Abstract
Background:
Liposuction of the arms alone may be inadequate for aesthetic improvement because of skin laxity. Radiofrequency-assisted liposuction (RFAL) and aggressive superficial liposuction (SupL) have been described to stimulate soft tissue retraction to improve results. We compare the techniques and describe a classification scheme that factors skin laxity, skin quality, and Fitzpatrick type to provide treatment recommendations.
Methods:
Ten consecutive female patients underwent RFAL of 1 arm and SupL on the contralateral arm. All patients had Fitzpatrick skin types of III, IV, or V with an average body mass index of 26.0. Using fluorescent tattooing, key points on the arm skin were measured preoperatively and postoperatively to indicate changes in surface area.
Results:
There were no complications in the group, and all patients reported satisfaction with the aesthetic results. All patients showed reduction of measured skin surface areas and skin distances postoperatively. At 1 year, the measured surface area reductions on the anterior arms averaged 15.0% for RFAL and 10.9% for SupL on the anterior arm skin. Posteriorly, RFAL showed 13.1% reduction and SupL 8.1% reduction in the surface areas at 1 year. Linear reduction for RFAL averaged 22.6% and 17.8% for SupL 1 year postoperatively anteriorly.
Conclusion:
Both RFAL and SupL of the arms showed quantifiable and sustained reductions in skin surface. Good contour and soft tissue contraction were achieved with both techniques but RFAL with its safety features presents an alternative to SupL, which has a higher complication rate, risk for contour deformities, and steeper learning curve.
Nonexcisional, surgical aesthetic improvement of the upper extremities remains a challenge. Depending primarily on skin quality or laxity, brachioplasty with skin resection and a resulting undesirable long incision may be required. For less severe cases of upper arm adipose excess, suction-assisted lipectomy (SAL) may be used but is often less than adequate. This is because fat is underresected due to concern with post aspiration skin laxity and/or overresection with resulting contour problems. Techniques introduced to stimulate skin and soft tissue retraction and address the issue of post aspiration laxity include superficial liposuction (SupL),1–5 ultrasonic-assisted liposuction,6 laser-assisted liposuction (LAL),7 and radiofrequency-assisted liposuction (RFAL).8–10 SupL, originally described by others including Gasperoni, includes aggressive manual liposuction of the superficial areolar subcutaneous layer.1–5 Ultrasonic-assisted liposuction has been shown to lower the hematocrit in the aspirate and preserve adipocyte derived stem cells for fat grafting and only modestly improved skin retraction.6 Randomized, blinded studies showed skin contraction of 17% at 3 months after LAL compared with under 10% for SAL.7
It has been postulated that radiofrequency (RF) energy modulated soft tissue tightening is because of immediate and long-term thermal contraction of the fibroseptal network (FSN) in the subcutaneous space and because of a nonablative, inflammatory heating of the dermis caused by the RF energy applied in a bipolar manner.9,10 Recent randomized, blinded papers have shown 35% soft tissue contraction at 12 months with RFAL. This was compared with 8.1% soft tissue contraction observed in nonthermal, traditional suction-assisted lipoplasty at the same time interval.11 Treating upper arms presents distinct challenges because the soft tissue is nonadherent to the underlying supportive structures and is often thin and lacking much fat. In either case, there is less FSN “substrate” available to be stimulated with RF energy to result in significant contraction.
In this study, 10 patients underwent preoperative fluorescent tattoo marking of the bilateral arms. One extremity was treated with RFAL plus traditional SAL and the contralateral arm was treated with aggressive, SupL also followed by standard SAL. In addition to photographic documentation, key tattoo markings were measured at 6 and 12 months postoperative periods. The purpose of this study is to compare the results of RFAL and SAL on 1 arm and those obtained with SupL in the contralateral arm in the same patient. By measuring the differences in the preoperative and postoperative markings, changes in the skin are quantified. Based on these data and clinical experience in upper extremity arm contouring, we propose a new classification scheme that takes into account skin laxity, skin quality, and Fitzpatrick skin type. This acts a “road map” of recommended treatments to help navigate the difficult waters of arm contouring.
MATERIALS AND METHODS
Between July 2012 and July 2013, 10 female patients, aged 18–48 (average age 33.6) underwent RFAL using the Bodytite minimally invasive RF platform (Invasix Corp., Yokneam, Israel) and completion standard SAL on 1 upper extremity and SupL and completion SAL on the contralateral upper extremity. Completion SAL was performed with the power-assisted liposuction device (Microaire, Charlottesville, Va.). The procedures were either performed under Institutional Review Board protocol (Essex Inc., Lebanon, N.J.). All patients underwent a complete history and physical with appropriate screening laboratory values and medical workups as needed. One arm was randomly selected by coin flip to be treated with RFAL, whereas the contralateral arm was treated with SupL + SAL (ie, no RF energy). The Fitzpatrick skin type ranged from III to V (with 50% of the patients being skin types IV and V), and the average body mass index was 26.0. All operations were performed under general anesthesia with tumescent infiltration. Total average aspirate volume for both arms was 957 mL.
Markings
As described previously,12 it is helpful to identify the point of maximal dependency (PMD), which coincides with the point of maximal laxity when the arm is held perpendicular to the long axis of the body and with the forearm at 90 degrees to the humerus whereas the palm of the hand is facing anteriorly (Fig. 1). A line is then drawn perpendicularly from the same point at the bicipital groove to the PMD; this measurable distance can be used to determine skin retraction following a procedure. Similarly, 3 points are marked in the anterior and posterior skin to form 2 equilateral triangles of known area (Figs. 2, 3). The resulting changes in the markings are measurable postoperatively, and the areas of the triangles may be calculated using a geometrical equation known as Heron’s formula, which states that the area (T) of a triangle whose sides have lengths a, b, and c equals:
Fig. 1.
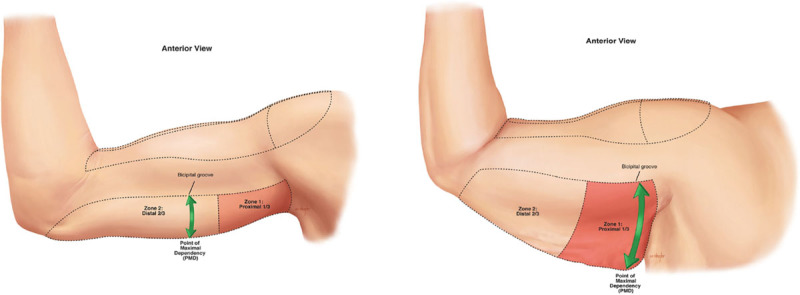
ASL is quantified as the distance measured between the most dependent point of the skin, or PMD, and the perpendicular point on the bicipital groove.
Fig. 2.
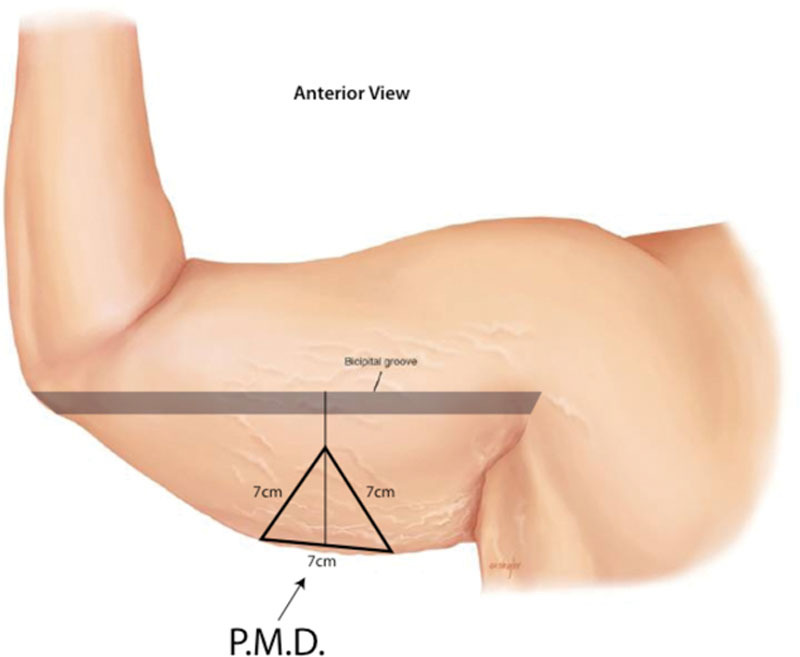
The 2 points of the PMD and the 3 corners of an equilateral triangle of known dimensions and surface area are tattooed with fluorescent ink preoperatively. The limbs of the triangle are measured at specific times postoperatively to calculate the change in surface area.
Fig. 3.
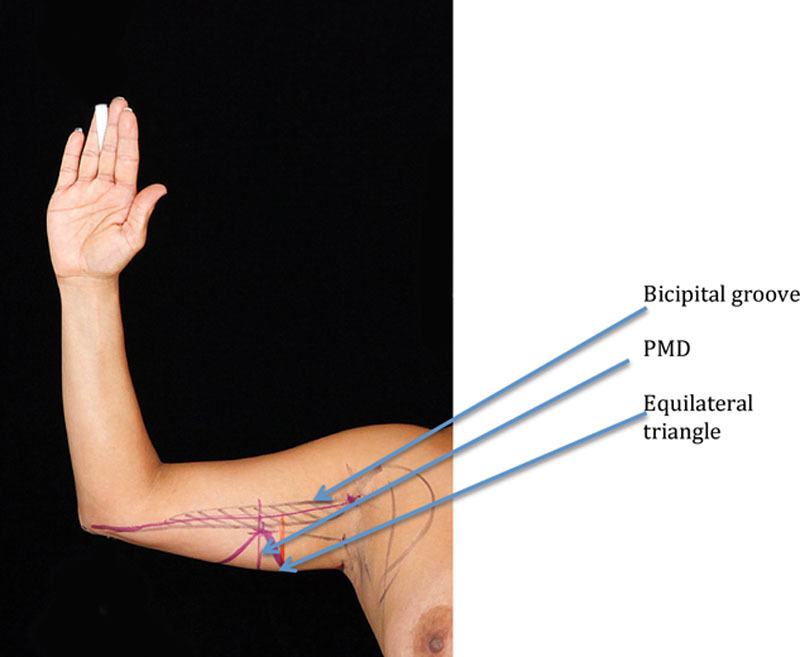
Clinical correlate of preoperative markings. The bicipital groove (hash marks) is perpendicular to the PMD (vertical purple line). The PMD represents the height of the equilateral triangle with the vertex coincident with the bicipital groove and the base of the triangle along the most dependent portion of the triceps skin in this position.
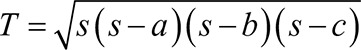 |
where S is the semiperimeter of the triangle:
 |
These quantifiable changes in area correspond to the degree of skin and soft tissue retraction. Over time, the stability of the changes in area may indicate the durability of the outcomes over 6 and 12 months postoperatively. For this study, intradermal fluorescent tattoo ink was used to mark the key points, as previously described.6 In ordinary light, the marks are invisible but are easily found using an ultraviolet light source to make the measurements.
Next, the quality of the skin of the arms is then evaluated where the presence or absence of striae, measurement of the dermal thickness, quantity of subcutaneous fat, and Fitzpatrick skin type are noted. The presence of striae indicates permanent damage to the dermis. Patients are counseled that the presence of striae may affect the overall aesthetic result by limiting the contractile nature of the dermis and compromising the redraping of the skin envelope. Total dermal thickness and quantity of underlying soft tissue structures, particularly the amount of adipose tissue and FSN, affect the potential for skin contraction with RFAL.10,13 We have found, in our experience, that the thicker the dermis, the greater the degree of contraction and that the skin quality, laxity, and Fitzpatrick skin type are the most important determinants in candidate selection for RFAL of the arm. We define arm skin laxity (ASL) as the distance between the most dependent point of the skin and the bicipital groove with the arm positioned in a 90 degree flexed position (Fig. 1). The ASL ranges from mild (<5 cm), moderate (5–10 cm), or severe (>10 cm; Table 1). Arm skin quality (ASQ) is defined by subjective visual assessment and the pinch test. Good ASQ has good skin turgor, no striae, and an absence of fine wrinkling. Poor ASQ has moderate to poor skin turgor with the presence of striae and fine wrinkles (Table 2). The presence or absence of excess adipose tissue is an important factor in candidate selection. RF-mediated FSN contraction requires an adequate adipose layer and underlying matrix for it to be effective.10,13
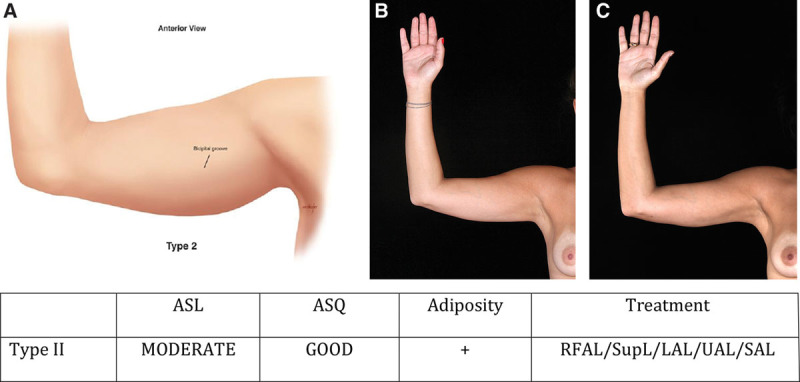
Table 1.
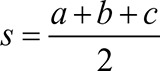
Average Percent Changes Measured Postoperatively in Bicipital Groove to PMD Distance Compared with Preoperative Measurements
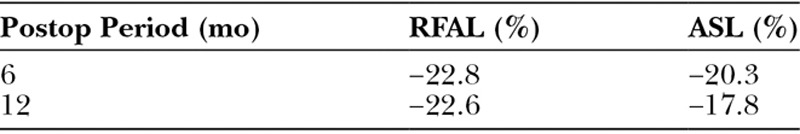
Table 2.
Average Postoperative Surface Area Percent Changes Measured (Anterior Arm)
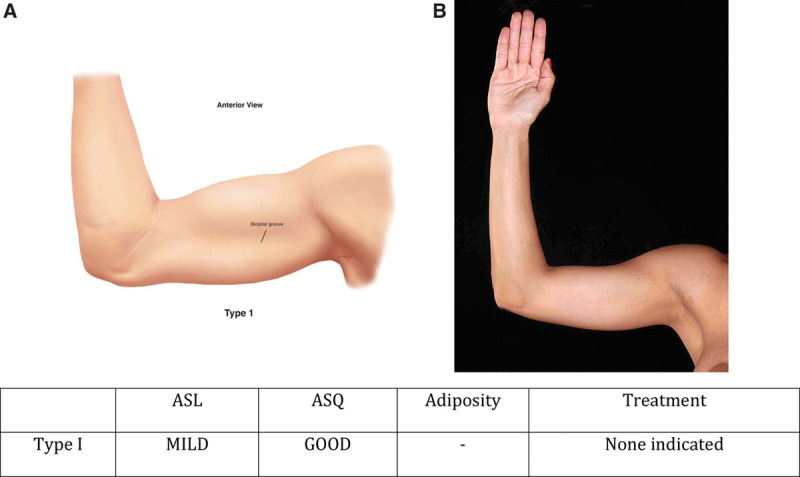
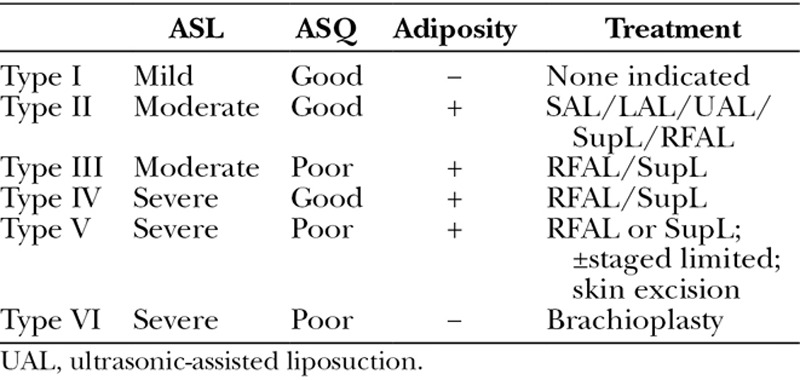
Once the patient’s arms are classified according to their ASQ and ASL, a treatment plan is proposed (Table 3). The ASL ranges are shown (Table 4), and the ASQ terms of definition are provided (Table 5). A type I arm is defined as one that has mild ASL with good ASQ and no adiposity (Fig. 5). A type II arm has moderate ASL, good ASQ, and moderate subcutaneous fat (Fig. 6). A moderate ASL, poor ASQ, and moderate to large quantities of fat are typical of a type III arm (Fig. 7). Type IV arms are generally larger in size with severe ASL but with good ASQ and large quantities of fat (Fig. 8). Type V arms (Fig. 9) have more severe ASLs, poor ASQs, and larger quantities of fat. Type VI arms (Fig. 10) exhibit severe ASL, poor ASQ, and a relative lack of fat and other soft tissues like FSN.
Table 3.
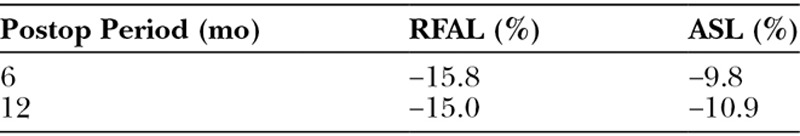
Average Postoperative Surface Area Percent Changes Measured (Posterior Arm)
Table 4.
ASL Ranges
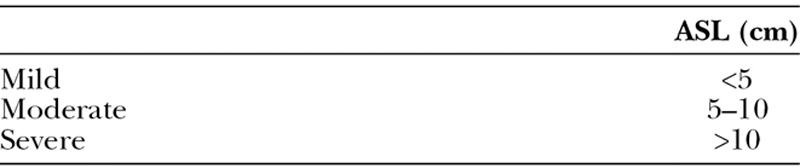
Table 5.
ASQ Definition of Terms
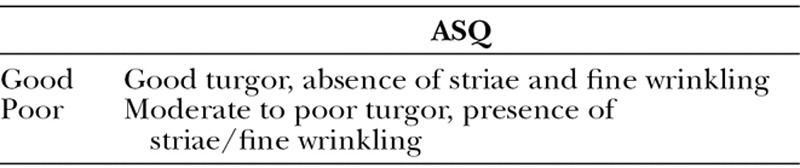
Fig. 5.
Idealized image (A) and clinical correlate (B) of a type I arm, right anterior view. No operation is indicated.
Fig. 6.
Idealized image (A) and clinical correlate of a type II arm, preoperative (B) and 1 year postoperative (C), right anterior view after LAL as an alternative procedure of bilateral arm of a 25-year-old woman at 1450 mL aspirate volume and 49,000 J RF.
Fig. 7.
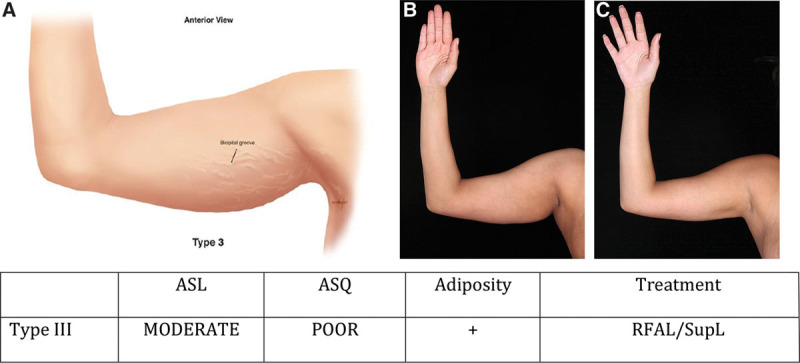
Idealized image (A) and clinical correlate of a type III arm preoperative (B) and 1 year postoperative (C), right anterior view of right arm of a 30-year-old woman at 35 watts, 38°C temperature maximum, 600 mL aspirate volume, and 30.2 kJ RF.
Fig. 8.
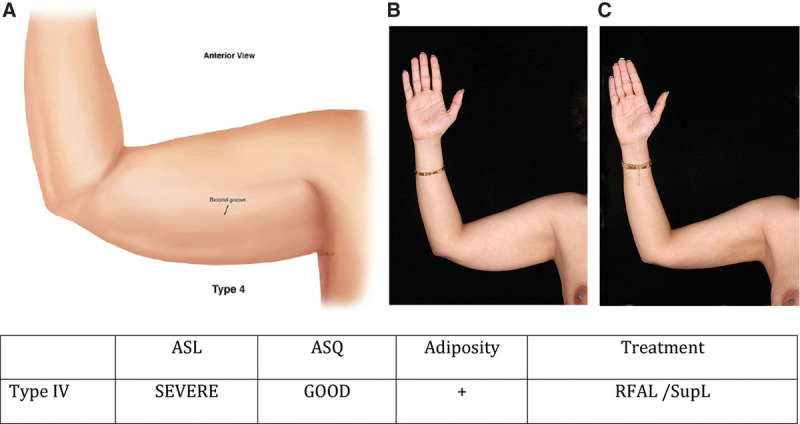
Idealized image (A) and clinical correlate of a Type IV arm, preoperative (B) and 1 year postoperative (C), right anterior view of right arm of a 40-year-old woman at 35 watts, 38°C temperature maximum, 700 mL aspirate volume, and 20.3 kJ RF.
Fig. 9.
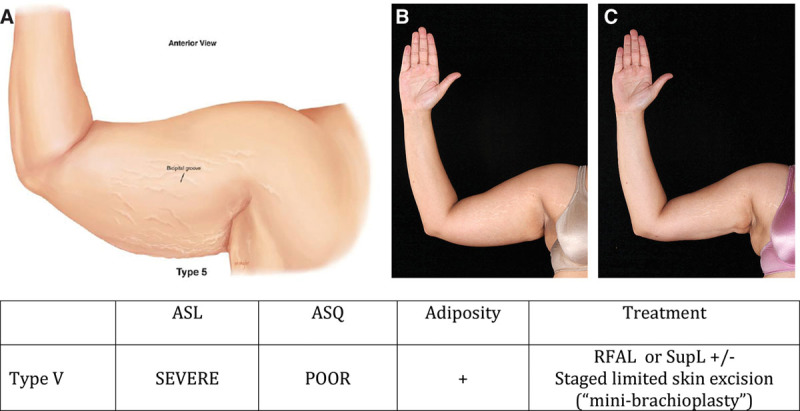
Idealized image (A) and clinical correlate of a type V arm, preoperative (B) and 1 year postoperative (C), right anterior view of right arm of a 28-year-old woman at 35 watts, 38°C temperature maximum, 1200 mL aspirate volume, and 18.3 kJ RF. RFAL only.
Fig. 10.
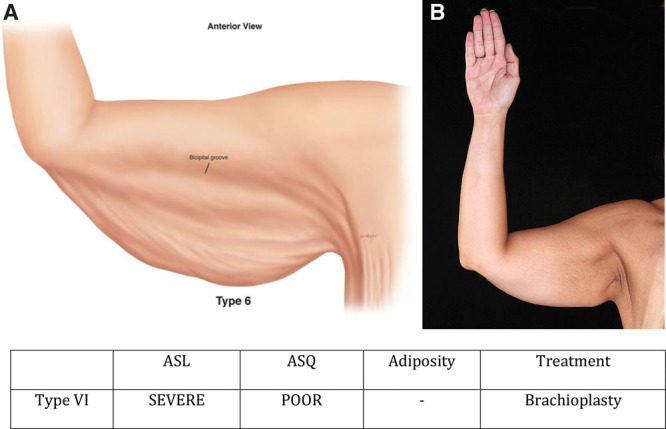
Idealized image (A) and clinical correlate (B) of a type VI arm, right anterior view. This patient is not an RFAL candidate.
Procedure
All procedures were performed under general anesthesia. Sequential compression stockings were in place, and prophylactic intravenous antibiotics were given. In addition to the tattoo markings, standard topographic liposuction markings were drawn preoperatively. Access puncture incisions in the elbow, axilla, and deltoid were made with a 14-gauge needle. Tumescent solution was composed of 400 mg of lidocaine (0.04%) and 1 mL of 1:1000 concentration epinephrine per liter normal saline infused into the subcutaneous space of the upper extremity. The arm to be treated with RFAL was chosen randomly by coin flip. After tumescent infiltration, the inferior electrode of the BodyTite device (Invasix Corp.) was placed into the subcutaneous space with the corresponding external electrode on the surface of the skin (Fig. 4). Sterile aqueous-based gel was used to decrease the impedance of the contact patch between the skin and the external electrode. The RFAL device settings included an epidermal temperature maximum setting (Tmax) of 38–40°C and the power setting at 38 watts. The device was moved in a back and forth motion similar to liposuction technique to deliver the RF energy evenly. Multiple depths of the soft tissue were treated to the target temperature with special consideration given to not exceeding the preset Tmax. The device has a real-time thermostat that gives continuous temperature reading at the skin surface. The automatic cutoff feature prevents overheating the tissues as the current is discontinued as soon as the high temperature setting is reached.12
Fig. 4.
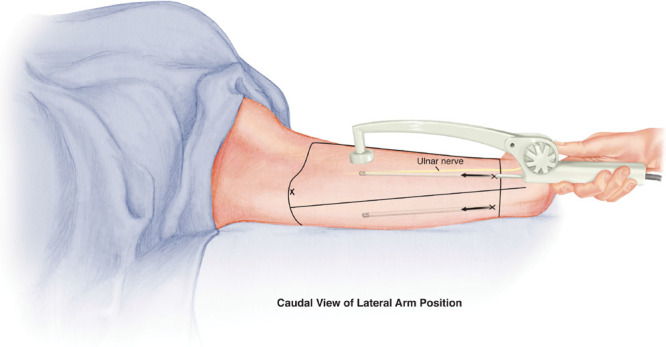
RFAL device illustrated with left upper extremity in extended and flexed position. Note the entry points proximal to elbow and consideration given to avoiding the ulnar nerve.
The deep, intermediate, and superficial layers were individually treated to ensure the FSN, and the skin components were included. This resulted in even heating of the soft tissues between the electrodes and coagulation of the adipose tissue. In this study, internal RF energy was not applied directly to the subdermal space. The internal electrode has an aspirating port to remove any excess fluid and heated oil byproducts immediately to avoid any “hot spots.” Once the Tmax was achieved evenly, the device was moved to the next area of treatment until all proposed areas were treated. This was followed by standard liposuction utilizing the power-assisted liposuction device. The contralateral arm underwent identical tumescent infiltration. Aggressive manual and power-assisted SupL was performed until comparable quantities of aspirate and appropriate visual and tactile endpoints were achieved. All access incisions were closed with 5-0 nylon sutures, and the patient was placed in compression garments for 3 weeks.
RESULTS
There were no mortalities or complications. Five patients were classified as type III, 3 as type IV, and 2 as type V. The average amount of aspirate was 534 mL total and 341 mL fat per arm. All 10 patients had measurable changes in the markings and calculations and reported satisfaction with the overall operation (all 10 patients would have undergone the procedure again given the choice). The average percentage of change in the linear reduction in the PMD measured in the arms treated with RFAL was 22.8% at 6 months and 22.6% at 12 months. The contralateral arms treated with SupL showed 6-month and 12-month reductions in the PMD of 20.3% and 17.8%, respectively (Table 1).
The surface areas of the anterior and posterior arms were calculated using a mathematical ( Heron’s) formula where the limbs of a triangle are known. At 6 months, the RFAL treated arms showed reductions in surface area of 15.8%, and the SupL arms showed a 9.8% reduction anteriorly. After 1 year, RFAL treated arms were at 15.0% and the SupL arms 10.9% reduction (Table 2). Posteriorly, RFAL treated arms showed reductions in the surface area of 7.9% at 6 months and 13.1% after 12 months. The SupL arms indicated 6- and 12-month posterior surface area reductions of 2.0% and 8.1%, respectively (Table 3).
DISCUSSION
Energy-assisted liposuction exists in multiple modalities. Previous studies have shown skin tightening to occur in response to energy-assisted liposuction.6,7,10,11,13 Aesthetic contouring of the arm presents challenges where laxity of the skin can be exacerbated with liposuction unless appropriate patient selection and operative technique are chosen. This article compares RFAL with SupL and (1) quantifies the soft tissue contraction postoperatively, (2) measures these changes over 12 months, (3) provides a group not treated with RF energy (SupL treated contralateral arms) with which to compare, and (4) presents a classification scheme with a so-called “road map” of recommended therapies.
The data collected after 12 months show a durable result in aesthetic improvement of the arms in all measurable aspects. Although there was a trend suggestive of greater soft tissue contraction after RFAL compared with SupL, this was not shown to be statistically significant because of the small sample size. In a recent, randomized, blinded study, it was shown that RFAL resulted in 35% contraction of the soft tissue at 1 year compared with 8.1% on the contralateral side of the abdomen, where standard liposuction was performed.11 It was noted in this study that the soft tissue of the abdomen was located in what has been described as an “adherent zone” where there is more FSN to recruit with the RF energy than that is seen in the upper arm. In addition, the patients in the abdomen study were categorized as Fitzpatrick skin types I and II. These patients generally have a thinner dermis and are less likely to respond to aggressive subdermal SAL or standard SAL alone. In this study, all patients were categorized as Fitzpatrick types III–V. Patients with darker complexions have been postulated to respond to nonthermal (mechanical) and thermal stimulus with greater collagen formation, which may help, together with the aggressive subdermal liposuction, explain the more favorable skin contraction seen with SupL in our study, compared with other papers in the literature. Specifically, this study showed 17.8% area soft tissue contraction at 1 year using nonthermal, aggressive, superficial, subdermal liposuction in darker Fitzpatrick patients. Other contraction studies11 have shown traditional SAL to achieve less than 8% soft tissue at 12 months, as the subdermal space was not aggressively violated. However, the risks associated with aggressive SupL have made this a less popular technique for liposuction surgeons. RFAL provides an option with safer, monitored temperature controlled RF contraction without having to violate the immediate subdermal space. The average percentage of change in the linear reduction in the PMD measured in the arms treated with RFAL was 22.6% at 12 months. This 22.6% RFAL contraction at 1 year is noteworthy as there was little FSN for RF-mediated contraction and aggressive subdermal techniques did need to be used. There is a subdermal, nonaspirating RF heating applicator (Invasix, Yokanem, Israel) that can be applied safely and directly to subdermal space to deliver a coagulative subdermal heating, leading to remodeling and direct dermal contraction without the need for FSN. By combining subdermal heating with RFAL, soft tissue contraction and subdermal heating can be performed, which may lead to even greater skin contraction than RFAL alone.14 By employing RFAL, surgeons may avoid the more difficult and potentially more morbid, superficial, aggressive subdermal liposuction procedures and achieve equivalent, if not superior, results.
Based on the categories of arms described in the Materials and Methods section, a treatment protocol may then be proposed (Table 6.) A type I arm has minimal ASL with good ASQ and minimal adiposity; no intervention is recommended (Fig. 5). Type II arms (moderate ASL, good ASQ and moderate subcutaneous fat) may benefit from SAL, LAL, or RFAL (Fig. 6). Type III arms have moderate ASL, poor ASQ, and moderate to large quantities of fat (Fig. 7). These patients are RFAL and SupL candidates. Type IV arms are generally larger in size with severe ASL but with good ASQ and large quantities of fat. These patients may also benefit from RFAL or SupL (Fig. 8). A patient underwent RFAL in the right arm and SupL on the left to provide a direct comparison of the 2 techniques. She had equal quantities of total aspirate removed (320 mL) from both arms and did not have any complications. The aesthetic results of the RFAL arm are at least comparable, if not more favorable, than with the contralateral SupL arm. Type V (Fig. 9) arms with severe ASL, poor ASQ, and large quantities of fat may be treated with RFAL or SupL and a staged limited skin excision operation, or modified brachioplasty. Type VI arms (Fig. 10) are not candidates for RFAL or SupL at any stage because the severe ASL, poor ASQ, and relative lack of fat and other soft tissue require an excisional operation to achieve a satisfactory aesthetic result. Ideal candidates for RFAL are types II, III, and IV.
Table 6.
Triceps Skin Classification Scheme with Proposed Treatment
The overall aesthetic results between the RFAL treated arms and the aggressive SupL treated arms appeared comparable in this small sample size. However, aggressive superficial SAL, while effective, is technically much more demanding and at much greater risk of causing contour deformities with a steeper learning curve than traditional SAL or RFAL. Even surgeons with vast experience, Kim et al15 demonstrated an 8.6% overall major complication rate in 2398 patients. Complications included seroma, skin necrosis, infection, asymmetry, pigmentation changes, and chronic induration in addition to skin irregularities.15 In this small sample size of 10 patients (20 arms), there were no complications noted despite the previous publications from Kim et al15 (8.6%) and Theodorou et al12 (minor 8.3%, major 6.3% complication rates). The second generation RFAL device has real-time temperature reading, automatic cutoff mechanisms, and a much deeper and controlled depth of thermal treatment. This current RFAL platform has several inherent safety features that allow the less experienced operator to confidently approach these difficult challenges with potentially superior soft tissue contraction and a lower complication rate. In particular, the deeper plane in which RFAL is performed minimizes unwanted, uneven contouring that may occur during the liposuction phase when compared with the aggressive, superficial SAL technique. We hypothesize that surgeons utilizing RFAL of the upper arms may obtain comparable or superior results to aggressive superficial, subdermal SAL with a favorable safety profile and fewer aesthetic complications. The learning curve with RFAL is much less onerous than that of SupL and can be performed in a reproducible and predictable manner. In addition, RFAL may be a safe and effective option for upper arm contouring in patients with lighter Fitzpatrick skin types I and II where nonthermal techniques are likely to be less effective in stimulating the dermis than those of patients with darker skin types.
CONCLUSIONS
RFAL exhibited good soft tissue contraction on the soft tissue of arms where there was a relative paucity of adipose tissue, which was nonadherent and devoid of large amounts of FSN. Despite the reduced FSN compared with larger more adherent areas of the body, the average soft tissue contraction with RFAL was significant (22.8%) at 1 year, and good contour and soft tissue retraction was achieved without using the more risky aggressive subdermal liposuction techniques. In this study, aggressive subdermal liposuction also appears to provide a significant degree of soft tissue contraction, with an average of 17.8% in darker skin Fitzpatrick patients with a thicker, more responsive dermis. RFAL, with computer monitored and temperature controlled RF delivery, appears to be a safer alternative to elicit soft tissue contraction in upper arms without the need for aggressive, subdermal liposuction. Together with qualitative and quantitative terms to categorize the upper arms, a new classification of upper arm liposuction is presented and one that helps guide treatment options.
Footnotes
Disclosure: C.T. Chia and S.J. Theodorou are consultant for Invasix Corp. Invasix Corporation provided transportation and lodging for C.T. Chia, S.J. Theodorou, and G.H. Pitman and patients received remuneration of $325 each. Dr. Hoyos does not have any financial disclosures. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Gasperoni C, Salgerello M, Emiliozzi P, et al. Subdermal liposuction. Aesthetic Plast Surg. 1990;14:137–142. doi: 10.1007/BF01578339. [DOI] [PubMed] [Google Scholar]
- 2.Gasperoni C, Gasperoni P. Subdermal liposuction: long-term experience. Clin Plast Surg. 2006;33:63–73,vi. doi: 10.1016/j.cps.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 3.Gasperoni C, Salgarello M. Rationale of subdermal superficial liposuction related to the anatomy of subcutaneous fat and the superficial fascial system. Aesthetic Plast Surg. 1995;19:13–20. doi: 10.1007/BF00209305. [DOI] [PubMed] [Google Scholar]
- 4.Gasperoni C, Salgarello M. MALL liposuction: the natural evolution of subdermal superficial liposuction. Aesthetic Plast Surg. 1994;18:253–257. doi: 10.1007/BF00449790. [DOI] [PubMed] [Google Scholar]
- 5.Toledo LS. Syringe liposculpture. Clinics in Plast Surg. 1996;23:683–693. [PubMed] [Google Scholar]
- 6.Nagy MW, Vanek PF., Jr A multicenter, prospective, randomized, single-blind, controlled clinical trial comparing VASER-assisted lipoplasty and suction-assisted lipoplasty. Plast Reconstr Surg. 2012;129:681e–689e. doi: 10.1097/PRS.0b013e3182442274. [DOI] [PubMed] [Google Scholar]
- 7.DiBernado BE. Randomized, blinded, split abdomen study evaluating skin shrinkage and skin tightening in laser-assisted liposuction versus liposuction control. Aesth Surg J. 2010;30:593–602. doi: 10.1177/1090820X10380707. [DOI] [PubMed] [Google Scholar]
- 8.Hurwitz D, Smith D. Treatment of overweight patients by radiofrequency-assisted liposuction (RFAL) for aesthetic reshaping and skin tightening. Aesthetic Plast Surg. 2012;36:62–71. doi: 10.1007/s00266-011-9783-z. [DOI] [PubMed] [Google Scholar]
- 9.Mulholland RS. Radio frequency energy for non-invasive and minimally invasive skin tightening. Clin Plast Surg. 2011;38:437–448, vi. doi: 10.1016/j.cps.2011.05.003. [DOI] [PubMed] [Google Scholar]
- 10.Paul M, Mulholland RS. A new approach for adipose tissue treatment and body contouring using radiofrequency-assisted liposuction. Aesth Plast Surg. 2009;83:687–694. doi: 10.1007/s00266-009-9342-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Duncan DI. Nonexcisional tissue tightening: creating skin surface area reduction during abdominal liposuction by adding radiofrequency heating. Aesthet Surg J. 2013;33:1154–1166. doi: 10.1177/1090820X13505862. [DOI] [PubMed] [Google Scholar]
- 12.Theodorou SJ, Chia CT. Radiofrequency-assisted liposuction for arm contouring: technique under local anesthesia. Plast Reconstr Surg-Global Open. 2013;1:e37. doi: 10.1097/GOX.0b013e3182a58c80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Paul M, Blugerman G, Kreindel M, et al. Three-dimensional radiofrequency tissue tightening: a proposed mechanism and applications for body contouring. Aesth Plast Surg. 2011;35:87–95. doi: 10.1007/s00266-010-9564-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mulholland RS. Nonexcisional, minimally invasive rejuvenation of the neck. Clin Plast Surg. 2014;41:11–31. doi: 10.1016/j.cps.2013.09.002. [DOI] [PubMed] [Google Scholar]
- 15.Kim YH, Cha SM, Naidu S, et al. Analysis of postoperative complications for superficial liposuction: a review of 2398 cases. Plast Reconstr Surg. U.S. 2011;127:863–871. doi: 10.1097/PRS.0b013e318200afbf. [DOI] [PubMed] [Google Scholar]


