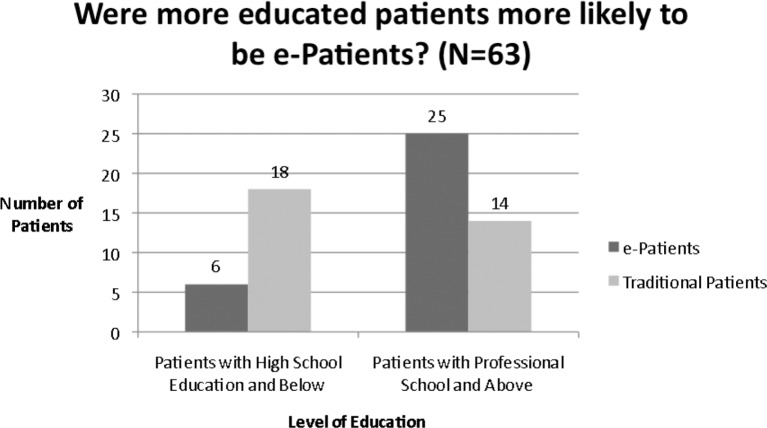
This trend is more dramatic when all the education levels were combined into two categories: high school education and below versus those with higher level degrees (p = 0.0026). (Data presented below in Figure 8.)
Figure 8.
Patients with nurse navigators to assist them were no less likely to use the Internet for supplementary information about their healthcare (p = 0.38).
E-Patients were not less satisfied by the information they received from their medical teams (p = 0.41).
Discussion
This study assessed the manner in which patients utilize modern means of communication to interact with their medical teams. Unsurprisingly, in 2011-2012, most patients had an e-mail address and Internet access. Most of the patients did not have any e-mail contact with their treatment team, and did not desire such contact. Roughly half of the patients went on the Internet to get information about their condition.
Most of the patients did not get Internet references from the treatment team, but roughly half (44%) wished they had received them. Most of the patients did not wish to complete the survey online, make appointments online, or communicate with the hospital via SMS.
In a prior study, Peleg et al. found that 47% of patients were very interested in receiving their physician’s cell phone number (5). This percentage of patients is roughly comparable to the findings in our study where 44% of patients would have liked to receive links from their medical teams. This similarity could indicate that roughly 45% of cancer patients feel they have questions, which they cannot answer on their own. Alternatively, this could indicate that roughly 45% of cancer patients could be considered particularly engaged and that they would like all possible resources of information made available to them. Either way, providing patients with a list of approved websites presents another option for patients to learn more about their disease and treatment.
Of the 225 patients involved in this study only 19 (8%) of patients received links to medically relevant websites. Out of the 98 patients who indicating that they wished their medical teams provided them with links to websites containing information about their illness, about one-third of these patients did not independently search for links. This indicates that a substantial minority of patients wish to become e-Patients, but that the lack of direction from their care team is the primary obstacle to this transformation.
Regarding to the relationship between demographic information and internet usage, prior studies have established age (6-8) and gender (8) as major predictors of which patients will use the Internet for supplementary information, these findings were not replicated in our population.
Bansil et al. found that women were 1.36 times more likely to search for medical information on the Internet (8). However, our study found no significant effect of gender on the likelihood of a patient to be an e-Patient. Surprisingly, men were actually significantly more likely to indicate that they wished to receive links from their medical teams.
Regarding the effect of age on e-Patients, roughly 50% of each age-group in our patient population made the criteria to be considered e-Patients. As of 2009, in Canada 71.6% of 35-54 year olds, 69.1% of 55-64 year olds, and 65.9% of individuals 65+ years of age, were likely to use the Internet once a day (9). Given the minor disparity in average Internet usage rates between age groups, it seems likely that a patient’s age is no longer a useful indication of his or her likelihood to act as an e-Patient. It is important to note that in this study there were only 3 patients in the 35-44 age group, and only 7 patients in the 75+ group. Therefore, despite the fact that in this study no significant effect of age on a patient’s likelihood to be an e-Patient was found, further studies with larger sample sizes are needed to confirm this finding.
Taken together the findings in this study related to gender and age represent a closing of the gap between patients of different ages and genders and the likelihood of these patients to act as e-Patients. Therefore, it is important that medical teams make web resources available to their patients, regardless of age or gender.
However, in line with previous findings (7, 10), education level was found to be significantly related to Internet usage. The most dramatic results were found when comparing those with up to a high school diploma versus those who have achieved higher levels of education.
It was hypothesized that patients with nurse navigators would be less motivated to become e-Patients, because they would have more accessible health care guidance available to them. However, whether a patient had a nurse navigator, or not, had no significant effect on whether or not a patient was likely to be an e-Patient.
It was also hypothesized that patients who were dissatisfied with the information they received from their medical teams would have been more likely to turn to the Internet and to become e-Patients, but no such effect was found. However, it is important to note that of the patients who responded, they were all either satisfied or very satisfied, making statistical testing unlikely to yield meaningful results.
Other common demographic variables such as patient’s race and family income were not investigated in this study. Previous research has demonstrated that race has no significant impact on whether or not patients were likely to act as e-Patients (4, 10). Regarding family income, findings have been conflicting (4, 8, 10).
Though physician reactions to e-Patients vary, according to findings by Ahmad et al. many physicians are resistant to patients mentioning information they have learned about their conditions from the Internet, because the information acquired can confuse the patient and encourages the formation of misguided self-diagnoses (11). According to this view, physicians have been impelled to adopt a new role as interpreters of web resources (11). Similarly, other researchers have observed that some patients are hesitant to discuss information they have learned from the Internet about their condition because they fear being labeled difficult (12, 13). However, given the results of this study and others (12), e-Patients exist in large numbers and are likely to become increasingly common as the Internet continues to expand. One encouraging finding is that both patients and physicians were more satisfied after the initial medical consultation if online health information was discussed (12). Therefore, it will be beneficial for medical teams to adjust to their new role as apomediaries of medical knowledge.
Conclusion
Given the key finding in this study i.e., many patients wish to be provided with links aggregated by their healthcare teams, the radiation oncology department at CHUM is currently compiling a collection of web-resources to give to patients. Hopefully, this will enable more patients to become e-Patients. Similarly, because roughly half of the patients surveyed would have liked to have their physician’s e-mail address, physicians at CHUM will begin communicating with their patients via e-mail.
While this study focused on results from a modern means of communication survey given to a relatively small number of patients at CHUM in Montreal, Quebec, the results have more general implications. To continue providing satisfactory and above satisfactory healthcare medical teams must continue adapting to patient evolving communication needs.
Abbreviations
- e-Patient:
Electronic Patient
- CEGEP:
Collège d’enseignement général et professionnel (General and Vocational College)
- CHUM:
Montreal University Health Centre
Footnotes
Conflict of Interest: We certify that while performing this study and writing this paper we had no conflicts of interest. Furthermore, this paper is original and has not been submitted for publication elsewhere.
References
- 1.Ferguson T & Group e-PSW. e-patients: how they can help us heal healthcare (2007).
- 2.Canada Go. Internet use by individuals, by location of access, by province (Canada) (2010).
- 3.Canada Go. Internet use by individuals, by location of access, by province (Quebec) (2010).
- 4.Kim K, Kwon N. Profile of e-patients: analysis of their cancer information-seeking from a national survey. Journal of Health Communication 15, 712-733 (2010). DOI: 10.1080/10810730.2010.514031. [DOI] [PubMed] [Google Scholar]
- 5.Peleg R, Avdalimov A, Freud T. Providing cell phone numbers and e-mail addresses to patients: the physician’s perspective. BMC Research Notes 4, 76 (2011). DOI: 10.1186/1756-0500-4-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ybarra ML, Suman M. Help seeking behavior and the internet: a national survey. International Journal of Medical Informatics 75, 29-41 (2006). DOI: 10.1016/j.ijmedinf.2005.07.029. [DOI] [PubMed] [Google Scholar]
- 7.Koch-Weser S, Bradshaw YS, Gualtieri L, Gallagher SS. The Internet as a health information source: findings from the 2007 Health Information National Trends Survey and implications for health communication. Journal of Health Communication 15 (Suppl. 3), 279-293 (2010). DOI: 10.1080/10810730.2010.522700. [DOI] [PubMed] [Google Scholar]
- 8.Bansil P, Keenan NL, Zlot AI, Gilliland JC. Peer reviewed: health-related information on the web: results from the HealthStyles Survey, 2002-2003. Preventing Chronic Disease 3 (2006). [PMC free article] [PubMed] [Google Scholar]
- 9.Canada Go. Internet use by individuals, by selected frequency of use and age (At least once a day) (2010).
- 10.Atkinson NL, Saperstein SL, Pleis J. Using the internet for health-related activities: findings from a national probability sample. Journal of Medical Internet Research 11, e4 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ahmad F, Hudak PL, Bercovitz K, Hollenberg E, Levinson W. Are physicians ready for patients with Internet-based health information? Journal of Medical Internet Research 8 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hay MC, Cadigan RJ, Khanna D, Strathmann C, Lieber E, Altman R, McMahon M, Kokhab M, Furst DE. Prepared patients: internet information seeking by new rheumatology patients. Arthritis and Rheumatism 59, 575-582 (2008). DOI: 10.1002/art.23533. [DOI] [PubMed] [Google Scholar]
- 13.Imes RS, Bylund CL, Sabee CM, Routsong TR, Sanford AA. Patients’ reasons for refraining from discussing Internet health information with their healthcare providers. Health Communication 23, 538-547 (2008). [DOI] [PubMed] [Google Scholar]