Sir,
We describe an unusual case of acute bacterial arthritis affecting the glenohumeral joint secondary to Streptococcus dysgalactiae subsp. equisimilis (SDSE).
A 26-year-old right-handed Caucasian male retail worker presented to the emergency department (ED) with 5 days of gradually increasing right shoulder pain and decreased range of movement (ROM). No history of injury/trauma/infection/pyrexia/travel. Examination revealed some tenderness on deep-palpation over the anterior joint-line with decreased passive and active ROM. Plain-film radiographs were normal. The patient was discharged with appropriate counseling, analgesia and planned review in 10 days.
Four days later, he re-attended the ED with significantly increased pain and was referred to the acute shoulder clinic. He was pyrexial (38.0°C), C-reactive protein 187 mg/L, erythrocyte sedimentation rate 38 mm/h and normal white blood cell count. Nevertheless, he felt systemically well. Blood-borne virus screen was negative with no history of intravenous drug use/recent tattoos.
An ultrasound scan revealed an intact rotator cuff with a small to moderate glenohumeral effusion, which was aspirated. Magnetic resonance imaging (MRI) [Figure 1] showed moderate glenohumeral effusion with abnormal marrow T1 signal within the bone and edema in the region of the posterior greater tuberosity, a small cystic area posteriorly was demonstrated. This was consistent with septic arthritis with underlying acute osteomyelitis.
Figure 1.
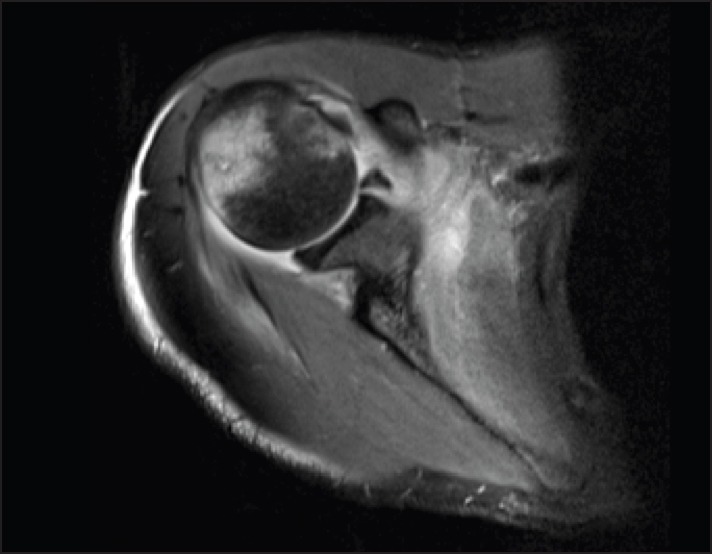
Presenting magnetic resonance imaging showing small cystic area posteriorly features would be consistent with osteomyelitis with a tiny intraosseous collection (original)
Arthroscopic washout was undertaken. Extensive synovial thickening was seen and arthroscopic capsular release performed to improve ROM. Under direct vision, percutaneous drilling of the posterior-aspect of the humeral head (bare area) was performed, and samples sent for microbiological and histological analysis.
Three synovial fluid samples cultured SDSE. The patient received intravenous benzylpenicillin for 26 days and discharged with 3 further weeks of clindamycin plus physiotherapy rehabilitation.
Two-month follow-up revealed a good recovery with restored function and the patient was happy with the outcome. MRI showed complete resolution of glenohumeral effusion, but ongoing asymptomatic static partial bony collapse at the posterior-aspect of the humeral head was demonstrated [Figure 2].
Figure 2.
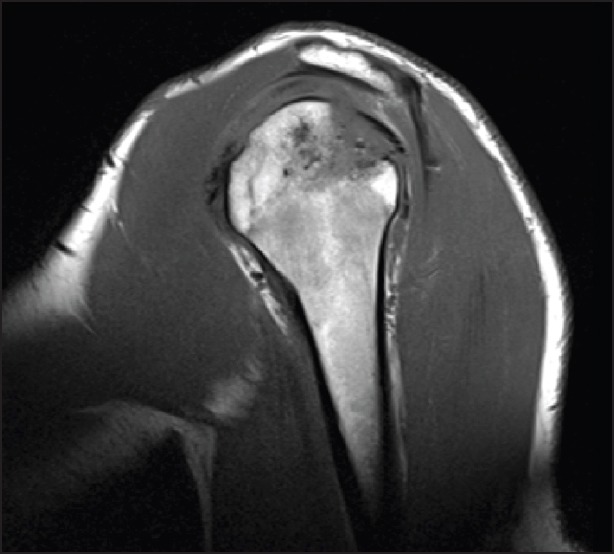
Follow-up magnetic resonance imaging after completion of treatment demonstrating partial collapse of the posterior superior humeral head (original)
Literature review failed to reveal a case of septic arthritis associated with SDSE where only the glenohumeral joint was affected, we found one case of glenohumeral involvement in the setting of polyarticular arthritis.[1]
Streptococcus dysgalactiae subsp. equisimilis is a beta-hemolytic streptococci and is a colonizer of the respiratory, gastro-intestinal and genito-urinary tract.[2] Unlike others in the same class no infective animal reservoir has been demonstrated and transmission is person-person.[3] Although rare the incidence of septic arthritis due to SDSE appears to be increasing (unclear if this is due to improved microbiological diagnosis) with weight bearing joints the most commonly affected.[1] Both healthy individuals and those with pre-existing comorbidities can be affected, there appears to be a male predominance.[1] SDSE is susceptible to penicillin and beta-lactam agents therefore penicillin is the first line antibiotic.[2,3] In some an increased minimum-inhibitory-concentration of 0.25 μg/mL for penicillin has been noted thus in serious infections some add an aminoglycoside.[3]
Above is what we believe to be the first description of glenohumeral arthritis (as a monoarthropathy) due to SDSE. This case reinforces the need for accurate organism identification as this informs treatment and guides investigations for associated complications/conditions. Finally where unusual pathogens are identified appropriate investigation for immunodeficiency is essential.
REFERENCES
- 1.González Terán B, Roiz MP, Ruiz Jimeno T, Rosas J, Calvo-Alén J. Acute bacterial arthritis caused by group C streptococci. Semin Arthritis Rheum. 2001;31:43–51. doi: 10.1053/sarh.2001.21405. [DOI] [PubMed] [Google Scholar]
- 2.Broyles LN, Van Beneden C, Beall B, Facklam R, Shewmaker PL, Malpiedi P, et al. Population-based study of invasive disease due to beta-hemolytic streptococci of groups other than A and B. Clin Infect Dis. 2009;48:706–12. doi: 10.1086/597035. [DOI] [PubMed] [Google Scholar]
- 3.Brandt CM, Spellerberg B. Human infections due to Streptococcus dysgalactiae subspecies equisimilis. Clin Infect Dis. 2009;49:766–72. doi: 10.1086/605085. [DOI] [PubMed] [Google Scholar]


