Abstract
Purpose
Smoking is causally associated with certain prevalent visually impairing eye diseases, including age-related macular degeneration and cataract. Studies have found that people are afraid of “going blind” and may be motivated to quit smoking if they know that vision loss is associated with smoking behavior.
Methods
A random-digit dialed telephone survey was used to measure health knowledge of adult smokers in Canada (n 5 2,765), the United States (n 5 3,178), the United Kingdom (n 5 2,767), and Australia (n 5 2,623) as part of the International Tobacco Control Four-Country Project.
Results
A low proportion of smokers from Canada (13.0%), the United States (9.5%), and the United Kingdom (9.7%) believed that smoking can cause blindness. In contrast, 47.2% of Australian smokers believed that smoking causes blindness. Australia was the only country during the sampling period to have national awareness campaigns about smoking and its effects on eye health.
Conclusion
These findings point to the need across countries to educate the public on this important consequence of smoking. There is an opportunity for the public health and eye health communities to work to educate the public about the impacts smoking has on eye health to improve quit rates and help discourage people from starting to smoke.
Keywords: public health, smoking, blindness, age-related macular degeneration, cataract
INTRODUCTION
Smoking is causally linked to a number of eye diseases, particularly age-related macular degeneration (AMD)1–4 and cataract,5–8 2 leading causes of blindness.9,10 Smoking has also been linked to thyroid-associated ophthalmopathy, anterior ischemic optic neuropathy, and tobacco–alcohol amblyopia and is a known facilitator of diabetic and hypertensive retinopathy.11–14 In 1988, the United States Surgeon General concluded that nicotine, present in tobacco smoke, is addictive, and nicotine addiction is similar to heroin or cocaine addiction.15 Nicotine can reach the brain within 10 seconds after the smoke is inhaled16 and induces feelings of pleasure.17
Cigarettes negatively affect the human body in numerous ways. Cigarette smoke contains more than 4,000 chemicals and gases, including hydrogen cyanide, formaldehyde, carbon monoxide, and benzene. There are more than 50 compounds present in cigarette smoke that have been identified by the United States Environmental Protection Agency or the International Agency for Research on Cancer as known or probable human carcinogens.18 When cigarette smoke is inhaled, these chemicals and gases are absorbed through the lungs and transferred to the blood-stream.19 The carbon monoxide in cigarette smoke binds to the hemoglobin in red blood cells, preventing affected cells from carrying a full load of oxygen to cells.20 Smoking also deprives the body of oxygen because of blood vessel constriction. Both experimental and clinical studies have found that active or passive smoking promotes vasomotor dysfunction, atherogenesis, and thrombosis in multiple vascular beds.21 Some of the cancer-causing agents in the cigarette smoke, including benzo(a)pyrene, can damage genes that control the growth of cells by binding to cells in the airways and major organs of smokers.22 Cigarette smoke is high in oxidants, which deplete plasma and tissue antioxidants.23 Nicotine is known to depress the body’s immune system, making it harder to protect the body from illness and more difficult to heal or repair tissues.24 These various negative effects of cigarette smoking have been shown to cause morbidity and premature death, most often from myocardial infarctions, cerebrovascular accidents, lung cancer, and chronic obstructive pulmonary disease.25 Smoking cigarettes can cause harm to the eye and nearly every other organ in the body.26 Visual impairment, unlike other health consequences of smoking, does not kill people, but it greatly affects their quality of life.27,28 The United Kingdom, one of the few countries with published prevalence rates on smoking and blindness, has an estimated 18,000 people who are blind as a result of smoking-induced AMD.29 Cigarette smoking increases the risk of AMD 2- to 3-fold, and smokers may develop the disease about 10 years earlier than nonsmokers.30 A similar relationship exists between smoking and cataract (particularly nuclear and posterior subcapsular), with higher levels of smoking increasing the risk of cataract and its severity.5 An Australian study estimated that smoking causes or contributes to around 20% of new blindness in people over the age of 50.31
Despite more than 50 years of literature about the adverse effects of smoking, awareness of the range of health risks associated with smoking is neither high nor uniform among either smokers or nonsmokers. Studies have found that there are significant gaps in smokers’ knowledge and understanding of the health risks of smoking, in particular knowledge about health conditions that affect quality of life, including impotence,32 osteoporosis, and early menopause.33 It is not well understood to what extent smokers or nonsmokers are aware of the link between tobacco smoking and “blindness”; however, there are indications that knowledge of a causal association is very low.34
For example, survey studies in Canada, the United Kingdom, and Singapore35–37 have found that knowledge of the causal relationship of smoking to blindness is quite low, especially relative to other health conditions linked to smoking. A cross-sectional study of 882 Canadian patients found that only 3.5% of them reported that smoking was a risk factor for AMD, despite smoking being the most important known preventable risk factor in the development of the disease.35 A nonrandom cross-sectional survey of 358 United Kingdom adult smokers (mean age, 59.3 years) attending a district hospital found that respondents were much more likely to believe smoking causes lung cancer (92.2%), heart disease (87.6%), and stroke (70.6%) than blindness (9.5%).36 Although the United Kingdom smokers were less fearful of blindness compared with the other 3 conditions, about half of them stated that they would definitely or probably quit smoking if they developed early signs of any of the conditions, with no significant differences between the conditions. Awareness and fear of these same 4 health consequences of smoking were also studied in a United Kingdom cross-sectional study of 260 16- to 18-year-olds attending 4 organized social events.38 These youth were much more likely to believe that smoking probably or definitely causes lung cancer (81%) compared with heart disease (27%), stroke (15%), and blindness (5%).38 The youth participants were significantly (P<0.01) more fearful of blindness than the other 3 conditions, and a significantly greater percentage (P<0.01) said they would stop smoking if early signs of blindness developed compared with early signs of the other 3 conditions.38 These findings suggested that although awareness of the risk of blindness from smoking is low among British youth; “fear of blindness may be more likely to motivate teenagers to stop smoking than fear of lung or heart disease.”38 Finally, a comparative, cross-sectional survey of adult patients in Scotland (n=112) and Singapore (n=163) found that more than 85% of the respondents knew smoking was related to lung cancer, mouth and throat cancer, heart disease, and stroke; however, only 36.5% of the Singapore sample and 30.5% of the Scotland sample reported being aware that smoking could cause blindness.37
The impact of the findings in the above studies that measured knowledge about smoking’s causal association with “blindness” is limited by the sampling methods, which for each study were not random (i.e., all participants were seeking medical treatment or attending a social event).
Increasing and measuring knowledge of harm associated with tobacco smoking behavior is important because knowledge about the health effects of smoking is strongly associated with intentions to quit smoking.32 In a 2008 Danish study, researchers found that smokers with a high knowledge of the harms associated with smoking were more likely to quit and remain abstinent at a 5-year follow-up examination.39
A small number of jurisdictions are working toward increasing public knowledge about the risks to eye diseases associated with smoking. Australia’s National Tobacco Campaign, launched in 1997, included a variety of health promotion initiatives, including print and television ads linking smoking and “loss of eyesight,” starting in 1998 and were used from time to time ever since.40 An evaluation was conducted to measure the relative efficiency of different television advertisements used in this campaign to encouraging smokers to call the national Quitline. Carroll and Rock41 reported that the television commercial about the association between smoking and macular degeneration was more efficient in generating Quitline calls than other ads that contained information about tar in smoker’s lungs. Some of the success of the Australian “Eye” ads was attributed to the fact that the information about blindness was new to most smokers and was portrayed in a dramatic manner with blood vessels in the retina of a smoker bursting and leading to blindness.42 Similarly, New Zealand health authorities ran television commercials during 2002 and 2003 that encouraged people to call their national cessation support phone line (Quit Group). The television commercial about smoking and blindness were found to be the most effective at generating calls to Quit Group.43 Australia and New Zealand recently introduced a graphic warning label on cigarette packaging to communicate that smoking causes blindness.44 In contrast, most countries have not included eye health effects in their tobacco and public health campaigns.
At a global level, the World Health Organization (WHO) Framework Convention on Tobacco Control (FCTC) was adopted by the World Health Assembly in May 2003 and implemented in February 2005.45 The FCTC provides an internationally coordinated response to combating the public health epidemic that tobacco represents. The treaty addresses a range of issues including comprehensive bans on advertising, health warnings on tobacco packaging, taxation policies, and smoke-free policies. Article 12 of the FCTC includes detailed expectations for national parties to adopt comprehensive education and program development to communicate the health effects of smoking tobacco.45
The International Tobacco Control (ITC) Policy Evaluation Project is an international longitudinal cohort study, the main objective of which is to evaluate the psychosocial and behavioral effects of FCTC policies.47 In 2002, the ITC launched the first wave of the ITC Four-Country (ITC-4) Project, which involved collecting data from nationally representative samples of adult smokers in Canada, the United States, the United Kingdom, and Australia. These 4 countries are all predominantly English-speaking with relatively high incomes and a range of tobacco control policies. Knowledge of the health effects from tobacco use is typically measured annually using the ITC survey tool. Since Wave 3 (the third measure) in 2004, questions have been included about smokers’ knowledge of blindness and smoking.
The aim of the current study was to use nationally representative samples of adult smokers from Canada, the United States, the United Kingdom, and Australia to examine smokers’ knowledge that smoking causes blindness in comparison with other smoking-related diseases or health effects, in particular to see if we could find any evidence of the Australian campaign leading to higher awareness there. Of note, this study was conducted before the release of the warning labels in Australia, which included messages about smoking causing blindness, so only the television ad on macular degeneration could be responsible for any effects found.
MATERIALS AND METHODS
SAMPLE
Eligibility for the ITC-4 Project required participants to (1) live in Canada, the United States, the United Kingdom, or Australia; (2) be 18 years or older; (3) have smoked more than 100 cigarettes in their lives and at least once in the past 30 days; and (4) be willing to complete the ITC-4 phone survey. Between 2004 and 2007, there were 11,333 respondents who were daily smokers (Canada = 2,765; United States = 3,178; United Kingdom = 2,767; Australia = 2,623).
PROCEDURE
The study protocol was reviewed and received ethics clearance from the Institutional Review Board or Research Ethics Board at each of the following institutions: the University of Waterloo (Canada), Roswell Park Cancer Institute (United States), the University of Illinois-Chicago (United States), the University of Strathclyde (United Kingdom), the University of Stirling (United Kingdom), the Open University (United Kingdom), and The Cancer Council Victoria (Australia). Detailed information on the procedures used in the ITC-4 Project can be found in Fong et al.46 and Thompson et al.,47 and from the ITC Technical report.48 The cohort of the ITC-4 Project was constructed from probability sampling methods using telephone numbers selected at random from the population of each country, within strata defined by geographic region and community size.48 The United States sample, for example, was based on 12 geographic strata. Eligible households were identified by asking potential household informants the number of adult smokers. The “next birthday” method was used to select the respondent in households with multiple eligible adult smokers. The survey was conducted using computer-assisted telephone interviewing software and was completed in 2 calls: a 10-minute recruitment call was followed 1 week later by a 40-minute main survey. To increase recruitment rates, participants were mailed a compensation equivalent to $10 United States before completing the main survey. A knowledge question for blindness was first included in Wave 3 (June through December 2004) and continued through Wave 4 (October 2005 through January (2006), and Wave 5 (September 2006 through January 2007). The analysis in this report is limited to respondents answering the blindness knowledge question for their first time. Because each wave incorporates new participants to replenish those who have been lost to follow-up, there are new participants in all 3 waves who are answering the blindness knowledge question for their first time. Combining respondents from the 4 countries, across 3 waves, results in a sample size of 11,333 daily smokers, nationally representative of these countries.
MEASURES
The ITC-4 Survey was standardized across the 4 countries: respondents in each country were asked the same questions, with only minor variations for colloquial speech. In addition to demographic questions (i.e., age, sex, ethnicity, education, and income), respondents were asked to state whether they believed smoking causes (1) stroke in smokers, (2) impotence in male smokers, (3) lung cancer in nonsmokers from secondhand smoke, and (4) blindness. The question was worded, “I am going to read you a list of health effects and diseases that may or may not be caused by smoking cigarettes. Based on what you know or believe, does smoking cause (insert health effect)?” The response options were: “Yes,” “No,” “Refused,” or “Don’t Know.”
Respondents were classified by different socioeconomic measures including sex, level of education, household income, ethnicity or language, and age. Two age groups were created- a youth or younger group for people age 18 to 24 years in their first wave, and all others. The rationale for grouping respondents by age was to build on ideas explored by Moradi et al.38 who found that younger people may respond to messages of blindness differently. Education classifications were created that grouped respondents in either a “low” group (i.e., completed high school or less in Canada, the United States, and Australia, or secondary/vocational or less in the United Kingdom), or a “moderate and high” group. Income was classified by 3 groups: “low” (i.e., under $30,000 in Canada, the United States, and Australia, or under £15,001 in the United Kingdom), “moderate and high” group (i.e., $30,000 or £15,000 or greater), and “refused.” Ethnicity was measured using census questions from each country and then analyzed as a dichotomous variable- the majority being “white or Caucasian” versus “nonwhite” except in Australia where language was used (language spoken at home as “English” or “non-English”) as a proxy measure for ethnicity, consistent with the Australian census. All surveys were conducted in English, except for in Canada, where Francophone respondents were given a French-language version if requested.
ANALYSIS
All data were analyzed using SPSS 17.0 (SPSS Inc., Chicago, Illinois). Only daily smokers were included in the analysis. Frequencies and means are reported with unweighted data. All proportions, Pearson χ2 tests, and the logistic regression were computed with weighted data using the complex sample feature in SPSS 17.0; an alpha level of .05 was used for all statistical tests.
RESULTS
Table 1 provides sample characteristics by country (n=11,333) of the unweighted data. The majority of respondents were women (56.2%), at least 25 years old (90.5%), and members of the majority ethnic group for their country (88.9%). Approximately half of the sample (55.2%) was classified as having a lower level of education, and most of the sample (61.1%) was classified as having a medium or high annual income level.
Table 1.
Characteristics of the International Tobacco Four Country Survey (ITC-4) Sample, Wave 3 and Replenishment Waves 4 – 5, by country (n = 11,333)
| Canada | United States |
United Kingdom |
Australia | Total | ||
|---|---|---|---|---|---|---|
| Sample Size | ||||||
| Respondents | 24.4% (2,765) |
28.0% (3,178) |
24.4% (2,767) |
23.1% (2,623) |
100% (11,333) |
|
| Sex | ||||||
| Male | 44.3% (1,224) |
41.4% (1,316) |
43.9% (1,214) |
46.1% (1,209) |
43.8% (4,963) |
|
| Female | 55.7% (1,541) |
58.6% (1,862) |
56.1% (1,553) |
53.9% (1,414) |
56.2% (6,370) |
|
| Age – Categorical | ||||||
| 18 – 24 years | 10.8% (299) |
9.1% (289) |
7.2% (198) |
11.1% (291) |
9.5% (1,077) |
|
| 25+ | 89.2% (2,466) |
90.9% (2,889) |
92.8% (2,569) |
88.9% (2,332) |
90.5% (10,256) |
|
| Age – Continuous | ||||||
| Mean | 43.2 | 45.5 | 45.7 | 41.8 | 44.1 | |
| Ethnicity | ||||||
| Majority | 90.2% (2,494) |
82.1% (2,601) |
96.1% (2,657) |
88.1% (2,312) |
88.9% (10,064) |
|
| Minority | 9.7% (269) |
17.8% (565) |
3.8% (105) |
11.8% (310) |
11.0% (1,249) |
|
| Education | ||||||
| Low | 49.5% (1,365) |
46.2% (1,466) |
61.7% (1,693) |
65.3% (1708) |
55.2% (6,232) |
|
| Medium/High | 50.5% (1,394) |
53.8% (1,706) |
38.3% (1,050) |
34.7% (909) |
44.8% (5,059) |
|
| Income | ||||||
| Low | 27.8% (767) |
36.8% (1,171) |
31.6% (875) |
30.1% (790) |
31.8% (3,603) |
|
| Moderate/High | 64.8% (1,791) |
57.4% (1,825) |
59.5% (1,645) |
63.4% (1,664) |
61.1% (6,925) |
|
| Refused | 7.4% (205) |
5.7% (182) |
8.9% (247) |
6.4% (169) |
7.1% (803) |
|
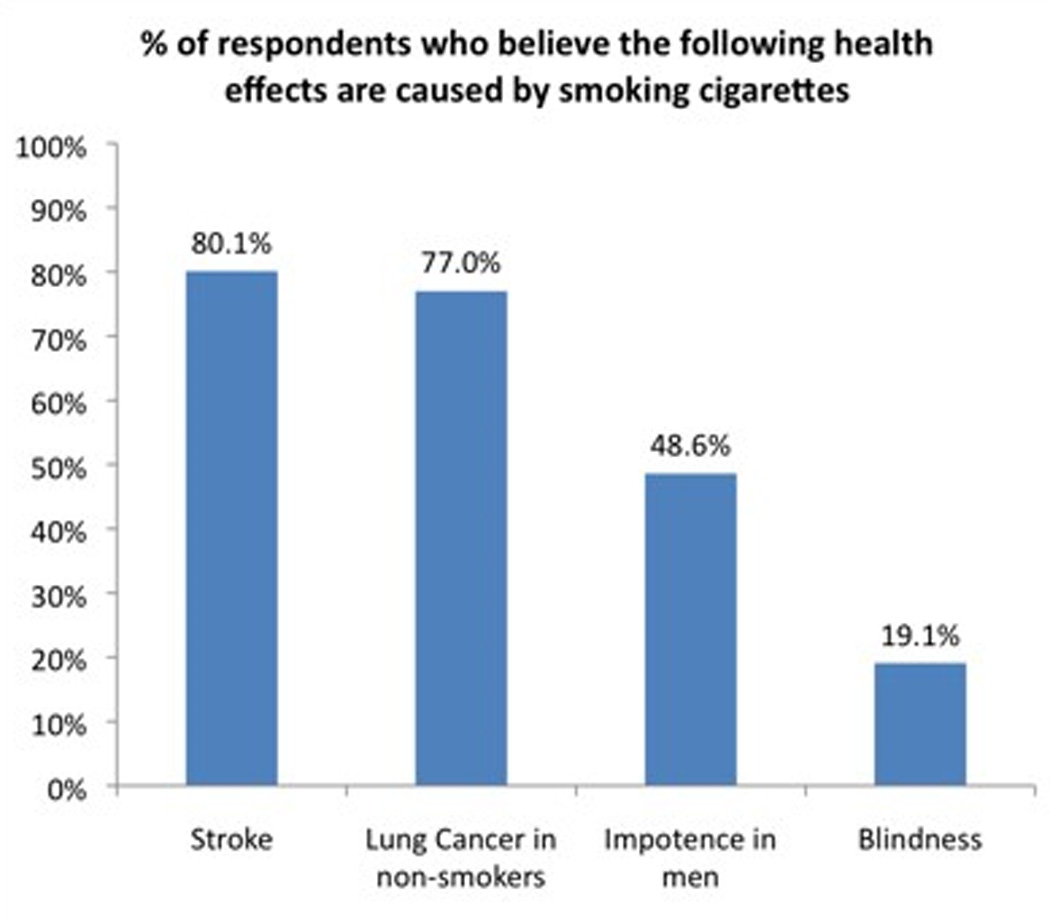
Participants were asked if smoking causes stroke (n=11,318), impotence in men (n=11,293), lung cancer in nonsmokers (n=11,318), or blindness (n=11,311). The sample sizes reported in each analysis vary slightly because of differences in missing data across different variables included in that analysis. The majority of respondents believed that smoking causes lung cancer in nonsmokers from secondhand smoke (77.0%) and stroke (80.1%); however, less than half (48.6%) of survey respondents reported that smoking causes impotence in male smokers, and less than one fifth (19.1%) reported that smoking causes blindness (see Figure 1).
Figure 1.
Knowledge of smoking causing blindness differed across countries. A relatively small proportion of respondents from Canada (13.0%), the United States (9.5%), and the United Kingdom (9.7%) reported that they believed smoking caused blindness, and just less than half of the respondents from Australia (47.2%) indicated that smoking causes blindness (see Figure 2). In all 4 countries, for those who either reported “No” or “Don’t Know,” more participants responded “No” (i.e., smoking does not cause blindness) rather than “Don’t Know.” A pairwise comparison of the proportions of respondents that answered “Yes” with those who indicated “No” and “Don’t Know” showed significant country pair differences (P < 0.001) except for the United States–United Kingdom pairing (P < 0.759, using a Pearson χ2 test).
Figure 2.
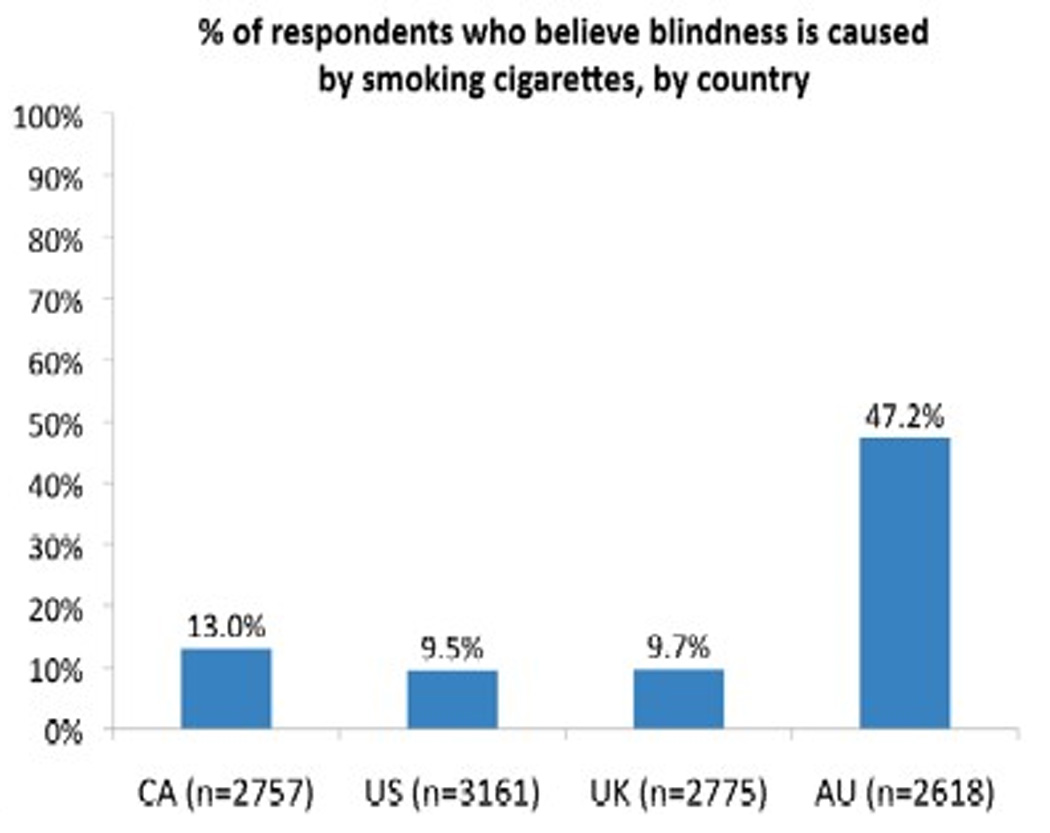
Logistic regression analyses were conducted to identify the factors that predicted knowledge of the causal association between smoking and blindness (n=11,249). Table 2 shows that Canadian, United States, and United Kingdom smokers are much less likely to know that smoking causes blindness compared with Australian smokers. People with lower levels of education were significantly less likely to know that smoking causes blindness relative to people with moderate or high education levels. People from the ethnic or linguistic majority were less likely than those from the minority group to know that smoking causes blindness; however, the results were not statistically significant. Knowledge that smoking causes blindness did not differ across levels of income, sex, or age.
Table 2.
Logistic Regression: Knowledge among Daily Smokers that Smoking Causes Blindness, Weighted
| Odds Ratio | 95% C.I. | p | |
|---|---|---|---|
| Sex | |||
| Female (vs. Male) | .964 | .858–1.084 | .543 |
| Age | |||
| 18–24 (vs. 25+) | 1.035 | .856–1.252 | .723 |
| Ethnicity | |||
| White/English Speaking (vs. Other) | .843 | .699–1.017 | .075 |
| Education | |||
| Low (vs. Medium/High) | .869 | .768–.983 | .025* |
| Income | |||
| Low (vs. No Answer) | 1.074 | .846–1.363 | .220 |
| Medium/High (vs. No Answer) | .955 | .759–1.200 | |
| Country | |||
| Canada (vs. Australia) | .164 | .141–.191 | <.001* |
| United Kingdom (vs. Australia) | .111 | .094–.131 | |
| United States (vs. Australia) | .121 | .101–.145 |
indicates a statistically significant finding
DISCUSSION
This is the first study to report awareness of “blindness” as a smoking-related condition with nationally representative samples of smokers. Most smokers in this survey were aware of some negative health outcomes from smoking, specifically chronic health issues that can result in death, but relatively few respondents understood that smoking is a risk for non–life-threatening health effects, such as “blindness.” Australians were much more likely to report smoking causes blindness. The most likely explanation for the difference between Australia and the other 3 countries is that since 1998, Australia has had a variety of public health and social marketing campaigns to educate citizens about the causal association of smoking and blindness as part of its National Tobacco Advertising Campaign.40 This campaign has included various forms of paid advertising, including a television commercial that explains AMD as part of the “Every Cigarette is Doing You Damage” campaign. However, even with more than a decade of health education efforts (albeit not continuous), less than half of the Australian respondents believed that blindness could be caused by smoking.
It is commonly assumed and often argued by the tobacco industry that smokers are adequately informed about the health risks of smoking.49–51 The results of this study and other reported studies35–37 show that smokers have not been adequately educated about some of the health implications of smoking, specifically that smoking causes blindness, except in part where governments have taken proactive steps to inform them. The lack of knowledge about smoking and blindness crosses all sociodemographic groups we investigated.
Public health campaigns linking smoking and blindness are effective at encouraging smokers to seek cessation supports.42,43 The American Public Health Association has recommended that “Producers of all tobacco cessation materials include information that shows the negative relation between tobacco use and environmental exposure to smoke to an increasing risk of blindness.”52 The American Public Health Association has also recommended that “All national professional health care organizations prompt clinicians to provide information about the link between smoking and eye diseases to their evidence-based intervention counseling.” The results of this study suggest that the eye health message will be new for most smokers in these 4 countries and presumably most jurisdictions across the world. This is likely to result in more patients seeking information or advice from their eye care professionals about their increased risk of “blindness.”
A potential next step after this study is to determine the extent to which optometrists and ophthalmologists currently work to educate their patients about the causal association of smoking and “blindness,” either to discourage nonsmokers from starting to smoke or to encourage smokers to quit and not resume smoking. The need for increased involvement from eye care professionals in this domain has been highlighted previously by numerous public health and eye health researchers.53–55 It is important to understand how these primary health care professionals currently address their patients’ smoking behaviors and what, if any, opportunities or barriers exist in more meaningfully integrating their profession into cessation referral networks. Other next steps may include the development of clinical practice guidelines on how to address tobacco use with patients. Similar guidelines have already been developed for primary care providers and other health care workers including family physicians, dentists, pharmacists, nurses, and physiotherapists.56
This study is limited in that respondents may have different understandings of what the term blindness means, and these different ideas about vision loss and definitions may have influenced how participants responded. The survey instrument also did not use a distracter condition for the knowledge questions.
CONCLUSION
Smokers recognize that smoking is associated with diseases that cause premature death but are less likely to realize that smoking can cause blindness, a health condition more related to quality of life. These findings suggest that public education campaigns contribute to higher knowledge among smokers about the causal links between smoking and blindness; however, these campaigns may not be enough on their own to raise knowledge in the majority of the public. There is an opportunity for both public health and eye health communities to educate smokers and nonsmokers about the effects of smoking on eye health to improve quit rates and help discourage people from starting to smoke. Future research is needed to determine what eye health professionals around the world are currently doing with respect to smoking behavior and their patients and what can be done to further engage this community in tobacco control efforts including cessation referral and prevention efforts.
Acknowledgments
Funding: Research funding is from the National Cancer Institute of the United States R01CA100362 and P50 CA111236 (Roswell Park Transdisciplinary Tobacco Use Research Center), Canadian Institutes of Health Research (57897 and 79551), Robert Wood Johnson Foundation (045734), National Health and Medical Research Council of Australia (265903), Cancer Research UK (C312/A3726), Canadian Tobacco Control Research Initiative (014578), Centre for Behavioural Research and Program Evaluation, National Cancer Institute of Canada/Canadian Cancer Society, and the Ontario Institute of Cancer Research. Additional support is from a Canadian Institutes of Health Research Doctoral Award and the Canadian Institutes of Health Research Strategic Training Program in Tobacco Research
Contributor Information
Ryan David Kennedy, University of Waterloo, Waterloo, Ontario, Canada; Global Center for Tobacco Control, Harvard School of Public Health, Boston, Massachusetts
Marlee M. Spafford, University of Waterloo, Waterloo, Ontario, Canada
Carla M. Parkinson, University of Waterloo, Waterloo, Ontario, Canada
Geoffrey T. Fong, University of Waterloo, Waterloo, Ontario, Canada
REFERENCES
- 1.Klein R, Knudtson MD, Cruickshanks KJ, et al. Further observations on the association between smoking and the long-term incidence and progression of age-related macular degeneration. The Beaver Dam Eye Study. Arch Ophthalmol. 2008;126:115–121. doi: 10.1001/archopht.126.1.115. [DOI] [PubMed] [Google Scholar]
- 2.O’Dell LE. Smoking as a risk factor for AMD. Optometry. 2008;79:293–294. [Google Scholar]
- 3.Gurwood AS. Relationship between smoking and risk of age-related macular degeneration. Optometry. 2006;77:206. [Google Scholar]
- 4.Khan JC, Thurlby DA, Shahid H, et al. Smoking and age related macular degeneration: the number of pack years of cigarette smoking is a major determinant of risk for both geographic atrophy and choroidal neovascularisation. Br J Ophthalmol. 2006;90:75–80. doi: 10.1136/bjo.2005.073643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Solberg Y, Rosner M, Belkin M. The association between cigarette smoking and ocular diseases. Surv Ophthalmol. 1998;42:535–547. doi: 10.1016/s0039-6257(98)00002-2. [DOI] [PubMed] [Google Scholar]
- 6.Kelly SP, Thornton J, Edwards R, et al. The causal association between tobacco smoking and cataract. J Cataract Refract Surg. 2005;31:2395–2404. doi: 10.1016/j.jcrs.2005.06.039. [DOI] [PubMed] [Google Scholar]
- 7.Weintraub JM, Willett WC, Rosner B, et al. Smoking cessation and risk of cataract extraction among US women and men. Am J Epidemiol. 2005;155:72–79. doi: 10.1093/aje/155.1.72. [DOI] [PubMed] [Google Scholar]
- 8.Christen WG, Glynn RJ, Ajani UA, et al. Smoking cessation and risk of age-related cataract in men. JAMA. 2000;284:713–716. doi: 10.1001/jama.284.6.713. [DOI] [PubMed] [Google Scholar]
- 9.Au Eong K. Age-related macular degeneration: an emerging challenge for eye care and public health professionals in the Asia Pacific region. Ann Acad Med Singapore. 2006;35:133–135. [PubMed] [Google Scholar]
- 10.Tomany SC, Wang JJ, Van Leeuwen R, et al. Risk factors for incident age-related macular degeneration: Pooled findings from 3 continents. Ophthalmology. 2004;111:1280–1287. doi: 10.1016/j.ophtha.2003.11.010. [DOI] [PubMed] [Google Scholar]
- 11.Cheng ACK, Pang CP, Leung ATS, et al. The association between cigarette smoking and ocular diseases. Hong Kong Med J. 2000;6:195–202. [PubMed] [Google Scholar]
- 12.Chung SM, Gay CA, McCrary JA. Nonarteritic ischemic optic neuropathy. The impact of tobacco use. Ophthalmology. 1994;101:781–783. doi: 10.1016/s0161-6420(94)31266-8. [DOI] [PubMed] [Google Scholar]
- 13.Rizzo JF, Lessell S. Tobacco amblyopia. Am J Ophthalmol. 1994;116:84–87. doi: 10.1016/s0002-9394(14)71749-0. [DOI] [PubMed] [Google Scholar]
- 14.Mülhauser I, Sawicki P, Berger M. Cigarette-smoking as a risk factor for macroproteinuria and proliferative retinopathy in type I (insulin-dependent) diabetes. Diabetologia. 1986;29:640–643. doi: 10.1007/BF00453501. [DOI] [PubMed] [Google Scholar]
- 15.Center for Health Promotion and Education, Office on Smoking and Health, Public Health Service, Office of the Surgeon General. The Health consequences of smoking: nicotine addiction. A report of the Surgeon General. DHHS Publication No. (CDC) 88-8406. Rockville: Center for Health Promotion and Education, Office on Smoking and Health; 1988. [Google Scholar]
- 16.National Institute on Drug Abuse. NIDA Research Report: Tobacco Addiction. NIH publication no. 09-4342. Bethesda: NIDA, NIH, DHHS; Printed July 1998. Revised 2009. [Google Scholar]
- 17.Benowitz NL. Nicotine addiction. N Engl J Med. 2010;362:2295–2303. doi: 10.1056/NEJMra0809890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Cancer Institute. Smoking and Tobacco Control Monograph no. 10. NIH publication no. 99-4645. Bethesda: U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institutes; 1999. Health effects of exposure to environmental tobacco smoke: the Report of the California Environmental Protection Agency. [Google Scholar]
- 19.Health Canada. [Last accessed July 14, 2010];Tobacco: behind the smoke. Available at: http://www.hc-sc.gc.ca/hc-ps/tobac-tabac/fact-fait/smoking-tabagisme-eng.php.
- 20.The Health and Environment Handbook for Health Professionals. Ottawa, Ontario: Health Canada Publications; 1998. The Great Lakes Health Effects Program, Health Canada and Public Health Branch, Ontario Ministry of Health. Contaminant profiles. [Google Scholar]
- 21.Ambrose JA, Barua RS. The patho-physiology of cigarette smoking and cardiovascular disease: an update. J Am Coll Cardiol. 2004;43:1731–1737. doi: 10.1016/j.jacc.2003.12.047. [DOI] [PubMed] [Google Scholar]
- 22.Wiencke JK, Thurston SW, Kelsey KT, et al. Early age at smoking initiation and tobacco carcinogen DNA damage in the lung. JNCI J Natl Cancer Inst. 1999;91:614–619. doi: 10.1093/jnci/91.7.614. [DOI] [PubMed] [Google Scholar]
- 23.Fraga CG, Motchnik PA, Wyrobek AJ, et al. Smoking and low antioxidant levels increase oxidative damage to sperm DNA. Mutation Research/Fundamental and Molecular Mechanisms of Mutagenesis. 1996;351:199–203. doi: 10.1016/0027-5107(95)00251-0. [DOI] [PubMed] [Google Scholar]
- 24.Sopori M. Effects of cigarette smoke on the immune system. Nat Rev Immunol. 2002;2:372–377. doi: 10.1038/nri803. [DOI] [PubMed] [Google Scholar]
- 25.McNabola A, Gill LW. The control of environmental tobacco smoke: a policy review. Int J Environ Res Pub Health. 2009;6:741–758. doi: 10.3390/ijerph6020741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.US Surgeon General. The Health Consequences of Smoking: a Report of the Surgeon General. Atlanta: Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2004. [Google Scholar]
- 27.Covert D, Berdeaux G, Mitchell J, et al. Quality of life and health economic assessments of age-related macular degeneration. Surv Ophthalmol. 2007;52(1, suppl 1):S20–S25. doi: 10.1016/j.survophthal.2006.10.014. [DOI] [PubMed] [Google Scholar]
- 28.Mojon-Azzi SM, Sousa-Poza A, Mojon DS. Impact of low vision on well-being in 10 European countries. Ophthalmologica. 2008;222:205–212. doi: 10.1159/000126085. [DOI] [PubMed] [Google Scholar]
- 29.Kelly SP, Thornton J, Lyratzopoulos G, et al. Smoking and blindness. Strong evidence for the link, but public awareness lags. Br Med J. 2004;328:357–358. [Google Scholar]
- 30.Thornton J, Edwards R, Mitchell P, et al. Smoking and age-related macular degeneration: a review of association. Eye. 2005;19:935–944. doi: 10.1038/sj.eye.6701978. [DOI] [PubMed] [Google Scholar]
- 31.Mitchell P, Chapman S, Smith W. Smoking is a major cause of blindness. Med J Aust. 1999;171:173–174. doi: 10.5694/j.1326-5377.1999.tb123591.x. [DOI] [PubMed] [Google Scholar]
- 32.Hammond D, Fong GT, McNeill A, et al. Effectiveness of cigarette warning labels in informing smokers about the risks of smoking: findings from the International Tobacco Control (ITC) Four Country Survey. Tob Control. 2006;15(suppl III):iii19–iii25. doi: 10.1136/tc.2005.012294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Roth LK, Taylor HS. Risks of smoking to reproductive health: assessment of women’s knowledge. Am J Obstet Gynecol. 2001;184:934–939. doi: 10.1067/mob.2001.112103. [DOI] [PubMed] [Google Scholar]
- 34.Bintz D. Eye See Tobacco Free Program targets new contact lens wearers on dangers of tobacco use. Rural Roads. 2006;4:10–17. [Google Scholar]
- 35.Noertjojo K, Maberley D, Basset K, et al. Awareness of eye diseases and risk factors: identifying needs for health education and promotion in Canada. Can J Opthalmol. 2006;41:617–623. doi: 10.1016/S0008-4182(06)80035-9. [DOI] [PubMed] [Google Scholar]
- 36.Bidwell G, Sahu A, Edwards R, et al. Perceptions of blindness related to smoking: a hospital-based cross-sectional study. Eye. 2005;19:945–948. doi: 10.1038/sj.eye.6701955. [DOI] [PubMed] [Google Scholar]
- 37.Ng DHL, Roxburgh STD, Sanjay S, et al. Awareness of smoking risks and attitudes towards graphic health warning labels on cigarette packs: a cross-cultural study of two populations in Singapore and Scotland. Eye. 2010;24:864–868. doi: 10.1038/eye.2009.208. [DOI] [PubMed] [Google Scholar]
- 38.Moradi P, Thornton J, Edwards R, et al. Teenagers’ perceptions of blindness related to smoking: a novel message to a vulnerable group. Br J Ophthalmol. 2007;91:605–607. doi: 10.1136/bjo.2006.108191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pisinger C, Glumer C, Toft U, et al. High risk strategy in smoking cessation is feasible on a population-based level. The Inter99 study. Prev Med. 2008;46:579–584. doi: 10.1016/j.ypmed.2008.02.026. [DOI] [PubMed] [Google Scholar]
- 40.Australian Government Department of Health and Ageing. [Last accessed January 4, 2010];1997–2003 National Tobacco Campaign Evaluation Response and Recall Measures among Smokers and Recent Quitters. 2004 Available at: http://www.health.gov.au/internet/quitnow/publishing.nsf/Content/A290E7F6AFAA3F1ACA257475001ADBEE/$File/2003report.pdf. [Google Scholar]
- 41.Carroll T, Rock B. Generating Quitline calls during Australia’s National Tobacco Campaign: effects of television advertisement execution and programme placement. Tob Control. 2003;12(suppl II):ii40–ii44. doi: 10.1136/tc.12.suppl_2.ii40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Donovan RJ, Boulter J, Borland R, et al. Continuous tracking of the Australian National Tobacco Campaign: advertising effects on recall, recognition, cognitions and behavior. Tob Control. 2003;12(suppl II):ii30–ii39. doi: 10.1136/tc.12.suppl_2.ii30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wilson N, Grigg M, Cameron G, et al. Smoking and Blindness advertisements are effective in stimulating calls to a national quitline. Br Med J. 2004;238:537–538. [Google Scholar]
- 44.Tobacco Labelling Resource Centre. [Last accessed January 25, 2011];Health Effects Eye. Available at: http://www.tobaccolabels.ca/healthwarningimages/theme/health_effects_eye. [Google Scholar]
- 45.World Health Organization (WHO) [Last accessed July 30, 2009];About WHO framework convention on tobacco control. Available at: http://www.who.int/fete/about/en/index.html.
- 46.Fong GT, Cummings KM, Borland R, et al. The conceptual framework of the International Tobacco Control (ITC) Policy Evaluation Project. Tob Control. 2006;15:iii3–iii11. doi: 10.1136/tc.2005.015438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Thompson ME, Fong GT, Hammond D, et al. Methods of the International Tobacco Control (ITC) Four Country Survey. Tob Control. 2006;15(suppl 3):iii12–iii18. doi: 10.1136/tc.2005.013870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.ITC Four Country Survey Team. [Last accessed January 10, 2010];International Tobacco Control Policy Evaluation Survey (ITC 4-Country Survey) Wave 1 Technical Report. Available at: http://www.itcproject.org/Library/countries/4country/reports/itcw1techr. [Google Scholar]
- 49.Cummings KM, Hyland A, Giovino GA, et al. Are smokers adequately informed about the health risks of smoking and medicinal nicotine? Nicotine Tob Res. 2004;6(suppl 3):S333–S340. doi: 10.1080/14622200412331320734. [DOI] [PubMed] [Google Scholar]
- 50.Wilkenfeld J, Henningfield J, Slade J. It’s time for a change: cigarette smokers deserve meaningful information about their cigarettes. J Natl Cancer Inst. 2000;92:90–92. doi: 10.1093/jnci/92.2.90. [DOI] [PubMed] [Google Scholar]
- 51.Cummings KM, Morley CP, Hyland A. Failed promises of the cigarette industry and its effect on consumer misperceptions about the health risks of smoking. Tob Control. 2002;11(suppl I):i110–i116. doi: 10.1136/tc.11.suppl_1.i110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.American Public Health Association. [Last accessed July 14, 2010];Advocacy and policy: preventing vision loss through smoking cessation. Available at: http://www.apha.org/advocacy/policy/policysearch/default.htm?id=1364.
- 53.Loo DL, Ng DH, Tang W, et al. Raising awareness of blindness as another smoking related condition: A public health role for optometrists? Clin Exp Optom. 2009;92:42–44. doi: 10.1111/j.1444-0938.2008.00283.x. [DOI] [PubMed] [Google Scholar]
- 54.Passut J. Primary eye care providers should counsel patients on smoking cessation. Primary Care Optometry News. 2008;13:1, 18–19. [Google Scholar]
- 55.Sheck LH, Field AP, McRobbie H, et al. Helping patients to quit smoking in the busy optometric practice. Clin Exp Optom. 2009;92:75–77. doi: 10.1111/j.1444-0938.2009.00348.x. [DOI] [PubMed] [Google Scholar]
- 56.Fiore MC. US public health service clinical practice guideline: treating tobacco use and dependence. Respir Care. 2000;45:1200–1262. [PubMed] [Google Scholar]


