Abstract
OBJECTIVE:
To assess whether the implementation of English smoke-free legislation in July 2007 was associated with a reduction in hospital admissions for childhood asthma.
METHODS:
Interrupted time series study using Hospital Episodes Statistics data from April 2002 to November 2010. Sample consisted of all children (aged ≤14 years) having an emergency hospital admission with a principle diagnosis of asthma.
RESULTS:
Before the implementation of the legislation, the admission rate for childhood asthma was increasing by 2.2% per year (adjusted rate ratio 1.02; 95% confidence interval [CI]: 1.02–1.03). After implementation of the legislation, there was a significant immediate change in the admission rate of −8.9% (adjusted rate ratio 0.91; 95% CI: 0.89–0.93) and change in time trend of −3.4% per year (adjusted rate ratio 0.97; 95% CI: 0.96–0.98). This change was equivalent to 6802 fewer hospital admissions in the first 3 years after implementation. There were similar reductions in asthma admission rates among children from different age, gender, and socioeconomic status groups and among those residing in urban and rural locations.
CONCLUSIONS:
These findings confirm those from a small number of previous studies suggesting that the well-documented population health benefits of comprehensive smoke-free legislation appear to extend to reducing hospital admissions for childhood asthma.
KEY WORDS: smoke-free legislation, hospital admissions, asthma
What’s Known on This Subject:
A small number of studies have found that the introduction of smoke-free legislation has been associated with a reduction in hospital admissions and emergency department visits for asthma.
What This Study Adds:
The implementation of smoke-free legislation in England was associated with an immediate 8.9% reduction in hospitalizations for asthma along with a decrease of 3.4% per year.
Comprehensive smoke-free legislation covering all enclosed public places and workplaces was implemented in England on July 1, 2007. This legislation has resulted in substantial population health gain, including reductions in workplace exposure to secondhand smoke (SHS),1 increased smoking quit rates,2 and decreased hospital admissions for acute myocardial infarction.3,4
A small number of studies conducted in North America have found that making public places and workplaces smoke-free reduces hospital admissions and emergency department visits for asthma.5–7 A Scottish study also found that the introduction of comprehensive smoke-free legislation in March 2006 was associated with a reduction in hospital admissions for childhood asthma.8 These findings are consistent with evidence that SHS exposure increases the incidence and severity of childhood asthma9 and that smoke-free legislation is associated with reductions in SHS exposure in the home.10,11
This study examines whether the implementation of smoke-free legislation in England on July 1, 2007, covering virtually all enclosed public places and workplaces, was associated with a change in hospital admissions for childhood asthma. Because some studies suggest that this legislation may be associated with lower reductions in SHS exposure in poorer households,12 we also examine whether changes in asthma admissions differed by socioeconomic status (SES).
Methods
We obtained an extract of all nonplanned (emergency) hospital admissions for childhood asthma between April 1, 2002 and November 30, 2010 from Hospital Episode Statistics (HES). HES is the national administrative database for hospital activity in England and contains data on all admissions and outpatient appointments performed for the National Health Service, including patients whose treatment is funded by the service but performed in private hospitals.13 We identified all nonplanned admissions with a principal diagnosis of asthma based on an International Classification of Diseases, 10th Revision, code of J45 or J46. This procedure excluded admissions in which asthma was coded as a secondary diagnosis and was not the presenting complaint.
Denominator data for each study year were midyear population estimates derived from census data published by the Office for National Statistics. These contained the age and gender breakdown for each Middle Layer Super Output Area (MSOA) in England. MSOAs are a geographic area designed for the collection and publication of small area statistics. There are 6780 MSOAs in England with an average population of 7200, and information on each admitted patient’s MSOA is available in HES.
We divided children into preschool (0–4 years) and school age (5–14 years) groups to reflect their different levels of SHS exposure in the home and public places. (Younger children are mainly exposed to SHS in the home whereas school-age children are also exposed to SHS in public places.14) Children were classified into neighborhood socioeconomic status quintiles, geographic location (urban/rural), and English region based on the MSOA in which they reside. Neighborhood socioeconomic status was assigned using the Index of Multiple Deprivation 2007,15 based on the mid-2010 estimate. We used the Office for National Statistics classification for urban and rural (in which MSOAs with >10 000 residents were urban).
We used an interrupted time series negative binomial regression model to assess the impact of the smoke-free legislation. While taking into account the underlying time trend, this model estimates both the immediate change and change in time trend after policy implementation. We include a dummy variable coded as 0 for the period before and 1 after implementation of the legislation in July 2007 and a continuous variable set to 0 through July 2007, then equal to the number of years since the legislation took effect. The model also included time throughout the study period to capture any long-term secular trend, seasonal effect (dummy variable for each month), age (a categorical variable for age 0–4 and 5–14 years), gender, national quintile of sociodemographic status (with the least deprived area as reference group), geographic location (urban/rural), and English region (with London as the reference group). The model produces an admission rate ratio, which is the ratio of the actual admission rate in relation to the rate projected by the underlying trend. We tested for nonlinearity of the time trend, which produced a nonsignificant result, suggesting that a linear model gave an appropriate fit to the data.
We estimated the number of admissions prevented in the 3 years after implementation of the law by estimating the number of admissions if there were no legislation (the counterfactual) using the coefficients estimated in the model using all the data but setting the law dummy and time after the law variables to 0 for the whole time period, then adding the differences in number of admissions each month between the actual admissions and counterfactual estimate.
In addition, to examine whether there was a differential effect of this legislation in different population groups, we conducted subgroup analyses stratified on age group, gender, quintile of neighborhood socioeconomic status, urban or rural residence and English region using the same negative binomial regression analysis, with the stratification variable dropped. We separately ran our main model with interaction terms between smoke-free legislation and each predictor. We do not present the findings because they were substantially unchanged from our subgroup analysis. We analyzed the data using Stata 11.
Results
There were 217 381 hospital admissions for childhood asthma during the 8.5-year study period, evenly distributed between preschool (50.1%) and school-age children (49.9%). The number of admissions was higher in boys (63.4%) than girls (36.6%). Most admissions occurred in children living in urban locations (86.5%), and there were a higher number of admissions in children living in the most deprived areas.
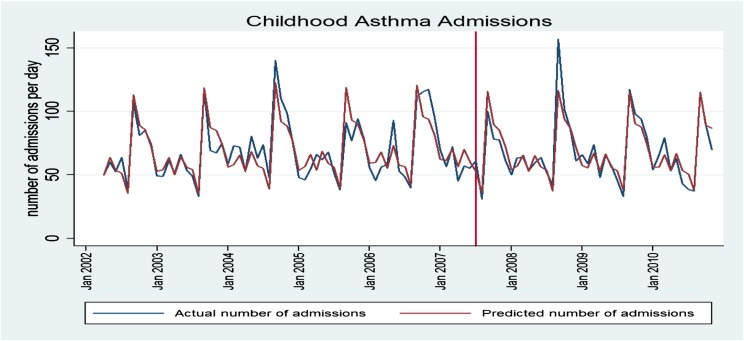
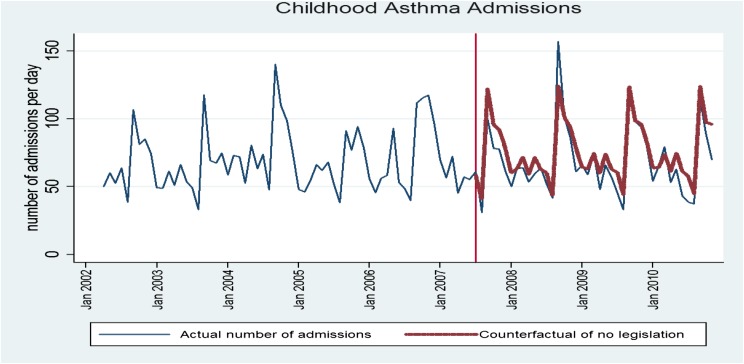
Mean daily childhood asthma admissions during each month of the study period are presented in Fig 1. Admissions peaked during autumn (from September to December), a pattern previously reported in England.16 Figure 1 also compares the predicted estimate with the actual counts using the full model. The close approximation of the actually and predicted value demonstrates that the model provides an accurate fit of the time series data. Figure 2 compares the actual number of admissions with the counterfactual (ie, predicted) admission rate had there been no law.
FIGURE 1.
Mean daily childhood asthma admissions during each month of the study period. Vertical line indicates implementation of smoke-free legislation in July 2007.
FIGURE 2.
Mean daily childhood asthma admissions during each month of the study period (actual vs counterfactual if there was no legislation).
Before the implementation of the legislation, there was a mean increase in the admission rate for asthma of 2.2% per year (adjusted rate ratio 1.02; 95% confidence interval [CI]: 1.02–1.03; Table 1). After implementation of the legislation, there was a significant immediate change in the admission rate of −8.9% (adjusted rate ratio 0.91; 95% CI: 0.89–0.93) and change in time trend of −3.4% per year (adjusted rate ratio 0.97; 95% CI: 0.96–0.98). Overall, the legislation was associated with a net 12.3% reduction of hospital admissions for childhood asthma in the first year. Using the method described earlier, we estimate that the legislation was associated with a reduction of 6802 hospital admissions in the first 3 years after implementation.
TABLE 1.
Smoke-free Legislation and Hospital Admission Rates for Childhood Asthma: Multivariate Analysis
| Admission Rate Ratios | 95% CI | |
|---|---|---|
| Time (y) | 1.02 | (1.02–1.03) |
| Smoke-free law | 0.91 | (0.89–0.94) |
| Time after smoke-free law (y) | 0.97 | (0.96–0.98) |
| Age group (preschool as reference group) | ||
| School age | 0.50 | (0.50–0.51) |
| Gender (Male as reference group) | ||
| Female | 0.63 | (0.63–0.64) |
| Location (Urban as reference group) | ||
| Rural | 1.14 | (1.12–1.16) |
| SES (the least deprived as reference group) | ||
| Quintile 2 | 1.13 | (1.11–1.15) |
| Quintile 3 | 1.33 | (1.31–1.36) |
| Quintile 4 | 1.55 | (1.52–1.58) |
| Quintile 5 (the most deprived) | 1.80 | (1.76–1.83) |
| Month (January as reference group) | ||
| February | 0.96 | (0.93–0.99) |
| March | 1.17 | (1.13–1.20) |
| April | 0.92 | (0.90–0.95) |
| May | 1.18 | (1.15–1.21) |
| June | 0.97 | (0.95–1.00) |
| July | 0.98 | (0.95–1.01) |
| August | 0.72 | (0.69–0.74) |
| September | 1.94 | (1.89–1.99) |
| October | 1.56 | (1.52–1.60) |
| November | 1.48 | (1.44–1.52) |
| December | 1.31 | (1.28–1.35) |
| Region (London as reference) | ||
| Northeast | 1.36 | (1.32–1.40) |
| Northwest | 1.58 | (1.54–1.61) |
| Yorkshire and Humber | 1.16 | (1.13–1.19) |
| East Midlands | 1.02 | (0.99–1.04) |
| West Midlands | 1.24 | (1.21–1.27) |
| East of England | 0.95 | (0.93–0.97) |
| Southeast coast | 1.13 | (1.10–1.16) |
| South central | 1.01 | (0.98–1.04) |
| Southwest | 1.13 | (1.10–1.15) |
Our stratified analyses (Table 2) indicate that the introduction of smoke-free legislation resulted in similar reductions in asthma admissions among children from different age, gender, and socioeconomic status groups and among those living in different geographic locations (urban vs rural). There were significant reductions in asthma admissions in all English regions.
TABLE 2.
Smoke-Free Legislation and Hospital Admission Rates for Childhood Asthma; Stratified Subgroup Analysis
| Smoke-Free Law | 95% CI | Time After Smoke-Free Law (per y) | 95% CI | |
|---|---|---|---|---|
| Sex | ||||
| Male | 0.90 | (0.87–0.93) | 0.96 | (0.95–0.98) |
| Female | 0.93 | (0.90–0.96) | 0.97 | (0.95–0.98) |
| Age group | ||||
| Preschool | 0.94 | (0.91–0.97) | 0.97 | (0.95–0.98) |
| School age | 0.88 | (0.86–0.91) | 0.96 | (0.95–0.97) |
| Area | ||||
| Urban | 0.91 | (0.89–0.94) | 0.97 | (0.96–0.98) |
| Rural | 0.91 | (0.87–0.96) | 0.96 | (0.94–0.98) |
| SES | ||||
| Quintile 1 (least deprived) | 0.94 | (0.89–0.99) | 0.96 | (0.93–0.98) |
| Quintile 2 | 0.91 | (0.87–0.96) | 0.97 | (0.95–0.99) |
| Quintile 3 | 0.86 | (0.82–0.90) | 0.97 | (0.95–0.99) |
| Quintile 4 | 0.92 | (0.87–0.96) | 0.96 | (0.94–0.98) |
| Quintile 5 (most deprived) | 0.93 | (0.89–0.98) | 0.96 | (0.94–0.98) |
| Region | ||||
| Northeast | 0.90 | (0.82–0.97) | 0.99 | (0.96–1.03) |
| Northwest | 0.93 | (0.88–0.98) | 0.99 | (0.96–1.02) |
| Yorkshire and Humber | 0.90 | (0.84–0.96) | 0.97 | (0.94–0.99) |
| East Midlands | 1.01 | (0.94–1.09) | 0.92 | (0.89–0.95) |
| West Midlands | 0.92 | (0.86–0.99) | 1.02 | (0.99–1.05) |
| East of England | 0.91 | (0.85–0.98) | 0.99 | (0.96–1.03) |
| London | 0.89 | (0.84–0.95) | 0.98 | (0.95–1.01) |
| Southeast coast | 0.82 | (0.76–0.88) | 0.95 | (0.92–0.99) |
| South central | 0.99 | (0.91–1.07) | 0.89 | (0.86–0.93) |
| Southwest | 0.88 | (0.83–0.94) | 0.90 | (0.87–0.93) |
All results based on full multivariate model except stratifying variable
Discussion
Smoke-free legislation in England, covering virtually all enclosed public places and workplaces, was associated with an immediate 8.9% reduction in hospitalizations for asthma along with an annual decrease of 3.4% per year, resulting in a reduction of >6802 admissions during the first 3 years after implementation. The findings suggest immediate as well as cumulative benefits over time applying across age, gender, SES, and geographic strata we studied.
Our findings are consistent with those from previous studies conducted in the United Kingdom and North America. The introduction of comprehensive smoke-free legislation in Scotland in April 2006 was associated with an 18.2% reduction in the annual rate of childhood asthma admissions.8 As in our study, the magnitude of the reduction did not differ by childhood characteristics, including age, gender, SES, or geographic location. A 22% reduction in asthma admissions (across all age groups) was identified in Arizona counties with no previous restrictions after the introduction of a comprehensive statewide smoking ban in public places in May 2007.5 The extension of smoke-free legislation to cover restaurants was associated with a significant additional decline in hospital admissions for asthma in Toronto.6 After taking the secular trends into account, emergency department visits for asthma declined by 22% in Lexington-Fayette County, Kentucky, after the introduction partial smoking ban in public places.7
The decline in asthma admissions identified in this and previous studies are likely due to reductions in SHS exposure among children in their homes associated with the introduction of smoke-free legislation. We had no data on changes in SHS exposure or cotinine levels in our sample, but health survey data from England suggest that the introduction of smoke-free legislation was associated with accelerated reductions in cotinine-validated SHS exposure in children17 and an increase in the proportion of smoke-free homes and cars.18 These findings are consistent with data from the United States, Ireland, France, Germany, the Netherlands, and Scotland.10,11,19 This suggests that our findings may be generalizable to these and other settings that have implemented comprehensive smoke-free legislation covering virtually all enclosed public places and workplaces . The impact of smoke-free legislation on differences in household SHS exposure in children between affluent and deprived households remains unclear. A Scottish study found higher absolute reductions in cotinine levels in children from lower SES households after the legislation.20 A similar study conducted in Wales found that associated reductions in SHS exposure were limited to children from higher SES households.12
In the absence of a control group, we cannot confirm that the reduction in hospital admissions was solely due to the implementation of smoke-free legislation. Furthermore, our model assumes a linear secular trend in the prepolicy period (and a different linear trend after the law). This regression model cannot distinguish between the effect of the law and other external influences affecting asthma incidence and exacerbations. These may include the introduction of new therapies and other strategies to improve asthma management. However, as far as we are aware, there was no major policy in England implemented concurrently with this legislation that could explain the sudden and substantial reduction in the rate of hospital admissions seen. Although leukotriene antagonists were introduced during the study period, this is unlikely to influence our findings substantially because prescribing rates increased gradually, and only a small percentage (<10%) of children in the United Kingdom with asthma were prescribed these medications when smoke-free legislation was introduced.21 Our models adjust for seasonality (month) and thus implicitly account for changes in admissions due to seasonal changes in air pollution. SES was assigned to admissions on the basis of an area deprivation score as individual-level measures, such as parental educational attainment, are not available in the HES data set. We did not have data on asthma deaths occurring outside of hospital. However, this number is likely to be small because the Scottish study (which, unlike us, had access to mortality data) identified only 5 deaths over a 9-year study period.8 HES are used extensively for epidemiologic and health services research.22,23 Although there are concerns about the accuracy of routinely collected data sets such as HES, they are continuously audited, and their quality and validity, including diagnostic coding, is high.22,24 Nonetheless, our findings may be subject to some bias due to changes in diagnostic coding over the study period, and we may have underestimated the effect of smoke-free legislation if coding of childhood asthma admissions improved over the study period. We are not aware of any major changes in how asthma is assessed and diagnosed over the study period.
Our findings confirm a small number of previous reports that the implementation of smoke-free legislation is associated with reductions in hospital admissions for childhood asthma. They add to an accumulating body of evidence of the substantial and equitable population health benefits gained by eliminating smoking from public places. The reductions in asthma admissions identified here are consistent with findings that smoke-free legislation may be associated with reductions SHS exposure in children due to an increase in voluntary smoke-free policies in the home or while traveling in a car.10,18 These results suggest that the legislation was associated with an important shift in social norms around exposing others to SHS in private as well as public places. Additional research is needed to better understand the relationship between the implementation of smoke-free legislation in public places and decreased SHS exposure in the home and other private places. Research should also seek to better characterize children who benefit most from the implementation of smoke-free legislation in terms of asthma severity, previous history of exacerbations, and SES and ethnic background.
The political declaration from the recent United Nations High Level Meeting on Non-Communicable Disease25 asks member states to accelerate implementation of the Framework Convention on Tobacco Control.26 Although the number of jurisdictions that have implemented Article 8 of the Framework on smoke-free public places is growing, most countries have no or limited legislation, and enforcement activities are generally weak. Data from the World Health Organization indicate that 89% of the world’s population lived without comprehensive smoke-free laws in 2009. Recent events in the Netherlands, where comprehensive smoke-free legislation covering the hospitality industry was introduced in 2008 but subsequently modified to exempt small bars, illustrates the importance of careful implementation, maintaining public support and guarding against tobacco industry lobbying.27
Conclusions
Our findings from a national study of a large population confirm those from a small number of previous studies suggesting that the well-documented population health benefits of comprehensive smoke-free legislation appear to extend to reducing hospital admissions for childhood asthma.
Acknowledgments
The Department of Primary Care & Public Health at Imperial College is grateful for support from the National Institute for Health Research Biomedical Research Centre Funding scheme, the National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care scheme, and the Imperial Centre for Patient Safety and Service Quality.
Glossary
- CI
confidence interval
- HES
Hospital Episode Statistics
- MSOA
middle layer super output area
- SES
socioeconomic status
- SHS
secondhand smoke
Footnotes
Dr Millett conceptualized and designed the study, supervised the statistical analysis, interpreted the findings, drafted the initial manuscript, and approved the final manuscript as submitted. Dr Lee undertook the statistical analysis, interpreted the findings, reviewed and revised the manuscript, and approved the final manuscript as submitted. Dr Laverty extracted and cleaned the data, interpreted the findings, reviewed and revised the manuscript, and approved the final manuscript as submitted. Dr Glantz supervised the statistical analysis, interpreted the findings, reviewed and revised the manuscript, and approved the final manuscript as submitted. Dr Majeed interpreted the findings, reviewed and revised the manuscript, and approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: Dr Millett is funded by the Higher Education Funding Council for England and the National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care scheme; Dr Laverty is funded by the National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care scheme; Dr Glantz is American Legacy Foundation Distinguished Professor in Tobacco Control; his work on this project was also supported by National Cancer Institute Grant CA-61021; and Dr Majeed has indicated he has no financial relationships relevant to this article to disclose.
FUNDING: No external funding.
References
- 1.Semple S, van Tongeren M, Galea KS, et al. UK smoke-free legislation: changes in PM2.5 concentrations in bars in Scotland, England, and Wales. Ann Occup Hyg. 2010;54(3):272–280 [DOI] [PubMed] [Google Scholar]
- 2.Hackshaw L, McEwen A, West R, Bauld L. Quit attempts in response to smoke-free legislation in England. Tob Control. 2010;19(2):160–164 [DOI] [PubMed] [Google Scholar]
- 3.Sims M, Maxwell R, Bauld L, Gilmore A. Short term impact of smoke-free legislation in England: retrospective analysis of hospital admissions for myocardial infarction. BMJ. 2010;340:c2161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mackay DF, Irfan MO, Haw S, Pell JP. Meta-analysis of the effect of comprehensive smoke-free legislation on acute coronary events. Heart. 2010;96(19):1525–1530 [DOI] [PubMed] [Google Scholar]
- 5.Herman PM, Walsh ME. Hospital admissions for acute myocardial infarction, angina, stroke, and asthma after implementation of Arizona’s comprehensive statewide smoking ban. Am J Public Health. 2011;101(3):491–496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Naiman A, Glazier RH, Moineddin R. Association of anti-smoking legislation with rates of hospital admission for cardiovascular and respiratory conditions. CMAJ. 2010;182(8):761–767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rayens MK, Burkhart PV, Zhang M, et al. Reduction in asthma-related emergency department visits after implementation of a smoke-free law. J Allergy Clin Immunol 2008;122(3):537–41.e3 [DOI] [PubMed] [Google Scholar]
- 8.Mackay D, Haw S, Ayres JG, Fischbacher C, Pell JP. Smoke-free legislation and hospitalizations for childhood asthma. N Engl J Med. 2010;363(12):1139–1145 [DOI] [PubMed] [Google Scholar]
- 9.Chilmonczyk BA, Salmun LM, Megathlin KN, et al. Association between exposure to environmental tobacco smoke and exacerbations of asthma in children. N Engl J Med. 1993;328(23):1665–1669 [DOI] [PubMed] [Google Scholar]
- 10.Mons U, Nagelhout GE, Allwright S, et al. Impact of national smoke-free legislation on home smoking bans: findings from the International Tobacco Control Policy Evaluation Project Europe Surveys [published online ahead of print Feburary 13, 2012]. Tob Control [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cheng K-W, Glantz SA, Lightwood JM. Association between smokefree laws and voluntary smokefree-home rules. Am J Prev Med. 2011;41(6):566–572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moore GF, Holliday JC, Moore LAR. Socioeconomic patterning in changes in child exposure to secondhand smoke after implementation of smoke-free legislation in Wales. Nicotine Tob Res. 2011;13(10):903–910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Honekamp I, Possenriede D. Redistributive effects in public health care financing. Eur J Health Econ. 2008;9(4):405–416 [DOI] [PubMed] [Google Scholar]
- 14.Ashley MJ, Ferrence R. Reducing children’s exposure to environmental tobacco smoke in homes: issues and strategies. Tob Control. 1998;7(1):61–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.The English Indices of Deprivation 2007. 2010. Available at: www.communities.gov.uk/publications/communities/indiciesdeprivation07. Accessed May 31, 2012
- 16.Fleming DM, Cross KW, Sunderland R, Ross AM. Comparison of the seasonal patterns of asthma identified in general practitioner episodes, hospital admissions, and deaths. Thorax. 2000;55(8):662–665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jarvis MJ, Sims M, Gilmore A, Mindell J. Impact of smoke-free legislation on children’s exposure to secondhand smoke: cotinine data from the Health Survey for England. Tob Control. 2012;21(1):18–23 [DOI] [PubMed] [Google Scholar]
- 18.Lee JT, Glantz SA, Millett C. Effect of smoke-free legislation on adult smoking behaviour in England in the 18 months following implementation. PLoS ONE. 2011;6(6):e20933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Akhtar PC, Haw SJ, Currie DB, Zachary R, Currie CE. Smoking restrictions in the home and secondhand smoke exposure among primary schoolchildren before and after introduction of the Scottish smoke-free legislation. Tob Control. 2009;18(5):409–415 [DOI] [PubMed] [Google Scholar]
- 20.Akhtar PC, Haw SJ, Levin KA, Currie DB, Zachary R, Currie CE. Socioeconomic differences in second-hand smoke exposure among children in Scotland after introduction of the smoke-free legislation. J Epidemiol Community Health. 2010;64(4):341–346 [DOI] [PubMed] [Google Scholar]
- 21.Thomas M, Murray-Thomas T, Fan T, Williams T, Taylor S. Prescribing patterns of asthma controller therapy for children in UK primary care: a cross-sectional observational study. BMC Pulm Med. 2010;10:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Campbell SE, Campbell MK, Grimshaw JM, Walker AE. A systematic review of discharge coding accuracy. J Public Health Med. 2001;23(3):205–211 [DOI] [PubMed] [Google Scholar]
- 23.Bottle A, Millett C, Khunti K, Majeed A. Trends in cardiovascular admissions and procedures for people with and without diabetes in England, 1996-2005. Diabetologia. 2009;52(1):74–80 [DOI] [PubMed] [Google Scholar]
- 24.Burns EM, Rigby E, Mamidanna R, et al. Systematic review of discharge coding accuracy. J Public Health (Oxf). 2012;34(1):138–148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.UN General Assembly. Draft resolution: Political Declaration of the High-level Meeting of the General Assembly on the Prevention and Control of Non-communicable Diseases; September 16, 2011. Available at: www.un.org/en/ga/ncdmeeting2011/pdf/NCD_draft_political_declaration.pdf. Accessed December 18, 2012 [Google Scholar]
- 26.World Health Organization (WHO). WHO Framework Convention on Tobacco Control. Geneva, Switzerland: WHO; 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gonzalez M, Glantz SA. Failure of policy regarding smoke-free bars in the Netherlands. Eur J Public Health. 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]