Abstract
Purpose
Previous researches of betatrophin on glucose and lipids metabolism under insulin-resistant condition have reached controversial conclusions. To further identify the possible impact of betatrophin, we measured the circulating betatrophin levels in newly diagnosed type 2 diabetes (T2DM) patients, and in subjects with both impaired glucose tolerance (IGT) and normal glucose tolerance (NGT) and investigated the relationship between serum betatrophin and other clinical parameters in these patients with different glucose tolerance statuses.
Methods
A total of 460 permanent residents of the Fengxian District, aged 40–60 years, were enrolled. Based on the results of a 75 g oral glucose tolerance test, we selected newly diagnosed T2DM (n = 50) patients and subjects with IGT (n = 51) and NGT (n = 50) according to their age, gender and body mass index (18–28 kg/m2). Anthropometric parameters, glycosylated haemoglobin, blood lipids and fasting insulin were measured. Serum betatrophin concentrations were determined via ELISA.
Results
Serum betatrophin levels in T2DM patients were increased significantly compared with IGT and NGT groups, and decreased in subjects with better islet beta cell function. Serum betatrophin was positively correlated with triglyceride, 2-hour postprandial glucose, alanine aminotransferase and aspartate transaminase after adjusting for age, sex and body mass index in all subjects. Multiple regression analysis showed that 2-hour postprandial glucose was independently associated with serum betatrophin significantly.
Conclusions
Circulating betatrophin is increased in newly-diagnosed T2DM patients and positively correlated with the triglycerides and postprandial glucose levels. The results suggest that betatrophin may participate in glucose and triglycerides metabolism.
Introduction
The prevalence of diabetes mellitus, which is a major public health issue, has been increasing dramatically over the last decade. In China, the prevalences of diabetes and prediabetes were 9.7% and 15.5% respectively, corresponding to 92.4 million adults with diabetes and 148.2 million adults with prediabetes according to a 2007 survey [1], and most of them were diagnosed with type 2 diabetes mellitus (T2DM). T2DM is accompanied by a cluster of serious complications including atherosclerosis, diabetic nephropathy and diabetic retinopathy, and leads to increased morbidity and mortality, resulting in a substantial burden and intangible cost to society. T2DM is characterized by beta cell dysfunction and insulin resistance. However, the available therapies forT2DM cannot prevent the gradual loss of beta cell function [2–3], and strategies to promote islet beta cell proliferation are therefore the focus of much attention.
Betatrophin, also known as lipasin or angiopoietin-like protein8 (ANGPTL8), is a 22kD hormone that is primarily expressed in the liver and adipose tissue. Recently, in a mouse model of insulin resistance developed via the administration of S961, Yi observed an increase in islet beta cell proliferation induced by the over-expression of betatrophin [4]. However, Gusarova [5] raised doubt by revealing that over-expression of angptl8 in mice doubles plasma triglyceride levels, but does not alter beta cell expansion. In clinical study, Espes observed an increased circulating betatrophin concentration in patients with long-standing type 1 diabetes [6], and studies on T2DM demonstrated that serum betatrophin was also increased in T2DM patients [7–8]. However, Gomez-Ambrosi [9] reported that serum betatrophin concentrations were decreased in patients with obesity and T2DM and Fenzl [10] reported that serum betatrophin presented no correlation with different glucose tolerance status but correlates with lipid profiles in patients with obesity or T2DM. Thus, no consistent conclusion has been reached thus far.
To further investigate the association of circulating betatrophin concentration with glucose and lipid metabolism, we measured betatrophin concentrations in subjects of newly-diagnosed T2DM, normal glucose tolerance (NGT) and impaired glucose tolerance (IGT) and analyzed the relationship between betatrophin and related clinical parameters. Our hypothesis was that serum betatrophin levels would increase in T2DM patients as compensation for the loss of beta cell function. An increase in serum betatrophin was observed in T2DM patients and serum betatrophin levels were correlated with both postprandial glucose and lipid levels.
Materials and Methods
This study was approved by the Ethics Committee of Fengxian Central Hospital, and was carried out in accordance with the principles of the Declaration of Helsinki as revised in 2000. All subjects provided written informed consent.
Subjects
A total of 460 permanent residents of the Fengxian District of Shanghai aged 40–60 years were enrolled (160 males, 300 females). Participants previously diagnosed with diabetes; special types of diabetes; acute and chronic inflammatory disease; heart, liver and lung disease; Cushing's syndrome and other diseases and on hypoglycaemic agents were excluded. Of the 460 individuals, 63 were newly diagnosed with T2DM, 108 with IGT and 289 with NGT based on oral glucose tolerance tests (OGTT) (WHO criteria, 1999). A total of 50 T2DM, 51 IGT and 50 NGT subjects were chosen to form matched groups in terms of age, gender and body mass index (BMI, 18–28 kg/m2).
Anthropometric measurements
Weight and height were measured, and BMI (kg/m2) was calculated by dividing the weight (kilograms) by the squares of the height (meters squared). Waist circumferences were measured at the narrowest point between the lowest rib and the uppermost lateral border of the right iliac crest, the hips were measured at their widest point, and the waist-to-hip ratio (WHR) was calculated. Seated blood pressure was taken twice after the subjects rested for 10 min.
Serum biochemistry
Blood samples were collected after an overnight fast in the morning and 2 hours after 75 g of glucose was taken. After clotting, the blood specimens were separated via centrifugation. The serum samples were subsequently stored in aliquots without preservatives at -80°C prior to the analysis of betatrophin. Fasting plasma glucose (FPG), 2-hour postprandial glucose (2hPG), triglycerides (TG), total cholesterol (TC), low-density lipoprotein (LDL-c), high-density lipoprotein (HDL-c), alanine aminotransferase (ALT) and aspartate transaminase (AST) were determined using an automatic biochemical analyser (Beckman DXC800, USA). Fasting insulin levels were determined through direct chemiluminescence (ADVIA Centaur automatic immunity analyser and the associated kit, Siemens), and glycosylated haemoglobin A1c (HbA1c) was determined via high performance liquid chromatography (HLC-723 G7 automated glycosylated haemoglobin analyser, Japan). Additionally, the homeostasis model assessment of insulin resistance (HOMA-IR) = (fasting insulin×fasting glucose)/22.5 and homeostasis model assessment-β(HOMA-β) = 20×fasting insulin/(fasting glucose-3.5) were employed. Body composition was analysed using a bioelectrical impedance analyser (INBODY 10, Korea).
Betatrophin measurement
Fasting serum betatrophin was determined using an ELISA kit (Wuhan Eiaab Science, Wuhan, China). A standard curve was drawn on logarithmic graph paper, with the concentration of the standard density on the horizontal axis (logarithmic scale) and the OD value on the vertical axis (logarithmic scale). Data analysis was carried out using the professional software Curve (Curve Expert 1.3), and standard curve regression equations were calculated based on the concentration of the standard density and the OD value. The concentrations of the samples were calculated using the sample OD value in the equation with multiplication by the dilution factor. All samples were analysed in duplicate.
Statistical analysis
Statistical analysis was performed using SAS version 8.0. The data are presented as the mean ± SD or median (25th and 75th percentiles). The DBP, triglyceride, 2hPG, HOMA-IR, HOMA-β and betatrophin values were logarithmically transformed due to their non-normal distribution. Analysis of variance (ANOVA) was used to compare differences among the three groups. Student-Newman-Keuls (SNK) test was employed to compare differences between any two of the three groups. To further investigate the relationship between serum betatrophin and insulin resistance or beta cell function, we chose 75th percentiles as cut points for HOMA-IR and HOMA-β, and divided the overall participants into two groups, respectively. Student t test was employed to compare the differences of betatrophin levels between the groups.
The correlations of betatrophin with the other variables were examined via Pearson’s bivariate correlation analysis. Although age, sex and BMI were controlled among the three groups, subjects of the three groups were not individually matched. To excluding the potential influence of these factors, multivariate regression was applied to adjust for age, sex and BMI as confounders and to investigate the independent influencing factors of betatrophin. Two-sided P values<0.05 were considered significant.
Results
Anthropometric and biochemical characteristics of the individuals included in the study are shown in Table 1. Among the three groups, systolic blood pressure (SBP), triglycerides, FPG, 2hPG, HbA1c and HOMA-IR were significantly increased, whereas HOMA-β was significantly lower in the T2DM subjects (P<0.05 or P<1.0E-4). No significant differences in the waist, WHR, percentage of body fat (PBF), diastolic blood pressure (DBP), total cholesterol, HDL-c and LDL-c measurements were found among the three groups. Between NGT and IGT groups, 2hPG, HOMA-IR and HOMA-β were different significantly (P<0.05). Compared with NGT, SBP, TG, FPG, 2hPG, HbA1c and HOMA-IR significantly increased (P<0.05), and HOMA-β was significantly lower (P<0.05) in T2DM group. Compared with IGT, TG, FPG and HbA1c significantly increased (P<0.05) in T2DM group.
Table 1. Demographic and biochemical characteristics of the study population.
| Variable | NGT(n = 50) | IGT(n = 51) | T2DM(n = 50) | p value |
|---|---|---|---|---|
| Age(years) | 52.44±5.87 | 52.54±5.88 | 52.24±5.89 | 0.967 |
| BMI(kg/m2) | 24.48±2.00 | 24.39±1.91 | 24.70±2.14 | 0.733 |
| Waist circumference(cm) | 82.50±8.21 | 83.98±6.17 | 85.04±7.33 | 0.226 |
| WHR | 0.91±0.07 | 0.91±0.07 | 0.93±0.08 | 0.240 |
| PBF(%) | 32.28±5.74 | 32.73±4.34 | 32.54±5.06 | 0.908 |
| DBP(mmHg) | 80.00(70.00,86.00) | 80.00(74.50,90.00) | 80.00(76.00,90.00) | 0.455 |
| SBP(mmHg) | 123.16±16.06† | 127.79±15.61 | 131.78±16.44† | 0.032 |
| AST(IU/L) | 24.66±1.465 | 21.80±0.941 | 26.30±1.851 | 0.834 |
| ALT(IU/L) | 27.72±2.576 | 25.82±1.606 | 40.72±6.375 | 0.523 |
| TC(mmol/L) | 5.23±1.11 | 5.16±1.03 | 5.47±1.13 | 0.337 |
| TG(mmol/L) | 1.16(0.77,1.70)† | 1.31(1.01,1.96)‡ | 1.67(1.09,2.55)† ‡ | 0.002 |
| HDL-c(mmol/L) | 1.31±0.25 | 1.28±0.25 | 1.32±0.24 | 0.791 |
| LDL-c(mmol/L) | 3.06±0.82 | 2.95±0.72 | 3.16±0.85 | 0.423 |
| FPG(mmol/L) | 5.24±0.44† | 5.76±0.59‡ | 7.93±2.71† ‡ | <1.0E-4 |
| 2h-PG(mmol/L) | 6.30(5.60,7.00)* † | 8.50(8.10,10.10)* ‡ | 14.70(12.50,17.80)† ‡ | <1.0E-4 |
| HbA1c(%) | 5.48±0.34† | 5.85±0.44‡ | 7.11±1.89† ‡ | <1.0E-4 |
| HOMA-IR | 1.58(1.19,2.55)† * | 2.48(1.89,3.39)* | 2.97(2.46,3.94)† | <1.0E-4 |
| HOMA-β | 85.10(61.10,131.57)† * | 88.60(63.23,127.65) * | 45.54(31.71,92.97)† | <1.0E-4 |
Data are shown as n or median (interquartile range). Statistical analyses were performed by SAS (version 8.0).p values from ANOVA, p values <0.05 are shown in bold.
*significantly different between IGT and NGT at P<0.05 from SNK.
†significantly different between T2DM and NGT at P<0.05 from SNK.
‡significantly different between T2DM and IGT at P<0.05 from SNK.
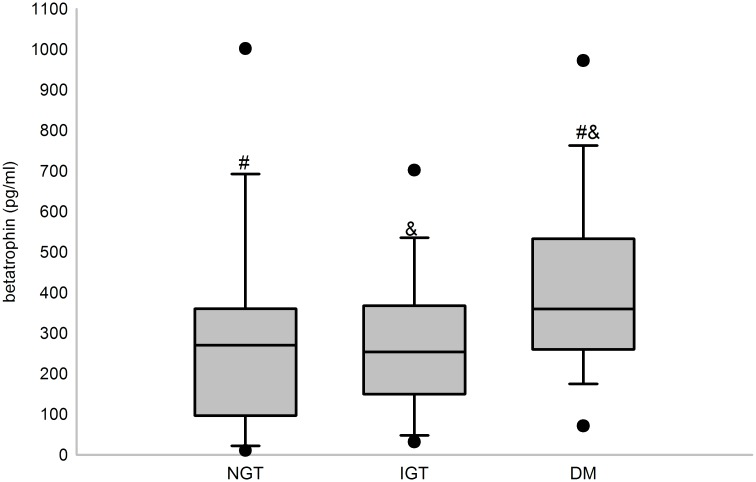
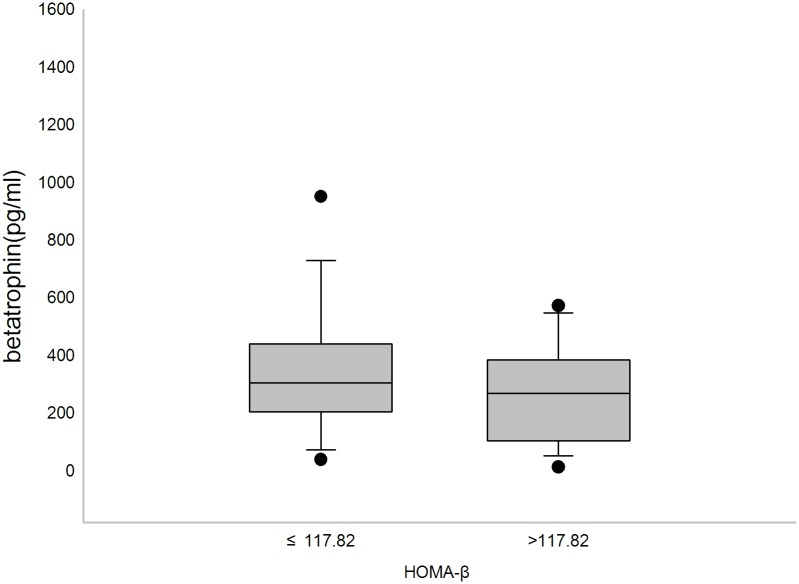
Serum betatrophin concentrations were significantly different among NGT, IGT and T2DM subjects (P = 0.003), with higher concentrations observed in the T2DM group than the NGT or IGT group (Fig 1) (P<0.05). However, no difference was detected between the NGT and IGT groups. In addition, serum betatrophin levels were significantly lower in subjects with comparatively better islet beta cell function (Fig 2) (P<0.05). However, no difference of betatrophin levels was found between subjects with different insulin resistant levels.
Fig 1. Serum betatrophin levels of subjects with different glucose tolerance statuses.
Box plot for serum betatrophin levels in NGT (n = 50), IGT (n = 51) and T2DM (n = 50) subjects. Serum betatrophin levels were significantly different in the three groups (P<0.01). #significantly different between T2DM and NGT at P<0.05 from SNK; &significantly different between T2DM and IGT at P<0.05 from SNK.
Fig 2. Serum betatrophin levels of subjects with different levels of beta cell function.
Box plot for serum betatrophin levels in subjects with HOMA-β below or equal to 117.82 (Q3) and subjects with HOMA-β above 117.82. Serum betatrophin levels were significantly different between the two groups (P<0.05).
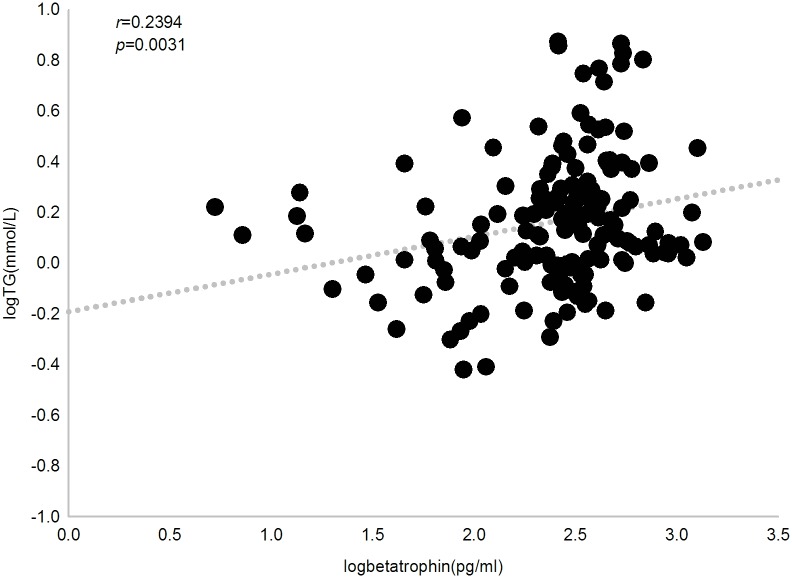
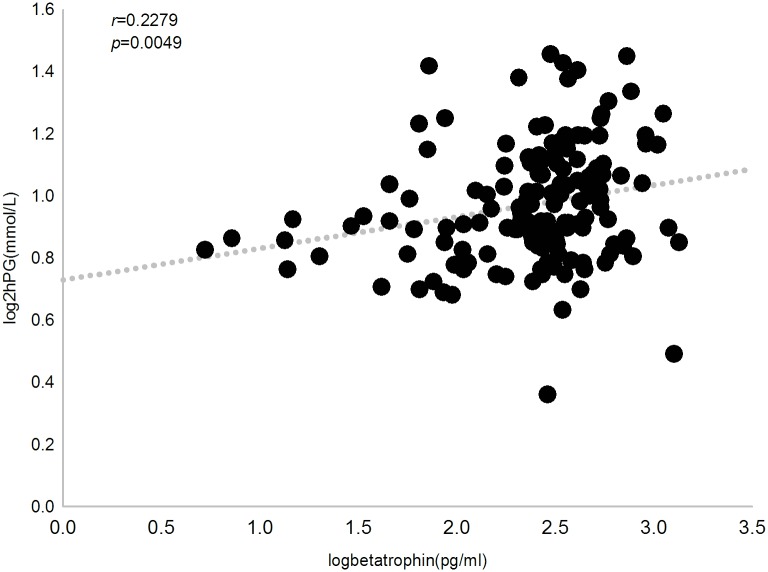
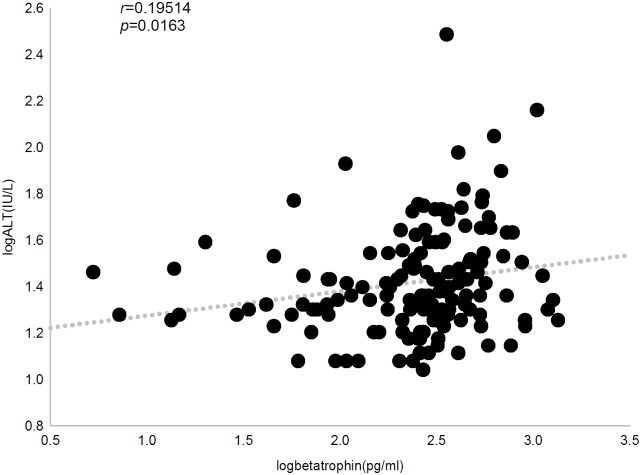
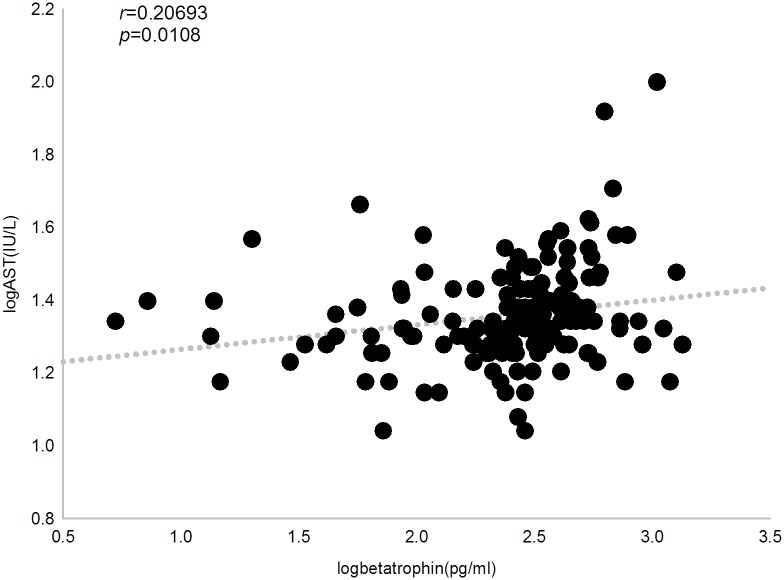
We then investigated the relationship between circulating betatrophin levels and clinical parameters by Pearson’s bivariate correlation analysis. In all subjects, betatrophin concentration was positively correlated with triglyceride, 2hPG, ALT, AST and ALP (r = 0.239, 0.228, 0.195, 0.207 and 0.183, respectively, P<0.05). When multivariate regression was applied and adjusted for age, sex and BMI as confounders, we observed that serum betatrophin levels were independently and significantly associated with triglyceride (P = 0.012), 2hPG (P = 0.004), ALT (P = 0.0388) and AST (P = 0.0306) (Figs 3, 4, 5 and 6).
Fig 3. Correlation between plasma betatrophin concentration and triglyceride level.
Betatrophin level positively correlates with triglyceride level in all subjects (r = 0.239, P = 0.0031).
Fig 4. Correlation between plasma betatrophin concentration and 2-hour plasma glucose level.
Betatrophin level positively correlates with 2-hour plasma glucose level in all subjects (r = 0.228, P = 0.0049).
Fig 5. Correlation between plasma betatrophin concentration and alanine aminotransferase level.
Betatrophin level positively correlates with alanine aminotransferase level in all subjects (r = 0.195, P = 0.016).
Fig 6. Correlation between plasma betatrophin concentration and aspartate transaminase level.
Betatrophinlevel positively correlates with aspartate transaminaselevel in all subjects (r = 0.207, P = 0.011).
Finally, we used multiple regression analysis to investigate the independent factors associated with betatrophin. The results showed that 2hPG (β = 0.386±0.189, P = 0.0425) was the only independent factor that was significantly associated with serum betatrophin.
Discussion
We analysed the serum levels of betatrophin in middle-aged, newly diagnosed T2DM patients and compared them with age-, gender- and BMI-matched IGT and NGT subjects. The results showed that serum betatrophin concentrations were increased in newly diagnosed T2DM patients, but no difference was observed between the NGT and IGT groups. In addition, serum betatrophin levels were decreased in subjects with better islet beta function. Circulating betatrophin was positively correlated with triglycerides, 2hPG, FPG and HbA1c. Betatrophin was independently and significantly associated with triglyceride and 2hPG after adjusting for age, sex and BMI. These results indicate that betatrophin may participate in triglyceride and glucose metabolism. We also observed that betatrophin positively correlated with particular liver enzymes-ALT and AST specifically.
Our results demonstrated a significant increase in serum betatrophin levels of newly diagnosed T2DM patients compared with the controls, which accorded with several previous studies [7–8, 11–12]. However, Gomez-Ambrosi and Fenzl recently reported that serum betatrophin showed no increase in T2DM patients [9–10]. This disparity may be due to sample size, hypoglycaemic agents and disease duration and disparity of BMI. In the study by Fenzl, all of the patients with T2DM received metformin and/or sulfonylurea and the mean disease duration was 8.3±1.0 years. In the study of Fu, the BMI of the subjects varied from 23.6±1.2 to 39.0±3.6. Whether these factors affect serum betatrophin levels is still not clear.
Our results also showed that 2hPG was the independent factor influencing betatrophin which indicates a probable impact of betatrophin in the pathogenesis of T2DM, but the mechanism remains exclusive. Yi reported that under the condition of insulin resistance induced by S961 (an insulin receptor antagonist), hepatic betatrophin mRNA expression was upregulated and correlated with high pancreatic beta cell proliferation rates. Betatrophin encoded a secreted protein which was proved to be responsible for the proliferation of pancreatic beta cell in animal models [4]. Nevertheless, the potential receptors and molecular mechanism of betatrophin still remain uncovered. This increase might be an indication of the ability to adapt to insulin resistance and a compensation for beta cell loss. In addition, the increase of serum betatrophin in subjects with poorer beta cell function could be seen as a compensation of beta cell loss.
However, controversy emerges regarding the role of betatrophin in glucose metabolism. Jiao showed that elevated hepatic betatrophin expression promoted the replication of mouse beta cells but not human beta cells transplanted into mice [13]. Gusarova reported that angptl8 knockout mice underwent entirely normal beta cell expansion in response to insulin resistance, and over-expression of ANGPTL8 either did not alter or only modestly increased beta cell replication, indicating that there may be unknown factors responsible for the variation of beta cell replication in over-expression of betatrophin [5]. Yi and colleagues responded to the findings of Gusarova and reported that they also found great variation in beta cell replication following the over-expression of betatrophin in mice [14]. Recent study of the relationship between betatrophin and irisin indicates that there might be other factors participating in this process [15] and study on the molecular mechanism of beta cell proliferation suggests that there might be a pathway involving both irisin and betatrophin in insulin resistance [16]. Therefore, studies on betatrophin are still in the nascent stages.
In the present study, serum betatrophin levels showed a positive correlation with triglycerides, illustrating that betatrophin might plays a role in regulating lipid metabolism. In fact, previous studies have shown that betatrophin regulates lipid metabolism. Ren found that the RIFL (refeeding induced in fat and liver) gene (a betatrophin gene) was important in fat metabolism and was specifically expressed in white adipose tissue and the liver following refeeding in fasting mice [17]. ANGPTLs play major roles in lipids metabolism, and ANGPTL8 regulates postprandial triglycerides and fatty acid metabolism in mice [18]. Angptl8 (-/-) knockout mice gained weight slowly, and their plasma triglycerides decreased after refeeding [19]. The proposed mechanism of these phenomena is that betatrophin inhibits lipoprotein lipase (LPL), thereby inhibiting triglycerides being taken up by peripheral tissues and reducing serum triglyceride clearance [20–21]. As a result, over-expression of betatrophin leads to hypertriglyceridemia. Thus, betatrophin is a nutritionally regulated factor that plays a role in lipid metabolism.
We also observed a positive correlation between betatrophin and liver enzymes, ALT and AST in particular, which coordinate with the results of Chen [12]. However, the reason for that is merely known. As discussed previously, serum betatrophin level positively correlated with serum triglycerides, and it is widely acknowledged that hypertriglyceridemia is closely related to non- alcohol fatty liver disease which can cause an increase in liver enzymes. Therefore, betatrophin may have an impact on the pathogenesis of non- alcohol fatty liver by increasing serum triglyceride level.
A main limitation of the present study is the limited sample size, which reduces the statistical power. Second, postprandial levels of betatrophin could not be analysed because only fasting betatrophin was measured. Third, serum betatrophin levels were determined only via ELISA, without verification by western blotting.
We conclude that circulating betatrophin levels are increased in newly diagnosed T2DM patients and decreased in patients with comparatively better islet beta cell function. Serum betatrophin levels show a positive correlation with triglycerides and 2hPG, indicating that betatrophin is associated with both glucose and lipid metabolism. However, we cannot reach conclusions on the role of betatrophin in glucose and lipid metabolism process based on the present results and further studies will still be needed.
Acknowledgments
We thank the participants in the research. We thank the nursing and medical staff at Fengxian Central Hospital for their dedication to this study.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was funded by grants from the Shanghai Committee of Science and Technology (134119b2500), China.
References
- 1. Yang W, Lu J, Weng J, Jia W, Ji L, Xiao J, et al. Prevalence of diabetes among men and women in China. N Engl J Med. 2010; 362:1090–1101. 10.1056/NEJMoa0908292 [DOI] [PubMed] [Google Scholar]
- 2. Stolar MW, Hoogwerf BJ, Gorshow SM, Boyle PJ, Wales DO. Managing type 2 diabetes: going beyond glycemic control. J Manag Care Pharm. 2008; 14: 2–19. [PubMed] [Google Scholar]
- 3. Bagust A, Beale S. Deteriorating beta-cell function in type 2 diabetes: a long-term model. QJM. 2003; 96:281–288. [DOI] [PubMed] [Google Scholar]
- 4. Yi P, Park JS, Melton DA. Betatrophin: a hormone that controls pancreatic β cell proliferation. Cell. 2013; 153:747–758. 10.1016/j.cell.2013.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 5. Gusarova Viktoria, Alexa Corey A., Na Erqian, Stevis Panayiotis E., Xin Yurong, Susan Bonner-Weir, et al. ANGPTL8/Betatrophin Does Not Control Pancreatic Beta Cell Expansion. Cell. 2014; 159: 691–696. 10.1016/j.cell.2014.09.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Espes D, Lau J, Carlsson PO. Increased circulating levels of betatrophin in individuals with long-standing type 1 diabetes. Diabetologia. 2014; 57: 50–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fu Z, Berhane F, Fite A, Seyoum B, Abou-Samra AB, Zhang R. Elevated circulating lipasin/ betatrophin in human type 2 diabetes and obesity. Sci Rep. 2014; 4: 5013 10.1038/srep05013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Espes D, Martinell M, Carlsson PO. Increased circulating betatrophin concentrations in patients with type 2 diabetes. Int J Endocrinol.2014; 10.1155/2014/323407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gómez-Ambrosi J, Pascual E, Catalán V, Rodríguez A, Ramírez B, et al. Circulating betatrophin concentrations are decreased in human obesity and type 2 diabetes. J Clin Endocrinol Metab. 2014; 99: E2004–E2009. 10.1210/jc.2014-1568 [DOI] [PubMed] [Google Scholar]
- 10. Fenzl A, Itariu BK, Kosi L, Fritzer-Szekeres M, Kautzky-Willer A, Stulnig TM, et al. Circulating betatrophin correlates with atherogenic lipid profiles but not with glucose and insulin levels in insulin-resistant individuals. Diabetologia. 2014; 57: 1204–1208. 10.1007/s00125-014-3208-x [DOI] [PubMed] [Google Scholar]
- 11. Hu H, Sun W, Yu S, Hong X, Qian W, Tang B, et al. Increased circulating levels of betatrophin in newly diagnosed type 2 diabetic patients. Diabetes Care. 2014; 37: 2718–2722. 10.2337/dc14-0602 [DOI] [PubMed] [Google Scholar]
- 12. Guo K 1, Lu J, Yu H, Zhao F, Pan P, Zhang L, et al. Serum betatrophin concentrations are significantly increased in overweight but not in obese or type 2 diabetic individuals. Obesity. 2015; 23: 793–797. 10.1002/oby.21038 [DOI] [PubMed] [Google Scholar]
- 13. Jiao Y, Le Lay J, Yu M, Naji A, Kaestner KH. Elevated mouse hepatic betatrophin expression does not increase human beta-cell replication in the transplant setting. Diabetes. 2014; 63: 1283–1288. 10.2337/db13-1435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yi P, Park JS, Melton DA. Perspectives on the activities ofANGPTL8/betatrophin. Cell. 2014; 159: 467–468. 10.1016/j.cell.2014.09.028 [DOI] [PubMed] [Google Scholar]
- 15. Xie Xinmiao, Gao Ting, Yang Meili, Chen Peihong, Jin Hua, Yang Lili, et al. Associations of betatrophin levels with irisin in Chinese women with normal glucose tolerance. Diabetology & Metabolic Syndrome. 2015; 7:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sanchis-Gomar F, Perez-Quilis C. The p38-PGC-1alpha-irisin-betatrophin axis: exploring new pathways in insulin resistance. Adipocytes. 2014; 3: 67–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ren G 1, Kim JY, Smas CM. Identification of RIFL, a novel adipocyte-enriched insulin target gene with a role in lipid metabolism. Am J Physiol Endocrinol Metab. 2012; 303: E334–E351. 10.1152/ajpendo.00084.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Quagliarini F, Wang Y, Kozlitina J, Grishin NV, Hyde R, Boerwinkle E, et al. Atypical angiopoietin-likeprotein that regulates ANGPTL3. Proc Natl Acad Sci USA. 2012; 109:19751–19756. 10.1073/pnas.1217552109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wang Y, Quagliarini F, Gusarova V, Gromada J, Valenzuela DM, Cohen JC, et al. Mice lacking ANGPTL8 (Betatrophin) manifest disrupted triglyceride metabolism without impaired glucose homeostasis. Proc Natl Acad Sci USA. 2013; 110: 16109–14. 10.1073/pnas.1315292110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Zhang R. Lipasin, a novel nutritionally-regulated liver-enriched factor that regulates serum triglyceride levels. Biochem Biophys Res Commun. 2012; 424:786–792. 10.1016/j.bbrc.2012.07.038 [DOI] [PubMed] [Google Scholar]
- 21. Zhang R, Abou-Samra AB. Emerging roles of Lipasin as a critical lipid regulator. Biochem Biophys Res Commun. 2013; 432:401–405. 10.1016/j.bbrc.2013.01.129 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.