Abstract
We examined the association between physical activity (PA), neurocognitive impairment (NCI), and instrumental activities of daily living (IADLs) among older HIV+ persons. One hundred older HIV+ adults completed the International Physical Activity Questionnaire (IPAQ), a neurocognitive battery, and IADL scale. Higher levels of moderate PA were associated with lower odds of NCI (p=0.01), even when covariates were modeled. The association between moderate PA and NCI was driven by executive function (p=0.04). Higher levels of moderate PA were also associated with lower odds of IADL Dependence (p = 0.03), although this fell to a trend (p = 0.08) when including covariates. Follow-up analysis showed those with both NCI and IADL Dependence had lower moderate PA than those with neither (p=0.03). While these cross-sectional findings suggest PA is associated with better neurocognitive and everyday functioning in older HIV+ adults, longitudinal studies utilizing objective PA methods are needed to evaluate directionality and mechanisms.
Keywords: Exercise, Aging, HIV/AIDS, Cognition, IADLs, Physical Therapy
Introduction
There has been a recent increase in the incidence and prevalence of HIV among older adults (i.e., aged 50 and above) due to an increase in new diagnoses in older adults and decreases in mortality with antiretroviral therapy (ART), respectively (1). By 2015, half of those living with HIV/AIDS in the U.S. will be aged 50 and above, and the proportion is expected to rise to 70% by 2020 (2,3). Recent reports by the NIH Office of AIDS Research and the U.S. Senate Special Committee on Aging emphasize the significant public health priority for research in this vulnerable and growing population (3,4). In particular, research on cognitive aging with HIV is needed, given that HIV and aging have additive detrimental effects on brain structure and function (5-10), which may translate to additive (and potentially synergistic) effects on neurocognitive impairment (NCI) (11).
HIV-associated neurocognitive disorders (HAND) are observed in as many as half of HIV-infected (HIV+) adults (12), and older adults with HIV are at a three-fold increased risk of HAND relative to younger HIV+ adults (13). At the neurocognitive domain level, older HIV-infected adults appear to be particularly vulnerable to deficits in the areas of executive functions (e.g., 14) and episodic memory (e.g., 15,16). These neurocognitive deficits among older HIV+ individuals translate to an increased risk for problems in real-world everyday functioning, including difficulties with driving, managing medications, and other instrumental activities of daily living (IADLs) (17-21). IADL impairments in this group represent a significant public health burden and a threat to successful cognitive aging at the individual level.
There are numerous potential mechanisms underlying the heightened risk for NCI in older HIV+ adults. Medical comorbidities are elevated among older adults, and HIV+ persons have been shown to have a disproportionate number of these comorbidities (e.g., hypertension, diabetes, and cardiovascular disease) as compared to HIV-uninfected individuals (22-26). Moreover, older individuals who present with HIV infection are more susceptible to a delayed HIV diagnosis and subsequently may present with more severe immunosuppression. In contrast, older HIV+ persons with a long duration of infection may have had longer ART exposure, and a greater potential to be exposed to older, more toxic ART regimens (22,27,28).
Physical activity (PA) as a cognitive protective factor and intervention strategy to improve cognitive functioning has grown in interest over the past decades in the general population, as well as in HIV populations. Intervention studies have shown that PA, as a behavioral tool, is associated with delayed cognitive decline in older, HIV-seronegative populations (e.g., 29-32). However, among HIV populations, the vast majority of the studies have examined the positive effects of PA on physiological outcomes, such as body composition (33,34), lipodystrophy (35), muscle strength (36,37), vascular and metabolic biomarkers such as cholesterol and triglycerides (38), and aerobic capacity (i.e., maximal oxygen consumption [VO2max]) (34,38,39).
The few studies of PA and neurocognitive outcomes among HIV populations have yielded significant associations. Honn et al., (40) found that self-reported PA was associated with better performance on measures of psychomotor speed and attention/working memory in a sample of HIV+ young adult men (mean age = 33.0; standard deviation = 7.0). Fillipas et al., (41) found that a PA intervention in middle-aged (mean age = 43.5; standard deviation = 8.0) HIV+ men resulted in significant improvements in self-reported cognitive problems; however, objective cognitive performance was not examined. A study by our group (i.e., the HIV Neurobehavioral Research Program [HNRP]) (42) found that self-reported PA was associated with less NCI, particularly in the working memory and speed of processing domains, in middle-aged adults (mean age = 47.4; standard deviation = 10.3) with HIV. Regarding everyday functioning, studies in HIV have shown positive effects of PA on psychosocial outcomes such as quality of life and mood (43,44), but no studies have explicitly examined PA and IADLs in HIV, which is an important outcome in aging populations.
Thus, the purpose of the current study was to examine the association between PA and concurrent neurocognitive and everyday functioning in a well-characterized sample of older HIV+ adults. This study extends the limited prior literature on the association between PA and neurocognitive and everyday functioning among HIV-infected adults in four important ways: 1) examining this association within older HIV+ adults; 2) assessing real-world everyday functioning (i.e., IADL Dependence); 3) examining the independence of the association by considering relevant covariates; and 4) using a well-validated PA instrument.
Method
Participants and Procedure
The present study examined 100 community-dwelling, older (i.e., aged 50 years and above), HIV-infected adults from Successfully Aging Seniors with HIV (SASH) study conducted at the University of California (UCSD) HNRP. The study was approved by the UCSD Institutional Review Board and all participants provided written informed consent to participate. Exclusion criteria included a history of non-HIV related neurologic disorders (e.g., Parkinson's Disease) or any other known conditions that may be associated with impaired neurocognitive performance (e.g., seizure disorder, stroke, head trauma with loss of consciousness greater than 30 minutes, and self-reported history of psychotic disorders). See Table I for the full list of sample characteristics.
Table I. Sample Demographic, Psychiatric, and HIV-Disease Characteristics (N=100).
| Variable | Mean (SD) or % | Range |
|---|---|---|
| Demographics | ||
| Age | 58.2 (6.5) | 50 – 79 |
| Sex (% Male) | 88% | -- |
| Education | 14.3 (2.6) | 8 – 20 |
| Race (% White) | 82% | -- |
| HIV Characteristics | ||
| Current CD4* | 597 (365.0 – 776.0) | 6 – 1,606 |
| Nadir CD4* | 135.5 (39.5 – 300.0) | 0 – 850 |
| AIDS Status (% Yes) | 66% | -- |
| ART status (% On) | 98% | -- |
| Plasma Viral Load (% Undetectable) | 92% | -- |
| Est. Duration HIV Infection (yrs) | 18.0 (8.0) | 1 – 30 |
| Comorbidities | ||
| Hypertension (% with) | 50% | |
| Hyperlipidemia (% with) | 61% | |
| Diabetes (% with) | 26% | |
| HCV (% with) | 22% | |
| Mental Health | ||
| Lifetime MDD Diagnosis (% Yes) | 60% | -- |
| Current MDD Diagnosis (% Yes) | 14% | -- |
| Lifetime Substance Diagnosis (% Yes) | 70% | -- |
| Current Substance Diagnosis (% Yes) | 6% | -- |
| Global Neurocognitive Impairment (% Yes) | 43% | -- |
Notes. ART=antiretroviral therapy; MDD=Major Depressive Disorder.
Median (IQR) reported for these variables.
Physical Activity
The International Physical Activity Questionnaire (IPAQ) Short Form (45) was used to measure self-reported engagement in PA over the past seven days. In the current study, staff administered the IPAQ to ensure consistency and accuracy of data collection. Participants were queried about their frequency (i.e., number of days) and duration (i.e., number of minutes per day) in walking, moderate-intensity activity, and vigorous-intensity activity, over the past seven days across any of the following domains: leisure time PA, domestic activities, work-related activities, and transport-related activities. Using established IPAQ guidelines for scoring, metabolic equivalent (MET) minutes per week continuous scores were generated for walking, moderate activity, vigorous activity, and total activity, separately. Higher IPAQ scores reflect greater engagement in PA, taking into account established MET values for each activity level (i.e., walking: 3.3; moderate: 4.0; vigorous: 8.0). An overall categorical IPAQ score is also yielded, which classifies subjects into three PA levels: low, moderate, and high. Descriptive detailed IPAQ data are reported in Table II.
Table II. International Physical Activity Questionnaire Descriptives (N=100).
| Variable | Median (IQR), M(SD), or % | Range |
|---|---|---|
| Walking | ||
| IPAQ Continuous Score | 594.0 (251.6 – 1,534.5) | 0 – 4,158 |
| Walking Minutes Per Week* | 180 (76.3 – 465) | 0 – 1,260 |
| Any Walking (% Yes)* | 89.0% | -- |
| Moderate PA | ||
| IPAQ Continuous Score | 210.0 (0 – 1,080.0) | 0 – 5,040 |
| Moderate Minutes Per Week* | 52.5 (0 – 270.0) | 0 – 1,260 |
| Any Moderate PA (% Yes)* | 59.0% | -- |
| Vigorous PA | ||
| IPAQ Continuous Score | 480.0 (0 – 1,440.0) | 0 – 10,080 |
| Vigorous Minutes Per Week* | 60 (0 – 180) | 0 – 1,260 |
| Any Vigorous PA (% Yes)* | 53.0% | -- |
| Total | ||
| IPAQ Continuous Score | 2,214.8 (462.0 – 4,101.8) | 0 – 16,398 |
| Total Minutes Per Week* | 510 (140 – 943.8) | 0 – 3,420 |
| Any PA (% Yes)* | 96% | -- |
| Categorical Score | ||
| Low Activity | 33% | -- |
| Moderate Activity | 20% | -- |
| High Activity | 47% | -- |
| Total Days of Activity* | 5.8 (2.1) | 0 - 7 |
| Hours Sitting on Average Day | 6.7 (4.0) | 1 - 22 |
Notes. IPAQ = International Physical Activity Questionnaire.
Not a standard IPAQ variable, these are only provided here to describe the sample.
Outcomes
Neurocognitive Functioning
Participants completed a standardized neurocognitive test battery that assesses seven cognitive domains commonly affected by HIV, including verbal fluency, working memory, speed of information processing, verbal and visual learning and delayed recall, executive function, and motor function. The test scores were adjusted to correct for normal effects of age, gender, education, and race/ethnicity, as indicated (46-48). Each neurocognitive test score was converted to a standard T-score and then into a domain deficit scores for each cognitive domain, as well as a global deficit score. Global deficit scores of .50 or greater were used to classify subjects as neurocognitively impaired (i.e., global NCI) or neurocognitively normal. Domain deficit scores greater than .50 were used to classify domain-level impairment (49).
IADL Dependence
Self-reported everyday functioning was assessed using a modified version of the Lawton and Brody Activities of Daily Living (ADL) Questionnaire (50). The ADL includes questions on the following 11 IADLs: managing finances, managing medications, shopping, buying groceries, cooking, child care, working, transportation, social activities, understanding written material/television, and using the telephone. For each IADL participants report current level of assistance needed as well as highest level of performance. Scoring includes total IADL complaints, which is used to derive the IADL Dependence variable, such that participants were classified as IADL Dependent if their self-reported current functioning level was lower than their highest level of functioning for at least two domains. In this way, the IADL Dependence variable captures both a need for assistance as well as a decline from previous functioning, consistent with the most current research nosology for defining HAND (i.e., Frascati criteria) (51).
Covariates
We also examined common confounders that may influence the relationship between PA and NCI and IADL Dependence, including demographic factors (i.e., age, gender, education, race/ethnicity), HIV disease characteristics (i.e., estimated duration of HIV, current and nadir CD4+ lymphocyte count, AIDS status, ART status, and plasma viral load), lifetime and current substance use disorder diagnosis, and lifetime and current major depressive disorder (MDD) diagnosis. The complete list of potential covariates examined is available in Table I. Nadir CD4+ count was self-reported unless a participant's laboratory CD4 count was lower than the self-reported value. AIDS diagnosis was derived using CDC criteria (52). Plasma HIV viral load was considered “undetectable” below 48 copies/mL. Comorbidity data was gathered using the International Classification of Diseases ninth revision (53). Substance use disorders (i.e., including any current or past diagnosis of substance abuse and/or dependence for the following substances: amphetamine, cocaine, hallucinogen, inhalant, sedative, opioid, PCP, alcohol, marijuana) and MDD diagnoses were assessed through the computer-assisted Composite International Diagnostic Interview, version 2.1 (54).
Statistical Analyses
T-tests and chi-square analyses were conducted to examine the association between IPAQ variables and the primary outcome (i.e., global NCI). In order to present a parsimonious summary of our findings, additional analyses only focus on the IPAQ variable(s) associated with global NCI. Similarly, associations between all Table I demographic, psychiatric, HIV-disease, and comorbidity variables and global NCI and our secondary outcome (i.e., IADL Dependence) were conducted to determine which variables should be considered as covariates in the respective main analyses. We considered covariates in our main analyses that were associated with both the independent variable (PA) and the outcomes at p < 0.10. Main analyses for both global NCI and IADL Dependence used multivariable logistic regressions and included all relevant covariates, determined by the backward stepwise selection method using the conservative minimum Bayesian Information Criterion (BIC) as the stopping rule. Finally, a planned post-hoc analysis was conducted to examine group differences on PA across four groups based upon global NCI and IADL Dependence status (Normal [n = 42], Impaired in Both [n =15], IADL Dependent/NC Normal [n=15], and IADL Independent/NC Impaired [n=28]), similarly controlling for variables associated with PA and NCI/IADL group. In this way we could examine the association between PA and syndromic NCI by combing global NCI and IADL Dependence.
Results
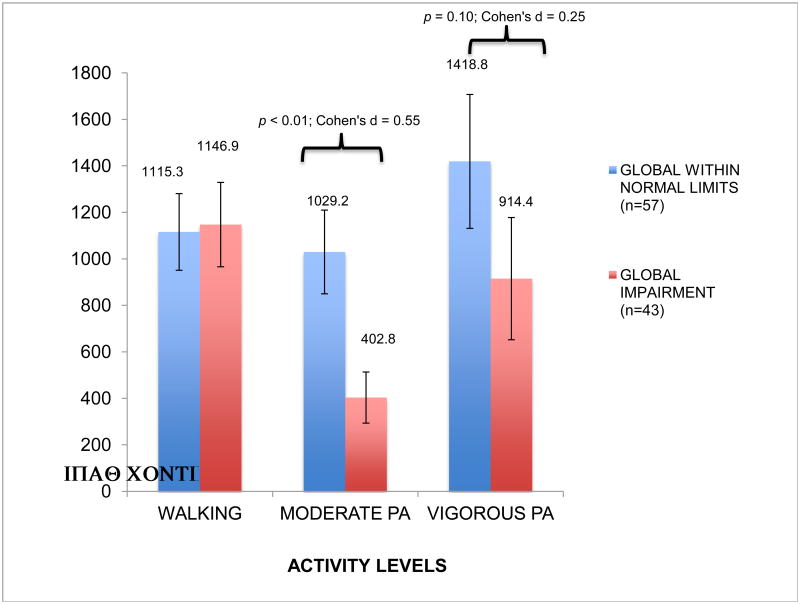
Preliminary t-tests showed that of the IPAQ variables, the moderate IPAQ continuous score was associated with global NCI, whereas other continuous IPAQ variables and the overall IPAQ categorical score were not (p-values > 0.05) (Figure I). Therefore, moderate IPAQ continuous scores were used in all subsequent analyses. Logistic regressions showed that the moderate IPAQ score was significantly associated with both global NCI (χ2 = 8.4, df = 1, p < 0.01) and IADL Dependence (χ2 = 5.0, df = 1, p = 0.03) at the bivariate level. Of the covariates listed in Table I, current MDD and age were associated with both the moderate IPAQ score and global NCI (p < 0.10) while lifetime MDD was associated with both moderate IPAQ score and IADL Dependence (p < 0.10).
Figure I. IPAQ Continuous Scores by Global Neurocognitive Impairment.
Note. Bars represent standard errors. IPAQ = International Physical Activity Questionnaire.
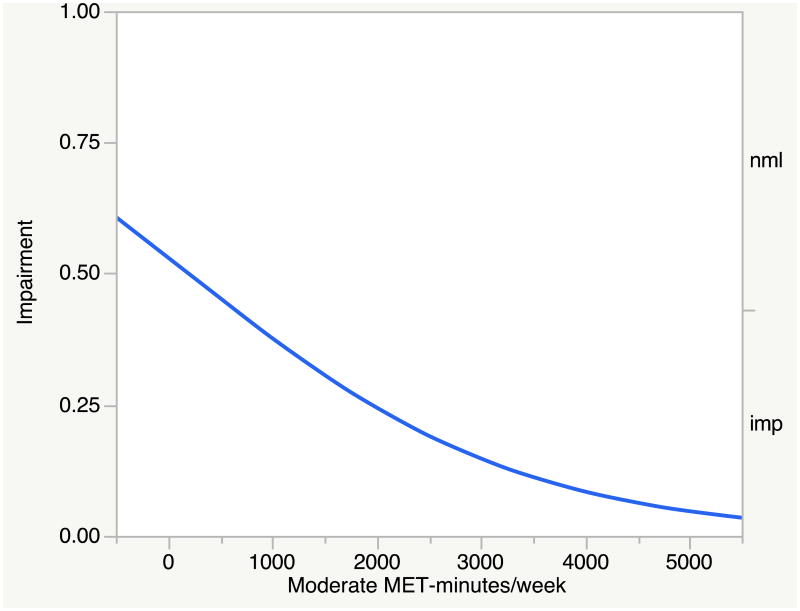
In order to balance good fit with model parsimony, a backward stepwise multivariable logistic regression was conducted entering the moderate IPAQ score as the independent variable, global NCI as the dependent variable, and the aforementioned covariates. Using the minimum BIC value as the stopping rule, only the moderate IPAQ score was retained in the model (p < 0.01). The association showed that higher moderate IPAQ scores were associated with lower odds of global NCI (odds ratio [OR] per 100 units = 0.94; confidence interval [CI] = 0.89–0.98, p < 0.01). For visual purposes, Figure II displays a plot of predicted probabilities from this model, showing that higher moderate IPAQ variables are associated with a lower probability of global NCI.
Figure II. Predicted Probabilities for Global Neurocognitive Impairment by Moderate IPAQ Scores.
Note. Imp = neurocognitively impaired; Nml = neurocognitively normal
We then examined the associations between the moderate IPAQ continuous score and domain level NCI. Bivariate logistic regressions showed that only NCI in the executive function domain was significantly associated with the moderate IPAQ score (χ2 = 6.5, df =1, p = 0.01). In a similar backward stepwise multivariable logistic regression as with global NCI with regard to independent variables, and with executive function NCI as the dependent variable, using the BIC stopping rule, the model retained only the moderate IPAQ score (p = 0.01). The direction of this association was such that higher moderate IPAQ scores were associated with lower odds of executive function NCI.
In order to examine the association between the moderate IPAQ score and IADL Dependence, a backward stepwise multivariable logistic regression was conducted including lifetime MDD as a covariate. Using the BIC value as the stopping rule, only lifetime MDD was retained in the model. A follow-up logistic regression was conducted including lifetime MDD and forcing in the moderate IPAQ score, and showed that higher moderate IPAQ scores were associated with lower odds of IADL Dependence at the trend level (OR per 100 units = 0.96, CI = 0.89 – 1.01, p = 0.08).
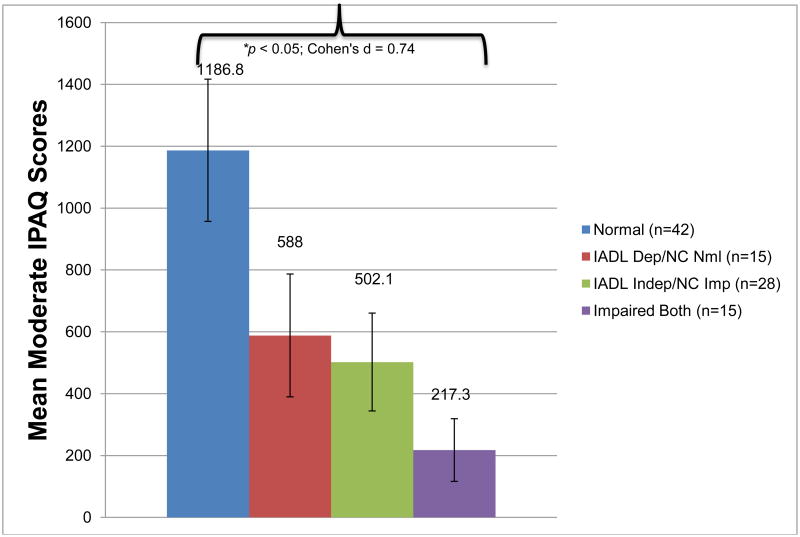
Finally, to examine the association between PA and syndromic NCI (i.e., global NCI and IADL Dependence combined), a planned post-hoc analysis of variance (ANOVA) was conducted examining the differences in the moderate IPAQ score between groups based upon NCI and IADL Dependence (i.e., Normal [n = 42], Impaired in Both [n =15], IADL Dependent/NC Normal [n=15], and IADL Independent/NC Impaired [n=28]). The omnibus ANOVA showed that there was a significant difference across groups on the moderate IPAQ score (F(3, 96) = 3.8, p = 0.01) and Tukey's Honest Significant Difference (HSD) pair-wise tests revealed specifically that the Normal group significantly differed between the Impaired in Both group (p = 0.03) and there was a trend towards a difference between the Normal group and the IADL Independent/NC Impaired group (p = 0.07). This difference remained when controlling for both current and lifetime MDD, which differed across groups and were associated with moderate IPAQ scores. Figure III presents unadjusted moderate IPAQ score means by NCI/IADL groups.
Figure III. Moderate IPAQ Scores by IADL Dependence and Global NCI Groups.
Note. Bars represent standard errors. IPAQ = International Physical Activity Questionnaire;
IADL = instrumental activities of daily living; NC = neurocognitive; Dep = dependent; Indep = independent; Nml = normal; Imp = impaired.
*p < 0.05 for difference between Normal and Impaired Both groups.
Discussion
This cross-sectional study shows that greater levels of self-reported moderate PA are associated with less neurocognitive and everyday functioning impairment among older adults living with HIV. The neurocognitive domain of executive functioning may be most benefited by PA, which is consistent with the non-HIV aging literature (e.g., 29). Furthermore, we found that those with neither IADL Dependence nor global NCI had the highest moderate PA levels compared to those with both IADL Dependence and global NCI.
The mechanisms underlying the association between PA and neurocognitive functioning may be due to changes at the brain level (e.g., via neuroplasticity, neurogenesis, and/or increased cerebral blood flow), an indirect effect via PA reducing cardiovascular comorbidities (e.g., diabetes, hypertension), or a combination of both direct and indirect mechanisms. Although the necessary neuroimaging and physiologic data were not available to examine a direct effect of PA on the brain, we did examine the associations between PA and comorbidities and PA was not associated with any of the cardiovascular conditions. The cross-sectional nature of this study does not allow for determination of causation, thus an alternative explanation of these findings could be that those with NCI and IADL Dependence are less likely and able to participate in PA. Nonetheless, our overall findings support the existing literature in HIV-uninfected populations showing that physical exercise may protect against neurocognitive and everyday functioning impairment.
The finding that only the moderate IPAQ variable was associated with neurocognitive functioning was somewhat unexpected, and warrants further examination. It is possible that the association with moderate PA may imply a dose-dependent response of PA levels on neurocognitive and everyday functioning. For example, low-intensity PA may not produce the optimal amount of neuroprotective physiologic effects whereas vigorous PA could possibly excite certain neurotoxins and further distribute them throughout the brain. Furthermore, perhaps the association with the IPAQ total score and NCI was not significant because on average, 52% of the total score was comprised of walking (meaning that was the most common for most people) and perhaps that was diluting the effect. On the other hand, studies have also shown that walking is associated with better cognitive outcomes (57); thus, caution should be used when interpreting the effect of moderate PA. Nonetheless, many interventional studies have used moderate PA with successful results on neurocognitive outcomes, and our findings support moderate PA as the optimal dose for positive neurologic outcomes (58,59).
However, it is likely that the unique association with moderate PA may also have been due to measurement limitations of the IPAQ. It should be noted that while the IPAQ continuous scores are independent (i.e., participants are instructed to report walking in the “walking” category only and not in the “moderate” category), neither the total continuous score (sum of walking, moderate, and vigorous activity) was associated with our outcomes, nor was a sum created based on walking and moderate continuous scores. This suggests there may be reporting and measurement issues with the IPAQ. Indeed, studies have shown that there are both under and over reporting issues with the IPAQ in both older and younger populations (60). Furthermore, one study found that individuals with HIV over-report vigorous PA as they may report an activity as vigorous from their perspective, when objectively the activity may only be moderate or less (61). Other studies have also found advantages to making cultural adaptations to the IPAQ for older adults, including modifying order of questions and providing more culturally relevant examples of PA (62).
These findings highlight the need for further research (both observational and interventional) to examine the association of PA with neurocognitive and everyday functioning outcomes in older HIV+ adults to determine both dosage and mechanisms (direct and indirect). Specifically, these studies should use objective PA and neuroimaging assessment methods (e.g., pedometers, accelerometers, cerebral blood flow, heart rate variability, fMRI) to more precisely examine these relationships. In addition to objectively measuring PA, performance-based everyday functioning assessments should be used as outcomes, which is a limitation of this study. Further, the nature of the PA (e.g., work-related, leisure time exercise) should be taken into consideration. This study also highlights the potential limitations of the IPAQ for older HIV+ populations. Future intervention studies should be carefully designed to objectively measure both PA and neurocognitive and functional trajectories over time, and may benefit from utilizing advanced, real-time mobile technological methods to capture and promote adherence (e.g., text-messaging reminders, cell phone step counts).
Acknowledgments
This work was primarily supported by ID10-SD-057 from California HIV/AIDS Research Program (CHRP) (Determinants of Successful Aging Among Older HIV+ Persons, D.J. Moore, PI) and the University of California San Diego (UCSD) Stein Institute for Research on Aging Faculty Pilot Research Grant, with additional support from the following National Institutes of Health (NIH) grants: P30MH062512 (The HIV Neurobehavioral Research Center [HNRC]); N01 MH22005, HHSN271201000036C, and HHSN271201000030C (The CNS HIV Anti-Retroviral Therapy Effects Research [CHARTER]); P50DA026306 (The Translational Methamphetamine AIDS Research Center [TMARC]); U01MH083506 and R24MH59745 (California NeuroAIDS Tissue Network [CNTN]).
Dr. Fazeli is supported by R25MH081482 from NIMH (Interdisciplinary Research Fellowship in NeuroAIDS, M. Cherner, PI), ID10-SD-057 from California HIV/AIDS Research Program (CHRP) (Determinants of Successful Aging Among Older HIV+ Persons, D.J. Moore, PI), R01MH099987 from NIMH (Multi-Dimensional Successful Aging Among HIV-Infected Adults, D. Jeste/D.J. Moore, co-PIs), L30-AG045921 from NIA (Mechanisms of Successful Cognitive and Functional Aging with HIV, P. Fazeli, PI), and 1K99 AG048762-01 from NIA (A Novel Neurorehabilitation Approach for Cognitive Aging with HIV, P. Fazeli, PI).
References
- 1.Manfredi R. HIV infection and advanced age: Emerging epidemiological, clinical, and management issues. Ageing Research Review. 2004;3:31–54. doi: 10.1016/j.arr.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 2.Smith G. Aging hearing: HIV over fifty, exploring the new threat Senate Committee on Aging. Washington, DC: 2006. [Google Scholar]
- 3.United States Senate Special Committee on Aging. Hearing: Older Americans: The Changing Face of HIV/AIDS in America; One Hundred Thirteenth Congress, first session; September 18, 2013; Washington, D.C. 2013. [Google Scholar]
- 4.High KP, Brennan-Ing M, Clifford DB, et al. HIV and aging: State of knowledge and areas of critical need for research. A report to the NIH Office of AIDS Research by the HIV and aging working group. J Acq Immun Def Synd. 2012;60:S1–S18. doi: 10.1097/QAI.0b013e31825a3668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ernst T, Chang L. Effects of aging on brain metabolism in antiretroviral-naïve HIV patients. AIDS. 2004;18:61–67. [PubMed] [Google Scholar]
- 6.Green DA, Masliah E, Vinters HV, Beizai P, Moore DJ, Achim CL. Brain deposition of beta-amyloid is a common pathologic feature in HIV positive patients. AIDS. 2005;19:407–411. doi: 10.1097/01.aids.0000161770.06158.5c. [DOI] [PubMed] [Google Scholar]
- 7.Jernigan TL, Gamst AC, Archibald SL, et al. Effects of methamphetamine dependence and HIV infection on cerebral morphology. Am J Psychiat. 2005;162:1461–1472. doi: 10.1176/appi.ajp.162.8.1461. [DOI] [PubMed] [Google Scholar]
- 8.Thomas JB, Brier MR, Snyder AZ, Vaida FF, Ances BM. Pathways to neurodegeneration: effects of HIV and aging on resting-state functional connectivity. Neurology. 2013;80(13):1186–1193. doi: 10.1212/WNL.0b013e318288792b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nir TM, Jahanshad N, Busovaca E, et al. Mapping white matter integrity in elderly people with HIV. Hum Brain Mapp. 2014;35(3):975–992. doi: 10.1002/hbm.22228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ances BM, Ortega M, Vaida F, Heaps J, Paul R. Independent effects of HIV, aging, and HAART on brain volumetric measures. J Acq Immun Def Synd. 2012;59(5):469–477. doi: 10.1097/QAI.0b013e318249db17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hardy DJ, Vance DE. The neuropsychology of HIV/AIDS in older adults. Neuropsychol Rev. 2009;19(2):263–272. doi: 10.1007/s11065-009-9087-0. [DOI] [PubMed] [Google Scholar]
- 12.Heaton RK, Clifford DB, Franklin DR, Jr, et al. HIV-associated neurocognitive disorders persist in the era of potent antiretroviral therapy. Neurology. 2010;75:2087–2096. doi: 10.1212/WNL.0b013e318200d727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Valcour V, Shikuma C, Shiramizu B, et al. Higher frequency of dementia in older HIV-1 individuals: The Hawaii Aging with HIV-1 Cohort. Neurology. 2004;63:822–827. doi: 10.1212/01.wnl.0000134665.58343.8d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Iudicello JE, Kellogg E, Weber E, et al. Semantic cueing improves category verbal fluency in persons living with HIV infection. J Neuropsych Clin N. 2012;24(2):183–190. doi: 10.1176/appi.neuropsych.11100301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sacktor N, Skolasky R, Selnes OA, et al. Neuropsychological test profile differences between young and old human immunodeficiency virus- positive individuals. J Neurovirol. 2007;13:203–209. doi: 10.1080/13550280701258423. [DOI] [PubMed] [Google Scholar]
- 16.Woods SP, Dawson M, Weber E, Grant I the HNRC Group. The semantic relatedness of cue-intention pairings influences prospective memory failures in older adults with HIV infection. J Clin Exp Neuropsyc. 2010;32:398–407. doi: 10.1080/13803390903130737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Foley JM, Gooding AL, Thames AD, et al. Visuospatial and attentional abilities predict driving simulator performance among older HIV-infected adults. Am J Alzheimers Dis. 2013;28(2):185–194. doi: 10.1177/1533317512473192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thames AD, Kim MS, Becker BW, et al. Medication and finance management among HIV-infected adults: The impact of age and cognition. J Clin Exp Neuropsyc. 2011;33:200–209. doi: 10.1080/13803395.2010.499357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vance DE, Fazeli PL, Gakumo CA. The impact of neuropsychological performance on everyday functioning between older and younger adults with and without HIV. J Assoc Nurses AIDS Care. 2013;24(2):112–125. doi: 10.1016/j.jana.2012.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vance DE, Wadley VG, Crowe MG, Raper J, Ball KK. Cognitive and everyday functioning in older and younger adults with and without HIV. Clinical Gerontologist. 2011;34(5):413–426. doi: 10.1080/07317115.2011.588545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Morgan EE, Iudicello JE, Weber E, et al. Synergistic effects of HIV infection and older age on daily functioning. J Acq Immun Def Synd. 2012;61:341–348. doi: 10.1097/QAI.0b013e31826bfc53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wendelken LA, Valcour V. Impact of HIV and aging on neuropsychological function. J Neurovirol. 2012;18(4):256–263. doi: 10.1007/s13365-012-0094-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Simone MJ, Applebaum JS. Medical concerns in HIV-positive aging. UCSF AIDS Health Project. 2009;24(3):1–4. [Google Scholar]
- 24.Valcour VG, Shikuma CM, Shiramizu BT, et al. Diabetes, insulin resistance, and dementia among HIV-1 infected patients. J Acq Immun Def Synd. 2005;38(1):31–36. doi: 10.1097/00126334-200501010-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Becker JT, Kingsley L, Mullen J, et al. Vascular risk factors, HIV serostatus, and cognitive dysfunction in gay and bisexual men. Neurology. 2009;73(16):1292–1299. doi: 10.1212/WNL.0b013e3181bd10e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vance DE, Mugavero M, Willig J, Raper JL, Saag MS. Aging with HIV: A cross-sectional study of comorbidity prevalence and clinical characteristics across decades of life. J Assoc Nurses AIDS Care. 2011;22(1):17–25. doi: 10.1016/j.jana.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 27.Mugavero MJ, Castellano C, Edelman D, Hicks C. Late diagnosis of HIV infection: the role of age and sex. Am J Med. 2007;120(4):370–373. doi: 10.1016/j.amjmed.2006.05.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schweinsburg BC, Taylor MJ, Alhassoon OM, et al. Brain mitochondrial injury in human immunodeficiency virus-seropositive (HIV+) individuals taking nucleoside reverse transcriptase inhibitors. J Neurovirol. 2005;11:356–364. doi: 10.1080/13550280591002342. [DOI] [PubMed] [Google Scholar]
- 29.Colcombe SJ, Kramer AF. Fitness effects on the cognitive function of older adults: A meta-analytic study. Psychol Sci. 2003;14:125–130. doi: 10.1111/1467-9280.t01-1-01430. [DOI] [PubMed] [Google Scholar]
- 30.Kramer AF, Hahn S, Cohen NJ, et al. Ageing, fitness, and neurocognitive function. Nature. 1999;400(6743):418–419. doi: 10.1038/22682. [DOI] [PubMed] [Google Scholar]
- 31.Erickson KI, Voss MW, Prakash RS, et al. Exercise training increases size of hippocampus and improves memory. Proc Natl Acad Sci USA. 2011;108(7):3017–3022. doi: 10.1073/pnas.1015950108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gomez-Pinilla F, Hillman C. The influence of exercise on cognitive abilities. Compr Physiol. 2013;3(1):403–428. doi: 10.1002/cphy.c110063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Smith BA, Neidig JL, Nickel JT, et al. Aerobic exercise: effects on parameters related to fatigue, dyspnea, weight and body composition in HIV-infected adults. AIDS. 2001;15:693–701. doi: 10.1097/00002030-200104130-00004. [DOI] [PubMed] [Google Scholar]
- 34.Terry L, Sprinz E, Stein R, Medeiros NB, Oliveira J, Ribeiro JP. Exercise training in HIV-1-infected individuals with dyslipidemia and lipodystrophy 5. Med Sci Sports Exerc. 2006;38(3):411–417. doi: 10.1249/01.mss.0000191347.73848.80. [DOI] [PubMed] [Google Scholar]
- 35.Segatto AFM, Freitas IF, dos Santos VR, et al. Lipodystrophy in HIV/AIDS patients with different levels of physical activity while on antiretroviral therapy. Revista da Sociedade Brasileira de Medicina Tropical. 2011;44(4):420–424. doi: 10.1590/s0037-86822011000400004. [DOI] [PubMed] [Google Scholar]
- 36.Dolan SE, Frontera W, Librizzi J, et al. Effects of a supervised home-based aerobic and progressive resistance training regimen in women infected with human immunodeficiency virus: a randomized trial. Arch Intern Med. 2006;166(11):1225–1231. doi: 10.1001/archinte.166.11.1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hand GA, Phillips KD, Dudgeon WD, Lyerly GW, Durstine JL, Burgess SE. Moderate intensity exercise training reverses functional aerobic impairment in HIV-infected individuals. AIDS Care. 2008;20(9):1066–1074. doi: 10.1080/09540120701796900. [DOI] [PubMed] [Google Scholar]
- 38.Thoni GJ, Fedou C, Brun JF, et al. Reduction of fat accumulation and lipid disorders by individualized light aerobic training in human immunodeficiency virus infected patients with lipodystrophy and/or dyslipidemia. Diabetes Metab. 2002;28(5):397–404. [PubMed] [Google Scholar]
- 39.Perna FM, Laperriere A, Klimas N, et al. Cardiopulmonary and CD4 cell changes in response to exercise training in early symptomatic HIV infection. Med Sci Sports Exerc. 1999;31(7):973–979. doi: 10.1097/00005768-199907000-00009. [DOI] [PubMed] [Google Scholar]
- 40.Honn VJ, Para MF, Whitacre CC, Bornstein RA. Effect of exercise on neuropsychological performance in asymptomatic HIV infection. AIDS Behav. 1999;3(1):67–74. [Google Scholar]
- 41.Fillipas S, Oldmeadow LB, Bailey MJ, Cherry CL. A six-month, supervised, aerobic and resistance exercise program improves self-efficacy in people with human immunodeficiency virus: a randomised controlled trial. Aust J Physiother. 2006;52(3):185–190. doi: 10.1016/s0004-9514(06)70027-7. [DOI] [PubMed] [Google Scholar]
- 42.Dufour CA, Marquine MJ, Fazeli PL, et al. Strenuous exercise is associated with less neurocognitive impairment in HIV-infected adults. J Neurovirol. 2013;19(5):410–417. doi: 10.1007/s13365-013-0184-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stringer WW, Berezovskaya M, O'Brien WA, Beck CK, Casaburi R. The effect of exercise training on aerobic fitness, immune indices, and quality of life in HIV+ patients. Med Sci Sports Exerc. 1998;30(1):11–16. doi: 10.1097/00005768-199801000-00003. [DOI] [PubMed] [Google Scholar]
- 44.Neidig JL, Smith BA, Brashers DE. Aerobic exercise training for depressive symptom management in adults living with HIV infection. J Assoc Nurses AIDS Care. 2003;14(2):30–40. doi: 10.1177/1055329002250992. [DOI] [PubMed] [Google Scholar]
- 45.Craig CL, Marshall AL, Sjostrom M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 46.Heaton RK, Miller SW, Taylor MJ, Grant I. Revised Comprehensive Norms for an Expanded Halstead-Reitan Battery: Demographically Adjusted Neuropsychological Norms for African American and Caucasian Adults. Lutz, FL.: Psychological Assessment Resources; 2004. [Google Scholar]
- 47.Heaton RK, Taylor MJ, Manly JJ. Demographic effects and use of demographically corrected norms with the WAIS-III and WMS-III. In: Tulsky D, Saklofske D, Heaton RK, et al., editors. Clinical Interpretation of the WAIS-III and WMS-III. San Diego, CA: Academic Press; 2002. [Google Scholar]
- 48.Norman MA, Moore DJ, Taylor M, et al. Demographically corrected norms for African Americans and caucasians on the Hopkins Verbal Learning Test-Revised, Brief Visuospatial Memory Test-Revised, Stroop Color and Word Test, and Wisconsin Card Sorting Test 64-Card Version. J Clin Exp Neuropsyc. 2011;33(7):793–804. doi: 10.1080/13803395.2011.559157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Carey C, Woods SP, Rippeth JD, et al. Initial validation of a screening battery for the detection of HIV-associated cognitive impairment. Clin Neuropsychol. 2004;18(2):234–248. doi: 10.1080/13854040490501448. [DOI] [PubMed] [Google Scholar]
- 50.Lawton MP, Brody EM. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9(3):179–186. [PubMed] [Google Scholar]
- 51.Antinori A, Arendt G, Becker JT, et al. Updated research nosology for HIV-associated neurocognitive disorders. Neurology. 2007;69:1789–1799. doi: 10.1212/01.WNL.0000287431.88658.8b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Castro KG, Ward JW, Slutsker L, Buehler JW, Jaffe HW, Berkelman RL. 1993 revised classification system for HIV infection and expanded surveillance case definition for AIDS among adolescents and adults. US Department of Health and Human Services; 1992. [PubMed] [Google Scholar]
- 53.American Medical Association. ICD-9-CM 2014 Physician Codebook. 1 and 2 [Google Scholar]
- 54.World Health Organization. Composite International Diagnostic Interview (CIDI, version 2.1) Geneva, Switzerland: 1998. [Google Scholar]
- 55.Rosa EF, Takahashi S, Aboulafia J, Nouailhetas VLA, Oliveira MGM. Oxidative stress induced by intense and exhaustive exercise impairs murine cognitive function. J Neurophysiol. 2007;98:1820–1826. doi: 10.1152/jn.01158.2006. [DOI] [PubMed] [Google Scholar]
- 56.Ogonovsky H, Berkes I, Kumagai S, et al. The effects of moderate-, strenuous- and over-training on oxidative stress markers, DNA repair, and memory, in rat brain. Neurochem Int. 2005;46:635–640. doi: 10.1016/j.neuint.2005.02.009. [DOI] [PubMed] [Google Scholar]
- 57.Weuve J, Kang JH, Manson JE, Breteler MMB, Ware JH, Grodstein F. Physical activity, including walking, and cognitive function in older women. JAMA. 2005;292(12):1454–1461. doi: 10.1001/jama.292.12.1454. [DOI] [PubMed] [Google Scholar]
- 58.Hogan CL, Mata J, Carstensen LL. Exercise holds immediate benefits for affect and cognition in younger and older adults. Psychol Aging. 2013;28(2):587–594. doi: 10.1037/a0032634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kamijo K, Hayashi Y, Sakai T, Yahiro T, Tanaka K, Nishihira Y. Acute effects of aerobic exercise on cognitive function in older adults. J Gerontol B Psychol Sci Soc Sci. 2009;64(3):356–363. doi: 10.1093/geronb/gbp030. [DOI] [PubMed] [Google Scholar]
- 60.Heesch KC, van Uffelen JGZ, Hill RL, Brown WJ. What do IPAQ questions mean to older adults? Lessons from cognitive interviews. Int J Behav Nutr Phy. 2010;7(35):e1–e13. doi: 10.1186/1479-5868-7-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Fillipas S, Cicuttini F, Holland AE, Cherry CL. The International Physical Activity Questionnaire overestimates moderate and vigorous physical activity in HIV-infected individuals compared to accelerometry. J Assoc Nurses AIDS Care. 2010;21:173–181. doi: 10.1016/j.jana.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 62.Hurtig-Wennlof A, Hagstromer M, Olsson LA. The International Physical Activity Questionnaire modified for the elderly: aspects of validity and feasibility. Public Health Nutr. 2010;13(11):1847–1854. doi: 10.1017/S1368980010000157. [DOI] [PubMed] [Google Scholar]