Key Clinical Message
Idiopathic Systemic Capillary Leak Syndrome is a potentially fatal disorder that is under diagnosed. It commonly presents as recurrent undifferentiated shock with hypotension, hypoalbuminemia and hemoconcentration. There are three distinct phases that define the syndrome; Prodromal, Extravasation and Recovery.
Keywords: Capillary, hemoconcentration, hypoalbuminemia, hypotension, leak, shock
Introduction
Idiopathic Systemic Capillary Leak Syndrome (ISCLS) is an extremely rare condition characterized by the triad of cyclical and episodic hypotension, hemoconcentration and hypoalbuminemia 1. The underlying pathological mechanism appears to manifest by episodic endothelial barrier dysfunction 1. ISCLS is a diagnosis of exclusion that without appropriate management has a significant morbidity and mortality 1. We report a new case of ISCLS, describing the approach to diagnosis and management.
Case Report
A 51-year-old male presented to an Australian emergency department with a one day history of increasing fatigue and general malaise preceded by nausea, vomiting, myalgia and arthralgia. This was the sixth presentation with similar symptoms within a six month period and despite extensive investigations, a diagnosis had not been established.
His past medical history included mild obstructive sleep apnea, prior intracranial hemorrhage, and two prior hospital admissions in the UK with undefined septic shock. He reported no allergies and was taking aspirin and vitamin B12. He was a nonsmoker, but did have a long history of significant alcohol intake. His family history included a brother with lymphoma who had required an allogeneic stem cell transplant.
On examination in the emergency department, he was tachycardic (103 bpm) with oxygen saturations of 92% on room air. Other vital signs were normal. Initial investigations revealed a polycythemia (Hb 224 and RCC 6.66 × 1012/L), hemoconcentration (HCT 64%), hypoalbuminemia (albumin 34 U/L), leukocytosis (WCC 19.7 × 109/L) and a acute kidney injury (eGFR 59 mL/min/1.73 m2, creatinine 121 mmol/L). The patient appeared polycythemic and based on these results, a 130 mL venesection was performed and he was admitted to hospital. Despite fluid resuscitation, he became hypotensive (BP 83/41 mmHg) and was transferred to the Intensive Care Unit (ICU).
Following ongoing fluid replacement during ICU admission, his blood pressure normalized, although his urine output remained low (26 mL/h). He then developed pitting edema to the knees, bilateral mild basal inspiratory crackles and sacral edema. Investigations revealed a mixed metabolic acidosis with a high lactate. Blood and urine cultures were negative. Within 24 h of his ICU admission, his urine output increased dramatically to 200–500 mL/h, his hemoglobin normalized and the patient requested to discharge.
He represented to the Emergency Department a day following discharge complaining of dyspnea. He was tachypneic and hypoxic and had evidence of pulmonary edema. He was diuresed with furosemide and improved quickly.
Similar blood results were seen in an episode 6 months earlier (see Fig.1). These results demonstrate the dramatic change over a 12 h period.
Figure 1.
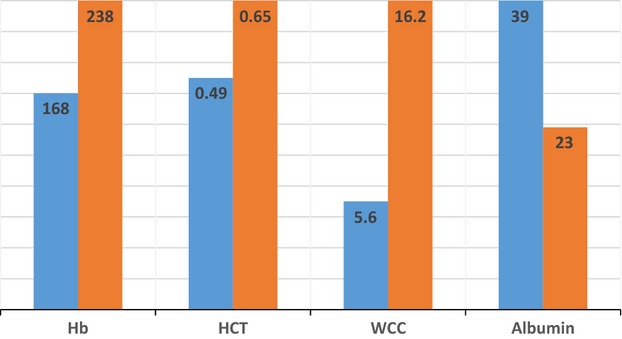
Morning versus Night blood results. Results presented as percentage of their maximum (Hb g/L, WCC 109/L, HCT %, Alb g/L).
During these presentations, he had undergone a number of investigations, the results of which are summarized in Table1. Differentials included; hematological malignancy, myeloproliferative disorder, autoimmune disease, hereditary angioedema, Gleich’s Syndrome, nephrotic syndrome and diuretic abuse (Table3).
Table 1.
Investigation results
| C3, C4, CH50 | Normal range |
| JAK 2 V617F | Negative |
| JAK exon 12 mutation | Negative |
| EPO | <1 |
| Serum Protein Electrophoresis | Monoclonal Protein Detected |
| Short Synacthen | Negative |
| Biogenic Amine Studies | Normal range |
| Serum FLC | Negative |
| Auto-immune screen | Negative |
| Bone marrow aspirate and trephine | Normal |
| Culture for SEC | Negative |
| Urine Chemistry | Normal range |
| Thyroid Function | Normal range |
| Urine diuretic screen | Negative |
Table 3.
Considered differential diagnoses
| Polycythemia Vera |
| Hereditary angioedema |
| Sepsis |
| Gleich’s Syndrome |
| Pancreatitis |
| Diuretic abuse |
| POEMS Syndrome |
| Nephrotic Syndrome |
In light of relevant negative investigation results and thorough research, it was clear that an extravasation of plasma was the cause of his hemoconcentration. Coupling his clinical picture with the Mayo Clinic Criteria 4, a diagnosis of ISCLS was made. Despite commencement of theophylline (4.5 mg BD) and terbutaline (400 mg BD), he experienced recurrent episodes. Monthly intravenous immunoglobulin (IVIG) injections were then added to his treatment regimen.
Following his previous frequent hospital and intensive care admissions the patient has now remained episode free for a year and has enjoyed a normal and healthy life. During this time he has been compliant with dual therapies, including the original Theophylline and Terbutaline as well as IVIG.
Discussion
Idiopathic Systemic Capillary Leak Syndrome, also known as Clarkson’s Disease, was first described in 1960 with a case report of cyclical edema and shock due to increased capillary permeability 2. It is a rare disorder of reversible plasma extravasation and vascular collapse accompanied by hemoconcentration and hypoalbuminemia 1(Fig.3). There are less than 150 reported cases worldwide 1,3. ISCLS is of unknown etiology, but thought to be the result of transient endothelial dysfunction due to endothelial contraction, apoptosis, and injury1 contributed by vascular endothelial growth factor (VEGF), complement, leukotrienes, and cytokines 4. As in the patient in our case report, ISCLS is often misdiagnosed as polycythemia, polycythemia vera, or sepsis. The condition has three phases, each with specific signs and risks (Fig.2). Criteria to define patients with ISCLS were described by the Mayo Clinic Experience (see Table2) 4. ISCLS commonly presents with shock and is managed predominantly in the critical care setting. It is critical to differentiate the type of shock to guide treatment. Traditionally this has been done with invasive monitoring, however, newer methods using ultrasound-based hemodynamic monitoring may play a role in differentiating types of shock, as well as guiding fluid resuscitation 12.
Figure 3.
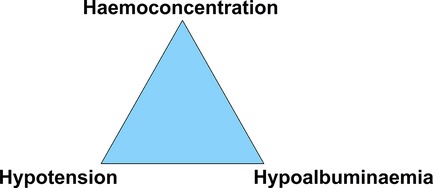
Classic triad of ISCLS.
Figure 2.
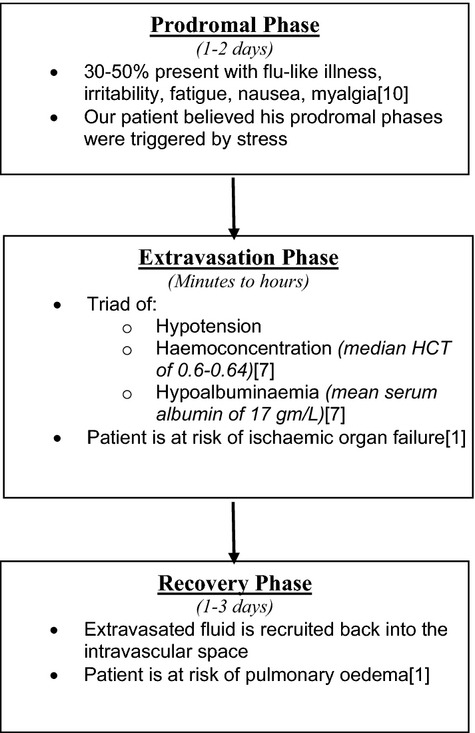
Distinct phases seen in ISCLS.
Table 2.
Mayo clinic criteria with matching case report findings
| Mayo clinic criteria 4 | Case report findings |
|---|---|
| Coexisting MGUS | Monoclonal protein detected |
| Warning signs | Myalgia, headache, fatigue, general malaise |
| Triggering factors | Stress |
| Oliguria with prodrome | Subjective oliguria |
| Pulmonary edema | Multiple episodes of florid pulmonary oedema |
| Polyuria in recruitment | Urine output of 200–500 mL/h seen in recruitment |
| Spontaneous resolution | Normalization of symptoms and signs following little to no treatment |
The pathogenesis of ISCLS still remains uncertain. Recently, Zhihui Xie et al. 6. applied sera taken from patients during an episode of ISCLS to human microvascular endothelial cells in vitro and observed vascular endothelial cadherin internalization and disruption of interendothelial junctions without inducing endothelial apoptosis 5. Their study also indicated that levels of Angiopoietin 2 (Ang-2) and VEGF were elevated during episodes. Furthermore, use of Angiopoietin 2 inhibition did seem to counteract the permeability although VEGF inhibition did not. This may support a molecular mechanism for ISCLS pathogenesis, involving humoral factors such as Ang-2 and VEGF 6.
Due to the rarity of ISCLS no gold standard treatment exists, and clinicians must instead use the limited number of case series to guide therapies. The broad therapy targets of ISCLS include endothelial signal transduction, immune modulation, and hematologic intervention 1. Terbutaline and theophylline is thought to increase cAMP and thus prevent endothelial dysfunction 1,9,10. This reduced the frequency of attacks 30-fold in the case series by Tahirkheli et al. 11. Our patient was treated with this regimen but continued to have attacks, and subsequently immunomodulation with monthly intravenous immunoglobulin injections was added. This treatment has been reported as being effective in both reducing the severity of an acute ISCLS episode as well as preventing further episodes 5, resulting in a 5-year survival rate between 73–76% 5.
During acute ISCLS episodes patients are at risk of the sequelae of shock including acute renal failure, rhabdomyolysis, compartment syndrome, and pulmonary edema 7 which may occur during both the extravasation and recruitment phases. Compartment syndrome may occur and treatment with multiple fasciotomies may be required 8. Our patient developed pulmonary edema, following aggressive fluid resuscitation. Reviews recommend initial fluid resuscitation (both colloid and crystalloid) to restore organ perfusion, followed by close monitoring and then diuretic following the extravasation period to avoid fluid overload 1,4.
Conclusion
In a shocked patient presenting with the triad of hypotension, hemoconcentration and hypoalbuminemia, the diagnosis of ISCLS should be considered. Once the diagnosis is made, the available evidence for therapy is limited. Greater awareness and a stepwise approach to diagnosis of this potentially fatal syndrome will hopefully allow earlier detection and more effective management of ISCLS.
Conflict of Interest
None declared.
References
- Druey K. Greipp P. Narrative review: the systemic capillary leak syndrome. Ann. Intern. Med. 2010;153:90–98. doi: 10.1059/0003-4819-153-2-201007200-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarkson B, Thompson D, Horwith M. Luckey H. Cyclical edema and shock due to increased capillary permeability. Am. J. Med. 1960;29:193–216. doi: 10.1016/0002-9343(60)90018-8. [DOI] [PubMed] [Google Scholar]
- Yabe H, Yabe M, Koike T, Shimizu T, Morimoto T. Kato S. Rapid improvement of life-threatening capillary leak syndrome after stem cell transplantation by bevacizumab. Blood. 2010;115:2723–2724. doi: 10.1182/blood-2009-11-247056. [DOI] [PubMed] [Google Scholar]
- Kapoor P, Greipp PT, Schaefer EW, Mandrekar S, Kamal A, Gonzalez-Paz N, et al. Idiopathic systemic capillary leak syndrome (Clarkson’s disease): the Mayo clinic experience. Mayo Clin. Proc. 2010;85:905–912. doi: 10.4065/mcp.2010.0159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gousseff M, Arnaud L, Lambert M, Hot A, Hamidou M, Duhaut P, et al. The systemic capillary leak syndrome: a case series of 28 patients from a European registry. Ann. Intern. Med. 2011;154:464–471. doi: 10.7326/0003-4819-154-7-201104050-00004. [DOI] [PubMed] [Google Scholar]
- Xie Z, Gosh C, Patel R, Iwaki S, Gaskins D, Delson C, et al. Vascular endothelial hyperpermeability induces the clinical symptoms of Clarkson disease (the systemic capillary leak syndrome) Blood. 2013;119:4321–4332. doi: 10.1182/blood-2011-08-375816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhir V, Arya V, Malav IC, Suryanarayanan B, Gupta R. Dey A. Idiopathic systemic capillary leak syndrome (SCLS): case report and systematic review of cases reported in the last 16 years. Intern. Med. 2007;46:899–904. doi: 10.2169/internalmedicine.46.6129. [DOI] [PubMed] [Google Scholar]
- Brown R, Downey C. Izaddoost S. Compartment syndrome in all four extremities: a rare case associated with systemic capillary leak syndrome. Hand. 2011;6:110–114. doi: 10.1007/s11552-010-9305-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ewan P, Lachmann P, Morice A, Forster P. Doorenbos C. Treatment of systemic capillary leak syndrome. Lancet. 1988;2:1496. [Google Scholar]
- Amoura Z, Papo T, Ninet J, Hatron P, Guillaumie J, Piette A, et al. Systemic capillary leak syndrome: report on 13 patients with special focus on course and treatment. Am. J. Med. 1997;103:514–519. doi: 10.1016/s0002-9343(97)00272-6. [DOI] [PubMed] [Google Scholar]
- Tahirkheli NK. Greipp PR. Treatment of the systemic capillary leak syndrome with terbutaline and theophylline. A case series. Ann. Intern. Med. 1999;130:905–909. doi: 10.7326/0003-4819-130-11-199906010-00015. [DOI] [PubMed] [Google Scholar]
- Horster S, et al. Cardiac output measurements in septic patients: comparing the accuracy of USCOM to PiCCO. Crit. Care Res. Pract. 2012;2012:270631. doi: 10.1155/2012/270631. [DOI] [PMC free article] [PubMed] [Google Scholar]


