Abstract
It is becoming evident that B-cell responses to particular epitopes or in particular contexts can be highly convergent at the molecular level. That is, depending on the epitope targeted, persons of diverse genetic backgrounds and immunological histories can use highly similar, stereotyped B-cell receptors (BCRs) for a particular response. In some cases, multiple people with immunity to a particular epitope or with a type of B-cell neoplasia will elicit antibodies encoded by essentially identical immunoglobulin gene rearrangements. In other cases, particular VH genes encode antibodies important for immunity against pathogens such as influenza and HIV. It appears that the conserved antibody structures driving these stereotyped responses are highly limited and selected. There are interesting and important convergences in the types of stereotyped BCRs induced in conditions of immunity and B-cell-related pathology such as cancer and autoimmunity. By characterizing and understanding stereotyped B-cell responses, novel approaches to B-cell immunity and in understanding the underlying causes of B-cell pathology may be discovered. In this paper, we will review stereotyped BCR responses in various contexts of B-cell immunity and pathology.
Keywords: immunoglobulin, B cell, variable gene
1. Introduction
It has long been appreciated that immunization of particular mouse strains with simple hapten antigens such as arsenate (Ars) [1–5] or 4-hydroxy-3-nitrophenylacetyl (NP) [6–9] would induce canonical immunoglobulin responses; that is, responses that induce essentially identical immunoglobulins from different mice, despite the massive potential diversity of VDJ rearrangement. For example, B-cell responses of C57BL/6 mice to NP select for canonical antibodies encoded by V186.2 recombined to DFI 16.1 D segment and the JH1 J segment that are paired with Vλ1 light chains. It had been assumed that the simplistic nature of the hapten antigens in combination with the inbred mice led to the highly limited possibilities to generate anti-NP antibodies, and thus the canonical immunoglobulins. Thus, it has been surprising in recent years to observe stereotyped responses with highly similar immunoglobulins in humans, despite having highly unique genetic backgrounds, diverse immunological histories and against complex antigens. Notably, however, most of these stereotyped responses resemble in a number of ways the canonical responses of inbred mice. That is, although the entire antigen molecules targeted are complex, the stereotyped responses typically target small discrete individual epitopes (when the epitopes have been identified). Thus even in complex outbred immune responses, certain epitopes are so unique that there are likely few means in which a human antibody can be formed from variable genes to target these epitopes.
Importantly, a number of these stereotyped responses have been identified because the antibodies bind conserved epitopes on pathogens that can escape immune protection because they are highly adaptable, including human immunodeficiency virus (HIV), influenza virus, hepatitis C virus (HCV) and malaria. Further, there are stereotyped immunoglobulin responses that are associated with B-cell cancers, neoplasms and with autoimmune diseases that may provide insight into the underlying causes of B-cell pathology or novel treatment options. Strikingly, there are commonalities between both the stereotyped protective responses to infectious diseases and to the neoplastic and autoimmune diseases, such as a tendency to use a particular immunoglobulin heavy chain variable region gene: VH1-69. Another type of stereotyped immunoglobulin occurs in discrete B-cell subpopulations. Elucidation of the specificity of these stereotyped responses will provide insights into the function of these types of B cells. In this article, we will discuss various examples of stereotyped immunoglobulin responses that occur in humans and speculate on the causes of these responses.
2. Molecular characteristics of stereotyped B-cell receptors
Stereotyped B-cell receptors (BCRs) as described herein refer to B cells from different individuals that share characteristic sequence elements. On one end of the spectrum, these characteristics can be a tendency to be encoded by a particular variable gene with little other to distinguish the receptors. This is often the case with antibodies to conserved epitopes on viruses, for example, or for BCR tendencies expressed by particular functional subsets of differentiated B cells. On the other end of the spectrum are antibodies with almost identical usage of variable, diversity and junctional gene segment rearrangements and even highly selected particular somatic hypermutations, but isolated from various people. Such receptors have been noted for certain B-cell lymphomas, for example. Most of the examples of stereotyped receptors described fall somewhere between these two extremes, with tendencies of B cells from different individuals having similar variable genes and also other characteristic amino acids introduced by usage of particular D or J gene segments, by junctional diversity, or by somatic hypermutation. In general, one can consider as stereotyped B cells with similar immunoglobulins that have undergone convergent selection for a particular response or associated with a subset or condition.
3. B-cell subpopulations can express stereotyped B-cell receptors
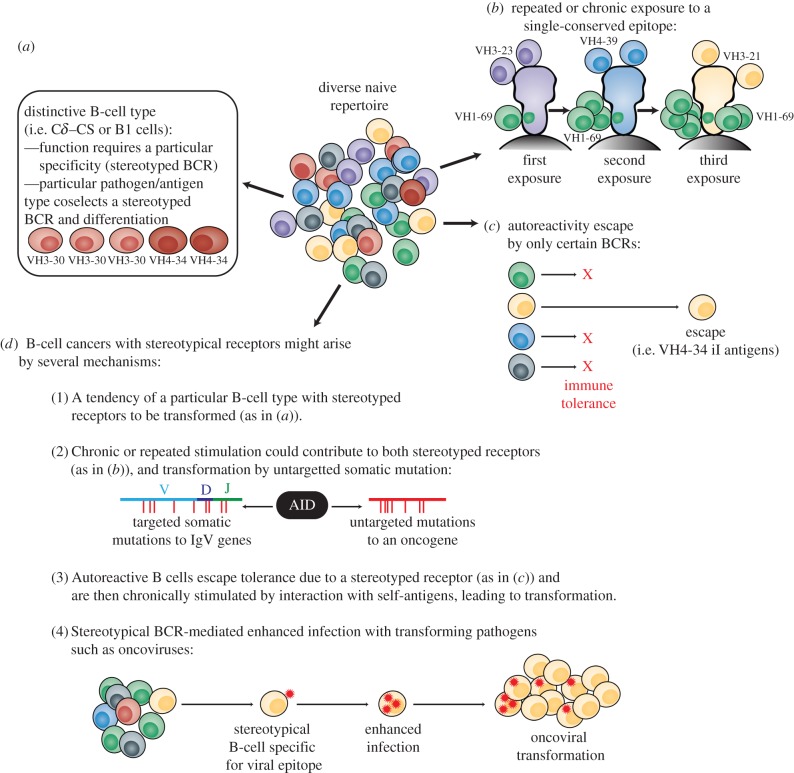
It has long been appreciated that certain B-cell subpopulations in mice, such as B1 cells, have stereotyped BCRs. For B1 cells, it is known that the cells encode antibodies that are more analogous to pattern recognition receptors such as Toll-like receptors. Thus, these populations are often referred to as innate-like B cells. The stereotyped BCRs likely bind to ‘natural epitopes’; that is, epitopes which particular variable genes have evolved to recognize. An example is bacterial phosphorylcholine bound by the T15 idiotype encoded by stereotyped VH1 and Vk22 heavy and light chains [10,11]. It is not clear if B1 cells develop with preferential rearrangements of particular BCRs or if B cells with particular BCRs will interact with bacteria or with a ‘self’ molecule and then be driven to differentiate into B1 cells (figure 1a). Notably, insertion of a BCR transgene from a B1 B cell so that all B cells in the mouse express that single specificity, causes most of the B cells to mature as B1 cells [12]. Thus, B1 cell specificity appears to drive its differentiation.
Figure 1.
Proposed mechanisms for inducing stereotyped B-cell responses in various contexts. (a) Potential mechanisms causing stereotyped BCRs in particular B-cell subsets or differentiations. (b) Potential mechanism for causing stereotyped BCRs against conserved epitopes. Example of epitopes located on the stalk portion of the influenza HA. (c) Escape from immune tolerance by particular autoreactive B cells may account for stereotyped BCRs associated with autoimmune specificities. (d) Various mechanisms may account for stereotyped BCRs associated with B-cell cancers.
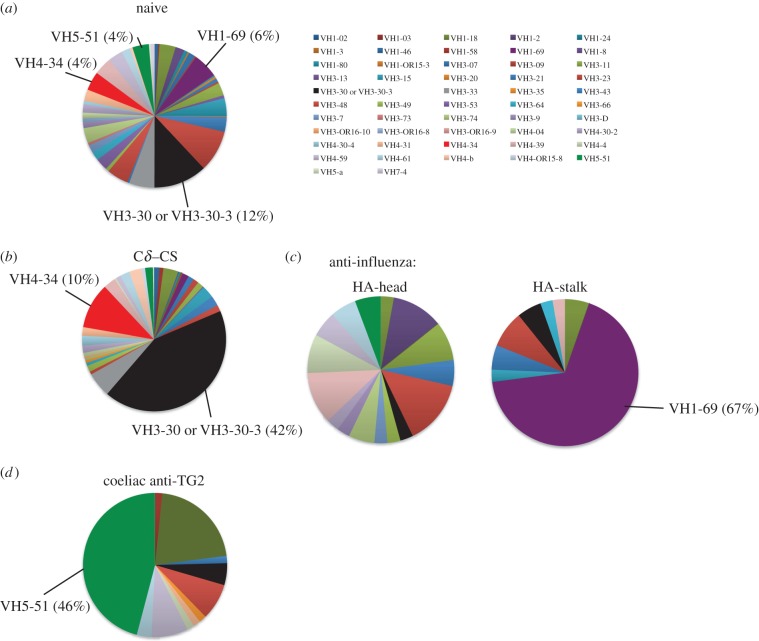
A human B-cell subset with stereotyped BCRs is the unusual C∂ class-switched, or the C∂–CS B-cell subset. Typically, immunoglobulins of the IgD class are generated as a transcript splice variant of a single transcript extending from the variable gene through the IgM gene (Cµ) and then through the IgD gene (C∂). Thus, naive B cells express both IgM and IgD simultaneously through differential splicing of the VDJ-Cµ–C∂ transcript. However, in humans, there is a class switch recombination signal sequence located between Cµ and C∂ that can be used to permanently class switch the cells to IgD through deletion of the IgM gene at the DNA level, similarly to class switching to IgG, IgA and IgE [13]. This C∂–CS population of B cells represents around 1% of peripheral blood B cells and has been demonstrated to secrete IgD class antibody in the lung, which then activates basophils through an IgD Fc receptor [14]. Antibody from these cells tends to be polyreactive, binding many antigens non-specifically with low affinity [15]. It is believed that C∂–CS B cells are the primary source of secreted IgD in human blood. These cells have a highly stereotyped BCR repertoire in which 90% of the cells use lambda light chains [16], and half of these cells have BCRs encoded by either VH3-30 [17] or VH4-34 [15,18] heavy chains (figure 2a versus b). C∂–CS BCRs are also preferentially encoded by the JH6 gene segment [15,16,18]. Notably, these C∂–CS variable genes are extensively adapted by somatic hypermutation [16].
Figure 2.
Examples of biased usage of VH immunoglobulin genes by (a,b) particular B-cell subpopulations or (c,d) B cells targeting particular epitopes.
The particular epitope or antigen bound by these stereotyped receptors is unknown, though almost certainly the epitope/antigens bound dictate the functional specialization of C∂–CS B cells. The stereotyped BCRs may be selected as a prerequisite for differentiation to C∂–CS B cells (class switch to IgD); that is, B cells destined for the C∂–CS lineage preferentially rearrange particular variable genes. Alternatively, activation in the context of a particular kind of immune response typified by particular BCR specificities may drive selection of stereotyped BCRs as well as class switch to IgD and the C∂–CS phenotype (figure 1a). In order to understand the function both of the stereotyped receptors as well as the C∂–CS B-cell subset, on the whole, current research efforts aim to identify the antigens and epitopes targeted by these receptors.
4. Human B cells specific for conserved epitopes on infectious antigens can have stereotyped B-cell receptors
A second instance where stereotypic BCRs are seen more and more commonly is in B cells from different individuals that are selected for binding to a particular epitope. An important aspect of vaccinology is the search for epitopes that are broadly conserved on the surfaces of pathogens which evade immunity through diversification of their surface molecules. For example, HIV evades antibody-mediated immunity in infected patients by encoding its genome with an error-prone polymerase such that its envelope proteins can rapidly evolve away from antibody targeting. Influenza similarly evades immunity through ‘antigenic drift’, introducing point mutations to its critical receptor haemagglutinin, or more dramatic antigenic shifts through gene segment exchange with disparate strains when both co-infect the same host [19]. Thus, as technologies advance to isolate monoclonal antibodies, the vaccine community is searching for rare B-cell specificities that are conserved despite antigenic drift and shift. This has led to the realization that B cells binding such conserved and typically inaccessible epitopes require highly restricted immunoglobulins which are often quite similar in overall structure. Antibodies against the HIV envelope protein tend to be encoded by VH5-51 when against one type of conserved epitope, the V3 loop [20], but by VH1-69 when against conserved portions of the gp41 glycoprotein [21–23]. Against influenza, most antibodies bind haemagglutinin (HA), the sialic acid binding protein that attaches virions to cells upon infection. Most neutralizing antibodies bind to the ‘globular head’ of HA where the sialic acid binding site is located. However, epitopes in the stalk portion of HA that attaches the protein to the viral envelope are highly conserved between most influenza strains. Interestingly, antibodies to the HA stalk are preferentially encoded by VH1-69 and the highly similar VH1-18 gene segments (figure 2c) [19,24–28]. Such antibodies were preferentially induced in individuals infected or vaccinated with the 2009 pandemic H1N1 influenza strains such that, in some cases, half of all neutralizing antibodies induced were encoded by VH1-69 or VH1-18 [29–31]. We hypothesize that expansion of these stereotyped BCRs occurred through selection of memory B cells to past strains because of the highly conserved nature of only the HA-stalk epitopes, for which stereotyped B cells existed (figure 1b).
An analysis by high-throughput immunoglobulin variable gene sequencing also identified stereotyped responses to the HA head that was encoded by VH3-7/JH6 variable genes with a conserved 18 amino acid CDR3 and that arose independently in multiple individuals [32]. Analyses of historical data by Jackson and colleagues identified VH3-7/JH6 immunoglobulin arising in past studies also [30,32,33].
Antibodies reactive to rotavirus envelope proteins have restricted repertoires that differ depending on whether they were isolated from resting naive or memory B-cell subsets in which there is a biased usage of the VH1-46 gene [34], versus whether they were isolated from gut mucosal plasma cells in which VH4-39 is over-represented [35].
In patients infected with hepatitis C (HCV), there is often stereotyped usage of the VH1-69 gene in various contexts such as in HCV-associated immunocytomas [36]. HCV reactive VH1-69- and VH4-34-encoded immunoglobulins are common in patients with mixed cryoglobulinaemia [37] and in HCV-associated nodal marginal zone B-cell lymphoma [38].
Bacterial antigens can also induce stereotyped antibody responses. For example, antibodies reactive to Streptococcus pneumoniae capsular polysaccharides have a restricted repertoire, with biased usage of VH3-7 and VH3-15 rearrangements [39]. Interestingly, a clonal population of splenic and circulating IgM + IgD + CD27 + marginal zone B cells harbouring this restricted repertoire has been identified in vaccinated children [40].
Another way that particular VH types can be expanded is through superantigen activation. For example, plasmablasts activated in patients with Staphylococcus aureus express predominantly VH3-encoded variable genes because the virulence factor staphylococcal protein A binds to VH3-encoded antibodies, activating these cells non-specifically [41].
The tendency for epitopes targeted by stereotyped receptors to be broadly conserved in mutagenic pathogens such as HIV and influenza has caused an increased focus on the cells expressing these genes. Thus, current research efforts are aimed at preferentially activating naive or memory B cells with stereotyped receptors, such as use of VH1-69. Other efforts aim to identify B cells expressing these receptors using anti-idiotypic antibodies. Efforts are also underway to identify circumstances, such as vaccination conditions, that will preferentially activate B cells with stereotyped BCRs with the aim of increasing the frequency of broad protection.
5. Self-reactive antibodies often use stereotyped B-cell receptors
Another class of stereotyped or restricted BCRs is those that bind to self- or autoantigens. One of the most famous examples of stereotyped autoantibodies are those encoded by the VH4-34 gene segment that are the sole cause of cold-agglutinin disease [42–44]. VH4-34-encoded antibodies have also been associated with lupus [45] and autoimmune B-cell populations [18]. VH4-34 binds to particular glycans known as polylactosamines or iI antigens. Polylactosamines are expressed on the surface of many human cells including erythrocytes such that VH4-34 antibody responses will tend to cause painful and dangerous red blood cell agglutination and/or anaemia (cold-agglutinin disease). However, polylactosamines also have structural similarities to many pathogen glycans and are therefore likely to be ‘natural antibodies’ evolved to target particular pathogen epitopes. Thus, despite having an autoimmune potential, B cells expressing VH4-34 or other stereotyped BCRs that are autoimmune associated may escape immune tolerance mechanisms. That is, the importance for protection of certain specificities that pose a risk for autoimmunity may have outweighed the danger of allowing these specificities to persist in the B-cell repertoire, leading to stereotyped responses to these autoantigens (figure 1c). By being encoded by only certain BCRs, these specificities could be preferentially maintained in the repertoire despite the risk.
Other stereotyped autoantibody responses include anti-desmoglein antibodies in pemphigus patients which tend to be from B cells with highly similar variable region gene rearrangements encoded by VH1-46 and with highly similar CDR3s [46,47]. B-cell clonal expansions found in the salivary glands of patients with Sjögren's syndrome tend to use one of three VH genes, including the pervasive VH1-69 gene in a third of the isolates [48]. We have reported that there is a highly restricted usage of the VH5-51 gene in autoreactive B cells reactive to transglutaminase-2 from coeliac disease patients (figure 2d) [49]. Interestingly, antibodies from coeliac disease patients that bind to gluten proteins (such as gliadin) are also stereotyped, and preferentially encoded by two heavy/light chain combinations: VH3-23/VLambda4-69 or VH3-15/Vk4-1 [50]. These stereotyped autoantibody responses could arise from the mechanism of tolerance escape described above for VH4-34-encoded cold-agglutinins (figure 1c). Alternatively, certain B-cell subpopulations that have stereotyped BCRs (figure 1a) may be more prone to cause autoimmune diseases.
Current research efforts are directed at identifying the particular epitopes of autoimmune stereotyped B cells or exploiting the fact that these cells have structurally unique surface immunoglobulins. These cells, when causing pathology, make an attractive potential target for therapy because of their conserved nature. It may be possible to reduce pathology with anti-idiotypic antibodies used to deplete the offending cells in a specific manner. Further, by understanding the targets of these stereotyped autoantibodies, measures can be taken to avoid or control autoimmune pathology.
6. B-cell-related cancers often have stereotyped B-cell receptors
As many as 30% of patients with chronic lymphocytic leukaemia (CLL) have stereotyped BCRs of various types [51]. As early as 1989, it was appreciated that multiple individuals could have CLL with BCRs encoded by the VH1-69 gene segment. Later, the Chiorazzi laboratory [52] and independently the Burrone group [53] found that the entire VH gene and CDR3 junction were highly conserved between multiple people with CLL. Restriction for the light chains encoding the BCRs in CLL was also noted [54]. In fact, approximately 1% of CLL patients express essentially identical tumour-associated immunoglobulins [55]. Another study found restriction for VH4 genes, including the autoreactive VH4-34 gene in CD5 + IgG + CLL B cells [56]. As described in §5, VH4-34 is well known for encoding autoreactive BCRs that bind to polylactosamine [42–44]. A critical observation was that discrete subsets of patients would have stereotyped receptors, suggesting that various CLL tumours would have occurred in an antigen-driven manner [57–60]. For example, subsets of CLL patients had lymphomas restricted for similar VH3-21/Iglambda-encoded BCRs [59], or for the VH4-34, VH4-39 or VH1-69 stereotyped receptors, each with similar CDR3s and other identifying characteristics [57–60]. CLLs have also been demonstrated to be generally autoreactive [61], binding human antigens, and thus there may be an important rule for chronic or repeated exposure to antigens driving the neoplasia and restricted immunoglobulin usage. Another class of stereotyped CLL Ig gene has an increased usage of VH3-33 [53] and VH3-21 paired to VLambda2-14 [62]. Marginal zone lymphoma also has restrictions in the VH and VL repertoire, particularly for VH1-2 [63,64], and salivary gland mucosa-associated lymphoid tissue leukaemic B cells also preferentially have VH1-69-encoded BCRs [65].
As reviewed elsewhere [51,66], stereotyped BCRs in CLL and other B-cell cancers can be used to subset patients into different classifications with associated clinicobiological features, including associated prognostic relevance. Molecular identification of the BCRs in various B-cell cancers may also be of value for tailoring treatment strategies and for understanding the underlying causes of these cancers. A number of causes for stereotyped BCRs in B-cell cancers have been proposed or can be envisioned (figure 1d). A B-cell subset or type may be particularly prone to have a stereotyped BCR as well as to become transformed. For example, the immunoglobulin somatic mutation factor, activation-induced deaminase can non-specifically target oncogenes located in super-enhancers and regulatory clusters depending on the cell type or differentiation [67]. Thus, a particular B-cell type that is subjected to repeated or extended mutagenesis of the BCR by somatic hypermutation during affinity maturation could be prone to mutation of oncogenes. Independent of B-cell subset, chronic stimulation of B cells with particular BCRs by either chronic infection such as HCV [38], or by autoantigens due to BCR autoreactivity [61], could lead to oncogene mutagenesis. Another cause of transformation could be enhancement of infection by oncogenic viruses owing to uptake of the viruses by certain BCR types.
Current research efforts aim to identify the antigens and epitopes targeted by the stereotyped receptors. With identification of the antigens, the direct or indirect role of B-cell specificity, for example, might be the key to understanding how the cells became transformed. Identifying the antigens could also be critical for treating or avoiding certain B-cell cancers associated with stereotyped receptors. For example, finding a particular viral association could drive further research into developing a vaccine that would allow avoidance of both infection and transformation. Other research is aimed at identifying the B-cell precursors that express stereotyped receptors but which are not transformed. The phenotype of these cells may identify therapeutic interventions for the tumour cells. Another possibility is to directly target stereotyped receptor expressing B cells with either anti-idiotype antibodies or with identified antigen that could have both diagnostic and therapeutic potential.
7. Certain B-cell receptors occur frequently in stereotyped B-cell responses
As readers may have noted, particular VH genes tend to occur more often in stereotyped BCRs in seemingly divergent contexts. VH4-34 has well-known autoimmune characteristics and is found increased in both CLL and in HCV mixed-cryoglobulinemia, likely related to this autoreactivity. Of particular note is VH1-69 that arises in association with various infectious disease antibody types including broadly protective antibodies against HIV and influenza as well as expanded and pathological antibodies in HCV, and even malaria [68]. VH1-69 also arises in conditions of autoimmunity, such as Sjögren's syndrome, and VH1-69 is the most prevalent VH gene for stereotyped BCRs in B-cell cancers. It is not clear what is unique about B cells expressing VH1-69-encoded BCRs but its common use in stereotyped responses could relate to the unique molecular structure of VH1-69-encoded antibodies. VH1-69-encoded antibody proteins have a distinct hydrophobic region within the antigen-binding site that may make this antibody type highly unique and important in various contexts [24–26]. This unique molecular character could target a particular class of epitopes shared by different antigens.
On the whole, there appears to be a balance between important roles for stereotyped BCR responses in immune protection, and B-cell-related pathology. The molecular commonalities of stereotyped receptors associated with protection versus pathology suggest that there are particular types of epitope which can only be targeted by BCRs that also pose a health threat. As technologies for identifying antibodies and characterizing the B-cell repertoire in a high-throughput manner continue to advance, we are likely to identify other stereotyped B-cell responses. Characterizing stereotyped B-cell responses could provide important understanding of the function of discrete types of B cells, how to immunize against certain pathogens, important prognostic indications, and could identify treatment options for various B-cell-related pathologies.
Authors' contributions
P.C.W. conceived the manuscript and designed the figures. C.J.H.D. and P.C.W. wrote the manuscript. Both authors approved the final version of the manuscript.
Competing interests
We declare we have no competing interests.
Funding
This work was funded in parts by NIH grants 2U19AI082724-06, 5U19AI090023-04, 1P01AI097092-03, 1U19AI109946-01, 2U19AI057266-11 and HHSN272201400005C.
References
- 1.Wysocki LJ, Gridley T, Huang S, Grandea AG, III, Gefter ML. 1987. Single germline VH and V kappa genes encode predominating antibody variable regions elicited in strain A mice by immunization with p-azophenylarsonate. J. Exp. Med. 166, 1–11. ( 10.1084/jem.166.1.1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Siekevitz M, Huang SY, Gefter ML. 1983. The genetic basis of antibody production: a single heavy chain variable region gene encodes all molecules bearing the dominant anti-arsonate idiotype in the strain A mouse. Eur. J. Immunol. 13, 123–132. ( 10.1002/eji.1830130207) [DOI] [PubMed] [Google Scholar]
- 3.Siekevitz M, Gefter ML, Brodeur P, Riblet R, Marshak-Rothstein A. 1982. The genetic basis of antibody production: the dominant anti-arsonate idiotype response of the strain A mouse. Eur. J. Immunol. 12, 1023–1032. ( 10.1002/eji.1830121208) [DOI] [PubMed] [Google Scholar]
- 4.Landolfi NF, Capra JD, Tucker PW. 1986. Germ-line sequence of the DH segment employed in Ars-A antibodies: implications for the generation of junctional diversity. J. Immunol. 137, 362–365. [PubMed] [Google Scholar]
- 5.Kuettner MG, Wang AL, Nisonoff A. 1972. Quantitative investigations of idiotypic antibodies. VI. Idiotypic specificity as a potential genetic marker for the variable regions of mouse immunoglobulin polypeptide chains. J. Exp. Med. 135, 579–595. ( 10.1084/jem.135.3.579) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Allen D, Simon T, Sablitzky F, Rajewsky K, Cumano A. 1988. Antibody engineering for the analysis of affinity maturation of an anti-hapten response. EMBO J. 7, 1995–2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cumano A, Rajewsky K. 1985. Structure of primary anti-(4-hydroxy-3-nitrophenyl)acetyl (NP) antibodies in normal and idiotypically suppressed C57BL/6 mice. Eur. J. Immunol. 15, 512–520. ( 10.1002/eji.1830150517) [DOI] [PubMed] [Google Scholar]
- 8.Bothwell AL, Paskind M, Reth M, Imanishi-Kari T, Rajewsky K, Baltimore D. 1982. Heavy chain variable region contribution to the NPb family of antibodies: somatic mutation evident in a gamma 2a variable region. Cell 24, 625–637. ( 10.1016/0092-8674(81)90089-1) [DOI] [PubMed] [Google Scholar]
- 9.Boersch-Supan ME, Agarwal S, White-Scharf ME, Imanishi-Kari T. 1985. Heavy chain variable region. Multiple gene segments encode anti-4-(hydroxy-3-nitro-phenyl)acetyl idiotypic antibodies. J. Exp. Med. 161, 1272–1292. ( 10.1084/jem.161.6.1272) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gearhart PJ, Sigal NH, Klinman NR. 1977. The monoclonal anti-phosphorylcholine antibody response in several murine strains: genetic implications of a diverse repertoire. J. Exp. Med. 145, 876–891. ( 10.1084/jem.145.4.876) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Claflin JL, Lieberman R, Davie JM. 1974. Clonal nature of the immune response to phosphorylcholine. I. Specificity, class, and idiotype of phosphorylcholine-binding receptors on lymphoid cells. J. Exp. Med. 139, 58–73. ( 10.1084/jem.139.1.58) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lam KP, Rajewsky K. 1999. B cell antigen receptor specificity and surface density together determine B-1 versus B-2 cell development. J. Exp. Med. 190, 471–477. ( 10.1084/jem.190.4.471) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.White MB, Word CJ, Humphries CG, Blattner FR, Tucker PW. 1990. Immunoglobulin D switching can occur through homologous recombination in human B cells. Mol. Cell. Biol. 10, 3690–3699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen K, et al. 2009. Immunoglobulin D enhances immune surveillance by activating antimicrobial, proinflammatory and B cell-stimulating programs in basophils. Nat. Immunol. 10, 889–898. ( 10.1038/ni.1748) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koelsch K, et al. 2007. Mature B cells class switched to IgD are autoreactive in healthy individuals. J. Clin. Investig. 117, 1558–1565. ( 10.1172/JCI27628) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu YJ, de Bouteiller O, Arpin C, Briere F, Galibert L, Ho S, Martinez-Valdez H, Banchereau J, Lebecque S. 1996. Normal human IgD+IgM-germinal center B cells can express up to 80 mutations in the variable region of their IgD transcripts. Immunity 4, 603–613. ( 10.1016/S1074-7613(00)80486-0) [DOI] [PubMed] [Google Scholar]
- 17.Seifert M, Steimle-Grauer SA, Goossens T, Hansmann ML, Brauninger A, Kuppers R. 2009. A model for the development of human IgD-only B cells: genotypic analyses suggest their generation in superantigen driven immune responses. Mol. Immunol. 46, 630–639. ( 10.1016/j.molimm.2008.07.032) [DOI] [PubMed] [Google Scholar]
- 18.Zheng NY, et al. 2004. Human immunoglobulin selection associated with class switch and possible tolerogenic origins for Cδ class-switched B cells. J. Clin. Investig. 113, 1188–1201. ( 10.1172/JCI20255) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kaur K, Sullivan M, Wilson PC. 2011. Targeting B cell responses in universal influenza vaccine design. Trends Immunol. 32, 524–531. ( 10.1016/j.it.2011.08.007) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gorny MK, et al. 2009. Preferential use of the VH5–51 gene segment by the human immune response to code for antibodies against the V3 domain of HIV-1. Mol. Immunol. 46, 917–926. ( 10.1016/j.molimm.2008.09.005) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gustchina E, et al. 2010. Structural basis of HIV-1 neutralization by affinity matured Fabs directed against the internal trimeric coiled-coil of gp41. PLoS Pathog. 6, e1001182 ( 10.1371/journal.ppat.1001182) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Luftig MA, et al. 2006. Structural basis for HIV-1 neutralization by a gp41 fusion intermediate-directed antibody. Nat. Struct. Mol. Biol. 13, 740–747. ( 10.1038/nsmb1127) [DOI] [PubMed] [Google Scholar]
- 23.Sabin C, et al. 2010. Crystal structure and size-dependent neutralization properties of HK20, a human monoclonal antibody binding to the highly conserved heptad repeat 1 of gp41. PLoS Pathog. 6, e1001195 ( 10.1371/journal.ppat.1001195) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ekiert DC, Bhabha G, Elsliger MA, Friesen RH, Jongeneelen M, Throsby M, Goudsmit J, Wilson IA. 2009. Antibody recognition of a highly conserved influenza virus epitope. Science 324, 246–251. ( 10.1126/science.1171491) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Avnir Y, et al. 2014. Molecular signatures of hemagglutinin stem-directed heterosubtypic human neutralizing antibodies against influenza A viruses. PLoS Pathog. 10, e1004103 ( 10.1371/journal.ppat.1004103) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sui J, et al. 2009. Structural and functional bases for broad-spectrum neutralization of avian and human influenza A viruses. Nat. Struct. Mol. Biol. 16, 265–273. ( 10.1038/nsmb.1566) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Corti D, et al. 2010. Heterosubtypic neutralizing antibodies are produced by individuals immunized with a seasonal influenza vaccine. J. Clin. Invest. 120, 1663–1673. ( 10.1172/JCI41902) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dreyfus C, et al. 2012. Highly conserved protective epitopes on influenza B viruses. Science 337, 1343–1348. ( 10.1126/science.1222908) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li GM, et al. 2012. Pandemic H1N1 influenza vaccine induces a recall response in humans that favors broadly cross-reactive memory B cells. Proc. Natl Acad. Sci. USA 109, 9047–9052. ( 10.1073/pnas.1118979109) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wrammert J, et al. 2011. Broadly cross-reactive antibodies dominate the human B cell response against 2009 pandemic H1N1 influenza virus infection. J. Exp. Med. 208, 181–193. ( 10.1084/jem.20101352) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thomson CA, et al. 2012. Pandemic H1N1 influenza infection and vaccination in humans induces cross-protective antibodies that target the hemagglutinin stem. Front. Immunol. 3, 87 ( 10.3389/fimmu.2012.00087) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jackson KJ, et al. 2014. Human responses to influenza vaccination show seroconversion signatures and convergent antibody rearrangements. Cell Host Microbe 16, 105–114. ( 10.1016/j.chom.2014.05.013) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Krause JC, Tsibane T, Tumpey TM, Huffman CJ, Briney BS, Smith SA, Basler CF, Crowe JE. 2011. Epitope-specific human influenza antibody repertoires diversify by B cell intraclonal sequence divergence and interclonal convergence. J. Immunol. 187, 3704–3711. ( 10.4049/jimmunol.1101823) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Weitkamp JH, Kallewaard NL, Bowen AL, Lafleur BJ, Greenberg HB, Crowe JE., Jr 2005. VH1–46 is the dominant immunoglobulin heavy chain gene segment in rotavirus-specific memory B cells expressing the intestinal homing receptor alpha4beta7. J. Immunol. 174, 3454–3460. ( 10.4049/jimmunol.174.6.3454) [DOI] [PubMed] [Google Scholar]
- 35.Di Niro R, et al. 2010. Rapid generation of rotavirus-specific human monoclonal antibodies from small-intestinal mucosa. J. Immunol. 185, 5377–5383. ( 10.4049/jimmunol.1001587) [DOI] [PubMed] [Google Scholar]
- 36.Ivanovski M, Silvestri F, Pozzato G, Anand S, Mazzaro C, Burrone OR, Efremov DG. 1998. Somatic hypermutation, clonal diversity, and preferential expression of the VH 51p1/VL kv325 immunoglobulin gene combination in hepatitis C virus-associated immunocytomas. Blood 91, 2433–2442. [PubMed] [Google Scholar]
- 37.Charles ED, Green RM, Marukian S, Talal AH, Lake-Bakaar GV, Jacobson IM, Rice CM, Dustin LB. 2008. Clonal expansion of immunoglobulin M+CD27+ B cells in HCV-associated mixed cryoglobulinemia. Blood 111, 1344–1356. ( 10.1182/blood-2007-07-101717) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Marasca R, Vaccari P, Luppi M, Zucchini P, Castelli I, Barozzi P, Cuoghi A, Torelli G. 2001. Immunoglobulin gene mutations and frequent use of VH1-69 and VH4-34 segments in hepatitis C virus-positive and hepatitis C virus-negative nodal marginal zone B-cell lymphoma. Am. J. Pathol. 159, 253–261. ( 10.1016/S0002-9440(10)61691-4) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lucas AH, Moulton KD, Tang VR, Reason DC. 2001. Combinatorial library cloning of human antibodies to Streptococcus pneumoniae capsular polysaccharides: variable region primary structures and evidence for somatic mutation of Fab fragments specific for capsular serotypes 6B, 14, and 23F. Infect. Immun. 69, 853–864. ( 10.1128/IAI.69.2.853-864.2001) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Weller S, et al. 2004. Human blood IgM ‘memory’ B cells are circulating splenic marginal zone B cells harboring a prediversified immunoglobulin repertoire. Blood 104, 3647–3654. ( 10.1182/blood-2004-01-0346) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pauli NT, et al. 2014. Staphylococcus aureus infection induces protein A-mediated immune evasion in humans. J. Exp. Med. 211, 2331–2339. ( 10.1084/jem.20141404) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pascual V, Victor K, Spellerberg M, Hamblin TJ, Stevenson FK, Capra JD. 1992. VH restriction among human cold agglutinins. The VH4-21 gene segment is required to encode anti-I and anti-i specificities. J. Immunol. 149, 2337–2344. [PubMed] [Google Scholar]
- 43.Potter KN, Li Y, Pascual V, Williams RC, Jr, Byres LC, Spellerberg M, Stevenson FK, Capra JD. 1993. Molecular characterization of a cross-reactive idiotope on human immunoglobulins utilizing the VH4-21 gene segment. J. Exp. Med. 178, 1419–1428. ( 10.1084/jem.178.4.1419) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Thompson KM, Sutherland J, Barden G, Melamed MD, Randen I, Natvig JB, Pascual V, Capraj JD, Stevenson FK. 1991. Human monoclonal antibodies against blood group antigens preferentially express a VH4-21 variable region gene-associated epitope. Scand. J. Immunol. 34, 509–518. ( 10.1111/j.1365-3083.1991.tb01574.x) [DOI] [PubMed] [Google Scholar]
- 45.Pugh-Bernard AE, Silverman GJ, Cappione AJ, Villano ME, Ryan DH, Insel RA, Sanz I. 2001. Regulation of inherently autoreactive VH4-34 B cells in the maintenance of human B cell tolerance. J. Clin. Invest. 108, 1061–1070. ( 10.1172/JCI200112462) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cho MJ, et al. 2014. Shared VH1-46 gene usage by pemphigus vulgaris autoantibodies indicates common humoral immune responses among patients. Nat. Commun. 5, 4167 ( 10.1038/ncomms5167) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yamagami J, Payne AS, Kacir S, Ishii K, Siegel DL, Stanley JR. 2010. Homologous regions of autoantibody heavy chain complementarity-determining region 3 (H-CDR3) in patients with pemphigus cause pathogenicity. J. Clin. Invest. 120, 4111–4117. ( 10.1172/JCI44425) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.De Re V, De Vita S, Gasparotto D, Marzotto A, Carbone A, Ferraccioli G, Boiocchi M. 2002. Salivary gland B cell lymphoproliferative disorders in Sjogren's syndrome present a restricted use of antigen receptor gene segments similar to those used by hepatitis C virus-associated non-Hodgkins's lymphomas. Eur. J. Immunol. 32, 903–910. () [DOI] [PubMed] [Google Scholar]
- 49.Di Niro R, et al. 2012. High abundance of plasma cells secreting transglutaminase 2-specific IgA autoantibodies with limited somatic hypermutation in celiac disease intestinal lesions. Nat. Med. 18, 441–445. ( 10.1038/nm.2656) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Steinsbo O, Henry Dunand CJ, Huang M, Mesin L, Salgado-Ferrer M, Lundin KE, Jahnsen J, Wilson PC, Sollid LM. 2014. Restricted VH/VL usage and limited mutations in gluten-specific IgA of coeliac disease lesion plasma cells. Nat. Commun. 5, 4041 ( 10.1038/ncomms5041) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Darzentas N, Stamatopoulos K. 2013. The significance of stereotyped B-cell receptors in chronic lymphocytic leukemia. Hematol. Oncol. Clin. North America 27, 237–250. ( 10.1016/j.hoc.2012.12.001) [DOI] [PubMed] [Google Scholar]
- 52.Fais F, et al. 1998. Chronic lymphocytic leukemia B cells express restricted sets of mutated and unmutated antigen receptors. J. Clin. Invest. 102, 1515–1525. ( 10.1172/JCI3009) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Efremov DG, Ivanovski M, Siljanovski N, Pozzato G, Cevreska L, Fais F, Chiorazzi N, Batista FD, Burrone OR. 1996. Restricted immunoglobulin VH region repertoire in chronic lymphocytic leukemia patients with autoimmune hemolytic anemia. Blood 87, 3869–3876. [PubMed] [Google Scholar]
- 54.Stamatopoulos K, et al. 2005. Immunoglobulin light chain repertoire in chronic lymphocytic leukemia. Blood 106, 3575–3583. ( 10.1182/blood-2005-04-1511) [DOI] [PubMed] [Google Scholar]
- 55.Widhopf GF, II, Rassenti LZ, Toy TL, Gribben JG, Wierda WG, Kipps TJ. 2004. Chronic lymphocytic leukemia B cells of more than 1% of patients express virtually identical immunoglobulins. Blood 104, 2499–2504. ( 10.1182/blood-2004-03-0818) [DOI] [PubMed] [Google Scholar]
- 56.Hashimoto S, et al. 1995. Somatic diversification and selection of immunoglobulin heavy and light chain variable region genes in IgG+ CD5+ chronic lymphocytic leukemia B cells. J. Exp. Med. 181, 1507–1517. ( 10.1084/jem.181.4.1507) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Messmer BT, et al. 2004. Multiple distinct sets of stereotyped antigen receptors indicate a role for antigen in promoting chronic lymphocytic leukemia. J. Exp. Med. 200, 519–525. ( 10.1084/jem.20040544) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ghiotto F, et al. 2004. Remarkably similar antigen receptors among a subset of patients with chronic lymphocytic leukemia. J. Clin. Investig. 113, 1008–1016. ( 10.1172/JCI19399) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tobin G, Soderberg O, Thunberg U, Rosenquist R. 2004. V(H)3-21 gene usage in chronic lymphocytic leukemia—characterization of a new subgroup with distinct molecular features and poor survival. Leuk. Lymphoma 45, 221–228. ( 10.1080/1042819031000147018) [DOI] [PubMed] [Google Scholar]
- 60.Tobin G, et al. 2004. Subsets with restricted immunoglobulin gene rearrangement features indicate a role for antigen selection in the development of chronic lymphocytic leukemia. Blood 104, 2879–2885. ( 10.1182/blood-2004-01-0132) [DOI] [PubMed] [Google Scholar]
- 61.Herve M, Xu K, Ng YS, Wardemann H, Albesiano E, Messmer BT, Chiorazzi N, Meffre E. 2005. Unmutated and mutated chronic lymphocytic leukemias derive from self-reactive B cell precursors despite expressing different antibody reactivity. J. Clin. Invest. 115, 1636–1643. ( 10.1172/JCI24387) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tobin G, et al. 2003. Chronic lymphocytic leukemias utilizing the VH3-21 gene display highly restricted Vlambda2-14 gene use and homologous CDR3s: implicating recognition of a common antigen epitope. Blood 101, 4952–4957. ( 10.1182/blood-2002-11-3485) [DOI] [PubMed] [Google Scholar]
- 63.Bikos V, et al. 2012. Over 30% of patients with splenic marginal zone lymphoma express the same immunoglobulin heavy variable gene: ontogenetic implications. Leukemia 26, 1638–1646. ( 10.1038/leu.2012.3) [DOI] [PubMed] [Google Scholar]
- 64.Bikos V, et al. 2012. Selection of antigen receptors in splenic marginal-zone lymphoma: further support from the analysis of the immunoglobulin light-chain gene repertoire. Leukemia 26, 2567–2569. ( 10.1038/leu.2012.207) [DOI] [PubMed] [Google Scholar]
- 65.Miklos JA, Swerdlow SH, Bahler DW. 2000. Salivary gland mucosa-associated lymphoid tissue lymphoma immunoglobulin V(H) genes show frequent use of V1-69 with distinctive CDR3 features. Blood 95, 3878–3884. [PubMed] [Google Scholar]
- 66.Darzentas N, Stamatopoulos K. 2013. Stereotyped B cell receptors in B cell leukemias and lymphomas. Methods Mol. Biol. 971, 135–148. ( 10.1007/978-1-62703-269-8_8) [DOI] [PubMed] [Google Scholar]
- 67.Qian J, et al. 2014. B cell super-enhancers and regulatory clusters recruit AID tumorigenic activity. Cell 159, 1524–1537. ( 10.1016/j.cell.2014.11.013) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wajanarogana S, Prasomrothanakul T, Udomsangpetch R, Tungpradabkul S. 2006. Construction of a human functional single-chain variable fragment (scFv) antibody recognizing the malaria parasite Plasmodium falciparum. Biotechnol. Appl. Biochem. 44, 55–61. [DOI] [PubMed] [Google Scholar]