Abstract
OBJECTIVE:
To determine the residual physical disability after inpatient rehabilitation for children 7 to 18 years old with traumatic injuries.
METHODS:
This was a retrospective cohort study of patients aged 7 to 18 years who underwent inpatient rehabilitation for traumatic injuries from 2002 to 2011. Patients were identified from the Uniform Data System for Medical Rehabilitation. Injuries were captured by using standardized Medicare Inpatient Rehabilitation Facility Patient Assessment Instrument codes. Functional outcome was measured with the Functional Independence Measure (FIM) instrument. A validated, categorical grading system of the FIM motor items was used, consisting of clinically relevant levels of physical achievement from grade 1 (need for total assistance) to grade 7 (completely independent for self-care and mobility).
RESULTS:
A total of 13 798 injured children underwent inpatient rehabilitation across 523 facilities during the 10-year period. After a mean 3-week length of stay, functional limitations were reduced, but children still tended to have residual physical disabilities (median admission grade: 1; median discharge grade: 4). Children with spinal cord injuries, either alone or in combination with other injuries, had lower functional grade at discharge, longer lengths of stay, and more comorbidities at discharge than those with traumatic brain injuries, burns, and multiple injuries (P < .0001 for all comparisons).
CONCLUSIONS:
Children had very severe physical disability on admission to inpatient rehabilitation for traumatic injuries, and those with spinal cord injuries had persistent disability at discharge. These traumatic events during critical stages of development may result in a substantial care burden over the child’s lifespan.
KEY WORDS: disability, injury, rehabilitation, trauma, functional outcomes
What's Known on This Subject:
Outcomes analyses after trauma reveal long-term disability but are limited to specific injuries, older data, or all ages combined. There are no contemporary assessments of physical disability among children after inpatient rehabilitation for a wide range of traumatic injuries.
What This Study Adds:
This is the first contemporary study to describe the physical disability of a large pediatric cohort after inpatient rehabilitation for various injuries. After a mean 21-day inpatient rehabilitation stay, significant reductions in functional disability were achieved across injury mechanisms.
Although injury remains the leading cause of death for children aged >1 year in the United States,1 the overall survival rate of moderate to severe pediatric trauma is >95%.2,3 These nonfatal, yet serious injuries can have significant short- and long-term consequences on functionality and quality of life. It is critical to understand the epidemiology of trauma-related disability to improve prevention, acute care, and rehabilitation of these injuries. The ultimate objective of rehabilitation for injured children is to maximize function and enable return to their home, school, and community.4 Functional status provides a practical assessment that is used to develop goals and treatment plans for rehabilitation.5–7 A focus on functional outcome is valuable because improvements will enhance the child’s capacity to participate meaningfully in their natural home, school, and community environments.
Previous studies have examined long-term outcomes after pediatric injury. These have used large, older trauma databases,8,9 older versions of rehabilitation databases,10 and/or were focused on specific injuries such as traumatic brain injury (TBI).11–14 However, these previous studies were limited by small sample sizes; restricted injury diagnoses or mechanisms; absent disability assessments after inpatient rehabilitation; or a lack of detailed injury data, clinically relevant outcomes data, or a pediatric focus.
Although quantification of long-term disability and quality of life after trauma is important to injury prevention researchers, acute care providers, and rehabilitation specialists, no current estimates are available from a contemporary, large cohort of injured pediatric patients that describe the physical functionality at the time of reintegration into society. Therefore, the aim of this study was to describe the distribution of physical disability among a large sample of children and adolescents who underwent inpatient rehabilitation for a wide range of disabling injuries by using a practical and clinically relevant grading system.
Methods
Design, Setting, and Population
This was a retrospective cohort study of patients identified in the Uniform Data System for Medical Rehabilitation (UDSMR) database. The UDSMR is a nonprofit data collection and analysis service associated with the State University of New York at Buffalo.15 The UDSMR maintains the world’s largest database for adult and pediatric medical rehabilitation outcomes, with >829 rehabilitation centers currently contributing data, representing ∼72% of the 1152 Centers for Medicare & Medicaid Services designated for inpatient rehabilitation facilities in the United States. Inpatient evaluation of each patient in the UDSMR is conducted by using the Inpatient Rehabilitation Facility Patient Assessment Instrument (IRF-PAI)16 developed by the Centers for Medicare & Medicaid Services. The IRF-PAI includes demographic information (age, gender, and race/ethnicity), hospitalization and diagnostic information (length of stay [LOS], payer, impairment codes, clinical diagnoses from the International Classification of Diseases, Ninth Revision [ICD-9] codes), and functional status via the Functional Independence Measure (FIM) instrument. All UDSMR patients aged 7 to 18 years who underwent trauma-related rehabilitation from 2002 to 2011 were included in the analysis. This age range was selected because the FIM instrument has only been validated for individuals aged ≥7 years. The sample was further restricted to patients who completed inpatient rehabilitation for an acute injury event, excluding those who had a readmittance to rehabilitation.
Exposures
The individual injuries for each patient were identified by using the UDSMR center-assigned impairment codes. There are 20 trauma-related impairment codes in the UDSMR database. The impairment codes are assigned on admission by the rehabilitation center according to each injury or injuries for which the patient is primarily requiring rehabilitation, as categorized according to the IRF-PAI.16 Codes were grouped into the following 11 categories for the purposes of this analysis: TBI, TBI and multiple fracture/amputation, TBI and spinal cord injury (SCI), quadriplegia (complete), quadriplegia (incomplete or unspecified), paraplegia (complete), paraplegia (incomplete or unspecified), other SCI, SCI and multiple fracture/amputation, burns, and other multiple trauma. These 11 categories were further collapsed into 4 categories: TBI, quadriplegia, paraplegia, or other.
Outcomes
Functional status of patients, the primary outcome of interest, was assessed by using the FIM instrument,17,18 which has previously been used to evaluate trauma-related disability at short- and long-term intervals in children.9,19,20 The UDSMR database includes FIM measurements at 2 time points: at the time of admission to the rehabilitation hospital and at the time of discharge. FIM is a commonly used measure to assess patient progress, outcome, and disability that is composed of 18 items which express 2 primary domains of related function referred to as motor (which combines self-care, sphincter control, transfers, and locomotion functions) and cognitive (which combines communication and social cognition).21 The absolute motor FIM scores range from 13 (full physical dependence) to 91 (full physical independence). The absolute cognitive FIM score ranges from 5 (full cognitive disability) to 31 (full cognitive independence). Motor FIM scores have been previously categorized into a clinically relevant grading22 system, which has been validated in a variety of settings for assorted purposes.23,24 Explicit grade definitions were presented in tabular form previously.22
Given the importance of physical functionality after severe injury, the primary outcome of this analysis was discharge physical grade based on the 13 motor items. The categorical grades of physical disability ranged from grade 1 (need for total assistance in multiple physical self-care tasks such as eating, bathing, dressing, bowel and bladder management, and walking [heaviest care burden]) to grade 7 (able to complete all physical self-care and mobility tasks without difficulty, safety issues, or need for assistive device [full functional independence]).22 Each grade defines a distinct set of thresholds for each physical activity that the child must, by definition, meet or exceed. By placing a ceiling on the maximum amount of assistance a child can require for each task and still be at a particular grade, grade thresholds convey the types of problems the child and his or her caregivers will experience in the transition from leaving the rehabilitation hospital and reentering the home and school system. Knowledge of the grade makes support needed and challenges experienced by these broad subpopulations of injured children more transparent, thus helping to establish clinical and support service care planning, coordination, and tracking.
Additional analyses were performed by examining the prevalence of medical comorbidities for injured patients via ICD-9 codes. Standard ICD-9 categories were used to group individual codes. The database does not differentiate between preexisting medical comorbidities and those acquired during rehabilitation.
Statistical Methods and Data Analysis
Standard descriptive statistics were used to summarize demographic variables, injury characteristics, and outcome scores. Derived variables included the mean delta grade (ie, the individual patients’ average grade change from admission to discharge). A paired t test was used to compare these mean delta admission and discharge grades within each injury impairment code. Univariate analysis of variance was used to compare LOS across impairment codes. The 2-sample t test was also used to compare LOS between patients with and without an SCI. The LOS change over time (years) was examined by using the Kruskal-Wallis test. The association between discharge grade and average medical comorbidities was assessed by using Spearman’s coefficient. The χ2 test was used to compare the proportion of medical comorbidities for the major injury subgroups.
Results
From 2002 to 2011, there were 13 798 patients aged 7 to 18 years who completed trauma-related inpatient rehabilitation for acute injuries, representing 523 of the 829 contributing facilities. Table 1 displays the demographic characteristics of the overall sample. The majority of the sample was older, male, and white/non-Hispanic, with private health insurance.
TABLE 1.
Demographic and Rehabilitation-Related Characteristics of the Sample
| Characteristic | Total (N = 13 798) |
|---|---|
| Age at the start of rehabilitation, y | 16.2 ± 2.0 |
| Age, y | |
| 7–9 | 274 (2.0) |
| 10–12 | 465 (3.4) |
| 13–15 | 2487 (18.0) |
| 16–18 | 10 571 (76.6) |
| Gender | |
| Male | 9152 (66.4) |
| Female | 4637 (33.6) |
| Race/ethnicity | |
| White, non-Hispanic | 9705 (71.7) |
| Black, non-Hispanic | 1716 (12.7) |
| Hispanic/Latino | 1565 (11.6) |
| Other | 550 (4.1) |
| Primary payer | |
| Private | 9424 (68.3) |
| Public | 3151 (22.8) |
| Other | 1223 (8.9) |
| Admission to rehabilitation from | |
| Acute unit of another facility | 7840 (56.8) |
| Acute unit of own facility | 5391 (39.1) |
| Other | 560 (4.1) |
| Discharge living setting | |
| Home | 12 334 (89.4) |
| Acute or subacute care | 1169 (8.5) |
| Rehabilitation facility | 222 (1.6) |
| Died | 4 (0.03) |
| Other | 69 (0.5) |
Data are presented as mean ± SD or n (%).
Figure 1 shows the distribution of admission and discharge grades for 4 subgroups: TBI, quadriplegia, paraplegia, and other injuries. Although most children at admission to rehabilitation were at grade 1, by discharge the overall sample improved in functional independence with the most frequent grade of 4, and results were distributed across all 7 grades. This overall improvement was seen more notably in patients without SCI. Table 2 shows the median admission and discharge grades with interquartile ranges, the average difference between the admission and discharge grade, and the mean LOS for the 11 grouped impairment codes. Overall, TBI accounted for the largest proportion of children. SCI, either partial, complete, alone, or in combination with other injuries, accounted for 21.6% of the children. Across all diagnoses, children had uniformly poor functional status on admission to inpatient rehabilitation. Although nearly all injury types demonstrated improvements in grade at discharge from rehabilitation (P < .0001 for each), children who had SCIs (particularly those with complete cord dysfunction) had more severe discharge disability compared with those with TBIs, burns, and multiple injuries. Children who had isolated SCI or SCI with another injury had longer LOS when compared with those without SCI (P < 0.0001). Additional analyses demonstrated a slight decrease in the median LOS over time (15 days in 2002 to 13 days in 2011; P = .02), with the most significant difference found in those with discharge grade 1 (30 days in 2002 to 23 days in 2011; P < .001). In contrast, patients who had TBIs had an increased LOS over time (27 days in 2002 to 34 days in 2011; P < .01). Other analyses of children who had isolated TBIs revealed that younger children (ages 7–9 years) had less average recovery (mean grade improvement of 1.5 from admission to discharge, and median discharge grade of 3) compared with those aged 10 to 18 years (mean grade improvement of 2.2 from admission to discharge, and median discharge grade of 4).
FIGURE 1.
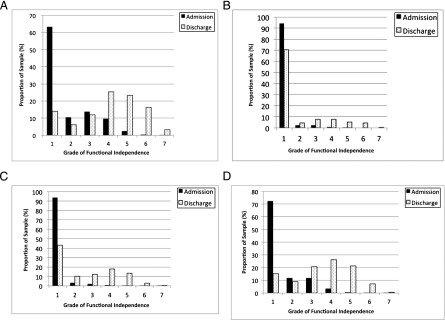
The proportion of the study population at each functional independence grade at admission and discharge from inpatient rehabilitation. Disability grades ranged from grade 1 (need for total assistance in multiple physical self care tasks) to grade 7 (full functional independence). A, TBI (n = 6297); B, quadriplegia (n = 946); C, paraplegia (n = 1244); D, other injuries (n = 5311).
TABLE 2.
Distribution of Admission and Discharge Grades for Functional Independence and Length of Inpatient Rehabilitation
| Injury Impairment Code | N | % | Median Admission Grade | IQR | Median Discharge Grade | IQR | Mean, Paired Difference Between Admission and Discharge Gradea | Mean LOS in Daysb |
|---|---|---|---|---|---|---|---|---|
| TBI | 6297 | 45.6 | 1 | 1–3 | 4 | 3–5 | 2.2 | 20 |
| TBI + multiple fracture/amputation | 3001 | 21.8 | 1 | 1–1 | 4 | 1–4 | 2.2 | 17 |
| Other multiple trauma | 1379 | 10.0 | 1 | 1–1 | 4 | 1–3 | 2.0 | 11 |
| Paraplegia, complete | 683 | 5.0 | 1 | 1–1 | 1 | 1–4 | 1.2 | 31 |
| Paraplegia, incomplete or unspecified | 561 | 4.1 | 1 | 1–1 | 3 | 1–1 | 1.8 | 23 |
| Quadriplegia, incomplete or unspecified | 532 | 3.9 | 1 | 1–2 | 1 | 3–5 | 1.3 | 39 |
| Quadriplegia, complete | 414 | 3.0 | 1 | 1–3 | 1 | 2–5 | 0.1 | 53 |
| TBI + SCI | 330 | 2.4 | 1 | 1–1 | 3 | 1–4 | 1.5 | 30 |
| Other SCI | 244 | 1.8 | 1 | 1–2 | 4 | 3–5 | 2.4 | 14 |
| SCI + multiple fracture/amputation | 188 | 1.4 | 1 | 1–1 | 2 | 1–4 | 1.2 | 23 |
| Burns | 169 | 1.2 | 1 | 1–2 | 4 | 3–5 | 1.7 | 15 |
IQR, interquartile range.
P < .0001 for all individual mean, paired delta grades.
P < .0001 for LOS across various Impairment Codes.
Table 3 summarizes the differences in the proportion of medical conditions for the 4 groups of impairment codes: TBI, quadriplegia, paraplegia, and other injuries. Most notably, patients who had SCIs had more overall comorbidities (P < .0001) and a higher proportion of genitourinary and digestive system conditions but a smaller proportion of mental disorders than those without SCI (P < .0001).
TABLE 3.
Proportion of Individuals With Medical Comorbidities Within Each Injury Category
| Proportion of Medical Comorbidities | TBI | Quadriplegia, All Types | Paraplegia, All Types | Other Injuries | P |
|---|---|---|---|---|---|
| Mean no. of comorbidities per patient | 2.7 | 4.3 | 4.1 | 3.3 | <.0001 |
| Medical diagnosis code groups, % | |||||
| Infections and parasitic diseases | 3.4 | 5.6 | 5.3 | 3.5 | <.0001 |
| Endocrine, nutritional, and metabolic diseases, and immunity disorders | 3.6 | 2.8 | 2.1 | 4.0 | <.0001 |
| Diseases of blood and blood forming organs | 3.7 | 2.3 | 3.9 | 8.0 | <.0001 |
| Mental disorders | 16.6 | 6.3 | 7.8 | 13.4 | <.0001 |
| Diseases of the nervous system | 10.0 | 11.4 | 12.9 | 6.7 | <.0001 |
| Diseases of the sense organs | 4.8 | 0.4 | 0.4 | 2.7 | <.0001 |
| Diseases of the circulatory system | 3.5 | 4.0 | 3.2 | 3.3 | .08 |
| Diseases of the respiratory system | 6.2 | 6.8 | 3.9 | 5.9 | <.0001 |
| Diseases of the digestive system | 3.1 | 12.6 | 15.4 | 5.4 | <.0001 |
| Diseases of the genitourinary system | 3.3 | 14.9 | 16.8 | 5.2 | <.0001 |
| Diseases of the skin and subcutaneous tissue | 2.1 | 6.2 | 4.6 | 2.3 | <.0001 |
| Diseases of the musculoskeletal system and connective tissue | 5.1 | 5.2 | 5.6 | 5.7 | .06 |
| Symptoms, signs, and ill-defined conditions | 20.0 | 8.6 | 7.6 | 14.9 | <.0001 |
| Supplementary factors influencing health status | 14.5 | 12.9 | 10.6 | 19.0 | <.0001 |
| Total, % | 100.0 | 100.0 | 100.0 | 100.0 |
Table 4 displays the average number of medical comorbidities for each discharge functional grade. A lower discharge functional grade was associated with a greater number of average medical comorbidities, ranging from an average 4.1 comorbidities for a discharge grade of 1, to an average of 1.9 comorbidities for a discharge grade of 7 (Spearman r –0.99; P < .0001).
TABLE 4.
Average Medical Comorbidities per Patient by Functional Grade at Discharge From Rehabilitation
| Discharge Grade | 1 | 2 | 3 | 4 | 5 | 6 | 7 | Spearman’s Coefficient | P |
|---|---|---|---|---|---|---|---|---|---|
| Average medical comorbidities per patient | 4.1 | 3.4 | 3.1 | 3.0 | 2.8 | 2.6 | 1.9 | −0.99 | <.0001 |
Discussion
To the best of our knowledge, this is the first contemporary assessment of physical disability resulting from injuries among a large national cohort of children discharged from inpatient rehabilitation facilities over the past 10 years. Physical disability at admission was universally severe (median grade 1) across the diagnostic groups. After a mean LOS of 3 weeks, functional limitations were reduced at discharge, but children still tended to have residual physical disabilities (median grade 4), with greater disabilities remaining in patients with SCI (median grade 2). More medical comorbidities were associated with lower grades and with SCI.
For our study, ∼70% of injured children overall entered inpatient rehabilitation at grade 1, documenting a need for total assistance in any or all 13 motor FIM items at that time. This finding suggests that perhaps only the most severely affected children are being referred for inpatient rehabilitation. Overall, children improved by rehabilitation discharge; more than one-half the population achieved physical grade ≥4 and thus no longer had severe or moderate disabilities, whereas children with SCI had minimal to no recovery of physical functionality. New knowledge about the proportion of children who achieve (or exceed) each grade at discharge from rehabilitation has major implications for clinical and support service care planning, coordination, and tracking as children reenter the community after their injuries.
This study complements existing literature on outcomes after injury in children. Various analyses have used the National Pediatric Trauma Registry, a large, nonpopulation-based cohort of injured children treated in trauma centers between 1985 and 2001.8 Results using this database have described long-term outcomes of children with multitrauma,9 isolated TBI,20,25,26 and isolated SCI.27 These studies concluded that there was a burden of functional disability after pediatric trauma, rehabilitation may be underutilized, and there may be disparities in outcomes in disadvantaged children. One older study of 3815 children aged 0 to 21 years who had TBIs requiring inpatient rehabilitation found significant improvement in functionality, especially in those who had higher initial functional status and shorter time between injury and rehabilitation.10 A multicenter study of >300 children 5 to 15 years old with severe TBI from any mechanism demonstrated significant disability on multiple aspects of health-related quality of life scores, executive functioning, family burden, and emotional impact.12,28,29 Similarly, a more recent prospective multicenter study of >900 children ages 0 to 17 years with TBI and upper extremity injuries found that quality of life was lower for children with moderate or severe TBI, which was influenced by persistent symptoms such as headache and sleep disturbances.13,30,31 In another, more recent analysis examining >4400 children 7 to 14 years old with TBI, the authors found that children were more likely to have disability if the mechanism was motor vehicle–related or they also had severe fractures in addition to their TBI.20 In addition, a recent meta-analysis of 28 publications showed that severe TBI results in poor cognitive outcomes up to 2 years after injury.32 Another study of children aged 0 to 21 years who had SCIs demonstrated that long-term motor function depends on neurologic level and completeness of injury, with possible continued improvement after treatment.33 Finally, 2 recent analyses using the UDSMR examined children and adults 7 to 105 years old with TBI14 from 2000 to 2007 and SCI from 2002 to 2010.34 The goal was to provide benchmarking information and inform facility-level quality improvement. Outcomes included gain in absolute FIM scores during rehabilitation and FIM improvement over time. Similar to the current study, the authors found in both groups that LOS decreased over time while functional independence gains were stable. Because these were broad benchmarking studies, there were no subanalyses for pediatric age groups, inclusion of patients with non-TBI/SCI trauma, or use of clinically applicable functional grades.
Children in this cohort with SCI had more comorbidities, longer LOS, and lower functionality at discharge than those without. This was particularly evident in the quadriplegic patients, of whom 84% had a discharge grade ≤3. It is likely that these SCI patients do not regain physical function due to the inherent physiology of these injuries. Although SCI-related physical disability is high, even minimal improvement in functionality is beneficial to disabled patients and worth the cost of rehabilitation,35 and children may continue to regain additional motor function months to years after SCI.33,36 In addition, SCI patients have more medical comorbidities than non-SCI patients, including ventilator dependence, pulmonary complications, autonomic hyperreflexia, deep vein thrombosis, and orthopedic complications.36,37 It is important to consider that pediatric rehabilitation serves a wide range of purposes in addition to improving functionality, including postacute care of medical comorbidities, patient and caregiver adaptation to current state, and maximizing remaining potential for reintegration into the school, family, and community to return to lives that are meaningful and fulfilling.36,38–41
Low functionality at discharge was correlated with a number of comorbid medical conditions, with mental disorders as the most common system-specific comorbidity. This finding is consistent with existing literature demonstrating increased rates of and impairment from posttraumatic stress, anxiety, depression, and substance use in children who have severe trauma.42–45 Future study should explore in which populations these conditions are preexisting versus acquired, and how these conditions and other medical comorbidities affect LOS and gains in functionality across the acute care to rehabilitation spectrum.
Several study limitations should be noted. First, although the cohort included an overall small sample of younger children, it is likely representative of the most severely injured younger children, in particular those who have SCI, as these patients are the most likely to require inpatient rehabilitation. In addition, the brain continues to develop into the third decade of life,46 and the functional implications of trauma in adolescents may be distinct from that of young adults. Another limitation of the database is the infrequent documentation of ICD-9 E-codes that describe injury mechanism, which necessitated omission from this analysis. Certain mechanisms have been previously associated with injuries requiring higher levels of acute care and rehabilitation resources, in addition to distinct patterns of disability.47,48 An additional limitation is the lack of information surrounding premature discharge from inpatient rehabilitation. In particular, this information could bias the results if a systematic group of individuals with certain diagnoses or demographic characteristics were discharged before completing a standard inpatient rehabilitation regimen. Finally, the FIM only measures functionality and does not focus on quality of life, and this analysis was limited to physical disability. Although there is no current consensus about ideal outcome measurements, functional outcomes are broadly applicable, and the grading system has clinically meaningful relevance for goals and treatment plans.5–7,22
Conclusions
Children with severe injuries have poor functional status on admission to inpatient rehabilitation but most benefit substantially from their care. Those with SCI, however, have longer LOS, more comorbidities, and lower physical functionality at discharge. Many of these disabling injuries result in moderate or severe functional disability, which can confer a substantial care burden over the course of the child’s life span. Additional assessment of functionality from more specific patterns of injuries should be explored to more comprehensively understand these relationships. Future work should also consider tracking disabling injuries in children, from prehospital care, to emergency acute care, to intensive care, and then to rehabilitation to identify opportunities for improvement. Although there is a gradually developing body of literature on the epidemiology of disability after injury, relatively little is known about if or how acute and rehabilitation treatments influence short- and long-term functional outcomes. Additional considerations for research include potential risk factors for functional and quality of life outcomes, including racial and socioeconomic disparities, mechanism and severity of injury, access to medical and rehabilitation care, and preexisting or acquired comorbidities. Because the current results suggest that perhaps only the most severely affected children are being referred to inpatient rehabilitation, future studies should explore factors associated with decisions to admit to inpatient rehabilitation, and whether those less severely injured may benefit from such intensive therapy. To more comprehensively understand the complexities of disabling injuries in children, there has been a call for action to more robustly collect essential pediatric trauma outcomes data through multicenter research networks,49 in addition to suggestions for useful standardized outcome measures,50–52 rehabilitation quality of care measures,53 and rehabilitation research design strategies.54
Acknowledgments
The authors thank Paulette M. Niewczyk, MPH, PhD, and the staff at the UDSMR at the University of Buffalo, State University of New York, for use of the data, and Xuemei Zhang, MS, for assistance with data analysis.
Glossary
- FIM
Functional Independence Measure
- ICD-9
International Classification of Diseases, Ninth Revision
- IRF-PAI
Inpatient Rehabilitation Facility Patient Assessment Instrument
- LOS
length of stay
- SCI
spinal cord injury
- TBI
traumatic brain injury
- UDSMR
Uniform Data System for Medical Rehabilitation
Footnotes
Dr Zonfrillo conceptualized and designed the study, contributed to data analysis, interpreted the data, drafted the initial manuscript, critically reviewed the manuscript, and approved the final manuscript as submitted; Drs Durbin, Winston, and Stineman significantly contributed to study conception and design, interpreted the data, critically reviewed the manuscript, and approved the final manuscript as submitted; and Dr Zhao completed the initial analyses, critically reviewed the manuscript, and approved the final manuscript as submitted.
The views presented are those of the authors and not necessarily the views of the Academic Pediatric Association, the University of Pennsylvania, the National Science Foundation, Center for Child Injury Prevention Studies, The Children’s Hospital of Philadelphia, or the Uniform Data System for Medical Rehabilitation.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by the Academic Pediatric Association Young Investigators Award, the Thomas B. and Jeannette E. Laws McCabe Pilot Fund Award at the University of Pennsylvania, and the National Science Foundation Center for Child Injury Prevention Studies at The Children’s Hospital of Philadelphia.
References
- 1.Centers for Disease Control and Prevention, National Centers for Injury Prevention and Control. Ten leading causes of death and injury. Available at: www.cdc.gov/injury/wisqars/LeadingCauses.html. Accessed December 2, 2011
- 2.Burd RS, Madigan D. The impact of injury coding schemes on predicting hospital mortality after pediatric injury. Acad Emerg Med. 2009;16(7):639–645 [DOI] [PubMed] [Google Scholar]
- 3.Hakmeh W, Barker J, Szpunar SM, Fox JM, Irvin CB. Effect of race and insurance on outcome of pediatric trauma. Acad Emerg Med. 2010;17(8):809–812 [DOI] [PubMed] [Google Scholar]
- 4.Jaffe KM. Pediatric trauma rehabilitation: a value-added safety net. J Trauma. 2008;64(3):819–823 [DOI] [PubMed] [Google Scholar]
- 5.Long CE, Blackman JA, Farrell WJ, Smolkin ME, Conaway MR. A comparison of developmental versus functional assessment in the rehabilitation of young children. Pediatr Rehabil. 2005;8(2):156–161 [DOI] [PubMed] [Google Scholar]
- 6.Majnemer A. Focusing on function. Phys Occup Ther Pediatr. 2009;29(3):219–221 [DOI] [PubMed] [Google Scholar]
- 7.Niewczyk PM, Granger CV. Measuring function in young children with impairments. Pediatr Phys Ther. 2010;22(1):42–51 [DOI] [PubMed] [Google Scholar]
- 8.Tepas JJ, 3rd. The national pediatric trauma registry: a legacy of commitment to control of childhood injury. Semin Pediatr Surg. 2004;13(2):126–132 [DOI] [PubMed] [Google Scholar]
- 9.Aitken ME, Jaffe KM, DiScala C, Rivara FP. Functional outcome in children with multiple trauma without significant head injury. Arch Phys Med Rehabil. 1999;80(8):889–895 [DOI] [PubMed] [Google Scholar]
- 10.Rice SA, Blackman JA, Braun S, Linn RT, Granger CV, Wagner DP. Rehabilitation of children with traumatic brain injury: descriptive analysis of a nationwide sample using the WeeFIM. Arch Phys Med Rehabil. 2005;86(4):834–836 [DOI] [PubMed] [Google Scholar]
- 11.McCarthy ML, MacKenzie EJ, Durbin DR, et al. Children’s Health After Trauma Study Group . Health-related quality of life during the first year after traumatic brain injury. Arch Pediatr Adolesc Med. 2006;160(3):252–260 [DOI] [PubMed] [Google Scholar]
- 12.Sesma HW, Slomine BS, Ding R, et al. Executive functioning in the first year after pediatric traumatic brain injury. Pediatrics 2008;121(6). Available at: www.pediatrics.org/cgi/content/full/121/6/e1686 [DOI] [PubMed]
- 13.Rivara FP, Koepsell TD, Wang J, et al. Disability 3, 12, and 24 months after traumatic brain injury among children and adolescents. Pediatrics. 2011;128(5). Available at: www.pediatrics.org/cgi/content/full/128/5/e1129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Granger CV, Markello SJ, Graham JE, Deutsch A, Reistetter TA, Ottenbacher KJ. The uniform data system for medical rehabilitation: report of patients with traumatic brain injury discharged from rehabilitation programs in 2000-2007. Am J Phys Med Rehabil. 2010;89(4):265–278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Uniform Data System for Medical Rehabilitation (UDSMR). Available at: www.udsmr.org. Accessed December 15, 2011
- 16.Centers for Medicare & Medicaid Services. Inpatient Rehabilitation Facility (IRF) Patient Assessment Instrument (PAI). Available at: https://www.cms.gov/InpatientRehabFacPPS/04_IRFPAI.asp. Accessed March 29, 2012
- 17.Keith RA, Granger CV, Hamilton BB, Sherwin FS. The functional independence measure: a new tool for rehabilitation. Adv Clin Rehabil. 1987;1:6–18 [PubMed] [Google Scholar]
- 18.Hamilton BB, Granger CV, Sherwin FS, et al. A uniform national data system for medical rehabilitation. In: Fuhrer M, ed. Rehabilitation Outcomes: Analysis and Measurement. Baltimore, MD: Brookes; 1987:137–147 [Google Scholar]
- 19.Willis CD, Gabbe BJ, Butt W, Cameron PA. Assessing outcomes in paediatric trauma populations. Injury. 2006;37(12):1185–1196 [DOI] [PubMed] [Google Scholar]
- 20.Wechsler B, Kim H, Gallagher PR, DiScala C, Stineman MG. Functional status after childhood traumatic brain injury. J Trauma. 2005;58(5):940–949, discussion 950 [DOI] [PubMed] [Google Scholar]
- 21.Heinemann AW, Linacre JM, Wright BD, Hamilton BB, Granger C. Relationships between impairment and physical disability as measured by the functional independence measure. Arch Phys Med Rehabil. 1993;74(6):566–573 [DOI] [PubMed] [Google Scholar]
- 22.Stineman MG, Ross RN, Granger CV, Maislin G. Predicting the achievement of 6 grades of physical independence from data routinely collected at admission to rehabilitation. Arch Phys Med Rehabil. 2003;84(11):1647–1656 [DOI] [PubMed] [Google Scholar]
- 23.Jette DU, Warren RL, Wirtalla C. The relation between therapy intensity and outcomes of rehabilitation in skilled nursing facilities. Arch Phys Med Rehabil. 2005;86(3):373–379 [DOI] [PubMed] [Google Scholar]
- 24.Stineman MG, Kurichi JE, Kwong PL, et al. Survival analysis in amputees based on physical independence grade achievement. Arch Surg. 2009;144(6):543–551, discussion 552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Di Scala C, Osberg JS, Gans BM, Chin LJ, Grant CC. Children with traumatic head injury: morbidity and postacute treatment. Arch Phys Med Rehabil. 1991;72(9):662–666 [PubMed] [Google Scholar]
- 26.Haider AH, Efron DT, Haut ER, DiRusso SM, Sullivan T, Cornwell EE, 3rd. Black children experience worse clinical and functional outcomes after traumatic brain injury: an analysis of the National Pediatric Trauma Registry. J Trauma. 2007;62(5):1259–1262, discussion 1262–1263 [DOI] [PubMed] [Google Scholar]
- 27.Kokoska ER, Keller MS, Rallo MC, Weber TR. Characteristics of pediatric cervical spine injuries. J Pediatr Surg. 2001;36(1):100–105 [DOI] [PubMed] [Google Scholar]
- 28.Aitken ME, McCarthy ML, Slomine BS, et al. CHAT Study Group . Family burden after traumatic brain injury in children. Pediatrics. 2009;123(1):199–206 [DOI] [PubMed] [Google Scholar]
- 29.McCarthy ML, MacKenzie EJ, Durbin DR, et al. Children’s Health After Trauma Study Group . Health-related quality of life during the first year after traumatic brain injury. Arch Pediatr Adolesc Med. 2006;160(3):252–260 [DOI] [PubMed] [Google Scholar]
- 30.Tham SW, Palermo TM, Vavilala MS, et al. The longitudinal course, risk factors, and impact of sleep disturbances in children with traumatic brain injury. J Neurotrauma. 2012;29(1):154–161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Blume HK, Vavilala MS, Jaffe KM, et al. Headache after pediatric traumatic brain injury: a cohort study. Pediatrics. 2012;129(1). Available at: www.pediatrics.org/cgi/content/full/129/1/e31 [DOI] [PubMed] [Google Scholar]
- 32.Babikian T, Asarnow R. Neurocognitive outcomes and recovery after pediatric TBI: meta-analytic review of the literature. Neuropsychology. 2009;23(3):283–296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Allen DD, Mulcahey MJ, Haley SM, et al. Motor scores on the functional independence measure after pediatric spinal cord injury. Spinal Cord. 2009;47(3):213–217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Granger CV, Karmarkar AM, Graham JE, et al. The uniform data system for medical rehabilitation: report of patients with traumatic spinal cord injury discharged from rehabilitation programs in 2002-2010. Am J Phys Med Rehabil. 2012;91(4):289–299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dumas HM, Haley SM, Ludlow LH. Achieving a minimally important difference in physical function during pediatric inpatient rehabilitation. Int J Rehabil Res. 2008;31(3):257–260 [DOI] [PubMed] [Google Scholar]
- 36.Massagli TL. Medical and rehabilitation issues in the care of children with spinal cord injury. Phys Med Rehabil Clin N Am. 2000;11(1):169–182 [PubMed] [Google Scholar]
- 37.Vogel LC, Anderson CJ. Spinal cord injuries in children and adolescents: a review. J Spinal Cord Med. 2003;26(3):193–203 [DOI] [PubMed] [Google Scholar]
- 38.Zidek K, Srinivasan R. Rehabilitation of a child with a spinal cord injury. Semin Pediatr Neurol. 2003;10(2):140–150 [DOI] [PubMed] [Google Scholar]
- 39.Forsyth RJ. Back to the future: rehabilitation of children after brain injury. Arch Dis Child. 2010;95(7):554–559 [DOI] [PubMed] [Google Scholar]
- 40.Chevignard MP, Toure H, Brugel DG, Poirier J, Laurent-Vannier A. A comprehensive model of care for rehabilitation of children with acquired brain injuries. Child Care Health Dev. 2010;36(1):31–43 [DOI] [PubMed] [Google Scholar]
- 41.Garma SI, Kelly EH, Daharsh EZ, Vogel LC. Health-related quality of life after pediatric spinal cord injury. J Pediatr Psychol. 2011;36(2):226–236 [DOI] [PubMed] [Google Scholar]
- 42.Anderson CJ, Kelly EH, Klaas SJ, Russell H, Daharsh E, Vogel LC. Anxiety and depression in children and adolescents with spinal cord injuries. Dev Med Child Neurol. 2009;51(10):826–832 [DOI] [PubMed] [Google Scholar]
- 43.Zatzick DF, Jurkovich GJ, Fan MY, et al. Association between posttraumatic stress and depressive symptoms and functional outcomes in adolescents followed up longitudinally after injury hospitalization. Arch Pediatr Adolesc Med. 2008;162(7):642–648 [DOI] [PubMed] [Google Scholar]
- 44.Zatzick DF, Grossman DC. Association between traumatic injury and psychiatric disorders and medication prescription to youths aged 10-19. Psychiatr Serv. 2011;62(3):264–271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dasarathi M, Grace J, Kelly T, Forsyth R. Utilization of mental health services by survivors of severe paediatric traumatic brain injury: a population-based study. Child Care Health Dev. 2011;37(3):418–421 [DOI] [PubMed] [Google Scholar]
- 46.Groeschel S, Vollmer B, King MD, Connelly A. Developmental changes in cerebral grey and white matter volume from infancy to adulthood. Int J Dev Neurosci. 2010;28(6):481–489 [DOI] [PubMed] [Google Scholar]
- 47.Burd RS, Jang TS, Nair SS. Evaluation of the relationship between mechanism of injury and outcome in pediatric trauma. J Trauma. 2007;62(4):1004–1014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Haider AH, Crompton JG, Oyetunji T, et al. Mechanism of injury predicts case fatality and functional outcomes in pediatric trauma patients: the case for its use in trauma outcomes studies. J Pediatr Surg. 2011;46(8):1557–1563 [DOI] [PubMed] [Google Scholar]
- 49.Upperman JS, Burd R, Cox C, Ehrlich P, Mooney D, Groner JI. Pediatric applied trauma research network: a call to action. J Trauma. 2010;69(5):1304–1307 [DOI] [PubMed] [Google Scholar]
- 50.Alexander MS, Anderson KD, Biering-Sorensen F, et al. Outcome measures in spinal cord injury: recent assessments and recommendations for future directions. Spinal Cord. 2009;47(8):582–591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Winthrop AL. Health-related quality of life after pediatric trauma. Curr Opin Pediatr. 2010;22(3):346–351 [DOI] [PubMed] [Google Scholar]
- 52.Miller AC, Odenkirchen J, Duhaime AC, Hicks R. Common data elements for research on traumatic brain injury: pediatric considerations. J Neurotrauma. 2012;29(4):634–638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rivara FP, Ennis SK, Mangione-Smith R, et al. National Expert Panel for the Development of Pediatric Rehabilitation Quality Care Indicators. Quality of care indicators for the rehabilitation of children with traumatic brain injury. Arch Phys Med Rehabil. 2012;93(3):381–385.e9 [DOI] [PMC free article] [PubMed]
- 54.Barnett SD, Heinemann AW, Libin A, et al. Small N designs for rehabilitation research. J Rehabil Res Dev. 2012;49(1):175–186 [DOI] [PubMed] [Google Scholar]


