Abstract
The 2000 Centers for Disease Control and Prevention growth charts are unable to accurately define and display BMI percentiles beyond the 97th percentile. At Children’s Hospital Colorado, we created new growth charts that allow clinicians to track and visualize BMI values in severely obese children. This growth chart defines a child’s BMI as a “percentage of the 95th percentile.” It has the potential to allow clinicians to define subgroups of severe obesity, monitor trends in obese children, and measure treatment success or failure.
KEY WORDS: severe obesity, z-score, BMI, LMS method, growth chart, percentage of the 95th percentile
With the growing obesity epidemic, there is a significant need for improved characterization of extreme values of BMI in children and adolescents. It is well known that the risk for metabolic complications rises as BMI percentile increases. Freedman et al used results from the Bogalusa Heart Study to compare 6 cardiovascular risk factors 6 cardiovascular risk factors (triglycerides, low-density lipoprotein, high-density lipoprotein, fasting insulin, systolic blood pressure, and diastolic blood pressure) in children based on BMI percentile. The results showed that 39% of children >95th percentile and 59% of children ≥99th percentile had ≥2 risk factors, respectively, which was significantly greater than children in the 85th to 95th percentile. Both of the higher BMI groups were much more likely to become obese as adults.1 Therefore, it is important to classify and track severely obese children accurately and practically for both clinical and research purposes.
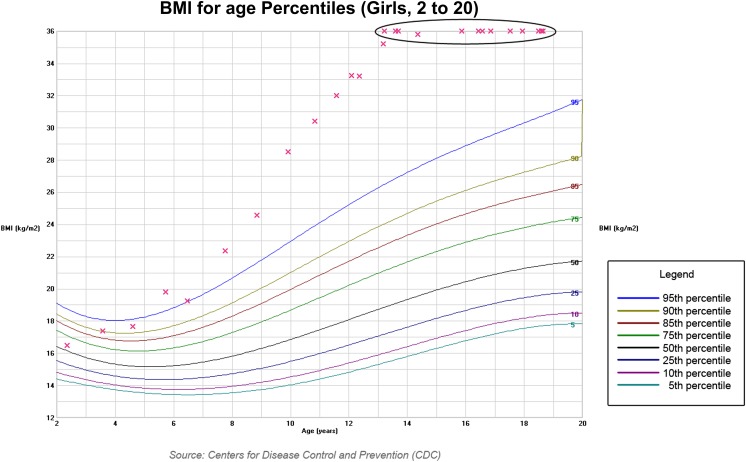
The 2000 Centers for Disease Control and Prevention (CDC) BMI growth charts cannot characterize severely obese children and adolescents. Ten selected empirical percentiles were chosen for evaluation (third, fifth, 10th, 25th, 50th, 75th, 85th, 90th, 95th, and 97th). The 99th percentile was not included.2 The CDC growth chart data set is based on a preobesity epidemic population (1963–1994), leaving sparse data available to construct percentiles beyond the 97th percentile.3,4 The smoothed percentile curves were derived through 2 stages. First, the selected empirical percentiles were smoothed by using a variety of parametric and nonparametric regression procedures. Second, normalized growth curves were constructed by using a modified LMS estimation procedure, which summarizes the distribution by 3 age-dependent smooth curves representing the skewness (L curve), median (M curve), and coefficient of variation (S curve).2 Cole’s LMS method adjusts the BMI distribution for skewness by using a power transformation, which stretches 1 tail of the distribution and shrinks the other, removing the skewness.5,6 The modified procedure used by the CDC applies the LMS technique to smoothed curves compared with the Cole’s original LMS procedure, which applies it directly to data points.2 Derivation of values from select percentiles, rather than from the entire distribution makes extrapolation to the 99th percentile flawed. Even after using the LMS method to normalize the distribution, the transformed data does not allow for modeling in the extreme tails of the distribution. Extrapolated LMS-calculated values for older girls are on average 2 BMI units higher than the empirical 99th percentile.7 In fact, the CDC warns against specifically extrapolating growth charts beyond the 97th percentile.4 Furthermore, the CDC growth charts have a maximum BMI value of 36 kg/m2, which precludes tracking of a severely obese child who has “hit the ceiling” of the chart (Fig 1).
FIGURE 1.
CDC BMI (2000) growth chart, girls aged 2 to 20 years.
Despite the inaccuracy of the 99th percentile on the 2000 CDC growth charts, most clinicians and researchers rely on this as their only measurement of severe obesity because there are no alternatives. This is impractical because at extreme BMIs, large changes in BMI are associated with small changes in percentiles and z scores. A single 99th percentile denotes a huge range of BMI values. BMI z scores have a practical upper limit of ≤4.0. At this upper limit, where BMI z score reaches asymptote, BMI and BMI z score differ by age, gender, and starting BMI.3 An unchanging BMI at the 99th percentile in an adolescent girl as she gets older correlates with a BMI z score that decreases, whereas in a boy, it remains stable or increases. For example, a 12-year-old girl with a BMI of 40 kg/m2, with an increase of BMI to 60 kg/m2 at age 19, would have a decline in her z score from 2.699 to 2.598, which could be misinterpreted as clinical improvement.3 The CDC recognizes that biologically implausible outliers can go undetected because of the z score upper limit. They have proposed an alternative calculation to “flag” these values, but this calculation is infrequently used. Using raw BMIs to classify severe obesity in the pediatric population is not a good solution either because of the expected BMI increases from age-related growth.3
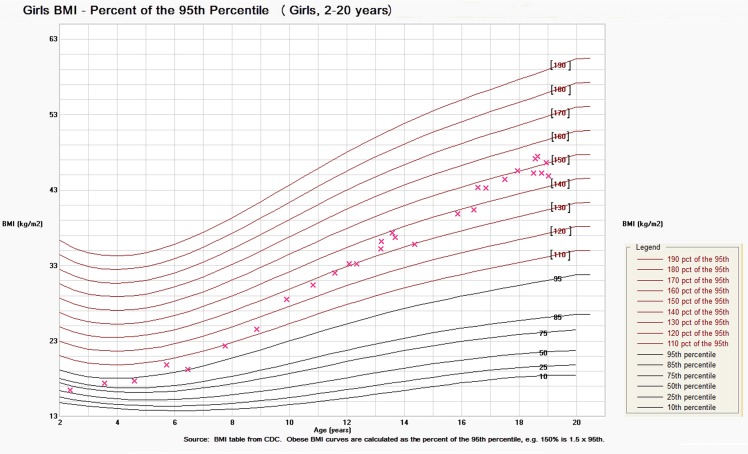
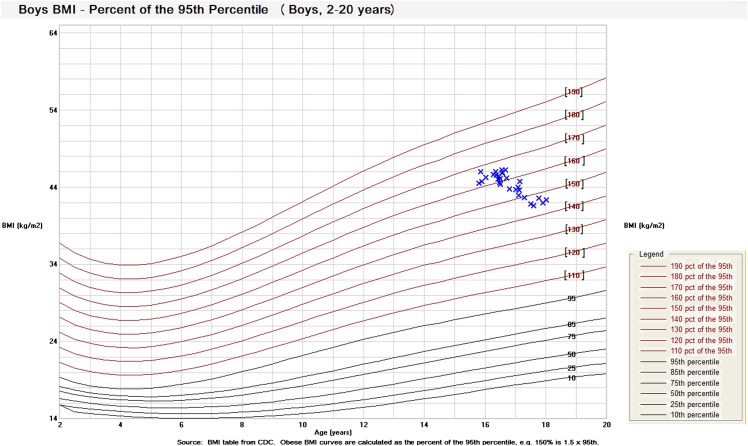
A unique suggestion to classify severe obesity in children was proposed by Flegal et al. They proposed describing the BMI of a very obese child as “the percentage of the 95th percentile.”7 This terminology circumvents the issues related to the 99th percentile. The authors calculated empirical data for the 99th percentile from the 2000 CDC growth chart data set and compared it to extrapolated values from CDC-LMS values. They found that the empirical 99th percentile fits 120% of the smoothed 95th percentile better than the extrapolated LMS values.7 At the Children’s Hospital Colorado, we applied this concept to a BMI growth chart for severely obese children and adolescents. It allows for improved visual tracking and monitoring of extreme BMIs. We were able to incorporate this new growth chart into our electronic medical record system (Epic, Verona, WI). The new curves are derived from CDC data tables for the 95th percentile and are reported as a “percentage of the 95th percentile.” For example, a patient can be categorized as 110% to 190% of the 95th percentile. Extreme BMIs were calculated by multiplying the BMI at the 95th percentile by a factor of 1.1 through 1.9 to derive the 110% to 190%, for both genders, aged 2 to 20 years. These data points were organized into an excel spreadsheet, representing a new data set for severely obese children. These extreme BMI points were plotted into our expanded version of the 2000 CDC growth chart to display the new percentile curves above the 95th percentile. The upper limit for BMI on the growth chart is 64 kg/m2. The CDC LMS-derived percentiles were maintained below these new curves to provide a frame of reference. Figures 2 and 3 show the new obesity growth charts for both boys and girls now used at Children’s Hospital Colorado.
FIGURE 2.
Obesity BMI growth chart, girls aged 2 to 20 years.
FIGURE 3.
Obesity BMI growth chart, boys aged 2 to 20 years.
This new nomenclature and growth chart will allow physicians to accurately define severe obesity, as well as monitor clinical changes. Take the example of a 15-year-old boy who weighs 250 lbs and is 5′8′′ tall. He has a BMI of 38.1 kg/m2, which is at the 99th percentile. If this same boy gained 70 lb, his BMI would increase to 48.8 kg/m2, which is also at the 99th percentile. By using the new nomenclature, he would increase from 142% of the 95th percentile to 182% of the 95th percentile. This terminology is more representative of the change in his weight than a “stable” 99th percentile. Given the restrictions of the 2000 CDC growth charts, these BMI values plot out at the upper limit of the chart. Using the new obesity growth chart, the dramatic increase in BMI can be visually appreciated. It helps clinicians avoid the false assumption that this patient has not changed percentiles or clinically worsened. Severe obesity in the current era has come to include a large spectrum of BMIs, and this classification will allow for subcategories of an overgeneralized group. The new growth charts provide a wide range of percentiles that include all severely obese children. Researchers can redefine the current 99th percentile as 120% of the 95th percentile, which was found to be more accurate based off Flegal’s findings.7 Additional subcategories using this nomenclature have the potential to help standardize research practices. Researchers may be better able to study differences among subgroups of the severely obese and their metabolic risk profiles.
Our new growth charts were uploaded into the electronic medical record making them accessible to all physicians at Children’s Hospital Colorado. Resident physicians (n = 60) completed a brief instructional pamphlet reviewing the concept behind the new obesity growth charts, as well as a follow-up survey to provide feedback. The majority of feedback from the resident questionnaires was positive, with residents ranking these new growth charts on average a 4 out of 5 for potential clinical utility (Likert scale: 0 = not useful to 5 = very useful). Physicians within our pediatric obesity clinics are using these growth charts to monitor the trends in their severely obese patients, and anecdotal reports from them cite improvement in their ability to track and monitor these patients. Pediatric residents are utilizing these growth charts in their primary care clinics and inpatient services. Future studies will evaluate possible changes to clinical and research practice as a result of these growth charts.
There were several concerns from physicians within our hospital regarding these obesity growth charts that could affect its clinical utility. Several physicians noted the lack of intuitiveness in reading them, combined with confusing phraseology (ie, use of 2 percentages). Others felt it was a difficult concept to explain to patients and families, who may misinterpret an obese BMI as “graphically normal” because the growth point would no longer appear at the top of the growth chart. Depending on a particular institution’s limits electronically, the maximum BMI that can be plotted may not be high enough to include all patients. Our electronic medical record system had specific restrictions in the legend, one of which was the inability to include the “%” sign and the other was a word limit. Therefore, the new curves labeled in the legend state, for example, “110 pct of the 95th” rather than “110% of the 95th percentile.”
In conclusion, there is a need for characterization of extreme BMIs in children and adolescents. The 2000 CDC BMI growth charts cannot define percentiles beyond the 97th percentile. Categorization of BMI as a “percentage of the 95th percentile,” as proposed by Flegal et al, is a potential approach that could help classify the 99th percentile.7 The newly formulated obesity growth charts within our electronic medical record at Children’s Hospital Colorado use this concept to allow visual tracking of severely obese patients. The main limitations include bulky phraseology and misinterpretation of the growth chart if it is not well explained to the patient and family. At this time, these growth charts have only been presented to physicians for use. We do not know whether they are being used regularly in practice, helping patients understand their weight or lose weight, or standardizing research practices within our institution. If the growth charts do become used in research, metabolic risks and outcomes of obesity can be differentiated or grouped by percentage of the 95th percentile. Our future research goals include assessing for changes in clinical and research practices in childhood obesity with the advent of these new growth charts.
Acknowledgments
Nola McDougall (Epic Software Team, Children’s Hospital Colorado) provided technical support in translating the obesity growth tables into new growth charts. Tia Brayman (Department of Photography, Children’s Hospital Colorado) provided technical support increasing resolution of the figures.
Glossary
- CDC
Centers for Disease Control and Prevention
- LMS
lamba-μ-σ
Footnotes
Dr Gulati conceptualized the new nomenclature and growth chart, created the excel data spreadsheet to develop the new growth charts, created and implemented the resident surveys, drafted the initial manuscript and revisions, and approved the final manuscript as written; Dr Kaplan conceptualized the new nomenclature and growth chart, worked with the information technology division to develop the new growth chart within the electronic medical record, reviewed and revised the manuscript, and approved the final manuscript as submitted; and Dr Daniels conceptualized the new nomenclature and growth chart, critically reviewed the manuscript, and approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: Dr Daniels has received funds for a consultancy for Merck, QLT, which is unrelated to the current work; Drs Gulati and Kaplan have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: No external funding.
References
- 1.Freedman DS, Mei Z, Srinivasan SR, Berenson GS, Dietz WH. Cardiovascular risk factors and excess adiposity among overweight children and adolescents: the Bogalusa Heart Study. J Pediatr. 2007;150(1):12–17, e2 [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Kuczmarski RJ, Flegal KM, et al. Centers for Disease Control and Prevention 2000 growth charts for the United States: improvements to the 1977 National Center for Health Statistics version. Pediatrics. 2002;109(1):45–60 [DOI] [PubMed] [Google Scholar]
- 3.Woo JG. Using body mass index Z-score among severely obese adolescents: a cautionary note. Int J Pediatr Obes. 2009;4(4):405–410 [DOI] [PubMed] [Google Scholar]
- 4.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat 11. 2002;246(246):1–190 [PubMed] [Google Scholar]
- 5.Cole TJ. The LMS method for constructing normalized growth standards. Eur J Clin Nutr. 1990;44(1):45–60 [PubMed] [Google Scholar]
- 6.Cole TJ, Green PJ. Smoothing reference centile curves: the LMS method and penalized likelihood. Stat Med. 1992;11(10):1305–1319 [DOI] [PubMed] [Google Scholar]
- 7.Flegal KM, Wei R, Ogden CL, Freedman DS, Johnson CL, Curtin LR. Characterizing extreme values of body mass index-for-age by using the 2000 Centers for Disease Control and Prevention growth charts. Am J Clin Nutr. 2009;90(5):1314–1320 [DOI] [PubMed] [Google Scholar]