Abstract
Objective
To examine usage patterns of hearing aids and cochlear implants in children up to three years of age, how usage changes longitudinally, and factors associated with device usage.
Design
Parent report and Parent’s Evaluation of Aural/oral performance of Children (PEACH) data were obtained at six and twelve months after hearing-aid fitting or cochlear implant switch-on, and again at three years of age. The effect of device use on auditory functional performance was investigated using the PEACH questionnaire.
Study sample
Four hundred and thirteen participants from the Longitudinal Outcomes of Children with Hearing Impairment (LOCHI) study were included for analysis.
Result
For users of hearing aids, higher usage at three years was associated with higher maternal education, and more severe hearing loss. For users of cochlear implants, higher usage was associated with higher maternal education and the absence of additional disabilities. Higher PEACH scores was associated with higher usage scores. After allowing for the effects of demographic characteristics, device use was not a significant predictor of functional performance.
Conclusions
Sixty-two percent of children achieved consistent use (>75% of waking hours) within the first year of receiving a hearing aid or a cochlear implant, and 71% by three years of age.
Keywords: Device use, hearing aids, cochlear implants, children, functional performance, PEACH, predictors of usage
Across Australia, infants have access to universal newborn hearing screening (UNHS) programs that provide early identification of hearing loss. Earlier detection allows intervention such as hearing aid (HA) fitting or cochlear implantation to occur earlier, providing the child with auditory access to the acoustic environment. Consistent usage of hearing devices is crucial for children to benefit from this early intervention (Moeller et al. 2009).
Current audiological protocols for the management of children in Australia primarily aim to facilitate optimal fitting and regular use of hearing devices by adopting a collaborative management process between families, the audiologist and other service providers relevant to the individual child (King 2010). An example within this process is the regular monitoring of a child’s use of hearing instruments by systematically soliciting information from parents or early education teachers through administering the Parent’s Evaluation of aural/oral Performance of Children (PEACH) and Teacher Evaluation of Auditory/oral performance of Children (TEACH) (Ching & Hill 2007; Ching et al. 2008). These tools also provide insight into the everyday auditory functioning of children, and identify situations that may impact negatively on the regular use of a child’s hearing devices.
Previous reports on usage of devices have mostly involved either small study samples or samples that spanned a wide age range. As such, little is known about usage of devices by infants who received early intervention after newborn hearing screening; and even less about how the usage routine changes over the first few years of life, for children fitted with hearing aids and children who received cochlear implants. Archbold et al (2009) assessed 138 children’s use of cochlear implants by using a questionnaire. With an average implantation age of 4.7 years (range 1.7–11.5 years), 83% achieved full-time usage by seven years after implantation. They found that earlier age of implantation, use of an oral mode of communication and mainstream educational placement were significant factors that were linked to consistent usage of device. They also noted that there were fluctuating patterns of use over time.
Two studies examined hearing aid usage in young children. Moeller et al (2009) conducted a structured interview with mothers of seven infants with mild to moderately severe hearing loss, and found that by 28.5 months of age, only two families established consistent full-time use across different everyday situations. Hearing aid use was inconsistent early in life but became more consistent with age. Qualitative analysis of the interviews revealed challenges relating to the child’s developmental changes, parental safety concerns, and particular situational challenges such as riding in a car. The authors recognised that it is difficult to generalise conclusions from their study due to the small number of subjects.
In a more recent study, Walker et al (2013) investigated predictors of hearing aid use time for 272 children ranging in age between 5 months and 7 years 3 months who were recruited from audiological clinics at three different sites. The children had hearing loss between 25 and 75 dB HL (better ear average hearing loss between 0.25 and 4 kHz). Children with additional disabilities were excluded, so were children from non-English speaking families and children who used manual communication as their primary mode of communication. The mean age of fitting for 211 participants whose hearing loss was identified via newborn hearing screening was 11 months, and the mean age of fitting for those identified after birth was 30 months. Parents completed a questionnaire and participated in an interview regarding hearing aid compliance when the participant was on average 3 years 4 months of age (range 5 months to 7 years 3 months). The authors found that longer hearing aid use time was associated with older age, poorer hearing, and higher maternal education. They also found that hearing aid use was different across the 3 recruitment sites, with children from one region displaying significantly less hearing aid use time than those from another region. This suggests that variations in service provision across sites or other unknown demographic characteristics of children across regions may have affected the findings reported. Data-logging information was also reported for 133 participants. Significant correlations were found between data-logging and caregiver report on device usage, with the latter found to have over-estimated daily hearing aid usage compared to logged data.
Reported challenges to consistent hearing aid use in young children include age, child temperament and practical challenges in specific listening environments such as travelling in a car (Moeller et al. 2009; Walker et al. 2013). The degree of hearing loss has been shown consistently to affect hearing aid use in older children, with moderate to severe hearing losses associated with increased acceptance compared to those with milder loss (Walker et al. 2013; Kiese-Himmel et al. 2000; Marttila & Karikoski 2006; Vesterager & Parving 1995) Other factors that have been investigated in different studies to have positively influenced the daily use of hearing aids or cochlear implants include female gender (Marttila & Karikoski 2006), younger age of initial hearing aid fitting (Marttila & Karikoski 2006), younger age of cochlear implantation (Archbold et al. 2009), lower levels of self-reported cochlear implant discomfort (Watson & Gregory 2005), oral communication mode (Archbold et al. 2009), higher maternal level of education and centre of hearing aid fitting (Walker et al. 2013). None of the previous studies investigated the extent to which these factors influence device usage in the same cohort.
Although previous studies are valuable in providing insights into usage of hearing aids, the wide age range reported in the studies does not permit a systematic investigation of what factors influence use of hearing device over the critical first few years of life. To date, there is little research into the consistency of hearing device usage in a prospective manner, and including hearing aids and cochlear implants within the same study. In reality children may well transition from a hearing aid to a cochlear implant, or be using cochlear implants with hearing aids. Especially with broadened cochlear implant candidacy criteria, bimodal fitting (unilateral cochlear implant combined with a hearing aid in the contralateral ear) is standard where there is residual hearing in the non-implanted ear that is usable with acoustic amplification (Ching et al. 2006; Tange et al. 2009). With UNHS, a major component of early intervention is to ensure that devices that are fitted are being used consistently to provide auditory stimulation and to support development. To capitalise on the potential benefit of early intervention, it is important to increase knowledge about usage patterns, and the factors that affect usage in young children, at a population level.
We took advantage of the Longitudinal Outcomes of Children with Hearing Impairment (LOCHI) study to collect information about device usage over the first few years of life and to examine factors influencing usage. The LOCHI study is a prospective population based study of outcomes of children with hearing loss across three states in Australia (Ching et al. 2013). All children with hearing loss in Australia receive uniform post-diagnostic hearing services from a single -funded national service provider, Australian Hearing (AH), up to 26 years of age, at no cost to families. After enrolment in the LOCHI study, children were assessed at six and twelve months after initial hearing aid fitting, and at the chronological age of three years. If a child received a cochlear implant before three years of age, they were also assessed at six and twelve months after activation of their cochlear implant. Data about usage of hearing devices were collected at the time of each assessment interval.
The aim of this paper was to examine the following questions related to hearing device use in young children:
Does hearing device use of young children differ between those who use hearing aids and those who use cochlear implants?
What audiological, child and environmental factors affect hearing device usage patterns at three years of age?
What factors affect changes in the routine of device usage over the first three years of life?
Is device usage related to the overall auditory functional performance of children at three years of age?
Method
Participants
The study sample consisted of 413 children who have available data regarding daily device use at three years of age. Table 1 shows the characteristics of the study sample at the time of their third birthday. All subjects were fitted with hearing aids before three years of age; with fifty-five percent of children receiving amplification prior to six months of age and the remaining forty-five percent receiving amplification between six and thirty-four months of age. Subjects received a range of early educational services including auditory-verbal, aural-oral, total communication and bilingual programs.
Table 1.
Demographic characteristics of participants at age 36 months
| Characteristics | Sample (n=413) |
HA Subgroup (n=297) |
CI Subgroup (n=116) |
|
|---|---|---|---|---|
| Hearing Device Used | Hearing Aid | 297 (71%) | - | - |
| Cochlear Implant | 116 (28%) | - | - | |
| Gender (Male) | No. (%) | 223 (54%) | 167 (56.2%) | 56 (48.3%) |
| Additional Disabilities (Nil) | No. (%) | 263 (63.7%) | 194 (65.3%) | 69 (59.5%) |
| Communication Mode at Home | Speech Only | 296 (71.7%) | 224 (75.4%) | 72 (62.1%) |
| Other | 100 (24.2%) | 64 (21.5%) | 36 (31.0%) | |
| Unknown | 17 (4.1%) | 9 (3%) | 8 (6.9%) | |
| Maternal Education | Less than University | 233 (56.4%) | 172 (57.9%) | 61 (52.6%) |
| University | 157 (38.0%) | 112 (37.7%) | 45 (38.8%) | |
| Unknown | 23 (5.6%) | 13 (4.4%) | 10 (8.6) | |
| FM Use (Nil) | No. (%) | 315 (76%) | 237 (79.8%) | 78 (67.2%) |
| Age at First Fitting (Months) | Mean (SD) | 9.1 (9.2) | 10.4 (9.8) | 6.0 (6.2) |
| Age at First Switch-on (Months) | Mean (SD) | 17.24 (8) | - | 17.24 (8) |
| Hearing Loss Better Ear 4FA | No. (%) | |||
| Mild (≤40dBHL) | 76 (18.4%) | 76 (25.6%) | 0 (0%) | |
| Moderate (40–-60dBHL) | 140 (33.9%) | 138 (46.5%) | 2 (1.7%) | |
| Severe (60–80dBHL) | 73 (17.7%) | 59 (19.9%) | 14 (12.7%) | |
| Profound (≥80dBHL) | 124 (30.0%) | 24 (8.1%) | 100 (86.21%) | |
| Socio-Economic Status (IRSAD) | Mean (SD) | 7 (2.5) | 7.1 (2.5) | 6.8 (2.6) |
| Early Intervention Hours | Mean (SD) | 141.3 (115.5) | 116.5 (107.9) | 202 (111.1) |
Demographic information
A custom designed questionnaire was completed by the child’s primary caregiver at each assessment interval (6 & 12 months post hearing aid or cochlear implant fitting and 3 years of age) to obtain demographic data.
Information extracted included gender and the diagnosis of any disabilities the child may have in addition to their hearing loss. The range of disabilities included developmental delay, cerebral palsy, autism spectrum disorder, and disorders of vision, speech output, various syndromes and other medical conditions. The child’s communication mode at home was specified in three categories: Speech Only, Sign Only and Other. In addition, maternal education was specified using three ordinal categories of the highest level completed - Twelve years or less of formal education, Diploma or Certificate, and University Qualification. Socio-economic status was categorised using the Index of Relative Socioeconomic Advantage and Disadvantage (IRSAD), one of the four indexes that make up the Socio Economic Index For areas or SEIFA (Australian Bureau of Statistics 2008). IRSAD scores were determined based on the subject’s residential postcode, with a lower score associated with greater relative disadvantage and higher scores associated with greater relative advantage. IRSAD scores were standardised with a mean of 1000 and approximately two thirds of scores for the national population falling between 900 and 1100 (Australian Bureau of Statistics 2008, p.25). A score falling within the seventh decile, like the mean IRSAD rating for the study sample in Table 1, approximately reflects a score between 1050 and 1085.
The type of hearing devices used by individuals were extracted and cross referenced with available audiological records held at the AH service database. Ear specific data were obtained on the type of device worn, the average number of days per week the device was worn, and the average number of hours it was worn at one time. The number of hours of device use was specified by five categories: never worn, less than one hour a day, one to four hours a day, four to eight hours a day, and more than eight hours a day.
Assessment of usage, Discomfort and Functional Performance
At each assessment interval, caregivers completed the Parents’ Evaluation of Aural/oral Performance of Children (PEACH) to assess the child’s functional everyday performance in a range of commonly encountered situations. Caregivers’ were given a PEACH diary and were asked to complete it, based on their observations of their child in everyday situations over a period of a week. The diary contained a question on device usage and a question on listening comfort. There were a further 11 items describing a range of quiet and noisy situations, and parents were asked to rate and describe their child’s auditory behaviour in the situations, and the child’s awareness of environmental sounds. An overall score of functional performance based on the 11 items was calculated, and corrected for age using normative data (Ching & Hill 2007).
Information on average device usage was extracted from question one of the PEACH which asks “How often has your child worn his/her hearing aids and/or cochlear implant?” Responses were coded on a five point scale with response values of “never” (0%), “seldom” (1- 25%), “sometimes” (26- 50%), “often” (51- 75%), and “always” (75- 100%). To provide an overall indication of daily device use, information from the demographic questionnaires and question one of the PEACH were aggregated. First, the ear-specific daily hours of device use in the demographic questionnaires were combined, with the higher category of hours taken when there was a difference. Each category of hours was then coded in alignment with the coding system used for the PEACH data on device use, as specified in Table 2. The overall level of device use was determined by combining the aligned demographic categories with the PEACH data. A total of 269 subjects (65.1% of total) had usage data from both the demographic questionnaire and PEACH at three years of age, of whom 182 (44.1%) subjects had the same rating from both sources, 35 (8.5%) had a higher rating on the PEACH compared to the demographic questionnaire, and 52 (12.6%) had a higher usage rating on the demographic form. When there was a difference in the usage rating between sources, the higher usage category was taken. Of the remaining subjects, 39 had usage data only from PEACH (9.4%), and 105 had usage data only from the demographic questionnaire (25.4%). For these subjects, the rating from either source was used in analyses.
Table 2.
Alignment of hearing device usage between demographic information and PEACH data.
| Code | Hearing device use: Demographic information |
Hearing device use: PEACH data |
|---|---|---|
| 0 | Never wears | Never (0%) |
| 1 | <1 hour a day | Seldom (1 – 25%) |
| 2 | 1 – 4 hours a day | Sometimes (26 – 50%) |
| 3 | 4 – 8 hours a day | Often (51 – 75%) |
| 4 | > 8 hours a day | Always (76 – 100%) |
Information on the level of discomfort experienced by the participant from their hearing devices was also independently extracted from question two of the PEACH.
Audiological information
Information regarding the age of hearing aid fitting, age of cochlear implant switch-on, type of hearing device used in each ear, degree of hearing loss and use of a frequency modulated (FM) system was extracted from each child’s record held at the AH database with caregiver consent.
Analysis
Three participants (n=3) were excluded from analyses as they were no longer aided at the time of their third birthday. Only three participants reported using sign only at home, and were aggregated into the “Other” category to result in a binary variable for home communication mode (Oral vs Other). Maternal education information was also collapsed into a binary variable for analysis (Less than University vs University).
All available data were entered and analysed using R 2.14.2 and R Studio statistical software packages (RStudio 2012)(Team 2012). For 48 children, information regarding communication mode at home, or maternal education, or socio-economic status was missing at 3 years of age. In such instances, information regarding the same fields collected at an earlier interval were used. The number of children with information available at previous intervals was 327, (6 & 12 months post initial HA fitting or CI switch-on) due to factors such as intervals overlapping with the child’s third birthday or the child not available for testing.
To examine whether hearing device use patterns differ between children who use hearing aids and those using cochlear implants at three years of age, cross-sectional analysis was completed for device use data at three years of age using Wilcoxon sum rank tests and ordered probit regression models. Due to the small numbers in the bottom three usage categories, overall device usage ratings were collapsed into three categories: Always, Often and <50%. To determine factors influencing hearing device usage at three years of age, bivariate analyses were performed separately for those using hearing aids at three years of age, and then again for those using cochlear implants (including 13 unilateral implant users, 51 bilateral implant users and 52 bimodal implant users) at three years of age, as it was theorised that different factors may be more important within these groups.
A multivariate ordered probit regression model with interactions was used to examine which factors affected device use for the total sample. The multivariate model was repeated separately with the hearing aid subgroup, and again with the cochlear implant subgroup. In the latter, age of initial hearing aid fitting was replaced by age of initial cochlear implant switch-on. As only two subjects had a unilateral hearing loss, statistical testing examining this factor was not carried out.
Longitudinal changes in hearing device use were examined using Wilcoxon sum rank tests and ordered probit regression models. To assess which factors were associated with changes in device usage over time, bivariate analyses of a range of child, family and intervention factors were completed. A multivariate ordered probit regression model was built to see which variables were associated with change in device usage over three years. For subjects who transitioned from hearing aids to a cochlear implant during the study period, information obtained on hearing aid usage was excluded from analysis. Tests of interactions were completed and accounted for in the model.
Finally, to determine if there was an association between device use and the overall functional performance as measured by the overall PEACH score, a linear regression analysis was carried out with usage ratings and the same child, family and intervention factors examined in previous regression models as predictor variables and the overall PEACH score as a dependent variable.
In line with standard practice, significance levels for analysis were set at an alpha level of p= 0.05.
Results
Device use at three years
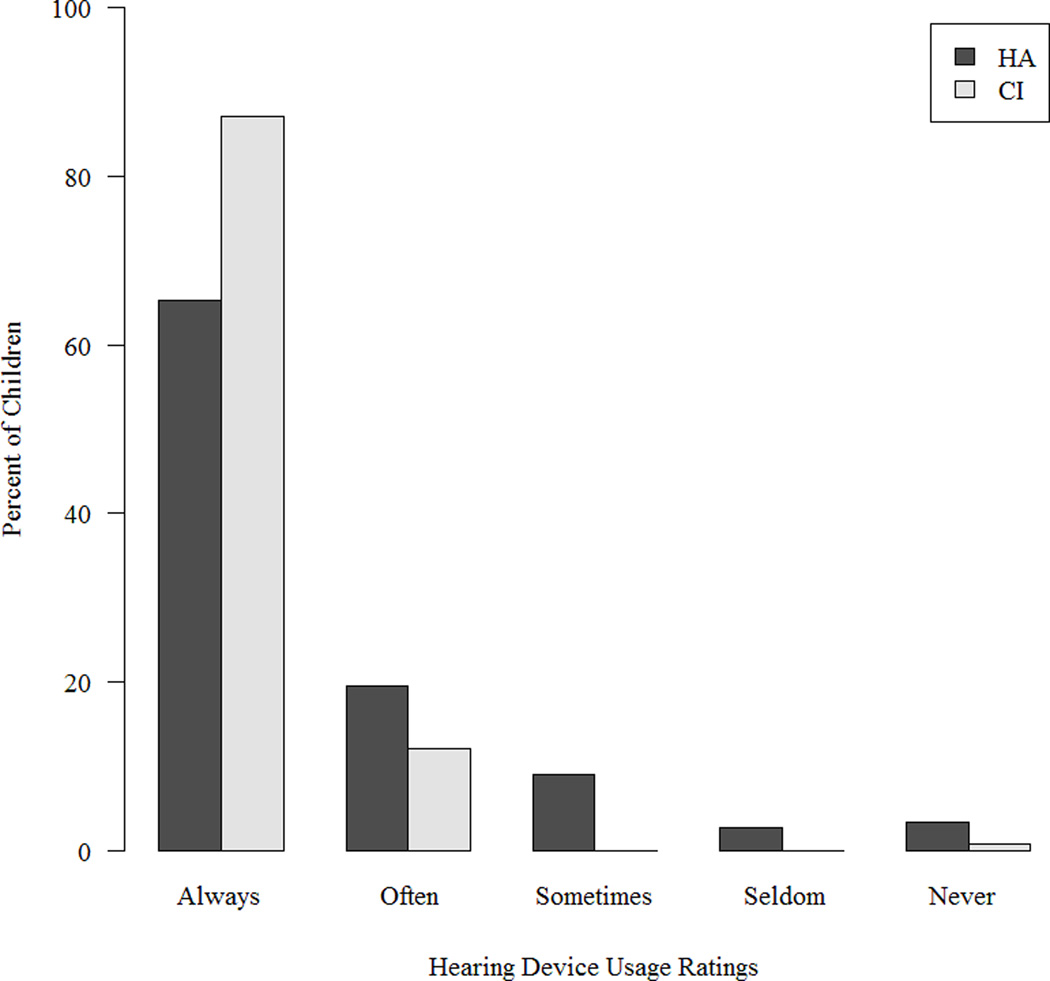
Figure 1 shows the distribution of device usage at 3 years of age, separately for children who used hearing aids and those who used cochlear implants.
Figure 1.
Frequency distribution of parent-reported device use by children at three years of age, separately for the hearing aid (HA) and cochlear implant (CI) user subgroups.
The distribution of children among the categories was quite unbalanced: 295 out of 413 children overall were in the “more than 8” or “always” category, while only 8 were in “less than 1” or “seldom” category , and only 11 were in “never”. Therefore, the three lowest categories were combined for further analysis.
At three years of age, over 71% of the entire study sample were reported to wear their hearing device consistently (see Table 3). Those using cochlear implants at three years of age were significantly more likely to report a higher hearing device usage rating compared to those exclusively using hearing aids (W(2) = 13193.5, p<0.001)
Table 3.
Hearing Device usage at three years of age: total study sample, hearing aid only subgroup and cochlear implant subgroup.
| Total Sample | HA subgroup | CI subgroup | ||||
|---|---|---|---|---|---|---|
| Usage Rating | n | % | n | % | n | % |
| Always | 295 | 71.4 | 194 | 65.3 | 101 | 87.1 |
| Often | 72 | 17.4 | 58 | 19.5 | 14 | 12.1 |
| <50 % of the time | 46 | 11.1 | 45 | 15.2 | 1 | 0.9 |
Eleven subjects were reported to “never” use their hearing aids or cochlear implant. The one unilateral cochlear implant non-user was described in clinical notes as having a family that believed that the cochlear implant didn’t work, and that the electrical stimulation contributed to an increase in facial tics in that child. The family had declined to receive any early intervention services. Of the ten remaining non-users of hearing aids, eight have mild hearing loss (4FAHL <40dBHL); and four have multiple additional disabilities.
Figure 2 shows the distribution of discomfort score for children at 3 years of age, separately for children with hearing aids and those with cochlear implants.
Figure 2.
Frequency distribution of parent-reported ratings of children’s listening discomfort in the PEACH questionnaire.
The data indicate that the majority of children did not experience discomfort (59.7%), or seldom experienced discomfort (26.9%), as reported by parents.
To examine the influence of each factor on device use, separate analyses with each factor were performed. For the entire participant group, higher device usage was associated with a younger age of initial hearing-aid fitting, higher degree of hearing loss, use of cochlear implant, higher levels of maternal education, higher socioeconomic status, and more early intervention hours (see Table 4). Factors that were not significantly associated with reported device use were gender, home communication mode and age of cochlear implantation.
Table 4.
Factors impacting reported daily device use for entire study group at three years of age: Wilcoxon rank sum tests and ordered probit regression.
| W | Estimate | SE | p | |
|---|---|---|---|---|
| Gender | 21489.5 | - | 0.7 | |
| Presence of additional disabilities | 16115.5 | - | 0.06 | |
| Home Communication Mode | 14978 | - | 0.9 | |
| Maternal Education | 14891 | - | <0.001* | |
| Hearing device combination used | 13193.5 | - | <0.001* | |
| Better ear 4FA | - | -0.02 | 0.003 | <0.001* |
| Socio economic status | - | -0.07 | 0.03 | <0.01* |
| Early intervention hours | - | -0.003 | 0.0007 | <0.001* |
| Age initial hearing aid fitting | - | 0.03 | 0.007 | <0.001* |
| Age cochlear implant switch-on | - | 0.009 | 0.007 | 0.2 |
For the hearing-aid only subgroup, factors uniquely and significantly associated with increased daily device use were: more severe hearing loss (Estimate = −0.02, SE=0.004, p <0.001), a younger age of initial hearing aid fitting (Estimate= 0.02, SE=0.007, p = 0.02), a higher maternal education level (W=7651.5, p = <0.001), a higher socioeconomic status (Estimate = −0.08, SE=0.03, p =< 0.01), and a higher number of early intervention hours (Estimate = −0.002, SE=0.001, p =<0.01). In line with the analyses on the entire sample gender (W=10976, p = 0.8), the presence/ absence of additional disabilities (W=8473.5, p = 0.1), and home communication mode (W=7355.5, p = 0.9) were not significantly associated with daily device use.
For those using a cochlear implant at three years of age, higher daily device use was associated with the absence of additional disabilities (W=1128, p = <0.01) and a higher maternal education level (W=1208.5, p= 0.04). Like for the whole study sample, the effects of age of cochlear implantation (Estimate=0.02, SE= 0.02, p=0.3), home communication mode (W=1149, p=0.09) and gender (W=1612, p=0.5) were not significant. Unlike findings from whole group analyses, the number of early intervention hours (Estimate= −0.0006, SE= 0.001, p =0.6) and socioeconomic status (Estimate=−0.07, SE=0.06, p=0.2) were not significantly associated with device use.
Factors influencing device use
Results from the ordered probit regression analyses for the entire study sample, the hearing aid only subgroup and the cochlear implant subgroup are presented in Table 5. After adjusting for the effects of all other variables in the model, level of maternal education level, degree of hearing loss, and socioeconomic status remained significant for the entire study group. There were no other significant factors.
Table 5.
Predictors of device use at three years: Ordered probit regression of Total group, HA subgroup and CI subgroup.
| Total Group | HA subgroup | CI subgroup | ||||
|---|---|---|---|---|---|---|
| Variable | Estimate (SE) | p | Estimate (SE) | p | Estimate (SE) | p |
| Gender (male) | −0.14 (0.15) | 0.09 | −0.10 (0.17) | 0.62 | −0.36 (0.51) | 1.00 |
| Additional disabilities (present) | 0.27 (0.52) | 0.11 | −0.07 (0. 27) | 0.52 | −1.09 (0.54) | 0.11 |
| Home communication mode (other) | 1.00 (0.59) | 0.28 | 1.10 (0.65) | 0.43 | 2.80 (1.51) | 0.50 |
| Maternal education (< university ) | −0.50 (0.17) | <0.001* | −0.03 (0.25) | 0.02* | −1.66 (0.82) | 0.03* |
| Hearing device type (CI) | −1.43 (1.32) | 0.6 | - | - | - | - |
| Better ear 4FA | −0.01 (0.01) | <0.001* | −0.01 (0.01) | <0.001* | −0.02 (0.02) | 0.45 |
| Socio economic status | −0.06 (0.17) | 0.03* | −0.06 (0.03) | 0.06 | 0.29 (0.18) | 0.97 |
| Early intervention hours | −0.001 (0.001) | 0.16 | −0.001 (0.001) | 0.10 | −0.001 (0.003) | 1.00 |
| Age initial HA fitting | 0.01 (0.01) | 0.06 | 0.03 (0.02) | 0.16 | 0.07 (0.05) | 0.35 |
| Age CI switch-on | - | - | - | - | −0.07 (0.05) | 0.21 |
Results from the ordered probit regression analyses for children with hearing aids alone revealed that the degree of hearing loss and maternal level of education were associated significantly with reported usage. The results from children with cochlear implants alone showed that increased device usage was associated with a higher level of maternal education.
Factors influencing changes in use of device over the first 3 years
Three hundred and twenty-seven participants had usage data at three years and from at least one earlier assessment interval. Of these, 58.7% (n=192) reported no change in usage patterns between earlier intervals and three years
Table 6 shows usage over time, separately for users of hearing aids only and users of cochlear implant. Of the 135 participants that reported some change in usage patterns, 67.4% (n=91) reported an increase in usage from previous intervals and 32.6% (n=44) reported a decrease in usage over time. For 13 subjects, a positive trend in usage was seen across intervals, with a higher rating given at twelve months post hearing aid fitting compared to six month post hearing aid fitting and at three years. Conversely, 18 subjects reported a negative trend in usage, with a lower usage rating given at the twelve month post hearing aid fitting or cochlear implantation interval compared to the six month post fitting or switch on date and three year interval. As seen in Table 6, the “change” variable in the dataset was collapsed into three categories: no change, negative change and positive change. Those subjects where fluctuating usage was reported across assessment intervals were moved into the “negative” or “positive” categories, depending on which direction the reported fluctuations occurred. The hearing-aid only group had a smaller proportion of subjects that reported no change between assessment intervals, but had a higher proportion of subjects reporting an increase in usage at three years of age. The hearing-aid only group also had the majority (30/31) of the subjects that reported a fluctuation in usage, both positive (increased usage over time) and negative (decreased usage over time).
Table 6.
Longitudinal usage changes separated by hearing aid and cochlear implant user groups.
| 3yr HA Users | 3yr CI Users | |||
|---|---|---|---|---|
| n | % | n | % | |
| No change | 118 | 49.4 | 74 | 84.1 |
| Positive Change | 87 | 36.4 | 4 | 4.5 |
| Negative Change | 34 | 14.2 | 10 | 11.3 |
| Total | 239 | 100.0 | 88 | 100.0 |
Bivariate analyses showed significant associations between the “change” variable and the type of device used (HA vs CI, W=7668, p <0.001), and degree of hearing loss (Estimate = −0.01, SE=0.002, p<0.01). No significant associations were found between change in device use up to three years of age and age of initial hearing-aid fitting (Estimate = −0.02, SE=0.01, p=0.07), age at cochlear implant switch-on (Estimate = 0.01, SE= 0.01, p=0.3), the presence/absence of additional disabilities (W=10376, p=0.1), home communication mode (W= 9247.5, p=0.6), gender (W=14242, p=0.2), maternal education level (W=10694.5, p=0.07), early intervention hours (Estimate = −0.0002, SE=0.0006, p=0.7) or socioeconomic status (Estimate = 0.04, SE=0.03, p=0.2).
After adjusting for the effect of all other variables in an ordered probit regression model, only the presence / absence of additional disabilities was significantly associated with changes in device use (Estimate= 0.9, SE= 0.36, LRT p= 0.01). Those who had one or more additional disabilities were more likely to experience a decrease in usage over time.
However, when the ordered probit regression model was repeated with those who use hearing aids, none of the factors were found to be significantly associated with changes in hearing device use. A trend was observed that boys tended to experience a decrease in hearing aid use compared to girls, but this did not reach significance (Estimate −0.33, SE= 0.16, LRT p= 0.06).
Lastly, when the ordered probit regression model was repeated with only the cochlear implant users, the presence/ absence of additional disabilities and maternal level of education were significantly associated with changes in cochlear implant use (Maternal education Estimate = 0.94, SE= 0.44, LRT p=0.03; Additional disabilities Estimate= 1.14, SE= 0.48, LRT p= 0.01). Those children whose mothers had completed a university level of education were less likely to report a decrease in cochlear implant usage at any point up to three years of age. Likewise, the presence of one or more additional disabilities was more likely to report a negative direction of cochlear implant usage up to three years of age.
Device use and functional performance
To investigate the relationship between use of device and functional performance in real life, reported device use was treated as an independent variable; with functional performance as scored by the PEACH total standard score as the outcome measure. There was a significant relationship between device use and functional performance standard score, with increased usage associated with higher standard scores (f=4.42, df=2, p=0.01). When incorporated into a multivariate linear regression model to adjust for the effect of all other factors, reported device use was not associated with functional performance (LRT p=0.3, effect size= 0.01). Children with higher functional performance at three years of age also had higher maternal level of education (LRT p=0.02, effect size = 0.04), a higher socio-economic status (LRT p=0.05, effect size =0.02), no additional disabilities (LRT p=<0.001, effect size =0.08), and used speech only as the communication mode at home (LRT p=0.02, effect size =0.03). Overall, these factors accounted for 28% of the variance in functional performance scores.
Discussion
This is the first population study to examine longitudinal use of hearing aids and cochlear implants in young children over the first three years of life. The present findings reveal that by 3 years of age, 71% of children were consistent users of hearing devices. The reported usage was higher for children who used cochlear implants than those who used hearing aids. For the entire sample, higher usage was associated with more severe hearing loss, higher maternal education, and higher socio-economic status.
As indicated in Table 5, severity of hearing loss was a significant predictor of hearing aid use. This finding is consistent with previous studies (Walker et al. 2013; Vesterager & Parving 1995). Children with mild hearing loss tend to use hearing aids less often than those with more severe loss. In the present cohort, about 20% of children have mild hearing loss. Further investigations will be necessary to increase understanding about their amplification needs and to guide best management.
Higher maternal education and socio-economic status were associated with higher device usage. The influence of these predictors on device use is possibly related to the knowledge and beliefs of parents about a potential link between consistent device usage and child development (Moeller et al. 2009; Elfenbein 1994).
The present study documented changes in use of device over the first 3 years of life, both for children with hearing aids and children with cochlear implants. For the entire sample, the presence of additional disabilities was the single factor that influenced changes in the use of device. Separate analyses for children with hearing aids showed a trend for girls to be more consistent users over time than boys, although it did not reach significance level. It may be that boys were involved in more situations such as sports in the playfield that might pose special challenges, and would therefore require clinical support to address their needs in specific environments. Further investigations into potential situational or developmental reasons (Walker et al. 2013; Archbold et al. 2009) affecting device use are likely to guide better support for consistent usage of hearing devices. For children with cochlear implants, higher maternal education and absence of additional disabilities were associated with consistent usage of device over the first 3 years of life.
A major strength of this study is in its population-base and its prospective design. The cohort is unique in its access to uniform audiological services of the single government-funded national hearing service provider, at no costs to families. The sample size allowed for the investigation of the influence of a range of demographic and audiological characteristics, including the presence of additional disabilities, on device usage in the same cohort. The prospective design allowed for an examination of changes in use of device from soon after fitting to 3 years of age. The findings revealed that consistent use (>75% of waking hours) was established for 62% (n=256) of children within the first year of amplification, and 71% (n=295) reported consistent usage at 3 years of age.
Limitations
The present study was based on parent reports. It is possible that parents might have over-estimated device usage in their reports. Although data logging features in devices may provide a more accurate record of device usage (Walker et al 2013), the use of parent reports lends itself to building rapport with the family and to encourage and support consistent device usage.
The present study found that the presence of additional disabilities influenced the frequency of device usage for children with cochlear implants. As the range of disabilities occurred in different combinations for many children, it was not possible at this time to examine the relationship between device usage and specific disability types. Future investigations of the effect of additional disability on device use will include nonverbal cognitive ability (to be assessed when the children turn 5 years of age) as a predictor variable. In line with previous investigations on this cohort showing that children with additional disabilities not entailing developmental delay had better language outcomes than those diagnosed with delays (Cupples et al, 2014), we hypothesized that cognitive ability, rather than type of disability, is likely to influence device usage.
The present study did not examine the impact of the use of FM systems or other assistive listening devices on daily hearing aid or cochlear implant use. This is an area we aim to investigate in future studies.
The findings of this study may not be generalizable to settings wherein access to uniform audiological services and technology varies from that in Australia. As indicated in a previous study on hearing device usage in children, clinical site could be a potential confounder (Walker et al. 2013).
Conclusion
The present population based study provides insights into factors that affect use of device over the first 3 years of life in young children with hearing loss while controlling for variations in service provision and a range of demographic variables. Within the first year of fitting, 62% of the cohort used hearing devices for more than 75% of their waking hours. By 3 years of age, 71% of the cohort was using hearing aids or cochlear implants consistently. Higher usage was associated with greater hearing loss, higher maternal education and socio-economic status. Device use was significantly associated with functional performance in real life.
Acknowledgments
We gratefully thank all the children, their families and their teachers for participation in this study.
We thank Kathryn Crowe and Nicole Mahler-Thompson for their assistance in data collection; and the many persons who served as clinicians for the study participants or assisted in other clinical or administrative capacities at Australian Hearing, Hear and Say Centre, the Royal Institute for Deaf and Blind Children, and the Shepherd Centre.
The project described was partly supported by Award Number R01DC008080 from the National Institute On Deafness And Other Communication Disorders. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute On Deafness And Other Communication Disorders or the National Institutes of Health.
The authors acknowledge the financial support of the HEARing CRC, established and supported under the Cooperative Research Centres Program – an Australian Government initiative.
Abbreviations
- 4FAHL
Four-frequency average hearing level, across 0.5, 1, 2, and 4 kHz
- AH
Australian Hearing Services
- CI
Cochlear implant
- dBHL
Decibels in hearing level
- FM
Frequency modulation
- HA
Hearing aid
- IRSAD
Index of Relative Socio-economic Advantage and Disadvantage
- LOCHI
Longitudinal Outcomes of Children with Hearing Impairment study
- PEACH
Parent’ Evaluation of Aural/oral performance of Children
- SEIFA
Socio-Economic Index For Areas
- SES
Socio-economic status
- TEACH
Teacher’s Evaluation of Aural/oral performance of Children
- UNHS
Universal newborn hearing screening
Footnotes
Declaration of interest:
The authors report no conflict of interest.
The authors alone are responsible for the content and writing of the paper.
References
- Archbold SM, Nikolopoulos TP, Lloyd-Richmond H. Long-term use of cochlear implant systems in paediatric recipients and factors contributing to non-use. Cochlear Implants International. 2009;10(1):25–40. doi: 10.1179/cim.2009.10.1.25. Available at: Publisher URL: www.cinahl.com/cgi-bin/refsvc?jid=3546&accno=2010203883. [DOI] [PubMed] [Google Scholar]
- Australian Bureau of Statistics. An introduction to Socio-Economic Indexes for Areas (SEIFA) 2006. Australian Bureau of Statistics; 2008. [Google Scholar]
- Ching TYC, et al. Outcomes of early- and late-identified children at 3 years of age: findings from a prospective population-based study. [Accessed September 6, 2013];Ear and hearing. 2013 34(5):535–52. doi: 10.1097/AUD.0b013e3182857718. Available at: http://www.ncbi.nlm.nih.gov/pubmed/23462376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ching TYC, et al. Performance in children with hearing aids or cochlear implants: Bilateral stimulation and binaural hearing. International Journal of Audiology. 2006;45:108–12. doi: 10.1080/14992020600783087. Available at: Publisher URL: www.cinahl.com/cgi-bin/refsvc?jid=2576&accno=2009306856. [DOI] [PubMed] [Google Scholar]
- Ching TYC, Hill M. The Parent’s Evaluation of Aural/Oral Performance of Children (PEACH) Scale: Normative data. Journal of the American Academy of Audiology. 2007;18(3):220–235. doi: 10.3766/jaaa.18.3.4. Available at: Publisher URL: www.cinahl.com/cgi-bin/refsvc?jid=946&accno=2009567833. [DOI] [PubMed] [Google Scholar]
- Ching TYC, Hill M, Dillon H. Effect of variations in hearing-aid frequency response on real-life functional performance of children with severe or profound hearing loss. International Journal of Audiology. 2008;47(8):461–475. doi: 10.1080/14992020802116128. Available at: http://0-ovidsp.ovid.com.library.newcastle.edu.au/ovidweb.cgi?T=JS&NEWS=N&PAGE=fulltext&D=medl&AN=18698522. [DOI] [PubMed] [Google Scholar]
- Cupples L, et al. Outcomes of 3-year-old children with hearing loss and different types of additional disabilities. Journal of Deaf Studies and Deaf Education. 2014;19(1):20–39. doi: 10.1093/deafed/ent039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elfenbein JL. Monitoring Preschoolers’ Hearing Aids. American Journal of Audiology. 1994;3:65–70. doi: 10.1044/1059-0889.0302.65. Available at: http://aja.asha.org/cgi/content/abstract/3/2/65. [DOI] [PubMed] [Google Scholar]
- Kiese-Himmel C, Ohlwein S, Kruse E. Acceptance of wearing hearing aids by children: a longitudinal analysis. HNO. 2000;48(10):758–764. doi: 10.1007/s001060050655. Available at: http://search.ebscohost.com/login.aspx?direct=true&db=cmedm&AN=11103348&site=ehost-live. [DOI] [PubMed] [Google Scholar]
- King AM. The national protocol for paediatric amplification in Australia. International Journal of Audiology. 2010;49:64–69. doi: 10.3109/14992020903329422. Available at: http://search.ebscohost.com/login.aspx?direct=true&db=rzh&AN=2010553755&site=ehost-live. [DOI] [PubMed] [Google Scholar]
- Marttila TI, Karikoski JO. Hearing aid use in Finnish children: Impact of hearing loss variables and detection delay. International Journal of Pediatric Otorhinolaryngology. 2006;70(3):475–480. doi: 10.1016/j.ijporl.2005.07.028. Available at: http://0-ovidsp.ovid.com.library.newcastle.edu.au/ovidweb.cgi?T=JS&NEWS=N&PAGE=fulltext&D=medl&AN=16174537. [DOI] [PubMed] [Google Scholar]
- Moeller MP, et al. Consistency of hearing aid use in infants with early-identified hearing loss. American Journal of Audiology. 2009;18(1):14–23. doi: 10.1044/1059-0889(2008/08-0010). Available at: http://aja.asha.org/cgi/content/abstract/18/1/14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RStudio. RStudio: integrated development environment for R. 2012 Available at: http://www.rstudio.org/.
- Tange R, Grolman W, Dreschler W. What to do with the other ear after cochlear implantation. Cochlear Implants International: An Interdisciplinary Journal. 2009;10(1):19–24. doi: 10.1002/cii.373. Available at: Publisher URL: www.cinahl.com/cgi-bin/refsvc?jid=3546&accno=2010203881. [DOI] [PubMed] [Google Scholar]
- Team RC. R: A Language and Environment for Statistical Computing. 2012 Available at: http://www.r-project.org.
- Vesterager V, Parving A. Rehabilitation of hearing-impaired children: Intervention and outcome. Audiology. 1995;34(4):207. doi: 10.3109/00206099509071913. Available at: http://search.proquest.com/docview/194776149?accountid=14723. [DOI] [PubMed] [Google Scholar]
- Walker EA, et al. Predictors of Hearing Aid Use Time in Children With Mild-to-Severe Hearing Loss. Language, Speech, and Hearing Services in Schools. 2013;44(1):73–88. doi: 10.1044/0161-1461(2012/12-0005). Available at: http://lshss.asha.org/cgi/content/abstract/44/1/73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson LM, Gregory S. Non-use of cochlear implants in children: Child and parent perspectives. Deafness and Education International. 2005;7(1):43–58. Available at: Publisher URL: www.cinahl.com/cgi-bin/refsvc?jid=2192&accno=2005097871. [Google Scholar]