Abstract
(1) Purpose
To describe survivorship services provided by the Children's Oncology Group (COG), an assessment of services was undertaken. Our overall aim was 1) to describe survivorship services, including the extent of services provided, resources (personnel, philanthropy, research funding), billing practices, and barriers to care and 2) to describe models of care that are in use for childhood cancer survivors and adult survivors of childhood cancer.
(2) Methods
179 of 220 COG institutions (81%) completed an internet survey.
(3) Results
One hundred fifty-five (87%) reported providing survivorship care. Fifty-nine percent of institutions provide care for their pediatric population in specialized late effects programs. For adult survivors, 47% of institutions chose models of care which included transitioning to adult providers for risk-based health care, while 44% of institutions keep survivors indefinitely at the treating institution (Cancer Center Based Model without Community Referral). Sixty-eight percent provide survivors with a copy of their survivorship care plan (SCP). Only 31% of institutions provide a detailed summary of results after each clinic visit, and 41% have a database to track survivor health outcomes. Survivorship care for initial and annual visits is estimated to be minimally 122 and 91 minutes respectively. The most prevalent barriers to care were the lack of dedicated time for program development and a perceived insufficient knowledge on the part of the clinician receiving the transition referral.
(4) Conclusions
Not all COG institutions provide dedicated survivorship care, care plans, or have databases for tracking outcomes. Transitioning to adult providers is occurring within the COG. Survivorship care is time-intensive.
Keywords: Cancer survivorship, late effect programs, late effect services
Introduction
Advances in the treatment of childhood cancer, improved supportive care strategies, enhanced diagnostic testing, and enrollment on clinical trials over several decades have contributed to a growing number of cancer survivors. As a result, children are surviving their diseases such that there is an estimated 5 year survival rate of 80% [1] and an estimated 300,000 cancer survivors in the United States [2-3]. Two thirds of survivors may exhibit some late effect of their therapy. [4-5] These late effects may be mild to severe, and include multiple physical and psychosocial health care problems such as changes in physical appearance, organ dysfunction, infertility, neurocognitive impairments, cardiotoxicity, second neoplasms, endocrinopathies, musculoskeletal dysfunction, and psychosocial challenges [5-30].
Despite hope that more contemporary protocols may reduce the frequency and severity of late effects, lifelong risk-based care is recommended for childhood cancer survivors (CCS). The need for health care transition during young adulthood from pediatric to adult-oriented providers has been advocated as a means of continuing appropriate monitoring and management of late effects across the lifespan [31]. However the best clinical practices, models of survivorship care, costs of providing survivorship care and transitioning practices linked to maximizing health care outcomes have not been fully delineated or evaluated. The Institute of Medicine and leaders in cancer survivorship have recommended that pediatric oncology begin the process of examining and evaluating services for survivors [2]. A first step in this process has been accomplished via the development of several guidelines [20-22, 32] which provide the foundation for further assessment of outcomes based on treatment exposures.
Our aims were 1) to describe survivorship services, including the extent of services provided, resources (personnel, philanthropy, research funding), billing practices, and barriers to care and 2) to describe models of care that are in use for childhood cancer survivors and adult survivors of childhood cancer. Specifically included in this survey were questions assessing health care transition practices for young adult survivors, given the emerging importance of that issue as this population ages.
Methods
A needs assessment of the COG Nursing Discipline membership revealed that there was uncertainty about how COG institutions provide survivorship care. The absence of literature about late effects services within COG warranted the development of a concept proposal to address this issue. Since the scope of this project crossed several committees within the COG, support for the concept proposal was obtained from the leadership of the Nursing Discipline, Late Effects and the Adolescent/Young Adult Committees.
A 67-item online survey was developed and housed on an investigator's institutional website from February 19, 2007 to August 20, 2007. Email announcements were sent to existing COG member institutions in good standing and to those in provisional status at the time of the project. An email announcement about the survey, including an introductory letter and instructions, was initially sent to institutional COG Principal Investigators (PIs) and institutional COG Nursing Responsible Investigators (RIs). To increase participation, two additional repeat email notifications were sent to PIs, Nursing RIs and clinical research associates (CRAs) approximately one month and two months later. For those institutions not responding to email notifications within the designated survey timeframe, the investigators made personal contact with institutional personnel to assure that the notification had reached the appropriate survivorship care personnel, and an additional two week time extension was granted to these institutions for survey completion. Institutions were informed that survey responses would be reported collectively for the COG, not individually. One set of responses per institution was requested.
The introductory screen seen by each participant prior to initiation of the survey informed the participant about the time required to complete the survey (estimated at 15-20 minutes). Participants were advised to complete the survey in its entirety due to the inability of the survey to recognize where participants left off. However, if participants did not initially complete the survey in its entirety, but returned later to complete it, the second, more complete set of answer responses was utilized.
In order to prepare participants for the types of questions that would be asked, it was recommended that each participant be aware of some general background information. Five examples of the types of general background information that would be necessary were provided on the introductory screen, including demographics, size and extent of services, personnel resources, funding resources and billing/coding information. Contact email and phone numbers of study investigators were provided to answer questions related to the survey.
The online survey asked about survivorship services, including the extent of services provided, program size and resources (including personnel, philanthropy and research funding), billing practices and perceived barriers to care. Additional information was ascertained to describe survivorship services and models of care utilized for adult survivors of childhood cancer. Demographic program information was collected for periodic updating of the Late Effects Directory of Services, currently housed on the CureSearch website at www.childrensoncologygroup.org.
An online survey service, Zoomerang™, was used for survey dissemination. Zoomerang™ provided a web-based product for internet surveys and included a variety of question formats, including yes/no, multiple choice, multiple response, and open-ended questions. Skip logic also was available to direct participants to omit certain questions depending on how a previous question was answered. For those institutions who reported that they did not provide late effects services no further information was obtained. Participants were allowed to skip questions at their discretion.
Survey responses were compiled by Zoomerang™ and results were available for download in either graphic or raw-data format. Raw data were downloaded in comma delimited format and transferred to an SPSS 14.0 for Windows (©SPSS, Inc.) database where statistical results were computed. Descriptive statistics, including frequency counts, percentages and means for nominal and ordinal variables were tabulated. Cross tabulation tables were also conducted to examine the relationships between responses to different questions. Responses to open-ended questions were tabulated into frequency distributions by two study investigators. An editing, organizing style of analysis was used. Responses in “other” categories were grouped according to themes. Where coding varied, investigators shared findings and came to agreement for coding [33]. Because the volume of data was not difficult to manage, qualitative data management software was not deemed necessary. Single responses from institutions were collected. In 3 cases 2 sets of institutional responses were received. In 2 of the 3 sets of institutional responses answers were identical. In the third case the more complete set of answers was used.
Results
Survivorship Services in COG Institutions
One hundred seventy-nine (81%) of 220 COG member institutions completed the online survey. Eighty-seven percent reported providing late effect (LE) services to survivors, while 13% of institutions reported that they did not. For those institutions who did not provide LE services no further information was obtained.
Fifty-nine percent of institutions who offer care to cancer survivors reported providing that care in a specialized LE program by a designated LE provider, 23% in regular oncology clinic by a survivor's treating oncologist, 16% in oncology clinic by a health care provider (HCP) staffing clinic that day, and a small number (2%) were beginning survivorship programs or using various combinations of health care providers when delivering care. Twenty-five institutions did not answer this question.
Questions were asked about selected subgroups of survivors, categorized as stem cell transplant survivors (SCTS), central nervous system survivors (CNSS) and survivors of non-oncologic conditions (e.g., those who may have received chemotherapy or irradiation for treatment of histiocytosis) in order to further define services for these groups. These survivors were eligible for late effects services in 94%, 97%, and 84% percent of institutions respectively. Eligibility criteria for entry into LE services for these selected subgroups varied widely. Some criteria were time dependent, some were protocol-or diagnosis-specific, some were dependent on current clinical status (i.e. no graft vs. host disease) and other criteria were dependent on the discretion of the treating physician. Some had no specific criteria or fixed formal criteria for referral to LE services.
Additional information about services for survivors who were not originally treated at each responding institution was ascertained. Eighty-eight percent of responding institutions provide clinical consultations to survivors originally treated at other institutions, and more than half (55%) do not offer consultation by phone. Patients can self-refer for LE services in 83% of institutions.
Pediatric Survivorship Services
General Practices
Routines for pediatric cancer survivors
Fifty percent of participants reported that survivors come to the LE clinic and are referred to specialists at alternate times. Thirty-five percent reported that survivors are seen by their general oncologist who manages their survivorship care and are referred to specialists at alternate times. Eight percent reported that survivors come to the clinic staffed by the LE team and required specialists, and six percent report various combinations of the aforementioned responses. Sixty seven percent of participants reported that risk-based screening (e.g. echocardiogram, bone density test) if indicated, would be done at the same LE clinic visit, while 33% reported that it would be scheduled on another day time.
Patient educational materials
Sixty-eight percent of participants reported that they provide survivors a copy of their survivorship care plan (SCP)/oncology treatment exposure summary, while 32% did not. Sixty-nine percent of participants reported that they did not provide written documentation about results to survivors after each visit.
Average Time for Survivor-related Services
Information was collected about the average amount of time health care personnel spend per survivor for 1) preparation of SCP 2) scheduling of tests, 3) clinical “face to face” time for an initial visit, 4) clinical “face to face” time spent in annual visits, 5) gathering, interpreting and compiling results, 6) post clinic conferencing, and 7) communication of results. These data were collected in time interval ranges expressed in minutes (less than 15, 15-30, 31-60, 61-90, 91-120, and greater than 120 minutes).
Overall survivor-related care
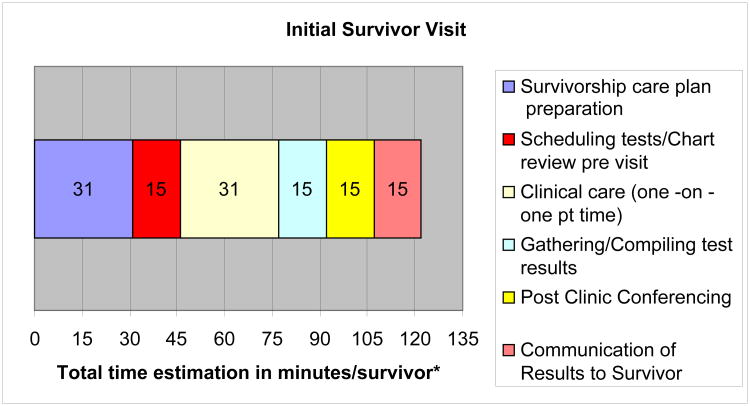
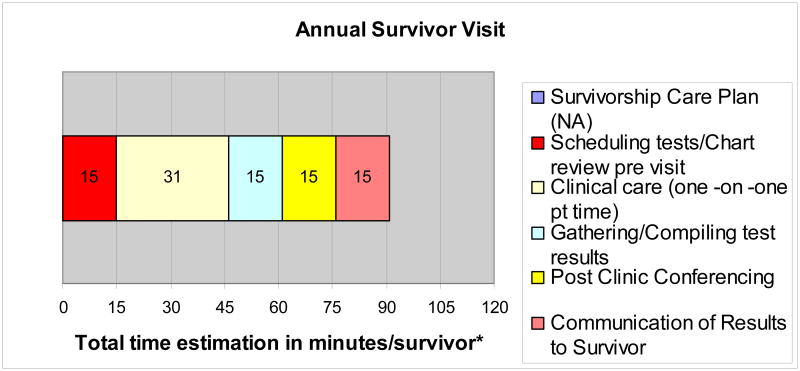
Estimates were calculated for the minimum amount of time required to complete various activities related to a scheduled survivor evaluation (pre-clinic preparation, direct contact time and post-clinic management) for both initial and annual visits. Each initial visit includes the preparation of the SCP and is estimated to require at least 122 minutes. Each annual visit (without preparation of the survivorship care plan) was calculated to require about 91 minutes. These data are illustrated in Figures 1 and 2.
Figure 1. Minimal Total Time Estimate for Initial Survivor Visit: 122 Minutes.
*Time estimations were calculated for the minimum amount of time required by at least two thirds of institutions for completion of various activities related to a scheduled survivor evaluation.
Figure 2. Minimal Total Time Estimate for Annual Survivor Visit: 91 minutes.
*Time estimations were calculated for the minimum amount of time required by at least two thirds of institutions for completion of various activities related to a scheduled survivor evaluation.
Adult Survivorship Care
Given the large number of survivors now entering adulthood we inquired “At what age (if applicable) are CCS referred outside the treating/pediatric center?” Out of 156 responses, 35% see adult survivors indefinitely at the treating institution and do not carry out transition elsewhere for continuation of risk-based care. Another 31% transition them when the survivor is ready, while others keep them to age 18 (5%), 21 (17%), 25 (4%) or 30 years old (1%).
To better define models for adult survivor care, four recognized models were described, and participants were asked to select from one of these, or further describe their own.[34] The most commonly chosen model provided by 44% of the 161 responding institutions was the “Cancer Center-based Model WITHOUT Community Referral”. This model has been described as a model where survivors are kept indefinitely at the treating institution for their cancer-related/late effects (LE) follow-up care. Generally care is with the same late effects or oncology clinicians who provide care to the pediatric survivor population. Other models and their descriptions are found in Table 1.
Table 1. Models of Cancer Survivor Care Utilized for Adult Survivors N= 161.
| MODEL | Description of Model | Number of institutions selecting model | % |
|---|---|---|---|
| Cancer Center Based Model Without Community Referral | Survivors are kept indefinitely at the treating institution for cancer-related care. Generally care is with the same survivorship team/oncology providers who provide care to the pediatric survivor population |
70 | 44 |
| Community Referral Model | Survivors are transitioned at adulthood to their primary care professional (PCP) for routine cancer- related care Survivors' routine testing is managed and coordinated by the PCP, with the survivorship team/oncology team serving as consultants to multiple PCPs. |
34 | 21 |
| Hybrid Model (Combined Cancer Center and Community Based Model) |
Survivors are transitioned to adult health care providers generally within the same health care system, with established opportunities (e.g. a formal mechanism) for collaborative research, collaboration in clinical care and/or other resource sharing. The survivorship team/oncology team and adult health care provider closely collaborate for survivor care. |
38 | 24 |
| Postal/Internet/Phone based Model | Survivors are dismissed from survivorship/oncology follow-up at the cancer center/treating institution. Contact is made regularly to document survivor outcomes via postal, phone, or internet based inquiry. |
5 | 3 |
| Adult Oncologist | Survivors are referred to adult oncologists for their survivorship care | 4 | 2 |
| In Process of Establishing a Model | 6 | 4 | |
| Other | 4 | 2 |
Barriers to care
Barriers for Pediatric and Adult Survivors
We asked participants to review a list of common barriers to 1) providing optimal long term follow up care and 2) transition, as previously described in the literature for pediatric and adult CCS. Participants were asked to select the three most common barriers in their institution. The most frequently chosen barriers are reported in Table 2 and 3.
Table 2. Barriers in Caring for Pediatric Cancer Survivors (266 responses).
| Barrier | Number of Responses |
|---|---|
| Perceived lack of dedicated time for late effects program development | 76 |
| Not enough funding for support of program | 53 |
| Perceived survivor knowledge deficit about the importance of maintaining cancer related follow-up | 45 |
| Survivor lack of health care insurance or insurance limitations | 34 |
| Perceived lack of survivor desire to be followed by the late effects team | 19 |
| Lack of perceived need or support for LE services/program by other oncologists | 18 |
| There are no barriers in my institution | 12 |
| Other | 9 |
Table 3. Barriers in Transitioning Survivors to Adult Care Providers for Cancer Related Care (238 responses).
| Barrier | Number of Responses |
|---|---|
| Perceived lack of knowledge about late effects on the part of clinician being referred to | 68 |
| Survivor lack of health care insurance or insurance limitations | 48 |
| Perceived survivor knowledge deficit about the importance of maintaining cancer related follow-up into adulthood | 34 |
| Perceived lack of survivor desire to leave the comfort of the treating institution or oncologist | 31 |
| Lack of survivor access to a primary care provider for reasons other than insurance, such as geography | 13 |
| We don't transition | 11 |
| Conflict between COG recommendations for risk-based care and adult provider recommendations | 10 |
| Perceived lack of oncology provider desire to “let go” of survivors | 10 |
| We don't have any barriers | 8 |
| Perceived lack of interest in caring for survivors from adult health care providers | 4 |
| Other | 1 |
Survivorship Databases
Less than half of the institutions (41%) reported having a database which was used to track survivors' clinical health care outcomes or other pertinent clinical information. The databases that were used included ACCESS (49%), Excel (15%), ONCOLOG (7%), institutionally devised/proprietary (7%), and OTHER responses (e.g. web-based, tumor registry assisted databases, Optex, POGO network databases) (22%).
Financial Issues and Support
Billing Practices
We collected information about billing practices according to Current Procedural Terminology (CPT) codes [35]. Seventeen percent of institutions did not respond to this question, and of those who did respond 10% reported that they did not know their billing practices. Most U.S. institutions bill at Level 4/Moderate Complexity Decision Making (CPT 99214) or Level 5/High Complexity Decision Making (CPT 99215). The remainder of the billing practices is reflected in Table 4.
Table 4. Reported Level of Billing for Survivorship Services.
| Number of Institutions | Percent | |
|---|---|---|
| Level 2 (CPT 99212) Straightforward Medical Decision Making | 3 | 2.0 |
| Level 3 (CPT 99213) Low Complexity Medical Decision Making | 14 | 9.5 |
| Level 4 (CPT 99214) Moderate Complexity Medical Decision Making | 47 | 31.8 |
| Level 5 (CPT 99215) High Complexity Medical Decision Making | 42 | 28.4 |
| Other, please specify* | 27 | 18.2 |
| Unknown | 46 | 27.3 |
| Total | 179 | 100.0 |
Other responses reflect billing practices for institutions outside U.S. reflecting universal health care or government health care practices.
Financial support of program operations/activities
About half (51%) of institutions reported some level of institutional/hospital support, such as salary funding. Institutions provided information about the availability (in the previous 5 calendar years) of philanthropic funding for support of LE personnel salaries and clinical care. Philanthropic funding was available but limited. It included salary support in about one third of institutions, while 19% reported philanthropic support for the clinical care of patients. Research funding specifically designated for clinical testing of survivors in the context of a research study (e.g. pulmonary function tests for survivors enrolled in a lung study) was available in about 22% of institutions.
Survivorship clinic personnel
Information was ascertained about various personnel known to be a part of survivorship programs or survivorship clinics. Specifically we asked about the number of personnel in a particular role, not in full time equivalents (FTEs) for each role, including nurse practitioners, physician assistants, nurse coordinators, social workers, administrative support staff, clinical research associates, nutritionists/dieticians, and neuropsychologists/educational specialists. Twenty-eight percent of institutions have no nurse practitioner, 47% have no nurse coordinator, 13% have no social worker, 51% have no nutritionist/dietician, and 26% have no neuropsychologist/education specialist. Additionally one quarter of survivorship programs had no clinical research associate, and 28% had no administrative support staff/secretarial support. Physician assistants were rarely utilized (5%). Thirty-nine percent of institutions reported that they provided dedicated personnel to solve insurance and/or employment related issues.
Discussion
Survivorship services are expanding and institutions are moving closer to reaching the goals set forth in the Institute of Medicine's (IOM) report [2]. Until recently only a few studies have addressed the availability of programs or services for survivors [36-40]. At the time of our survey, 155 of 179 responding institutions in COG (87%) reported providing LE services. This is an increase from a study approximately 10 years prior [37] in which 53% of Children's Cancer Group and Pediatric Oncology Group responding institutions (96) reported having a long term follow up clinic at their institution. In our study, more than half of institutions (59%) provided survivorship care in a specialized LE program by a designated provider. Specific subgroups of survivors, such as CNSS, SCTS, and survivors of non-oncologic diseases with similar treatment exposures, were eligible for LE services. Historically these groups have been followed by neuro-oncology specialists, transplant specialists or perhaps not monitored routinely for late effects. A recent study of programs for CNSS reports that care was provided in designated neuro-oncology long term follow up clinics (31.2%) or in general long term follow up programs for CCS (29.7%) [41]. In our study, ninety-seven percent of CNSS were eligible for survivorship services, lending further support that this subgroup has access to LE specialists.
A recent study reports that there are in excess of 300,000 CCS in the U.S. [3], and many may be lacking risk-based care. Recognizing that only a subset of this population is receiving risk-based care, we asked participants to quantify the total number of survivors eligible for a risk-based visit in the previous calendar year. If each institution participating in our study provided care for this entire population of approximately 300,000 survivors, then we estimate that each institution in our study would be accountable for the follow-up of some 2000 survivors, in either direct care or through referral and transition to community providers. We asked participants to quantify the number of survivors they felt were eligible for LE services at their institution. Our participants had difficulty quantifying a number of eligible survivors in a blank response box, or in many cases used descriptive terms to describe the potential survivorship number, such as “greater than”, “approximately”, “about”, “unknown”. This made the total number of survivors eligible for a survivorship visit uninterpretable. Of note, few participants identified quantities of greater than 1000 survivors, so we conclude that only a small subset of the eligible survivor pool have their risk-based long term care coordinated by institutions within the COG. This conclusion supports previously described findings which suggest that a large number of CCS do not receive recommended risk-based care [42].
Transitional and Adult Services
With an ever growing number of survivors that challenge the capacity for their care [43], institutions face the challenge of how to provide the “best” risk-based care in a time of competing resources, reduction in resources, and lack of trained and experienced providers. Care that is longitudinal, risk-based or -stratified, shared and encompasses formal transition to the adult setting has been advocated by many late effects clinicians, health care policy experts and survivors [2, 34, 43-51]. Our data support that survivors in some COG institutions are being transitioned outside of the catchment area of pediatric oncology for their continuing risk-based care. Formal transition of survivors to adult primary care providers with reciprocal and informative communication has been speculated to be rare [44]. Although our study did not assess methods for facilitating transition nor did it evaluate communication strategies when transitioning, our data reveal that transitioning survivors to adult providers is occurring to varying degrees within COG. Literature on transitioning children and adolescents with other chronic diseases is emerging, and may be informative to pediatric oncology in the future. [52-62]
Various models for risk-based care for adult survivors of pediatric cancers have been reported in the literature. When asked to choose a specific model for adult survivors, the most popular single choice was the Cancer Based Model without Community Referral, the model where survivors are kept indefinitely at the treating institution for their risk-based care (44%). However if one considers that three of the other models provided as choices (except for the postal/internet/phone based model) each included transitioning of survivors outside the realm of pediatric oncology in some capacity, such as to primary care physicians (21%), to adult health providers in the same health care system (24%) or to adult oncologists (2%), then an additional conclusion can be drawn. Cumulatively, it appears that almost equal numbers of COG institutions are transitioning adult survivors to adult providers (47%) as are keeping adult survivors indefinitely at the their institution (44%). Our findings support the work of others who have reported that a multitude of institutional, provider and individual survivor circumstances influence the methods by which adult survivors are systematically followed. In the current study, we have not explored exactly how this care is provided or how carefully this care is planned and executed. Our data indicate there is no single approach that is utilized universally. We recommend an evaluation of specific components of transitional care services as well as studies of methods to address the problem of survivor follow-up attrition [63].
In our study, the top three barriers to providing care for pediatric survivors and for successful transition for adult survivors were consistent with barriers previously reported [46, 64], and underscore the importance of educating survivors and future providers, especially primary care providers, about late effects of cancer treatment.
Approximately two thirds of institutions reported providing survivors with a copy of their SCP. This is far less than would be expected since this practice that has become commonplace in survivorship programs. It is hoped that our data underestimate current practice, and reflect the time of the survey (2007). Survivorship care plans may facilitate survivor knowledge about treatment related exposures, and include important health information that may be used to guide systematic follow-up according to the Children's Oncology Group (COG) Long-Term Follow-up Guidelines for Childhood, Adolescent and Young Adult Cancers [51]. The SCP can function as a communication tool for other clinicians to be knowledgeable about past exposures, and it can be useful in the event of a significant adverse event or when clinical decisions need to be made. Unfortunately, the additional provision of written documentation about pertinent findings after each survivor's health related visit is lacking in most COG institutions (69%), and would be an area for improvement, especially in light of reported survivor knowledge deficits [65] and the perceived barrier of lack of clinician knowledge about late effects. The lack of databases for documentation of health outcomes and clinical information potentially compromises easy accessibility to survivorship data useful for research initiatives. Perhaps a goal for the future preparation of SCP is for documentation to begin when therapy starts, especially for patients with anticipated good prognoses. If a list of exposures is compiled early, utilizing state of the art database technologies or electronic medical records, it could ease the transition to survivorship care by saving time for those abstracting medical records. Passport to Care, in development by the Baylor College of Medicine and the Children's Oncology Group, is an example of an on-line resource designed to provide a readily-accessible record of cancer treatment and associated individualized exposure-related recommendations.[66]
Costs involved in caring for survivors
When survivorship services were in their infancy, clinicians recognized that more time would be required for a comprehensive survivorship examination as compared to a routine oncology visit. In an early study, leukemia survivors required an average of 52 minutes of provider time, as compared to 37 minutes for the routine oncology patient. [67] Our data further support that survivor care is time intensive. Our time estimations were calculated for the minimum amount of time required by at least two thirds of institutions for completion of activities related to a survivor's evaluation (initial and annual visit), which includes pre-clinic preparation, direct contact time and post-clinic management. Therefore our estimations of time spent for various survivor related activities were based on conservative assumptions and are an underestimate of time spent. Exploration of ways to promote optimal health outcomes in a time efficient, cost effective manner is necessary. Furthermore, knowledge of current billing practices as elucidated by this study needs to be coupled with more information derived from research regarding reimbursement patterns.
Limitations
Our study provides initial data about survivorship services that was easily attainable via a web-based survey. Limitations of the study are those inherent to survey-based research. Although we sought to target health care professionals who were most knowledgeable about LE services to provide a single institutional response, we recognize that responses were subjective, and based on the individual participant knowledge. Not all questions were answered by all participants. In future surveys we recommend shorter, targeted surveys with enhanced skip logic so that participants do not become fatigued, and inclusion of a status of completion bar so that participants can track their time to completion of the survey. We also recommend enhanced survey methodology which will save user responses so that the survey can be answered within participant time constraints. Through enhanced survey techniques participants could seek information needed to answer a question, and enter it at a later time, without loss of previous data.
Implications for Cancer Survivors
Institutions within COG are striving to optimize positive outcomes for cancer survivors. Survivorship services are available, including transition, but best practices and models of care have not yet been fully defined. Both survivors and future providers need to be educated about survivorship issues, health-related risks, health promotion behaviors and early intervention strategies. Exploring ways to enhance this knowledge, evaluating strategies for effective teaching utilizing state of the art, cost effective technologies, and testing methods/models which prevent survivor follow-up attrition should be the subject of future study. Integrated and comprehensive transition models focused not only on the physical but the psychosocial needs of survivors are necessary. Finally, collaborative research with adult-focused providers and programs, utilizing survivor input, will be essential for defining and meeting the future needs of these young adult cancer survivors.
Footnotes
Preliminary data from this study was presented in poster at the 10th International Conference on Long-Term Complications of Treatment of Children and Adolescents for Cancer, Niagara on the Lake, Canada, June 2008.
References
- 1.Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T, et al. Cancer statistics, 2008. CA Cancer J Clin. 2008;58:71–96. doi: 10.3322/CA.2007.0010. [DOI] [PubMed] [Google Scholar]
- 2.Hewitt M, Weiner S, Simone J. Childhood Cancer Survivorship: Improving Care and Quality of Life. Wahington DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 3.Mariotto AB, Rowland JH, Yabroff KR, Scoppa S, Hachey M, Ries L, et al. Long-term survivors of childhood cancers in the United States. Cancer Epidemiol Biomarkers Prev. 2009;18:1033–40. doi: 10.1158/1055-9965.EPI-08-0988. [DOI] [PubMed] [Google Scholar]
- 4.Oeffinger KC, Eshelman DA, Tomlinson GE, Buchanan GR, Foster BM. Grading of late effects in young adult survivors of childhood cancer followed in an ambulatory adult setting. Cancer. 2000;88:1687–95. [PubMed] [Google Scholar]
- 5.Oeffinger KC, Mertens AC, Sklar CA, Kawashima T, Hudson MM, Meadows AT, et al. Chronic health conditions in adult survivors of childhood cancer. N Engl J Med. 2006;355:1572–82. doi: 10.1056/NEJMsa060185. [DOI] [PubMed] [Google Scholar]
- 6.Armstrong GT, Liu Q, Yasui Y, Neglia JP, Leisenring W, Robison LL, et al. Late mortality among 5-year survivors of childhood cancer: a summary from the Childhood Cancer Survivor Study. J Clin Oncol. 2009;27:2328–38. doi: 10.1200/JCO.2008.21.1425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Armstrong GT, Sklar CA, Hudson MM, Robison LL. Long-term health status among survivors of childhood cancer: does sex matter? J Clin Oncol. 2007;25:4477–89. doi: 10.1200/JCO.2007.11.2003. [DOI] [PubMed] [Google Scholar]
- 8.Askins MA, Moore BD., 3rd Preventing neurocognitive late effects in childhood cancer survivors. J Child Neurol. 2008;23:1160–71. doi: 10.1177/0883073808321065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bonato C, Severino RF, Elnecave RH. Reduced thyroid volume and hypothyroidism in survivors of childhood cancer treated with radiotherapy. J Pediatr Endocrinol Metab. 2008;21:943–9. doi: 10.1515/jpem.2008.21.10.943. [DOI] [PubMed] [Google Scholar]
- 10.Bowers DC, Liu Y, Leisenring W, McNeil E, Stovall M, Gurney JG, et al. Late-occurring stroke among long-term survivors of childhood leukemia and brain tumors: a report from the Childhood Cancer Survivor Study. J Clin Oncol. 2006;24:5277–82. doi: 10.1200/JCO.2006.07.2884. [DOI] [PubMed] [Google Scholar]
- 11.De Bruin ML, Van Dulmen-den Broeder E, Van den Berg MH, Lambalk CB. Fertility in female childhood cancer survivors. Endocr Dev. 2009;15:135–58. doi: 10.1159/000207613. [DOI] [PubMed] [Google Scholar]
- 12.Gurney JG, Kadan-Lottick NS, Packer RJ, Neglia JP, Sklar CA, Punyko JA, et al. Endocrine and cardiovascular late effects among adult survivors of childhood brain tumors: Childhood Cancer Survivor Study. Cancer. 2003;97:663–73. doi: 10.1002/cncr.11095. [DOI] [PubMed] [Google Scholar]
- 13.Hudson MM, Mertens AC, Yasui Y, Hobbie W, Chen H, Gurney JG, et al. Health status of adult long-term survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. JAMA. 2003;290:1583–92. doi: 10.1001/jama.290.12.1583. [DOI] [PubMed] [Google Scholar]
- 14.Janiszewski PM, Oeffinger KC, Church TS, Dunn AL, Eshelman DA, Victor RG, et al. Abdominal obesity, liver fat, and muscle composition in survivors of childhood acute lymphoblastic leukemia. J Clin Endocrinol Metab. 2007;92:3816–21. doi: 10.1210/jc.2006-2178. [DOI] [PubMed] [Google Scholar]
- 15.Johannesen TB, Rasmussen K, Winther FO, Halvorsen U, Lote K. Late radiation effects on hearing, vestibular function, and taste in brain tumor patients. Int J Radiat Oncol Biol Phys. 2002;53:86–90. doi: 10.1016/s0360-3016(01)02810-3. [DOI] [PubMed] [Google Scholar]
- 16.Kaste SC. Bone-mineral density deficits from childhood cancer and its therapy. A review of at-risk patient cohorts and available imaging methods. Pediatr Radiol. 2004;34:373–8. doi: 10.1007/s00247-003-1132-1. quiz 443-4. [DOI] [PubMed] [Google Scholar]
- 17.Kaste SC. Skeletal toxicities of treatment in children with cancer. Pediatr Blood Cancer. 2008;50:469–73. doi: 10.1002/pbc.21408. discussion 86. [DOI] [PubMed] [Google Scholar]
- 18.Maule M, Scelo G, Pastore G, Brennan P, Hemminki K, Pukkala E, et al. Risk of second malignant neoplasms after childhood central nervous system malignant tumours: an international study. Eur J Cancer. 2008;44:830–9. doi: 10.1016/j.ejca.2008.02.012. [DOI] [PubMed] [Google Scholar]
- 19.Mitby PA, Robison LL, Whitton JA, Zevon MA, Gibbs IC, Tersak JM, et al. Utilization of special education services and educational attainment among long-term survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. Cancer. 2003;97:1115–26. doi: 10.1002/cncr.11117. [DOI] [PubMed] [Google Scholar]
- 20.Mulhern RK, Merchant TE, Gajjar A, Reddick WE, Kun LE. Late neurocognitive sequelae in survivors of brain tumours in childhood. Lancet Oncol. 2004;5:399–408. doi: 10.1016/S1470-2045(04)01507-4. [DOI] [PubMed] [Google Scholar]
- 21.Nagarajan R, Mogil R, Neglia JP, Robison LL, Ness KK. Self-reported global function among adult survivors of childhood lower-extremity bone tumors: a report from the Childhood Cancer Survivor Study (CCSS) J Cancer Surviv. 2009;3:59–65. doi: 10.1007/s11764-008-0073-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nandagopal R, Laverdiere C, Mulrooney D, Hudson MM, Meacham L. Endocrine late effects of childhood cancer therapy: a report from the Children's Oncology Group. Horm Res. 2008;69:65–74. doi: 10.1159/000111809. [DOI] [PubMed] [Google Scholar]
- 23.Neglia JP, Robison LL, Stovall M, Liu Y, Packer RJ, Hammond S, et al. New primary neoplasms of the central nervous system in survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. J Natl Cancer Inst. 2006;98:1528–37. doi: 10.1093/jnci/djj411. [DOI] [PubMed] [Google Scholar]
- 24.Oeffinger KC, Buchanan GR, Eshelman DA, Denke MA, Andrews TC, Germak JA, et al. Cardiovascular risk factors in young adult survivors of childhood acute lymphoblastic leukemia. J Pediatr Hematol Oncol. 2001;23:424–30. doi: 10.1097/00043426-200110000-00007. [DOI] [PubMed] [Google Scholar]
- 25.Reilly JJ. Obesity during and after Treatment for Childhood Cancer. Endocr Dev. 2009;15:40–58. doi: 10.1159/000207609. [DOI] [PubMed] [Google Scholar]
- 26.Ritchey M, Ferrer F, Shearer P, Spunt SL. Late effects on the urinary bladder in patients treated for cancer in childhood: a report from the Children's Oncology Group. Pediatr Blood Cancer. 2009;52:439–46. doi: 10.1002/pbc.21826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Robison LL, Green DM, Hudson M, Meadows AT, Mertens AC, Packer RJ, et al. Long-term outcomes of adult survivors of childhood cancer. Cancer. 2005;104:2557–64. doi: 10.1002/cncr.21249. [DOI] [PubMed] [Google Scholar]
- 28.Shnorhavorian M, Friedman DL, Koyle MA. Genitourinary long-term outcomes for childhood cancer survivors. Curr Urol Rep. 2009;10:134–7. doi: 10.1007/s11934-009-0024-9. [DOI] [PubMed] [Google Scholar]
- 29.Crom DB, Lensing SY, Rai SN, Snider MA, Cash DK, Hudson MM. Marriage, employment, and health insurance in adult survivors of childhood cancer. J Cancer Surviv. 2007;1:237–45. doi: 10.1007/s11764-007-0026-x. [DOI] [PubMed] [Google Scholar]
- 30.Gurney JG, Krull KR, Kadan-Lottick N, Nicholson HS, Nathan PC, Zebrack B, et al. Social outcomes in the Childhood Cancer Survivor Study cohort. J Clin Oncol. 2009;27:2390–5. doi: 10.1200/JCO.2008.21.1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.American Academy of Pediatrics Section on Hematology/Oncology. Long-term follow-up care for pediatric cancer survivors. Pediatrics. 2009;123:906–15. doi: 10.1542/peds.2008-3688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Landier W, Bhatia S. Cancer survivorship: a pediatric perspective. Oncologist. 2008;13:1181–92. doi: 10.1634/theoncologist.2008-0104. [DOI] [PubMed] [Google Scholar]
- 33.Boeije H. A Purposeful Approach to the Constant Comparative Method in the Analysis of Qualitative Interviews Quality and Quantity. 2002;36:391–409. [Google Scholar]
- 34.Friedman DL, Freyer DR, Levitt GA. Models of care for survivors of childhood cancer. Pediatr Blood Cancer. 2006;46:159–68. doi: 10.1002/pbc.20611. [DOI] [PubMed] [Google Scholar]
- 35.American Medical Association. CPT 2010 Professional Edition. 2010. [Google Scholar]
- 36.Taylor A, Hawkins M, Griffiths A, Davies H, Douglas C, Jenney M, et al. Long-term follow-up of survivors of childhood cancer in the UK. Pediatr Blood Cancer. 2004;42:161–8. doi: 10.1002/pbc.10482. [DOI] [PubMed] [Google Scholar]
- 37.Oeffinger KC, Eshelman DA, Tomlinson GE, Buchanan GR. Programs for adult survivors of childhood cancer. J Clin Oncol. 1998;16:2864–7. doi: 10.1200/JCO.1998.16.8.2864. [DOI] [PubMed] [Google Scholar]
- 38.Guilcher GM, Fitzgerald C, Pritchard S. A questionnaire based review of long-term follow-up programs for survivors of childhood cancer in Canada. Pediatr Blood Cancer. 2009;52:113–5. doi: 10.1002/pbc.21701. [DOI] [PubMed] [Google Scholar]
- 39.Aziz NM, Oeffinger KC, Brooks S, Turoff AJ. Comprehensive long-term follow-up programs for pediatric cancer survivors. Cancer. 2006;107:841–8. doi: 10.1002/cncr.22096. [DOI] [PubMed] [Google Scholar]
- 40.Hudson MM, Hester A, Sweeney T, Kippenbrock S, Majcina R, Vear S, et al. A model of care for childhood cancer survivors that facilitates research. J Pediatr Oncol Nurs. 2004;21:170–4. doi: 10.1177/1043454204264388. [DOI] [PubMed] [Google Scholar]
- 41.Bowers DC, Adhikari S, El-Khashab YM, Gargan L, Oeffinger KC. Survey of long-term follow-up programs in the United States for survivors of childhood brain tumors. Pediatr Blood Cancer. 2009;53:1295–301. doi: 10.1002/pbc.22240. [DOI] [PubMed] [Google Scholar]
- 42.Nathan PC, Greenberg ML, Ness KK, Hudson MM, Mertens AC, Mahoney MC, et al. Medical care in long-term survivors of childhood cancer: a report from the childhood cancer survivor study. J Clin Oncol. 2008;26:4401–9. doi: 10.1200/JCO.2008.16.9607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Oeffinger KC, McCabe MS. Models for delivering survivorship care. J Clin Oncol. 2006;24:5117–24. doi: 10.1200/JCO.2006.07.0474. [DOI] [PubMed] [Google Scholar]
- 44.Oeffinger KC, Nathan PC, Kremer LC. Challenges after curative treatment for childhood cancer and long-term follow up of survivors. Pediatr Clin North Am. 2008;55:251–73. xiii. doi: 10.1016/j.pcl.2007.10.009. [DOI] [PubMed] [Google Scholar]
- 45.Mertens AC, Cotter KL, Foster BM, Zebrack BJ, Hudson MM, Eshelman D, et al. Improving health care for adult survivors of childhood cancer: recommendations from a delphi panel of health policy experts. Health Policy. 2004;69:169–78. doi: 10.1016/j.healthpol.2003.12.008. [DOI] [PubMed] [Google Scholar]
- 46.Zebrack BJ, Eshelman DA, Hudson MM, Mertens AC, Cotter KL, Foster BM, et al. Health care for childhood cancer survivors: insights and perspectives from a Delphi panel of young adult survivors of childhood cancer. Cancer. 2004;100:843–50. doi: 10.1002/cncr.20033. [DOI] [PubMed] [Google Scholar]
- 47.Skinner R, Wallace WH, Levitt GA. Long-term follow-up of people who have survived cancer during childhood. Lancet Oncol. 2006;7:489–98. doi: 10.1016/S1470-2045(06)70724-0. [DOI] [PubMed] [Google Scholar]
- 48.Freyer DR, Brugieres L. Adolescent and young adult oncology: transition of care. Pediatr Blood Cancer. 2008;50:1116–9. doi: 10.1002/pbc.21455. [DOI] [PubMed] [Google Scholar]
- 49.Viner R. Bridging the gaps: transition for young people with cancer. Eur J Cancer. 2003;39:2684–7. doi: 10.1016/j.ejca.2003.08.004. [DOI] [PubMed] [Google Scholar]
- 50.Skinner R, Wallace WH, Levitt G. Long-term follow-up of children treated for cancer: why is it necessary, by whom, where and how? Arch Dis Child. 2007;92:257–60. doi: 10.1136/adc.2006.095513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Landier W, Bhatia S, Eshelman DA, Forte KJ, Sweeney T, Hester AL, et al. Development of risk-based guidelines for pediatric cancer survivors: the Children's Oncology Group Long-Term Follow-Up Guidelines from the Children's Oncology Group Late Effects Committee and Nursing Discipline. J Clin Oncol. 2004;22:4979–90. doi: 10.1200/JCO.2004.11.032. [DOI] [PubMed] [Google Scholar]
- 52.Betz CL. Nurse's role in promoting health transitions for adolescents and young adults with developmental disabilities. Nurs Clin North Am. 2003;38:271–89. doi: 10.1016/s0029-6465(02)00050-6. [DOI] [PubMed] [Google Scholar]
- 53.Betz CL. Health care transitions of youth with special health care needs: the never ending journey. Commun Nurs Res. 2008;41:13–29. [PubMed] [Google Scholar]
- 54.Binks JA, Barden WS, Burke TA, Young NL. What do we really know about the transition to adult-centered health care? A focus on cerebral palsy and spina bifida. Arch Phys Med Rehabil. 2007;88:1064–73. doi: 10.1016/j.apmr.2007.04.018. [DOI] [PubMed] [Google Scholar]
- 55.Marelli AJ, Therrien J, Mackie AS, Ionescu-Ittu R, Pilote L. Planning the specialized care of adult congenital heart disease patients: from numbers to guidelines; an epidemiologic approach. Am Heart J. 2009;157:1–8. doi: 10.1016/j.ahj.2008.08.029. [DOI] [PubMed] [Google Scholar]
- 56.Shirodaria CC, Gwilt DJ, Gatzoulis MA. Joint outpatient clinics for the adult with congenital heart disease at the district general hospital: an alternative model of care. Int J Cardiol. 2005;103:47–50. doi: 10.1016/j.ijcard.2004.08.032. [DOI] [PubMed] [Google Scholar]
- 57.Telfair J, Alleman-Velez PL, Dickens P, Loosier PS. Quality health care for adolescents with special health-care needs: issues and clinical implications. J Pediatr Nurs. 2005;20:15–24. doi: 10.1016/j.pedn.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 58.Hagood JS, Lenker CV, Thrasher S. A course on the transition to adult care of patients with childhood-onset chronic illnesses. Acad Med. 2005;80:352–5. doi: 10.1097/00001888-200504000-00009. [DOI] [PubMed] [Google Scholar]
- 59.Lewis-Gary MD. Transitioning to adult health care facilities for young adults with a chronic condition. Pediatr Nurs. 2001;27:521–4. [PubMed] [Google Scholar]
- 60.LoCasale-Crouch J, Johnson B. Transition from pediatric to adult medical care. Adv Chronic Kidney Dis. 2005;12:412–7. doi: 10.1053/j.ackd.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 61.McDonagh JE. Growing up and moving on: transition from pediatric to adult care. Pediatr Transplant. 2005;9:364–72. doi: 10.1111/j.1399-3046.2004.00287.x. [DOI] [PubMed] [Google Scholar]
- 62.McDonagh JE, Viner RM. Lost in transition? Between paediatric and adult services. BMJ. 2006;332:435–6. doi: 10.1136/bmj.332.7539.435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Oeffinger KC, Mertens AC, Hudson MM, Gurney JG, Casillas J, Chen H, et al. Health care of young adult survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. Ann Fam Med. 2004;2:61–70. doi: 10.1370/afm.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ginsberg JP, Hobbie WL, Carlson CA, Meadows AT. Delivering long-term follow-up care to pediatric cancer survivors: transitional care issues. Pediatr Blood Cancer. 2006;46:169–73. doi: 10.1002/pbc.20610. [DOI] [PubMed] [Google Scholar]
- 65.Kadan-Lottick NS, Robison LL, Gurney JG, Neglia JP, Yasui Y, Hayashi R, et al. Childhood cancer survivors' knowledge about their past diagnosis and treatment: Childhood Cancer Survivor Study. JAMA. 2002;287:1832–9. doi: 10.1001/jama.287.14.1832. [DOI] [PubMed] [Google Scholar]
- 66.Poplack D, Fordis M, Horowitz ME, Landier W, Hudson MM, Bhatia S, et al. The Passport for Care Improving the lives of childhood cancer survivors: Development of a novel internet resource for managing long-term health risks. In: Hewitt M, Ganz P, National Coalition for Cancer Survivorship (U.S.)et al., editors. Implementing Cancer Survivorship Care Planning. Washington, DC: The National Academies Press; 2007. pp. 206–41. [Google Scholar]
- 67.Fergusson J, Ruccione K, Waskerwitz M, Perin G, Diserens D, Nesbit M, et al. Time required to assess children for the late effects of treatment. A report from the Childrens Cancer Study Group. Cancer Nurs. 1987;10:300–10. [PubMed] [Google Scholar]