Abstract
The 113th Congress of the United States begins in January 2013. With each new Congress, there are many changes, not only in the faces of the newly elected, but also in the membership of committees and the staff serving the members. As agendas for the session are set, there is a resurgence of conflicting priorities. In the past, when these conflicts were resolved, children were rarely at the top of the list. Given the numerous pressing national issues, both domestic and foreign, the same trend will likely occur.
KEY WORDS: Congress, public policy, recommendations
Although <10% of the federal budget was spent on children at the start of the 111th Congress, spending on children increased significantly during the first session of the 112th Congress as a result of stimulus spending targeted to children and families but declined for the first time in 30 years during 2012 to 1.9% of the gross domestic product, the lowest level in a decade. As Congress deals with Medicare, Medicaid, Social Security, and debt reduction, further decline is expected.1
In 2008, the leadership of 5 major pediatric organizations developed recommendations designed to assist advocates for children and adolescents during the 2008 elections.2 This time, all advocates for children and adolescents are being asked to carry a strong, focused message to the members of Congress as they organize and set the national agenda for the next 2 years. Although the voices in this article speak to the various concerns within pediatrics, they speak with resounding unity regarding the need to place children prominently in the larger scope of national priorities.
American Academy of Pediatrics’ Priorities FOR OUR NATIONS’ CHILDREN
Robert W. Block, MD, FAAP, Past President, American Academy of Pediatrics
In 1898, in an address to the American Medical Association Section on Diseases of Children, J.P. Crozer Griffith, a pediatrician leader, remarked, “…what a change! How the profession throughout the country is awakening to the demands of the times!”3 He described our aim as pediatricians thusly: “so study (pediatrics), practice it, write of it, teach it, (and) work for it.” Pediatricians took Dr Griffith’s challenge to heart and tackled demands such as smallpox and infant nutrition.
And what are the demands of our time in 2012 and beyond?
The American Academy of Pediatrics (AAP) is working diligently, along with other organizations, to accomplish a host of important goals, including:
Preserving and protecting the important gains for children contained in the Patient Protection and Affordable Care Act (ACA).4
Educating policy makers about the importance of Children’s Hospital Graduate Medical Education (CHGME), and Medicare Graduate Medical Education (GME) funding, to allow appropriate training for our next generation of pediatricians and pediatric specialists, including pediatric surgeons.
Supporting passage of several bills relating to the US Food and Drug Administration that address safer and more appropriately labeled drugs for children, focus on the need to prepare for and avert critical drug shortages, and promote development of important medical devices for children.
Encouraging commercial insurers and Medicaid/State Children’s Health Insurance Program payers to appropriately pay for the Early Periodic Screening, Diagnosis, and Treatment Program, guided by the Bright Futures guidelines, and to pay for immunizations, mental health, developmental screening, and other work of pediatricians that is vital to the goal of producing healthy children.
Providing education tools and opportunities for pediatricians to continue their lifelong learning and meet the requirements for Maintenance of Certification.
Addressing both gender and generation differences in the structure and function of various models of pediatric practice, thus attempting to meet the needs of younger physicians.
Supplying critical health information technology to pediatricians and to the government agencies that monitor and control meaningful use, as well as informing vendors and users about best practices for using this technology.
There are a number of different pediatric practice landscapes that have developed over the past years and which continue to diversify the way health care is delivered to children. Many continue to choose to follow traditional general pediatrics in private practices; others choose to practice in integrated delivery systems, while still others choose to pursue either an academic/research subspecialty career or a clinical subspecialty practice. Pediatrics is now divided into office practice or hospitalist practice. The pediatric patient–centered medical home is becoming a team approach to care, led by 1 or more board-certified pediatricians working collaboratively with a host of other professionals, including nurses, pediatric nurse practitioners, physician assistants, behavior and developmental specialists, social workers, and many others. Some pediatricians practice in emergency departments and/or urgent care centers. Others choose to practice in federally qualified centers as well as other models of community health centers. Regardless of the practice setting, all pediatricians share a passion for maintaining and improving child health, a trait referred to as having the “soul” of a pediatrician.
Our collective future rests upon our ability to come together and shape it. We hope to continue with a unified voice for pediatrics because we are the voice of our patients, who cannot always speak for themselves. Judy Palfrey, MD, FAAP, a former AAP president, said that we must manage the future.5 Regardless of changing landscapes, our goal remains the health and welfare of all infants, children, adolescents, and young adults. Primary care and subspecialty pediatricians, as well as our colleagues in surgical specialties, will achieve success in advocating for the rights and needs of children if we coalesce around that mission.
Our dedication to the health of all children requires constant attention to new discoveries and studies of human ecology. In January 2012, the AAP published 2 landmark articles, a policy statement and a technical report, addressing the issue of toxic stress and the lifelong consequences of serious adversities occurring during childhood.6,7 The articles addressed newly recognized biology describing the changes in brain and body chemistry caused by toxic stress. This work supports the conclusions of the previous Adverse Childhood Experiences8 work and lends biologic support to the economic equation for success developed by Professor James Heckman,9 simply stating that this country’s largest return on investment will derive from appropriate initial investments in early childhood health and education. These works are the substrate on which the AAP bases our current admonition: although not all children are able to become adults, it is certainly true that all adults once were children.
We must act on facts supporting the contention that lifelong health begins, and is firmly rooted, in childhood. The AAP Agenda for Children focuses on 2 issues (early brain and child development, and epigenetics) and recognizing the important science to underscore the work of all pediatricians to produce the healthiest children possible and to present them to the total US health care system as healthy adults.
Academic Pediatric Association’s Priorities: The Case for Ending Childhood Poverty
Benard P. Dreyer, MD, President, Academic Pediatric Association
The Academic Pediatric Association (APA) is dedicated to improving the health and well-being of all children and adolescents and to advocating for an equitable child health agenda. As such, a special focus of the organization is the well-being of poor and vulnerable children. It is appropriate, therefore, to focus the pediatric profession on the current state of childhood poverty in the United States and to suggest an action agenda.
Scope and Consequences of Childhood Poverty in the United States
Twenty-two percent of children in the United States are living below the federal poverty level (FPL).11 Children are the poorest segment of our society; childhood poverty in the United States has been persistent since the 1970s, except for some fluctuation due to economic cycles. As a society, we have made policy decisions to support the elderly but not, to the same extent, children. In 1959, 35% of seniors were living in poverty, but expansion of Social Security and the introduction of Medicare in the 1960s led to a dramatic drop in senior poverty, ultimately leading to a 9% level today.11,12
Present federal poverty thresholds, originally designed in the 1960s, are calculated based on the cost of a minimum food budget multiplied by 3 and adjusted for family size and average cost of living.13 However, food now accounts for only 10% to 20% of a family’s budget, with housing and child care accounting for much larger percentages. Therefore, depending on regional differences, 200% to 350% of the FPL is necessary for a family to meet its minimum needs.14 Using the conservative figure of 200% of the FPL, almost 1 in 2 children are living in poverty or near poverty.15
Furthermore, there are large racial/ethnic inequities in childhood poverty, with almost 1 in 2 African-American and Hispanic children living in poverty.15 Minority children are more likely to experience extreme poverty (<50% of the FPL) and persistent poverty lasting throughout childhood.16 Finally, the United States ranks 30 of 34 developed countries in rate of childhood poverty.17 Social policies in most of the other developed countries have led to an average child poverty rate of 12% compared with 22% for the United States.12
The consequences of poverty on the health and well-being of children are shown in Table 1.16,18,19 Although the consequences on child health are significant, the consequences of poverty on child and adolescent well-being change their life trajectories, lead to unproductive adult lives, and trap them in intergenerational poverty.
TABLE 1.
Consequences of Poverty on Child and Adolescent Health and Well-Being
| Health |
| • Increased infant mortality |
| • Low birth weight and subsequent health and developmental problems |
| • Increase in frequency and severity of chronic diseases such as asthma |
| • Poorer access to quality health care |
| • Increased accidental injury and mortality |
| • Increased obesity and its complications |
| Well-beinga |
| • Poorer educational outcomes: poor academic achievement; lower rates of high school graduation |
| • Less positive social and emotional development |
| • More problem behaviors leading to “trajectory altering events”: |
| – Early unprotected sex, with increased teen pregnancy |
| – Drug and alcohol abuse |
| – Increased criminal behavior as adolescents and adults |
| • More likely to be poor adults: intergenerational poverty and lack of economic productivity |
All outcomes are increased in frequency and severity if the child lives in extreme poverty (<50% FPL), long-term poverty, or poverty during early childhood.16
What Can We Do as a Nation?
As a nation, we can try to lift children out of poverty through cash benefits, supportive services, and tax breaks, as well as alleviate the effects of poverty on poor children. These types of interventions will lead to better health and well-being for poor children and give them a chance at more productive lives.
The United Kingdom is a model for what the United States might be doing. In 1999, the Labour government started a campaign against childhood poverty and pledged to reduce rates to one-half in 10 years.20,21 Due to the efforts of the UK government from 1999 to the present, the absolute childhood poverty rate, which started out higher than in the United States, was cut to 12% in 2008.20 Government policy and actions, therefore, do matter. In 2010, all 3 UK political parties pledged to continue these efforts through the Childhood Poverty Act of 2010, with goals of more than halving present childhood poverty rates by 2020.22,23
There is extensive research evidence that investments in early childhood, during the critical period of early brain development, are the most effective means of alleviating the impact of poverty on children.24,25 Most of the gap in school achievement between poor and non-poor children is already present at school entry.26 There are evidence-based programs to improve parenting and child development that include high-quality preschool, home visiting programs, and interventions in pediatric primary care.27–32 The United Kingdom’s plan has also included a strong emphasis on early childhood. An agenda for our nation to lift children out of poverty, as well as alleviate the effects of living in poverty, should include the actions listed in Table 2.13,14,18,20–33
TABLE 2.
A National Agenda to Reduce Childhood Poverty and Alleviate Its Effects
| Action | Example |
|---|---|
| Make a commitment to address child poverty | • Major political parties/leaders recognize child poverty as an important national issue |
| Set goals to reduce childhood poverty | • Emulate actions of the United Kingdom; set goal of reducing childhood poverty by one-half in 10 y20–33 |
| Expand existing benefits, cash transfers, and tax breaks that are now reducing childhood poverty levels13,18,33 | • Expand Earned Income Tax Credit; Child Tax Credit; Supplemental Nutritional Assistance Program; housing subsidies; energy assistance; Women, Infants, and Children program; school lunch programs |
| • Support continued expansion of Medicaid/Children’s Health Insurance Program; keep children’s coverage strong during health care reform efforts | |
| • Expand financial support for and availability of high-quality child care, especially for working families | |
| Invest in Early Childhood Programs to improve early childhood cognitive and social–emotional development and reduce toxic stress14–32 | • Expand high-quality preschool for poor children |
| • Implement evidence-based home visiting programs for all newborns in poor families through the ACA or other funding mechanisms | |
| • Disseminate evidence-based interventions in primary care pediatrics |
What Can We Do as Pediatricians and Pediatric Organizations?
As pediatricians, and as pediatric organizations, we need to raise our voices. What we say matters to our elected officials and policy makers. We need to place reducing childhood poverty at the top of our policy and advocacy agendas. We must integrate a focus on reducing childhood poverty into the activities and structures (committees, special interest groups, councils, regions, and chapters) of our organizations.
To begin that process, the APA Board has voted to form a Task Force on Childhood Poverty. The task force is charged with recruiting advocates, experts, and scientists from the APA, other pediatric organizations, and the economic and social sciences, as well as policy makers from private and public spheres, in the United States and internationally, to create and implement an action agenda. Let us join together to start the long and difficult process to end childhood poverty!
Association of Medical School Pediatric Department Chairs’ Priorities: Training and Access
Alan R. Cohen, MD, President, Association of Medical School Pediatric Department Chairs
The responsibility of pediatric department chairs for the training of medical students, residents, and fellows gives them a special investment in the education of future pediatricians and pediatric subspecialists. At the same time, the chairs have a responsibility to assure that the clinical mission of accessible high-quality care is fulfilled. With these responsibilities in mind, the Association of Medical School Pediatric Department Chairs (AMSPDC) has identified 2 different but ultimately related priorities in the national agenda for children and adolescents: training and access to care. The leadership of AMSPDC believes that it is highly likely that the activity of the 113th Congress will affect both of these priorities.
Training
GME in freestanding children’s hospitals is supported primarily by CHGME funding, which was enacted in 1999 to address disparities between children’s hospitals and other teaching hospitals and has been reauthorized since then with broad bipartisan support. Currently, CHGME provides funding to 56 children’s hospitals in 30 states.34 In general hospitals, GME is supported primarily by direct Medicare funding of the salaries of trainees and indirect payments to hospitals for the increased costs of care associated with education.35 In many states, Medicaid provides additional support for GME to both children’s hospitals and general hospitals.
According to data from the GME Database of the American Medical Association, between 2000 and 2011, the number of categorical pediatric residency programs increased by 40%, and the number of pediatric subspecialty programs increased by 42%. During this same period, the number of positions in these 2 types of programs increased by 38% and 54%, respectively. Although forces other than federal and state funding have contributed to this growth, CHGME funding has certainly been a major factor. In fact, the National Association of Children’s Hospitals and Related Institutions estimates that CHGME accounted for ∼74% of the growth in new pediatric subspecialists in the last decade.34
Substantial threats loom to the support of GME by CHGME, Medicare, and Medicaid. In President Obama’s fiscal year 2012 budget, CHGME was eliminated but subsequently restored by Congress with a 15% cut. The fiscal year 2013 budget proposed by the White House has a further 67% reduction in CHGME funding. The total number of training slots funded by Medicare was capped in 1997, and the Simpson-Bowles Commission has recently proposed major reductions in Medicare support for GME. As with CHGME funding, Medicare funding for training remains highly vulnerable as the 113th Congress charts a course to address the deficit.
State support for GME funding is no less tenuous. In 2005, a total of 47 states spent $3.78 billion to support training.35 By 2009, the number of states supporting GME decreased to 41, and the money spent had decreased by $600 million. Since then, another 15 states have indicated that they are considering reducing or ending support for training through Medicaid.
Undergraduate medical education is under pressure as well. In many states, support for medical education is directly affected by cuts in funding to state-related institutions. Further cuts come indirectly through reduced payments to academic medical centers and by reductions in state grants, scholarship, and loan forgiveness plans. As the incurred cost of medical education increases, anticipated consequences include a less diverse student body and the possibly profound effect of increased debt on career choices. Neither augurs well for the pediatric workforce.
Ironically, while governmental support of GME and undergraduate medical education is decreasing, the number of allopathic and osteopathic medical schools is increasing, as is the enrollment in many existing schools. By 2015, the first-year enrollment in medical schools is expected to be 35% higher than in 2002, and continuing increases are projected through 2020.35
If total graduate training slots remain at 2010 levels while medical school enrollment increases, there will not be a sufficient number of residency training slots to accommodate US and international medical graduates. If residency training slots decrease by 1% annually because of decreased funding, the number of positions will be insufficient to accommodate graduates of US allopathic and osteopathic schools by 2017. At present, both the funding and planning for undergraduate medical education and GME remain largely uncoordinated. Success in training tomorrow’s workforce dictates that they should be tightly related.
Subspecialty training has also declined. Ruth L. Kirschstein National Research Service Award postdoctoral training grants and fellowships such as T32s and F32s have decreased in the past 10 years, as have awards such as K08s and K23s. These reductions have further affected the future of pediatric clinical subspecialty capacity and limited our biomedical research capacity.36
Access to Care
The Association of American Medical Colleges projects a growing gap between the demand and supply for physicians across all specialties, leading to a shortage of >90 000 physicians by 2020.37 Although this shortage is fueled in part by an ageing population with greater medical needs, it is also driven by the restricted number of postgraduate training positions.
In pediatrics, access to care is already problematic. Waiting times to see subspecialists in pulmonology, neurology, endocrinology, and developmental pediatrics are, on average, 8 to 13 weeks, and may be much longer in some communities.38 These wait times are not surprising when physician vacancies for >12 months in these same subspecialties are reported to be 40% to 63%.38 Nor is it surprising that the average travel distances to see a developmental pediatrician or rheumatologist are 44 and 60 miles, respectively.39 As with the projected shortage in the total number of physicians, the shortage in certain pediatric subspecialties is not due to the number of training positions alone. Increased demand for some services, noncompetitive salaries, and uneven geographical distribution are just a few of the other factors affecting access to subspecialty care. Even though the number of pediatricians entering subspecialty training has been gradually but steadily increasing since 2000, the fact remains that access to subspecialists in developmental pediatrics or pulmonology, for example, is not likely to improve substantially when, according to the data from the American Board of Pediatrics, only 28 and 49 fellows, respectively, in these disciplines just completed their third year of training and are potentially entering the workforce.40
It is important to note that 40% of children’s hospitals report that they have created or expanded subspecialty fellowship programs as one approach to addressing shortages of care providers.38 It follows that reductions in training positions will almost certainly adversely affect the balance between demand and supply and therefore access to care, even as other contributing factors are addressed. As we prepare for increasing coverage for all children and adults through the ACA, we should be creating ways to expand all aspects of the pediatric workforce. The policies mentioned, in fact, further limit our ability to provide appropriate care for children and families.
Summary
The long pipeline that leads from medical school through residency and subspecialty training has numerous current and potential constrictions. The downstream effects of the reduced support for undergraduate and graduate training include significant threats to the development of an appropriate pediatric workforce and the future of biomedical innovation by physician–scientists. AMSPDC believes that access to care for children and their families is a critically important outcome of the educational continuum that calls for urgent and active engagement of the 113th Congress.
American Pediatric Society’s Priorities: The Need for a More Diverse Pediatric Workforce
F. Bruder Stapleton, MD, President, American Pediatric Society
Improving the health of children is the mission of all pediatricians. It is assumed that this mission includes all children, regardless of their race or ethnicity. As the demographic characteristics of children aged <18 years have grown increasingly diverse, the impact of health inequities and disparities will be disproportionately realized in our pediatric patients. To provide culturally relevant medical care and biomedical research, a culturally diverse and representative pediatric workforce is urgently needed.41
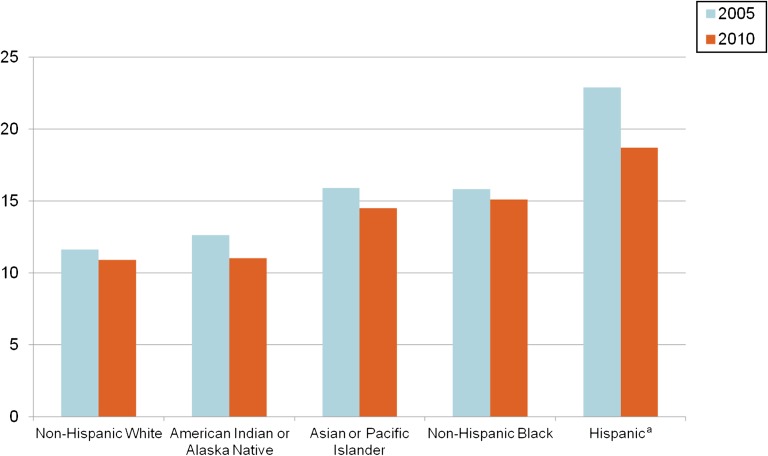
The pediatric population has shown significant demographic shifts. In 1996, among the 72 879 000 children in the United States, 23.6% were black, Hispanic, or Native American.41 Based on the extant birth rates, it was predicted that in 2010, minority children would comprise 42% of the pediatric population, and Hispanic children would represent 19% of the pediatric population.41 These predictions were remarkably prescient. Figure 1 demonstrates the birth rates in 2005 and 2010. Although birth rates have fallen among all racial and ethnic groups, the birth rate for Hispanic families has remained the highest among all groups at 18 live births per 1000 population.42 Among the 73.9 million US children aged <18 years in 2009, 40.6% were underrepresented minority children.43 Hispanic children represented 22.5%; black children, 15.4%; other minority race, 3.1%; Asian, 3.7%; and non-Hispanic white children, 55.7%. The growing minority pediatric population is most notable in the group of US children <6 years of age, 42.4% of whom are from minority communities. Based on current birth rates (Fig 1), we can expect the minority population, particularly the Hispanic pediatric population, to continue to represent a growing proportion of our patient population.
FIGURE 1.
US birth rates according to race and Hispanic origin (total number of births per 1000 population). aIncludes all persons of Hispanic origin of any race.42
Although the number of URM pediatric residents is unknown, in 2008 only 14.3% of US pediatricians were URM physicians.44 Hispanic pediatricians comprised 6.4%; black pediatricians, 7.5%; American Indian or Alaska Native pediatricians, 0.4%; Asian pediatricians, 12.4%; and non-Hispanic white pediatricians, 73.3%. It is important to increase the number of URM pediatricians because they tend to return to provide primary care to individuals of the same racial or ethnic backgrounds, often in medically underserved communities.45 Minority pediatricians can also serve as role models for their patients and inspire the next generation of promising students to consider medical careers.
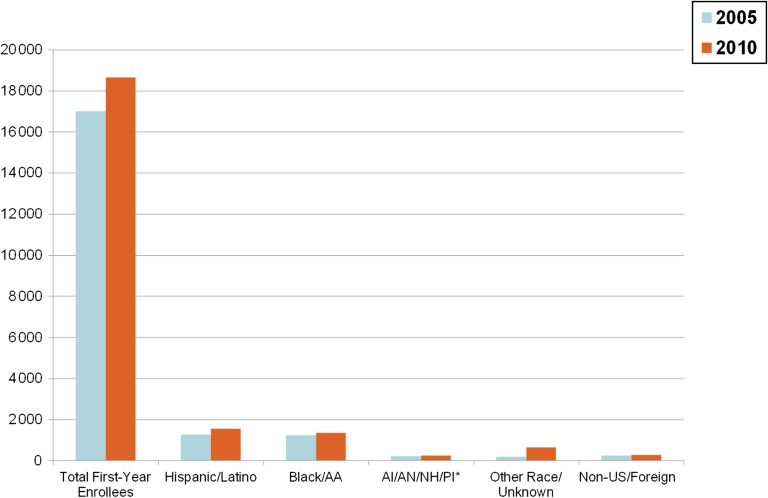
The proportion of URM pediatricians closely mirrors the percentage of URM medical school matriculants (Fig 2). As a result of the increasing absolute number of medical students, an incremental increase in URM medical students has also occurred.46 However, in 2011, only 7% of entering medical students were black, and 8% were Hispanic.47 These numbers have not seen significant growth since 1998 when URM medical students accounted for 12.4% of the entering matriculants41 and certainly do not reflect the growing diversity of the general population.
FIGURE 2.
Number of first-year enrollees to US medical schools.46 AA, African-American; AI, American Indian AN, Alaska Native; NH, Native Hawaiian; PI, Pacific Islander.
The leaders of the American Pediatric Society (APS) believe that greater racial and ethnic diversity is a critical need for academic pediatricians as well as for community-based providers. We do not have data concerning the racial and ethnic composition of the pediatric academic workforce; however, our experiences tell us that we are not significantly diverse. As educators, academic pediatricians have the opportunity to reach the URM medical students and introduce them to careers in pediatrics. Having greater diversity in academic pediatric faculty will create a more welcoming environment for URM students as they weigh career opportunities. Academic pediatricians also have the responsibility for creating new knowledge through research, which is vital to reducing the well-recognized disparities in health outcomes among races and ethnic groups. Currently, the number of URM pediatrician–scientists is small and should be a national priority.48
The APS believes that the need for diversity and inclusiveness is of such importance that we have revised our mission and value statements. The new APS value states, “Diversity, equity, and inclusion are essential values for academic pediatrics, pediatricians in training, and the practice of pediatrics.” We have also created a standing committee on diversity and inclusiveness to guide initiatives and begin collecting demographic data to monitor progress in broadening the workforce in academic pediatrics.
What can be done to develop a more diverse pediatric workforce? Much depends on societal commitments greater than and proximal to medical school. We need stronger educational programs for all segments of our communities, especially in the fields of science and math, to prepare students for success in the university setting. Creating opportunities for high school students to gain exposure to medical practices and research should be considered, despite the increasingly stringent privacy requirements. Finding ways to reduce the financial burden of higher education is an absolute requirement to develop an inclusive medical community, as all students must now consider their own financial viability after the expense of receiving a bachelor’s degree, a medical degree, and postgraduate medical education.
Academic pediatricians must lead the way by encouraging our amazing URM medical students to pursue careers in pediatrics. Academic departments should examine their mission statements to see if diversity and inclusiveness are clearly identified as a principle to guide the policies, practices, and decisions in their programs. America’s children are waiting for us to catch up.
THE SOCIETY FOR PEDIATRIC RESEARCH: INVESTING IN BASIC, CLINICAL, TRANSLATIONAL, AND POPULATION RESEARCH LEADS TO IMPROVEMENTS IN CHILD HEALTH
Susan L. Furth, MD, PhD, President, Society for Pediatric Research
“Our most basic common link is that we all inhabit this planet. We all breathe the same air. We all cherish our children’s future. ”
-John F Kennedy49
Since its founding in 1929, the Society for Pediatric Research (SPR) has had the expansive goal of advancing the well-being of children and youth by supporting the creation and broad communication of new knowledge that can improve child health. Since the society’s initial meeting in 1929 with 25 men in attendance,50 both the SPR and the threats to child health have clearly changed, yet SPR’s core values remain. These core values drive the SPR’s priorities in developing a national agenda for children and youth. The SPR’s priorities include support for initiatives that increase the quantity, quality, and dissemination of pediatric research. These research-oriented priorities are in addition to the SPR’s ongoing support of fundamental programs ensuring access to health care for children; namely, the ACA and funding for CHGME and Medicare GME. Together with the AAP, the APA, and the APS, we all cherish our children’s future.
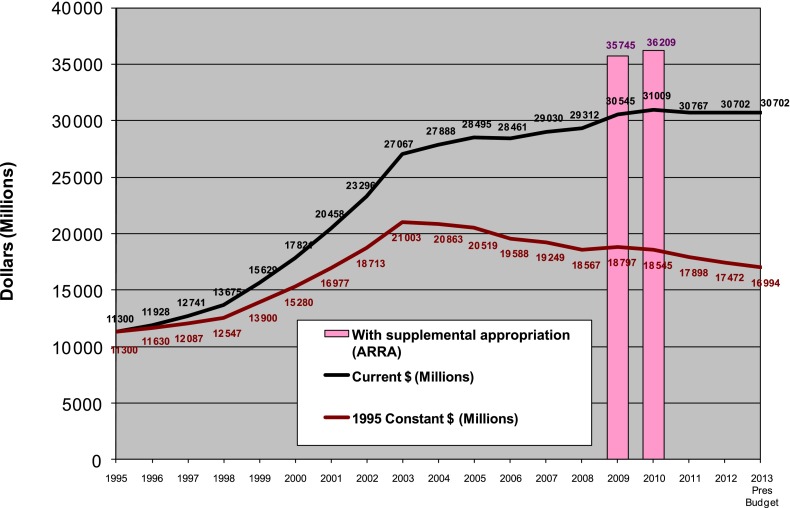
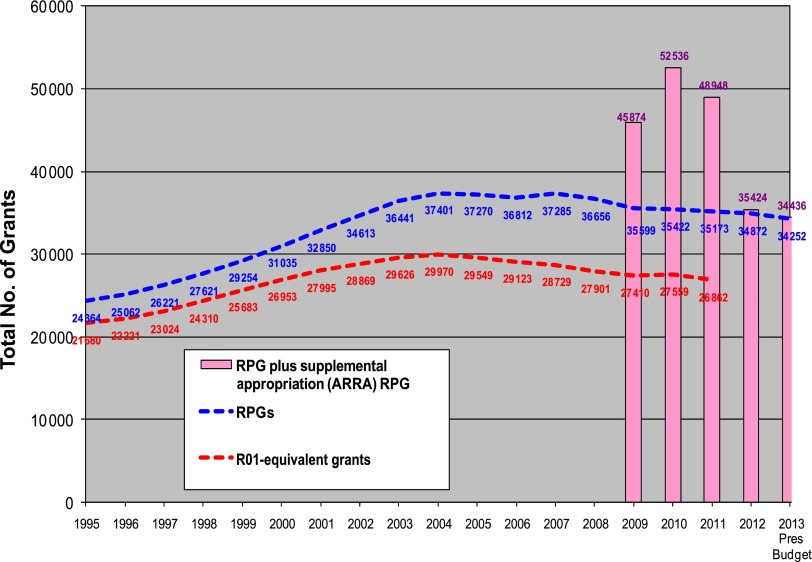
The founding of the SPR was spawned by the growth of the pediatric academic community and the new emphasis on clinical investigation. The threats to children’s health and challenges in clinical investigation that exist today are remarkably different from those that existed in 1929 at the society’s founding, yet the SPR still holds the core belief that investment in basic, clinical, translational, and population-based research can lead to dramatic improvements in the lives of children. Life expectancy for the average child born in the United States has increased to 78 years, >20 years longer than the life expectancy for a child born in 1929, the year the SPR was founded.51 The increase in life expectancy is at least partly due to decreases in child mortality, achieved through advances made possible through child health research. To sustain the pace of discovery and implementation of child health improvements that have evolved over the last century, the SPR supports ongoing investment in the National Institutes of Health (NIH). The SPR supports the mission of the NIH: to seek fundamental knowledge about the nature and behavior of living systems and the application of that knowledge to enhance health, lengthen life, and reduce the burdens of illness and disability.52 The NIH is currently facing a number of significant challenges.53 After taking inflation into account, the fiscal year 2012 budget and President Obama’s proposed budget for fiscal year 2013 are the lowest since 2001 (Fig 3).54 The number of research project grants funded by the NIH has declined every year since 2004 (Fig 4). In addition, perhaps most worrisome for the early career investigator contemplating a future career in research, grant application success rates have fallen >14 percentage points in the past decade. There is no reason to expect that this decline will be halted in future years. The NIH received $30.7 billion in fiscal year 2012 appropriations, and the Eunice Kennedy Shriver National Institute on Child and Human Development was funded at $1.3 billion. Although this institute contributes a significant proportion of NIH’s support of pediatric research, many other NIH institutes also support research that advances child health. The SPR supports broad-based funding across the institutes, as well as strongly supporting the newly established National Center for Advancing Translational Sciences. From early on, promoting collaboration across the spectrum of research methodologies has been a core value of the SPR, manifested through its support of the Pediatric Academic Societies’ Annual Meeting. The annual meetings have always been open to members and nonmembers and have served to promote free communication, critical review, and opportunities for integration of scientific findings. The stated goal of the National Center for Advancing Translational Sciences is to translate basic scientific discoveries into drugs, diagnostics, and devices, and the SPR strongly supports this type of translational research to bring scientific developments into medical practice and thus improve the care of children. The SPR urges Congress to continue to support and expand the NIH budget and to act to avoid the consequences of sequestration, which could lead to as much as a $2.8 billion reduction in the NIH extramural budget in early 2013. In a similar vein, the SPR supports programs that improve the evidence base for drug therapies in children, including renewal of the Best Pharmaceuticals for Children Act. Since its inception, the Best Pharmaceuticals for Children Act has led to studies improving our knowledge of medication use in children, and we support recent efforts to study older drugs that no longer qualify for pediatric exclusivity, and call for including studies on neonates.
FIGURE 3.
NIH appropriation in current and constant dollars.54 ARRA, American Recovery and Reinvestment Act of 2009; Pres, President’s.
FIGURE 4.
Number of NIH-supported research project grants (RPGs).54 ARRA, American Recovery and Reinvestment Act of 2009; Pres, President’s.
An additional core value of the SPR is to foster the research efforts and career development of investigators engaged in child health research. To this end, the SPR actively supports the development of future pediatric scientists. As a society, we sponsor a student research-training program and recognize outstanding research achievements in pediatrics through SPR-sponsored awards. The SPR strongly supports CHGME and GME funding because it affects potential trainee research exposure and activities, including investment in efforts to meet the challenge of attracting trainees into research and providing research training. Programs such as the Health Resources and Services Administration Pediatric Subspecialty Loan Repayment Program, the Title VII health professions programs, and the Health Careers Opportunity Program, including the diversity pipeline program, are crucial to supporting the development of future child health researchers who can maintain and propel the pace of discovery leading to improvements in child health. By funding both pediatric primary care and subspecialty fellowship training programs, these agencies can be assured that we will have the appropriately trained workforce to continue to develop treatments for tomorrow’s children.
CONCLUSIONS
Although most agree that children are our most precious resource, they are often forgotten when it comes to the overall priorities of Congress. The message here is clear: We must provide for the future health and well-being of our children by guaranteeing access to quality health care, which is provided by a culturally diverse primary care and specialty workforce that is adequate to meet their medical and social needs. At the same time, we must continue to foster biomedical research that focuses on children and develops pediatric scientists. Finally, we must strive to end childhood poverty. We have many challenges to overcome in the unified pursuit of adequately caring for our children and families. The 113th Congress is ideally positioned to help us move that agenda forward.
Acknowledgments
We thank the 2012 Pediatric Academic Societies Planning Committee and the members of the Public Policy Council for their help in planning and coordinating this symposium. In addition, we acknowledge the immeasurable support we received from Heidi Saliba, Coordinator of Research Programs, Division of General Pediatrics and Ped-I-Care, University of Florida, for her assistance in editing and assembling the manuscript.
Glossary
- AAP
American Academy of Pediatrics
- ACA
Patient Protection and Affordable Care Act
- AMSPDC
Association of Medical School Pediatric Department Chairs
- APA
Academic Pediatric Association
- APS
American Pediatric Society
- CHGME
Children’s Hospital Graduate Medical Education
- FPL
federal poverty level
- GME
Graduate Medical Education
- NIH
National Institutes of Health
- SPR
Society for Pediatric Research
- URM
underrepresented minorities
Footnotes
Dr Block was president of the American Academy of Pediatrics when he participated in the plenary session of the Public Policy Council during the 2012 Pediatric Academic Societies (PAS) meeting and outlined the American Academy of Pediatrics’ agenda for children for the new Congress to begin in 2013; Dr Dreyer was president of the Academic Pediatric Association when he participated in the plenary session of the Public Policy Council during the 2012 PAS meeting and outlined the Academic Pediatric Association’s agenda for children for the new Congress to begin in 2013; Dr Cohen was president of the Association of Medical School Pediatric Department Chairs when he participated in the plenary session of the Public Policy Council during the 2012 PAS meeting and outlined the Association of Medical School Pediatric Department Chairs’ agenda for children for the new Congress to begin in 2013; Dr Stapleton was president of the American Pediatric Society when he participated in the plenary session of the Public Policy Council during the 2012 PAS meeting and outlined the American Pediatric Society’s agenda for children for the new Congress to begin in 2013; Dr Furth was president of the Society for Pediatric Research when she participated in the plenary session of the Public Policy Council during the 2012 PAS meeting and outlined the Society for Pediatric Research’s agenda for children for the new Congress to begin in 2013; and Dr Bucciarelli was chair of the Public Policy Council of the PAS and was chair of the PAS Plenary Session.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: No external funding.
COMPANION PAPERS: Companions to this article can be found on pages 1 and 147, and online at www.pediatrics.org/cgi/doi/10.1542/peds.2012-2432 and www.pediatrics.org/cgi/doi/10.1542/peds.2012-3250.
References
- 1.First Focus Campaign for Children. Children’s Budget 2012. Available at: www.firstfocus.net/sites/default/files/CB2012%20Final-Web.pdf. Accessed August 15, 2012
- 2.Genel M, McCaffree MA, Hendricks K, et al. A National Agenda for America’s Children and Adolescents in 2008: recommendations from the 15th Annual Public Policy Plenary Symposium, annual meeting of the Pediatric Academic Societies, May 3, 2008. Pediatrics. 2008;122(4):843–849. Available at: http://pediatrics.aappublications.org/content/122/4/843.full.html. Accessed April 27, 2012 [DOI] [PubMed] [Google Scholar]
- 3.Crozer Griffith JP. The Rise, Progress and Present Needs of Pediatrics, Section on Diseases of Children, AMA. Chicago, IL: American Medical Association Press; 1898:14 [Google Scholar]
- 4.US Department of Labor. Employee Benefits Security Administration. Affordable Care Act. Available at: www.dol.gov/ebsa/healthreform/. Accessed July 12, 2012
- 5.Prepared remarks by Judith S. Palfrey, MD, FAAP, President, American Academy of Pediatrics. February 9, 2010. Available at: www.aap.org/en-us/about-the-aap/aap-press-room/pages/Prepared-Remarks-by-Judith-S–Palfrey,-MD,-FAAP-President,-American-Academy-of-Pediatrics.aspx?nfstatus=401&nftoken=00000000-0000-0000-0000-000000000000&nfstatusdescription=ERROR%3a+No+local+token. Accessed August 15, 2012
- 6.Garner AS, Shonkoff JP, Siegal BS, et al. Committee on Psychosocial Aspects of Child and Family Health. Committee on Early Childhood, Adoption, and Dependent Care. Section on Developmental and Behavioral Pediatrics . Early childhood adversity, toxic stress, and the role of the pediatrician: translating developmental science into lifelong health. Pediatrics. 2012;129(1). Available at: www.pediatrics.org/cgi/content/full/129/1/e224. [DOI] [PubMed] [Google Scholar]
- 7.Shonkoff JP, Garner AS; Committee on Psychosocial Aspects of Child and Family Health; Committee on Early Childhood, Adoption, and Dependent Care; Section on Developmental and Behavioral Pediatrics. The lifelong effects of early childhood adversity and toxic stress. Pediatrics 2012;129(1). Available at: http://pediatrics.aappublications.org/content/129/1/e232 [DOI] [PubMed]
- 8.Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, Anda RF. Adverse childhood experiences and the risk of depressive disorders in adulthood. J Affect Disord. 2004;82(2):217–225 [DOI] [PubMed] [Google Scholar]
- 9.Heckman JJ. The economics, technology, and neuroscience of human capability formation. Proc Natl Acad Sci U S A. 2007;104(33):13250–13255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Strategic Priorities and AAP Initiatives, 2011-2012. Available at: www.aap.org/en-us/Documents/Strategic_Priorities_and_AAP_Initiatives.pdf. Accessed July 12, 2012
- 11.DeNavas-Walt C, Proctor BD, Smith JC. US Census Bureau, Current Population Reports, P60-239, Income, Poverty, and Health Insurance Coverage in the United States: 2010. Washington, DC: US Government Printing Office; 2011 [Google Scholar]
- 12.Sachs JD. The Price of Civilization. New York, NY: Random House; 2011:196–199 [Google Scholar]
- 13.Short K. US Census Bureau, Current Population Reports, P60-241, The Research Supplemental Poverty Measure: 2010. Washington, DC: US Government Printing Office; 2011 [Google Scholar]
- 14.Allegretto SA. Economic Policy Institute Briefing Paper #165. Basic family budgets: working families’ incomes often fail to meet living expenses around the US. Available at: www.epi.org/publication/bp165/. Accessed June 23, 2012 [DOI] [PubMed]
- 15.Child Trends DataBank. Children in poverty. Available at: http://www.childtrendsdatabank.org/?q=node/221. Updated September 2011. Accessed June 23, 2012
- 16.Aber JL, Bennett NG, Conley DC, Li J. The effects of poverty on child health and development. Annu Rev Public Health. 1997;18:463–483 [DOI] [PubMed] [Google Scholar]
- 17.OECD Family Database. CO2.2: child poverty. Available at: www.oecd.org/dataoecd/52/43/41929552.pdf. Updates October 20, 2011. Accessed June 23, 2012
- 18.Moore KA, Redd Z, Burkhauser M, Mbwana K, Collins A. Child Trends Research Brief, Publication #2009-11. Children in poverty: trends, consequences, and policy options. Available at: www.childtrends.org/files/child_trends-2009_04_07_rb_childreninpoverty.pdf. Published April 6, 2009. Accessed June 23, 2012
- 19.Ogden CL, Lamb MM, Carroll MD, Flegal KM. Obesity and Socioeconomic Status in Children: United States 1988–1994 and 2005–2008. NCHS Data Brief No 51. Hyattsville, MD: National Center for Health Statistics; 2010 [Google Scholar]
- 20.Smeeding TM, Waldfogel J. Fighting poverty: attentive policy can make a huge difference. J Policy Anal Manage. 2010;29(2):401–407 [Google Scholar]
- 21.Waldfogel J. Britain’s War on Poverty. New York, NY: Russell Sage Foundation; 2010 [Google Scholar]
- 22.Child Poverty Act of 2010. Available at: www.legislation.gov.uk/ukpga/2010/9/pdfs/ukpga_20100009_en.pdf. Published 2010. Accessed June 23, 2012
- 23.Department for Work and Pensions, Department for Education. A new approach to child poverty: tackling the causes of disadvantage and transforming families’ lives. Available at: https://www.education.gov.uk/publications/standard/publicationDetail/Page1/CM%208061. Published April 2011. Accessed June 23, 2012
- 24.Knudsen EI, Heckman JJ, Cameron JL, Shonkoff JP. Economic, neurobiological, and behavioral perspectives on building America’s future workforce. Proc Natl Acad Sci U S A. 2006;103(27):10155–10162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shonkoff JP, Phillips D. From Neurons to Neighborhoods: The Science of Early Childhood Development. Washington, DC: National Academies Press; 2000 [PubMed] [Google Scholar]
- 26.Heckman JJ. Skill formation and the economics of investing in disadvantaged children. Science. 2006;312(5782):1900–1902 [DOI] [PubMed] [Google Scholar]
- 27.Schweinhart LJ, Montie J, Xiang Z, Barnett WS, Belfield CR, Nores M. Lifetime Effects: The High/Scope Pery Preschool Study through Age 40. Ypsilanti, MI: High/Scope Press; 2003:194–215 [Google Scholar]
- 28.Campbell FA, Pungello EP, Miller-Johnson S, Burchinal M, Ramey CT. The development of cognitive and academic abilities: growth curves from an early childhood educational experiment. Dev Psychol. 2001;37(2):231–242 [DOI] [PubMed] [Google Scholar]
- 29.Levenstein P, Levenstein S, Oliver D. First grade school readiness of former child participants in a South Carolina replication of the Parent-Child Home Program. Appl Dev Psychol. 2002;23:331–353 [Google Scholar]
- 30.Mendelsohn AL, Mogilner LN, Dreyer BP, et al. The impact of a clinic-based literacy intervention on language development in inner-city preschool children. Pediatrics. 2001;107(1):130–134 [DOI] [PubMed] [Google Scholar]
- 31.Mendelsohn AL, Dreyer BP, Flynn V, et al. Use of videotaped interactions during pediatric well-child care to promote child development: a randomized, controlled trial. J Dev Behav Pediatr. 2005;26(1):34–41 [PMC free article] [PubMed] [Google Scholar]
- 32.Mendelsohn AL, Valdez PT, Flynn V, et al. Use of videotaped interactions during pediatric well-child care: impact at 33 months on parenting and on child development. J Dev Behav Pediatr. 2007;28(3):206–212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tichen L, Jolliffe D, Gundersen C. Alleviating Poverty in the United States: The Critical Role of SNAP Benefits, ERR-132. Washington, DC: US Department of Agriculture, Economic Research Service; 2012 [Google Scholar]
- 34.Data from the National Association of Children’s Hospitals and Related Institutions. June 2012. Available at: www.childrenshospitals.net/AM/Template.cfm?Section=Search3&template=/CM/HTMLDisplay.cfm&ContentID=61357. Accessed May 22, 2012
- 35.Iglehart JK. The uncertain future of Medicare and graduate medical education. N Engl J Med. 2011;365(14):1340–1345 [DOI] [PubMed] [Google Scholar]
- 36.Rockey S. Rock Talk: Trends in NIH training and career development awards. Extramural Nexus, Office of Extramural Research, National Institutes of Health, October 7, 2011. Available at: http://nexus.od.nih.gov/all/2011/10/07/trends-in-nih-training-and-career-development-awards/. Accessed August 19, 2012
- 37.AAMC. Physician shortages to worsen without increases in residency training. Available at: https://www.aamc.org/download/150612/data/md-shortage.pdf. Accessed August 19, 2012
- 38.Groves D. Pediatric subspecialty shortages affect access to care. Data from the National Association of Children’s Hospitals and Related Institutions, 2010. Available at: www.childrenshospitals.net/AM/Template.cfm?Section=Search3&content=annual_survey&template=/cm/contentdisplay.cfm&contentfileid=10027. Accessed August 19, 2012
- 39.Mayer ML. Are we there yet? Distance to care and relative supply among pediatric medical subspecialties. Pediatrics. 2006;118(6):2313–2321 [DOI] [PubMed] [Google Scholar]
- 40.The American Board of Pediatrics. Workforce data 2011-2012. Available at: https://www.abp.org/abpwebsite/stats/wrkfrc/workforcebook.pdf. Accessed August 19, 2012
- 41.Stoddard JJ, Back MR, Brotherton SE. The respective racial and ethnic diversity of US pediatricians and American children. Pediatrics. 2000;105(1 pt 1):27–31 [DOI] [PubMed] [Google Scholar]
- 42.National Vital Statistics Reports. Vol 60, No 2. November 17, 2011. Births: preliminary data for 2010. Brady E, Hamilton BE, Martin JA, Ventura SJ, Division of Vital Statistics. Available at: www.cdc.gov/nchs/data/nvsr/nvsr60/nvsr60_02.pdf
- 43.US Department of Commerce. A child's day: 2009. Characteristics of children under 18 and their designated parents: 2009. Available at: www.census.gov/hhes/socdemo/children/data/sipp/well2009/tables.html. Accessed August 17, 2012.
- 44.Diversity in the Physician Workforce: Facts and Figures. Washington, DC: Association of American Medical Colleges; 2010:75 [Google Scholar]
- 45.Petersdorf RG, Turner KS, Nickens HW, Ready T. Minorities in medicine: past, present, and future. Acad Med. 1990;65(11):663–670 [DOI] [PubMed] [Google Scholar]
- 46.Association of American Colleges Washington, DC AAMC Reporter, November 2010. AAMC Data Warehouse: Applicant Matriculant File, Oct 2010.
- 47.Rosenthal E. Molding a new med student. New York Times. April 15, 2012:20–23
- 48.Shurin SB. The American Pediatric Society commentary: the future of pediatric physician scientists is in our hands. Arch Pediatr Adolesc Med. 2012;166(6):503–505 [DOI] [PubMed] [Google Scholar]
- 49.Kennedy JF. Commencement speech at American University, Washington, DC; June 10, 1963
- 50.Weil WB, Jr. The Society for Pediatric Research: from infancy to adulthood in sixty-five years. Pediatrics. 1996;97(1):129–136 [PubMed] [Google Scholar]
- 51.Guyer B, Freedman MA, Strobino DM, Sondik EJ. Annual summary of vital statistics: trends in the health of Americans during the 20th century. Pediatrics. 2000;106(6):1307–1317 [DOI] [PubMed] [Google Scholar]
- 52.National Institutes of Health. Mission statement. Available at: www.nih.gov/about/mission.htm. Accessed June 30, 2012
- 53.Federation of American Societies for Experimental Biology. Federal funding for biomedical and related life science research FY 2013. Available at: www.faseb.org/LinkClick.aspx?fileticket=10Qs6teI4kY%3d&tabid=64. Accessed May 22, 2012
- 54.Federation of American Societies for Experimental Biology. NIH research funding trends: FY1995-2012. Available at: www.faseb.org/Policy-and-Government-Affairs/Data-Compilations/NIH-Research-Funding-Trends.aspx. Accessed May 22, 2012