Abstract
A goal of the Minority Institution/Cancer Center Partnership between the Ponce School of Medicine in Puerto Rico and the H. Lee Moffitt Cancer Center & Research Institute in Florida is to provide cross-cultural training in cancer research. This is achieved through a collaborative summer exchange program, which provides US students with an opportunity to conduct research in Puerto Rico. As part of this program, students recruited participants and collected data for a study to enhance the understanding of sociocultural factors among Puerto Rican women regarding genetic testing for hereditary breast/ovarian cancer. Limited studies have examined cancer genetics issues among Latinos, particularly those specific to the various Latino subgroups, such as Puerto Ricans. As a result of the student training experience, culturally appropriate strategies for the recruitment of women in Puerto Rico have been identified. These recommendations can inform the design of cancer research projects and interventions targeting the Puerto Rican population.
Keywords: Cross-cultural research, Underserved populations, Puerto Rico, Latino health, Breast cancer, Genetic testing for cancer
Introduction
Latinos are the fastest growing ethnic group within the USA [1]. It is projected that the Latino population will grow from 12.5% in 2000 to 25% by the year 2050 [1, 2]. Latinos are an ethnic and racially diverse group, with origins throughout Central and South America, the Caribbean, and Spain [2]. Although ubiquitously referenced as a single ethnic group within the USA, Latinos are a heterogeneous group with variances in history, traditions, and sociocultural practices and norms rooted in their country of origin [1, 3]. For example, Puerto Ricans have been US citizens since 1917, which has resulted in their increased exposure to US culture [4]. As such, Puerto Ricans are differentiated from other Latino subgroups [1, 5], and these differences may influence their understanding and interpretation of health issues.
Latinos have lower cancer incidence and mortality, as compared to non-Hispanic whites [3, 6]. However, they tend to be diagnosed at a more advanced stage, which affects treatment outcomes, including differences in survival rates [6]. The reported cancer statistics, which present aggregate data on Latino health, camouflage the variation of cancer incidence among the different subpopulations, such as Puerto Ricans [3, 6]. A recent study by Pinheiro and colleagues illustrated that Puerto Ricans have the highest cancer rates of any Latino subpopulation [3].
In Puerto Rico, breast cancer is the most commonly diagnosed cancer among women, accounting for one third (33.0%) of all female cancers between 1999 and 2003 [7]. It is estimated that approximately 1,500 women in Puerto Rico are diagnosed with invasive breast cancer annually, whereas about 363 women die from breast cancer each year [7]. The age-adjusted incidence rate for breast cancer is 78.0 per 100,000 women per year [7]. Roughly one in 13 women in Puerto Rico will be diagnosed with breast cancer during her lifetime [7]. Trend data in Puerto Rico over the period of 1987 to 2004 show that the breast cancer incidence rate among females increased by approximately 1.8% annually, yet the mortality rates decreased by 0.3% [7]. The majority of Puerto Rican women are diagnosed with breast cancer between the ages of 55 and 64 (25.3%), with a median age of 59 years [7].
Recent advances in molecular genetics have helped to identify women who are at increased genetic risk for developing hereditary breast and ovarian cancer (HBOC). Specifically, several recent studies have documented the presence of BRCA mutations in US-based samples of Latinas [8–10]. Even though only 10% of cancers are attributable to hereditary cancer predisposition syndromes, women with HBOC have a 55–85% lifetime risk of developing a primary breast cancer and 15–60% risk of developing ovarian cancer [11–15]. Additionally, BRCA mutation carriers have a 40–60% lifetime risk for a second breast cancer [16–18].
A population-based study conducted in California reported that Latinas with a personal history of breast cancer have the highest prevalence of BRCA1 mutations when compared to women of other minority racial/ethnic minority groups (i.e., African American, Asian American) [19]. Coupled with the growing body of evidence supporting the efficacy of prophylactic surgery [20–23] and chemopreventive agents [24] in reducing the risk of breast and ovarian cancers in mutation carriers, genetic counseling and testing for BRCA mutations are important ways to identify those women most likely to benefit from early detection and prevention strategies to minimize cancer-related morbidity and mortality. However, recent studies suggest that cancer genetic services are underutilized within the Latino community [25–27].
While review papers identify a critical need for and use of genetic counseling and testing services among Latinas [28–30], there is nominal empirical data about factors that may contribute to utilization of these services within this community. Minimal research has been conducted to assess awareness about the availability of or interest in genetic testing for BRCA mutations among Latinas in the USA [31–37]. Furthermore, very little is known about these issues among women in Puerto Rico as most research has examined related knowledge, attitudes, and practices among Latinas in aggregate rather than by subethnicity. An underlying factor in the lack of research may be challenges experienced in the recruitment and retention of Latinas in cancer genetics studies.
Given the health disparities experienced by Latinos and their disproportionate participation in cancer prevention and treatment trials [38–42], enhancing the recruitment and retention of Latinos in cancer research has been prioritized by the National Cancer Institute [40]. The involvement of Latinos in cancer research is limited, in part, due to the lack of trained minority researchers and mentors [38, 43]. Furthermore, among non-Latino researchers, there may be minimal knowledge, training, and exposure regarding cultural differences, particularly regarding subethnicities and subcultures among Latinos [43]. These deficiencies among researchers result in the failure to develop and implement culturally appropriate interventions, studies, and instruments [43], which may be partially attributable for the underrepresentation of Latinos in cancer research [42, 43].
As part of the National Cancer Institute’s Minority Institution/Cancer Center Partnership program, the Ponce School of Medicine (PSM) in Puerto Rico and the H. Lee Moffitt Cancer Center & Research Institute (MCC) in Florida conducted a pilot study to better understand knowledge, attitudes, and interest related to genetic counseling and testing for HBOC. The current paper describes the challenges and lessons learned during the process of recruiting Puerto Rican women at increased risk for HBOC for a formative research study. The goal of the paper is to identify recruitment challenges faced by recruiters on the study team. The information from this study provides practical guidance for future efforts to recruit women to research studies based in Puerto Rico.
Methods
The PSM/MCC Partnership aims to build and enhance cancer research, training, and outreach programs at both institutions and to expand cancer health disparities research. One of the core areas of this collaborative initiative is the Cancer Education and Training program, which develops training and education activities for medical and graduate health students at PSM and the University of South Florida (USF—the partnering university with MCC). An ongoing student training opportunity has been a summer exchange program, in which graduate students in public health or medicine at USF can participate in a 4- to 8-week rotation at PSM. For the duration of the summer, students are paired with an investigator at the partner institution to guide and facilitate all aspects of this experiential learning program. Student participants facilitate research studies, which provide them with practical training and experience, particularly within resource-limited, underserved areas of Puerto Rico.
As part of the summer exchange program, a group of students worked in collaboration with researchers in Puerto Rico to collect data for the replication of a mixed method study that was previously conducted in Florida. This study applied social marketing principles to improve knowledge and awareness of cancer genetics among Latinos [31, 36, 37]. The team in Puerto Rico utilized this study as a prototype to guide the design and implementation of formative research, which sought to enhance understanding of cultural factors that may impact the utilization of BRCA testing for HBOC among Puerto Rican women living on the island.
The student research team consisted of three females with prior experience conducting qualitative research within Latino communities. Of the three students, two were public health graduate students (one masters level and the other was a doctoral candidate), while one was a medical student. Two were of Puerto Rican descent and fluent in both Spanish and English, while the third was a US-born, minority student who spoke conversational Spanish. Prior to departure, this student participated in supplemental Spanish language training.
Study Design
Upon receipt of Institutional Review Board approval from the Ponce School of Medicine, the students worked over a 4-week period to recruit a minimum of 20 women in Puerto Rico who met the following inclusion criteria: Puerto Rican women between the ages of 21 and 65 who had personally experienced breast cancer before the age of 50 or ovarian cancer at any age or had a first-degree relative (i.e., mother, sister, or daughter) with a history of these types of cancer. Eligible women were invited to participate in a 45–90-min in-person, semi-structured interview and were given the option of having the interview conducted in English or Spanish. These interviews were designed to elucidate the community’s knowledge and awareness of genetic testing and counseling for breast and/or ovarian cancer. In addition to the interview, the participants were requested to complete a quantitative questionnaire that collected demographic information, as well as knowledge and attitudes regarding cancer and genetic counseling and testing. The women were provided with $40 gift cards from a popular retail company as compensation for the time and participation in the study.
Multiple recruitment strategies were utilized for the study. Local community advocates assisted in word-of-mouth promotion of the study, as well as the establishment of linkages with support groups and local health care facilities. Additionally, research staff collaborated with the local affiliates of the American Cancer Society, community hospitals, and radiology offices to identify eligible women. Flyers specific to the study were developed and disseminated through these partner organizations and through community advocates. Interested women were prescreened over the phone using a brief questionnaire to determine eligibility and availability. Additionally, information regarding how they learned of the study was obtained.
Training of Researchers
The student researchers were provided with funding and resources to conduct data collection over a 4-week period of the summer exchange program in Puerto Rico. Prior to initiating the research study, the students were required to complete training in human subjects protections and were introduced to the informed consent procedures and forms created for the study (available in Spanish and English). Additionally, the students participated in a comprehensive training on qualitative research methodologies and completed an orientation to familiarize them with the study protocol and instruments.
Observational Learning
Throughout the duration of the summer exchange program, the student researchers maintained personal journals to log their reflections and experiences. Furthermore, the students participated in weekly debriefing sessions with their mentors in Puerto Rico. These activities provided a framework for the development and enhancement of appropriate and effective recruitment strategies for women in Puerto Rico. This informal observational process aided in the interpretation of study findings.
Results
Over the project period, a total of 49 women were prescreened by the student research team to participate in the study in Puerto Rico. A total of 14 women were found ineligible to participate in the study. The most common reason for ineligibility was that the personal or family breast cancer diagnosis occurred after the age of 50. Other reasons were that the reported family history of cancer was not in the woman’s mother, sister, or daughter; the woman was above the age of 65; or the woman reported that she had previously participated in genetic counseling and testing. The remaining 35 women were found to be eligible and expressed interest; however, only the first 25 eligible respondents were interviewed due to limited funding for additional interviews. Of these 25 interviews, roughly half (48%) were recruited from the greater San Juan area (the capital of Puerto Rico), while the remainder (52%) were from the southern region of Puerto Rico. Nearly half of the women were diagnosed with breast cancer when younger than age 50 (48%), whereas one third (32%) had a first-degree relative with this diagnosis. Ovarian cancer was more rare, with 12% of participants recounting a personal history of the disease and 8% reporting the diagnosis of a first-degree relative. Of the interviewees, only one (4%) chose to have the interview conducted in English, with the overwhelming majority (96%) preferring to communicate in Spanish.
Among the 49 women who were prescreened for the study, 16 (32.7%) reported that they received an email notification of the study, which originated from a local community advocate. Nearly one fourth (22.4%) were directly recruited by a community advocate. Other recruitment measures reported by the women, in order of frequency, include referral by: a friend (12.2%); any of the Puerto Rican branches of the American Cancer Society (10.2%); family members (8.2%); radiologists (4.1%); and flyers (4.1%). The remainder (6.1%) did not report how they learned of the study.
Lessons Learned
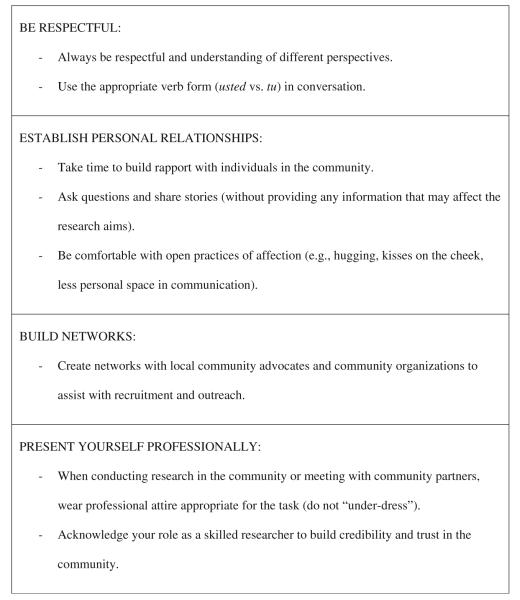
Over the course of the project period, multiple sociocultural cues were noted through the implementation of the formative research study to examine factors related to the utilization of genetic testing for hereditary breast–ovarian cancer. These sociocultural observations played an important role in the recruitment of Puerto Rican women for the study. Overall, the lessons learned resulted in the identification of core approaches that may be beneficial in the design of psychosocial, epidemiological, and clinical studies in Puerto Rico (Fig. 1).
Fig. 1.
Recommendations for conducting culturally appropriate research in Puerto Rico
Social Interactions and Interpersonal Communication
The experiences gleaned while conducting research within the Puerto Rican community illustrate that social interaction and communication are a central representation of Puerto Rican culture. It was observed that verbal communication was frequently accompanied by noteworthy nonverbal cues, such as physical proximity, touching, and emotional expression. In-person interactions were found to be preferential to other forms of communication, such as flyers or emails, as the most success in participant recruitment was experienced through visits to support groups and personal conversations with community advocates and representatives of local partnering organizations. Additionally, verbal and nonverbal expressions of affection, care, and kindness (e.g., hugging, kisses on the cheek, and terms of endearment) were frequently initiated and expected both by community advocates and participants. For example, the interviewers were often greeted with a hug or kiss on the cheek, and interviews were closed in a similar fashion, with the addition of colloquial phrases, such as “besitos” (i.e., kisses in Spanish).
Network Building
Partnership with key community advocates was an essential component of the recruitment process. Specifically, breast cancer advocates were helpful in the recruitment and identification of women for the study. By using advocates as the primary source for communicating information about the study—either through internet-based promotion (i.e., emails and listservs) and word of mouth—the research team was able to efficiently identify women who were eligible for the study. In addition, because advocates served as a conduit between the community and the research team, they delivered information about the study in a manner that would be easily understood and acceptable to the community.
Of the various methods employed, word of mouth through community networks was the most effective recruitment strategy. Minimal responses were obtained following posting of promotional flyers, and email announcements were only effective when distributed by known community advocates. Roughly one third of our participants learned of the study through an email from a community advocate. Participants reported that they were more willing to call about the study because they received information from either a friend or a trusted person in the community rather than just seeing a flyer.
Professionalism
Despite the importance of personal relationships within Puerto Rican culture, it was observed that professionalism is still expected. Respect for others should be relayed through more deferential language, principally through the use of the more formal verb form (usted rather than tu) in the Spanish language. This is particularly important when conversing with those considered to be in positions of authority or of a higher social status due to older age, senior employment position, or education. This was evidenced by individual conversations with community advocates and partners in Puerto Rico, who emphasized the importance of this practice throughout the recruitment and interview process.
When interacting with the community during the execution of research activities, attire appropriate for professional encounters was considered to be essential. On a daily basis, it is customary for individuals to take great care and consideration in their presentation and appearance, regardless of socioeconomic status. This was observed through recruitment activities throughout the community, as well as daily interactions with community members. Furthermore, for student researchers, it was found that their role as researchers should be prioritized above their role as students, as this contributes to their credibility and aids in establishing trust and confidence in the study and their capabilities. In other words, it was important for the student researchers to introduce themselves as researchers working in collaboration with community partners rather than students.
Discussion
The experiences acquired through the cross-cultural implementation of formative research in Puerto Rico illustrate that relationship building and networking are essential to the success of community-based research initiatives. With sufficient groundwork, the Puerto Rican community may be more responsive and communicative within research studies. Therefore, ample time should be allocated for this rapport building process, which should include collaborations with local community advocates and organizations.
Researchers from external organizations may experience resistance as “outsiders” without the partnership and support of key collaborators. Community advocates have been found to be essential in community-based research. Such individuals can help build bridges between the study and the community, allowing for the transfer of credibility and trust that will support the study’s initiation and growth. These relationships can be leveraged to expand the community network, which is beneficial in participant recruitment and attendance. For example, word of mouth through community networks has been found to be a highly effective recruitment strategy in Puerto Rico; flyers were ineffective.
Subsequent to networking and relationship building, qualitative research strategies may yield rich information, with participants sharing detailed accounts of their experiences. To conduct study outcomes and processes, adequate time should be allocated within qualitative data collection settings (i.e., focus groups, interviews) for opening (ice-breaker) questions and concluding statements. Conversely, when providing health information and creating educational materials, the depiction and sharing of stories to convey health messages may be an effective strategy. Furthermore, in-person education and communication is favored to web-based or media-centered interventions.
Conclusions
Although there is growing recognition of the importance of public health strategies that address the various subgroups of the Latino population, limited interventions and research studies have fully integrated this approach. The PSM/MCC Partnership has been established as a long-term initiative to address cancer disparities among Puerto Ricans. The summer exchange program offered by the partnering institutions provides health professions students with a process to develop their capacity to work cross-culturally and to enhance their research skills.
The lessons learned from the research team’s ongoing experience in the development of culturally appropriate research in Puerto Rico mirrors previous findings regarding culturally competent approaches among Latinos. For example, traditional values of respect, personal familiarity and relationships, and trust were identified as critical for working with Latino populations [6]. These findings provide concrete guidance for the development and implementation of culturally appropriate research within the Puerto Rican context.
As the recommendations provided within this paper are based on the experiences of a subset of student participants in the summer exchange program, this framework may not be universally appropriate or applicable to all community-based research in Puerto Rico. Additionally, the student perspectives may be influenced by their individual backgrounds and previous experiences with research and in cross-cultural settings. Consequently, further analysis of critical factors that influence research design in Puerto Rico is recommended.
Acknowledgments
Funding for this project was provided by Grant 1 R03 HG003887 from the National Human Genome Research Institute and by NIH U56 10-14352-03-07. The work contained within this publication was supported in part by the Survey Methods Core Facility at Moffitt Cancer Center. We would also like to thank Ms. Carmen Pacheco and Mr. Juan Carlos Vega for their assistance with recruitment in Puerto Rico.
Contributor Information
Euna M. August, Health Outcomes & Behavior Program, H. Lee Moffitt Cancer Center & Research Institute, 12902 Magnolia Drive, Tampa, FL 33612, USA; College of Public Health, Department of Community & Family Health, University of South Florida, Tampa, FL, USA
Gwen P. Quinn, Health Outcomes & Behavior Program, H. Lee Moffitt Cancer Center & Research Institute, 12902 Magnolia Drive, Tampa, FL 33612, USA
Rossybelle Perales, Health Outcomes & Behavior Program, H. Lee Moffitt Cancer Center & Research Institute, 12902 Magnolia Drive, Tampa, FL 33612, USA.
Zuheily Closser, University of South Florida, College of Medicine, Tampa, FL, USA.
Julie Dutil, Department of Biochemistry, Ponce School of Medicine, Ponce, PR, USA.
Marieva Puig, University of Puerto Rico, Bayamon, PR, USA.
Susan T. Vadaparampil, Health Outcomes & Behavior Program, H. Lee Moffitt Cancer Center & Research Institute, 12902 Magnolia Drive, Tampa, FL 33612, USA
References
- 1.Gonzalez-Burchard E, Borrell LN, Choudhry S, Naqvi M, Tsai H, Rodriguez-Santana JR, Chapela R, et al. Latino populations: a unique opportunity for the study of race, genetics, and social environment in epidemiological research. American Journal of Public Health. 2005;95:2161–2168. doi: 10.2105/AJPH.2005.068668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Solomon FM, Eberl-Lefko AC, Michaels M, Macario E, Tesauro G, Rowland JH. Development of a linguistically and culturally appropriate booklet for Latino cancer survivors: lessons learned. Heal Promot Pract. 2005;6(4):405–413. doi: 10.1177/1524839905278447. [DOI] [PubMed] [Google Scholar]
- 3.Pinheiro PS, Sherman RL, Trapido EJ, Fleming LE, Huang Y, Gomez-Marin O, Lee D. Cancer incidence in first generation US Hispanics: Cubans, Mexicans, Puerto Ricans, and New Latinos. Cancer Epidemiology, Biomarkers & Prevention. 2009;18(8):2162–2169. doi: 10.1158/1055-9965.EPI-09-0329. [DOI] [PubMed] [Google Scholar]
- 4.Puerto Rico USA Citizenship Foundation [Accessed 14 Feb 2011];View of Congress, the Courts and the Federal Government. 1998 http://www.puertoricousa.com/english/english_menu_views.htm.
- 5.Torres MI, Marquez DX, Carbone ET, Stacciarini JR, Foster JW. Culturally responsive health promotion in Puerto Rican communities: a structuralist approach. Heal Promot Pract. 2008;9(2):149–158. doi: 10.1177/1524839907307675. [DOI] [PubMed] [Google Scholar]
- 6.American Cancer Society [Accessed 23 Jun 2010];Cancer facts & figures for Hispanics/Latinos 2009-2011. 2010 http://www.cancer.org/downloads/STT/FF_Hispanics_Latinos_2009_2011.pdf.
- 7.Puerto Rico Central Cancer Registry [Accessed 22 Jun 2010];Stat fact sheet: cancer of the breast. 2008 http://www.salud.gov.pr/RCancer/Reports/Documents/Hojas%20informativas/Mama.pdf.
- 8.Mullineaux LG, Castellano TM, Shaw J, Axell L, Wood ME, Diab S, et al. Identification of germline 185delAG BRCA1 mutations in non-Jewish Americans of Spanish ancestry from the San Luis Valley, Colorado. Cancer. 2003;98(3):597–602. doi: 10.1002/cncr.11533. [DOI] [PubMed] [Google Scholar]
- 9.Weitzel JN, Lagos V, Blazer KR, Nelson R, Ricker C, Herzog J, et al. Prevalence of BRCA mutations and founder effect in high-risk Hispanic families. Cancer Epidemiol Biomarkers Prev. 2005;14(7):1666–1671. doi: 10.1158/1055-9965.EPI-05-0072. [DOI] [PubMed] [Google Scholar]
- 10.Weitzel JN, Lagos VI, Herzog JS, Judkins T, Hendrickson B, Ho JS, et al. Evidence for common ancestral origin of a recurring BRCA1 genomic rearrangement identified in high-risk Hispanic families. Cancer Epidemiol Biomarkers Prev. 2007;16(8):1615–1620. doi: 10.1158/1055-9965.EPI-07-0198. [DOI] [PubMed] [Google Scholar]
- 11.Carter RF. BRCA1, BRCA2 and breast cancer: a concise clinical review. Clin Invest Med. 2001;24(3):147–157. [PubMed] [Google Scholar]
- 12.MacDonald DJ, Choi J, Ferrell B, Sand S, McCaffrey S, Blazer KR, et al. Concerns of women presenting to a comprehensive cancer centre for genetic cancer risk assessment. J Med Genet. 2002;39(7):526–530. doi: 10.1136/jmg.39.7.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Robson ME, Boyd J, Borgen PI, Cody HS. Hereditary breast cancer. Curr Probl Surg. 2001;38(6):387–480. [PubMed] [Google Scholar]
- 14.Tonin PN. Genes implicated in hereditary breast cancer syndromes. Semin Surg Oncol. 2000;18(4):281–286. doi: 10.1002/(sici)1098-2388(200006)18:4<281::aid-ssu2>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 15.Verhoog LC, Brekelmans CT, Seynaeve C, van den Bosch LM, Dahmen G, van Geel AN. Survival and tumour characteristics of breast-cancer patients with germline mutations of BRCA1. Lancet. 1998;351(9099):316–321. doi: 10.1016/s0140-6736(97)07065-7. [DOI] [PubMed] [Google Scholar]
- 16.Ford D, Easton DF, Bishop DT, Narod SA, Goldgar DE. Risks of cancer in BRCA1-mutation carriers. Breast Cancer Linkage Consortium. Lancet. 1994;343(8899):692–695. doi: 10.1016/s0140-6736(94)91578-4. [DOI] [PubMed] [Google Scholar]
- 17.Metcalfe K, Lynch HT, Ghadirian P, Tung N, Olivotto I, Warner E, et al. Contralateral breast cancer in BRCA1 and BRCA2 mutation carriers. J Clin Oncol. 2004;22(12):2328–2335. doi: 10.1200/JCO.2004.04.033. [DOI] [PubMed] [Google Scholar]
- 18.Robson M, Svahn T, McCormick B, Borgen P, Hudis CA, Norton L, et al. Appropriateness of breast-conserving treatment of breast carcinoma in women with germline mutations in BRCA1 or BRCA2: a clinic-based series. Cancer. 2005;103(1):44–51. doi: 10.1002/cncr.20728. [DOI] [PubMed] [Google Scholar]
- 19.John EM, Miron A, Gong G, Phipps AI, Felberg A, Frederick P, et al. Prevalence of pathogenic BRCA1 mutation carriers in 5 US racial/ethnic groups. JAMA. 2007;298(24):2869–2876. doi: 10.1001/jama.298.24.2869. [DOI] [PubMed] [Google Scholar]
- 20.Hartmann LC, Schaid DJ, Woods JE, Crotty TP, Myers JL, Arnold PG, et al. Efficacy of bilateral prophylactic mastectomy in women with a family history of breast cancer. N Engl J Med. 1999;340(2):77–84. doi: 10.1056/NEJM199901143400201. [DOI] [PubMed] [Google Scholar]
- 21.Hartmann LC, Sellers TA, Schaid DJ, Frank TS, Soderberg CL, Sitta DL, et al. Efficacy of bilateral prophylactic mastectomy in BRCA1 and BRCA2 gene mutation carriers. J Natl Cancer Inst. 2001;93(21):1633–1637. doi: 10.1093/jnci/93.21.1633. [DOI] [PubMed] [Google Scholar]
- 22.Meijers-Heijboer EJ, Verhoog L, Brekelmans C, van Geel CA, Seynaeve C, van den Ouweland A, et al. Bilateral prophylactic mastectomy in BRCA1/2 mutation carriers: predictive factors and follow-up. Am J Hum Genet. 1999;65:A22. [Google Scholar]
- 23.Rebbeck TR, Friebel T, Lynch HT, Neuhausen SL, van’t Veer L, Garber JE, et al. Bilateral prophylactic mastectomy reduces breast cancer risk in BRCA1 and BRCA2 mutation carriers: the PROSE Study Group. J Clin Oncol. 2004;22(6):1055–1062. doi: 10.1200/JCO.2004.04.188. [DOI] [PubMed] [Google Scholar]
- 24.Gronwald J, Tung N, Foulkes WD, Offit K, Gershoni R, Daly M, et al. Tamoxifen and contralateral breast cancer in BRCA1 and BRCA2 carriers: an update. Int J Cancer. 2006;118(9):2281–2284. doi: 10.1002/ijc.21536. [DOI] [PubMed] [Google Scholar]
- 25.Chen WY, Garber JE, Higham S, Schneider KA, Davis KB, Deffenbaugh AM, et al. BRCA1/2 genetic testing in the community setting. J Clin Oncol. 2002;20(22):4485–4492. doi: 10.1200/JCO.2002.08.147. [DOI] [PubMed] [Google Scholar]
- 26.Hall MJ, Reid JE, Burbidge LA, Pruss D, Deffenbaugh M, Frye C, et al. BRCA1 and BRCA2 mutations in women of different ethnicities undergoing testing for hereditary breast-ovarian cancer. Cancer. 2009;115(10):2222–2233. doi: 10.1002/cncr.24200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ricker C, Lagos V, Feldman N, Hiyama S, Fuentes S, Kumar V, et al. If we build it … will they come?—establishing a cancer genetics services clinic for an underserved predominantly Latina cohort. J Genet Couns. 2006;15(6):505–514. doi: 10.1007/s10897-006-9052-5. [DOI] [PubMed] [Google Scholar]
- 28.Penchaszadeh VB. Genetic counseling issues in Latinos. Genet Test. 2001;5(3):193–200. doi: 10.1089/10906570152742236. [DOI] [PubMed] [Google Scholar]
- 29.Ramirez AG. Hispanic/Latino Genetics Community Consultation Network (HLGCCN) Summit Report 2003. Redes En Accion; San Antonio, TX: [Accessed 30 Jun 2010]. 2003. http://www.redesenaccion.org/ [Google Scholar]
- 30.Doksum T, Joseph C, Watson M, Leighna Kim SM, Brand A. Genetics education and underserved populations: summary of the literature. Abt Associates, Inc.; Cambridge: 2004. [Google Scholar]
- 31.Vadaparampil ST, McIntyre J, Quinn GP. Awareness, perceptions, and provider recommendation related to genetic testing for hereditary breast cancer risk among at-risk Hispanic women: similarities and variations by sub-ethnicity. J Genet Couns. 2010;19(6):618–629. doi: 10.1007/s10897-010-9316-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ramirez AG, Aparicio-Ting FE, de Majors SS, Miller AR. Interest, awareness, and perceptions of genetic testing among Hispanic family members of breast cancer survivors. Ethn Dis. 2006;16(2):398–403. [PubMed] [Google Scholar]
- 33.Lacour RA, Daniels MS, Westin SN, Meyer LA, Burke CC, Burns KA, et al. What women with ovarian cancer think and know about genetic testing. Gynecol Oncol. 2008;111(1):132–136. doi: 10.1016/j.ygyno.2008.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vadaparampil ST, Wideroff L, Breen N, Trapido E. The impact of acculturation on awareness of genetic testing for increased cancer risk among Hispanics in the year 2000 National Health Interview Survey. Cancer Epidemiology, Biomarkers & Prevention. 2006;15(4):618–623. doi: 10.1158/1055-9965.EPI-05-0378. [DOI] [PubMed] [Google Scholar]
- 35.Kinney AY, Gammon A, Coxworth J, Simonsen SE, Arce-Laretta M. Exploring attitudes, beliefs, and communication preferences of Latino community members regarding BRCA1/2 mutation testing and preventive strategies. Genet Med. 2010;12(2):105–115. doi: 10.1097/GIM.0b013e3181c9af2d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Quinn GP, McIntyre J, Vadaparampil ST. Preferences for hereditary breast and ovarian cancer information among Mexican, Cuban and Puerto Rican women at risk. Public Health Genomics. 2011;14:248–258. doi: 10.1159/000284582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vadaparampil ST, Quinn GP, Small BJ, McIntyre J, Loi CA, Closser Z, Gwede CK. A pilot study of hereditary breast and ovarian knowledge among a multiethnic group of Hispanic women with a personal or family history of cancer. Genetic Testing and Molecular Biomarkers. 2010;14(1):99–106. doi: 10.1089/gtmb.2009.0088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Larkey LK, Gonzalez JA, Mar LE, Glantz N. Latina recruitment for cancer prevention education via Community Based Participatory Research strategies. Contemp Clin Trials. 2009;30(1):47–54. doi: 10.1016/j.cct.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 39.Murthy VH, Krumholz HM, Gross CP. Participation in cancer clinical trials: race-, sex-, and age-based disparities. JAMA. 2004;291(22):2720–2726. doi: 10.1001/jama.291.22.2720. [DOI] [PubMed] [Google Scholar]
- 40.Ramirez AG, Talavera GA, Marti J, Penedo FJ, Medrano MA, Giachello AL. Redes En Acción. Increasing Hispanic participation in cancer research, training, and awareness. Cancer. 2006;107(8):2023–2033. doi: 10.1002/cncr.22148. [DOI] [PubMed] [Google Scholar]
- 41.Yancey AK, Ortega AN, Kumanyika SK. Effective recruitment and retention of minority research participants. Annu Rev Public Health. 2006;27:1–28. doi: 10.1146/annurev.publhealth.27.021405.102113. [DOI] [PubMed] [Google Scholar]
- 42.Sheppard VB, Cox LS, Kanamori MJ, Cañar J, Rodríguez Y, Goodman M, et al. Brief report: if you build it, they will come: methods for recruiting Latinos into cancer research. J Gen Intern Med. 2005;20(5):444–447. doi: 10.1111/j.1525-1497.2005.0083.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lange JW. Methodological concerns for non-Hispanic investigators conducting research with Hispanic Americans. Res Nurs Health. 2002;25(5):411–419. doi: 10.1002/nur.10049. [DOI] [PubMed] [Google Scholar]