Abstract
Importance
Although the majority of children with an unplanned admission to the hospital are admitted through the emergency department (ED), direct admissions constitute a significant proportion of hospital admissions nationally. Despite this, past studies of children have not characterized direct admission practices or outcomes. Pneumonia is the leading cause of pediatric hospitalization in the United States, providing an ideal lens to examine variation and outcomes associated with direct admissions.
Objectives
To describe rates and patterns of direct admission in a large sample of US hospitals and to compare resource utilization and outcomes between children with pneumonia admitted directly to a hospital and those admitted from an ED.
Design, Setting, and Participants
Retrospective cohort study of children 1 to 17 years of age with pneumonia who were admitted to hospitals contributing data to Perspective Data Warehouse. We developed hierarchical generalized linear models to examine associations between admission type and outcomes.
Main Outcomes and Measures
Outcome measures included (1) length of stay, (2) high turnover hospitalization, (3) total hospital cost, (4) transfer to the intensive care unit, and (5) readmission within 30 days of hospital discharge.
Results
A total of 19 736 children from 278 hospitals met eligibility criteria, including 7100 (36.0%) who were admitted directly and 12 636 (64.0%) through the ED. Rates of direct admission varied considerably across hospitals, with a median direct admission rate of 33.3% (interquartile range, 11.1%-50.0%). Children admitted directly were more likely to be white, to have private health insurance, and to be admitted to small, general community hospitals. In adjusted models, children admitted directly had a 9% higher length of stay (risk ratio, 1.09 [95% CI, 1.07-1.11]), 39% lower odds of high turnover hospitalization (odds ratio [OR], 0.61 [95% CI, 0.56-0.66]), and 12% lower cost (risk ratio, 0.88 [95% CI, 0.87-0.90]) than those admitted through the ED, with no significant differences in transfers to the intensive care unit (OR, 1.29 [95% CI, 0.83-2.00]) or 30-day readmissions (OR, 0.80 [95% CI, 0.57-1.13]).
Conclusions and Relevance
Increasing rates of direct admission among children with access to outpatient care might be an effective strategy to reduce hospital costs and the volume of patients in the ED. Additional research is needed to establish direct admission policies and procedures that are safe and cost-effective.
As health care costs in the United States continue to increase, the growing use of emergency departments (EDs) is being scrutinized by policy makers.1-3 More than 1 million children are admitted to hospitals through EDs annually,3 representing approximately half of all pediatric hospitalizations in the United States.2 An increase in the number of ED visits for ambulatory care–sensitive conditions has been documented in the adult literature,4 with an increasing proportion of individuals admitted to hospitals entering through the ED.5,6 Direct admission is an alternative approach whereby patients are referred by health care providers and admitted without first being seen in the ED. Direct admission may offer benefits over admission through the ED, including reduced costs and improved patient satisfaction,7 while reducing ED volumes. However, direct admission may be associated with delays in initial management, which may have adverse results.5,8 Given the paucity of research in this area, there has been a call for comparative effectiveness research to characterize resource utilization and outcomes among patients admitted through the ED compared with those admitted directly from non-ED settings.6
As the leading cause of pediatric hospitalization nationally, pneumonia is an ideal lens through which to examine associations between admission type and outcomes. Pneumonia is the most common ambulatory care–sensitive condition that results in hospitalization, accounting for more than 160 000 admissions and 1 billion dollars in hospital costs annually.9,10 Pneumonia also accounts for more than 1 million pediatric outpatient clinic visits annually, with approximately 8% of children who receive ambulatory care subsequently admitted to a hospital.11 Our study sought to characterize the rates and outcomes of direct admission across a large sample of US hospitals and to compare resource utilization and outcomes between children with pneumonia admitted directly and those admitted from EDs.
Methods
Study Design and Eligibility Criteria
We conducted a retrospective cohort study of children and adolescents 1 to 17 years of age admitted under inpatient status between July 1, 2007, and June 30, 2010, to hospitals that contribute data to the Perspective Data Warehouse (PDW) (Premier Healthcare Informatics), a highly detailed administrative database that measures health care utilization. The PDW incorporates approximately 15% of all hospitalizations in the United States, represents geographically and structurally diverse hospitals,12-14 and has been used in several studies of pediatric populations.15-17 The PDW contains de-identified information, including demographic characteristics, length of stay (LOS), all International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) discharge diagnoses and procedures, as well as a date-specific record of all billed items, including diagnostic tests, medications, and their associated costs. Data are collected electronically and audited regularly to ensure data integrity. For approximately 75% of hospitals contributing data to the PDW, these data reflected actual hospital costs taken from internal cost accounting systems, whereas the remaining hospitals provided cost estimates based on Medicare cost to charge ratios. Because the data do not contain identifiable information, the institutional review board of Baystate Medical Center in Springfield, Massachusetts, determined that our study did not constitute human subjects research.
We included children with a principal diagnosis of pneumonia (ICD-9-CM codes 480.0-2, 480.8-9, 481, 482.0, 482.30-2, 482.41-2, 482.83, 482.89-90, 483, 484.3, 485, 486, and 487.0), applying a highly specific, previously validated algorithm.18 To ensure that pneumonia was recognized at the time of admission, we excluded all children who did not have antibiotics initiated on the first day of hospitalization. Consistent with other studies, infants younger than 1 year of age were excluded because of the high prevalence of bronchiolitis in this age group and the increased likelihood of misclassifying lower respiratory tract disease.19-21 Children with complex chronic conditions were also excluded.22,23 Children without overnight stays and those admitted to the intensive care unit (ICU) were excluded because of concerns about potential confounding by indication. Children transferred to or from outside facilities or who left the hospital against medical advice were excluded because we were unable to accurately assess LOS or full course of hospital treatments. Patients for whom the admission source was unknown were excluded, as were patients admitted from court or law enforcement. Patients were then classified into 2 groups according to point of origin, a standardized variable on Universal Billing forms: (1) those admitted to the hospital through the ED and (2) those admitted directly to the hospital with physician, clinic, or health maintenance organization referral, without receiving care in the ED. All hospitals in the United States that receive reimbursement from the Centers for Medicare and Medicaid Services are required to use Universal Billing forms to document point of origin, and the validity of point of origin codes has been demonstrated in a previous study.24 In addition, we confirmed the validity of point of origin codes in our data set by assessing for ED billing codes among patients classified as direct admissions and ED admissions. Point of origin codes were consistent with ED billing codes for 12 407 of 12 636 patients (98.2%) who had an ED admission and for 6491 of 7100 patients (91.4%) who had a direct admission.
Outcome Variables
Outcome measures included (1) LOS, reported in days (and not reflective of days in the ED); (2) transfer to the ICU on or after the second day or hospitalization, a measure of clinical deterioration; (3) all-cause readmission within 30 days of hospital discharge; (4) high turnover hospitalization, defined as hospitalizations less than 2 days in duration25,26; and (5) total cost of hospitalization.
Patient, Hospital, and Pneumonia Management Variables
Study participants were characterized on the basis of year of admission, age, sex, race/ethnicity (as recorded by the staff members of participating hospitals using hospital-defined options), insurance status, and comorbid conditions. Characteristics of the admitting hospitals included geographic region, bed size, urban/rural location, children's hospital vs general community hospital, and teaching status. Children's hospitals included both freestanding children's hospitals and children's hospitals within larger adult centers, defined as institutions that had at least 10 pediatric subspecialties recorded in the database. Respiratory season was defined as occurring from October to March. We examined detailed billing and ICD-9-CM procedure codes to identify the use of diagnostic tests and adjunctive therapies. Initial investigations and therapies were defined as those provided in the ED or on the first day of hospitalization. Four initial investigations were defined as markers of disease severity: (1) chest computed tomography, (2) chest ultrasonography, (3) arterial blood gas analysis, and (4) cerebrospinal culture.
Statistical Analysis
We calculated patient-level summary statistics and assessed differences between groups using χ2 tests for categorical variables and Wilcoxon rank sum tests for continuous variables. We developed a hierarchical generalized linear model to estimate a patient's predicted probability, or propensity, for direct admission based on (1) the patient and hospital characteristics listed in Table 1, (2) year of admission, and (3) a random effect for hospital.27 Hierarchical generalized linear models were then developed to model LOS, high turnover hospitalization, total hospital cost, ICU transfer, and readmission, including a random effect for hospital. Logit-link models were used for binary outcomes, and identity-link models were used for log-transformed LOS and cost. Cost and LOS were trimmed at 3 SDs above the mean. Covariates in the adjusted models included propensity for direct admission, admission year, illness severity markers, and hospital and patient characteristics shown in Table 1. Cost models included an adjustment for the hospital costing method. We repeated our analyses in a cohort of children with limited disease severity as reflected in hospital stays of 1-day duration. To ensure the validity of point of origin codes, we repeated our multivariable analyses using the presence or absence of ED billing codes as a surrogate for point of origin codes.
Table 1. Patient and Hospital Characteristics and Initial Diagnostic Testing and Management of Children Admitted Directly to the Hospital Compared With Those Admitted Through the ED.
| Children, No. (%) | |||
|---|---|---|---|
|
|
|||
| Characteristic | Direct Admission (n = 7100) | ED Admission (n = 12 636) | P Value |
| Patient characteristics | |||
|
| |||
| Male sex | 3819 (53.8) | 6776 (53.6) | .82 |
|
| |||
| Age, y | |||
|
| |||
| Mean | 4.6 | 4.4 | <.001 |
|
| |||
| Median (IQR) | 3 (1-6) | 3 (1-6) | |
|
| |||
| Race/ethnicity | |||
|
| |||
| White | 4002 (56.4) | 5643 (44.7) | <.001 |
|
| |||
| Black | 900 (12.7) | 2512 (19.9) | |
|
| |||
| Hispanic | 800 (11.3) | 2088 (16.5) | |
|
| |||
| Other | 1398 (19.7) | 2393 (18.9) | |
|
| |||
| Insurance status | |||
|
| |||
| Public payer | 2993 (42.2) | 6845 (54.2) | <.001 |
|
| |||
| Private payer | 3823 (53.8) | 5069 (40.1) | |
|
| |||
| Self-pay | 187 (2.6) | 505 (4.0) | |
|
| |||
| Other/unknown | 97 (1.4) | 217 (1.7) | |
|
| |||
| Specialty of admitting physician | |||
|
| |||
| General pediatrician | 5689 (80.1) | 8857 (70.1) | <.001 |
|
| |||
| Subspecialty pediatrician | 331 (4.7) | 1387 (11.0) | |
|
| |||
| Other | 1080 (15.2) | 2392 (18.9) | |
|
| |||
| Admission during respiratory season | 4890 (68.9) | 8306 (65.7) | <.001 |
|
| |||
| Comorbid conditions | |||
|
| |||
| Asthma | 2509 (35.3) | 5382 (42.6) | <.001 |
|
| |||
| Influenza | 395 (5.6) | 584 (4.6) | <.01 |
|
| |||
| Fluid and electrolyte disorders | 2047 (28.8) | 3117 (24.7) | <.001 |
|
| |||
| Hospital characteristics | |||
|
| |||
| Rural (vs urban) | 1909 (26.9) | 1839 (14.6) | <.001 |
|
| |||
| Teaching (vs nonteaching) | 2233 (31.5) | 4730 (37.4) | <.001 |
|
| |||
| No. of beds | |||
|
| |||
| ≤200 | 1756 (24.7) | 2252 (17.8) | <.001 |
|
| |||
| 201-400 | 2748 (38.7) | 4988 (39.5) | |
|
| |||
| >400 | 2596 (36.6) | 5396 (42.7) | |
|
| |||
| Region | |||
|
| |||
| Northeast | 545 (7.7) | 2182 (17.3) | <.001 |
|
| |||
| Midwest | 1321 (18.6) | 2232 (17.7) | |
|
| |||
| West | 1056 (14.9) | 1732 (13.7) | |
|
| |||
| South | 4178 (58.8) | 6490 (51.4) | |
|
| |||
| Children's hospital (vs general community hospital) | 1008 (14.2) | 3644 (28.8) | <.001 |
|
| |||
| Initial investigations | |||
|
| |||
| Complete blood cell count | 5397 (76.0) | 11 195 (88.6) | <.001 |
|
| |||
| Blood culture | 4557 (64.2) | 10 068 (79.7) | <.001 |
|
| |||
| Chest radiography | 4514 (63.6) | 11 685 (92.5) | <.001 |
|
| |||
| Chest computed tomography | 54 (0.8) | 141 (1.1) | .02 |
|
| |||
| Chest ultrasonography | 15 (0.2) | 24 (0.2) | .75 |
|
| |||
| Arterial blood gas analysis | 121 (1.7) | 414 (3.3) | <.001 |
|
| |||
| Acute phase reactants (ESR or CRP) | 1580 (22.3) | 1964 (15.5) | <.001 |
|
| |||
| Urine culture | 842 (11.9) | 1981 (15.7) | <.001 |
|
| |||
| Cerebrospinal fluid culture | 12 (0.2) | 52 (0.4) | <.01 |
|
| |||
| Test for viral pathogens | 2153 (30.3) | 5037 (39.9) | <.001 |
|
| |||
| Initial therapies | |||
|
| |||
| Intravenous or oral steroids | 1999 (28.2) | 4898 (38.8) | <.001 |
|
| |||
| Short-acting β-agonists | 4225 (59.5) | 7851 (62.1) | <.001 |
|
| |||
| Medications for chronic asthma | 1351 (19.0) | 2200 (17.4) | <.01 |
|
| |||
| Initial antibiotics | |||
|
| |||
| Aminopenicillin or cephalosporina alone | 3763 (53.0) | 6022 (47.7) | <.001 |
|
| |||
| Macrolide alone | 524 (7.4) | 815 (6.4) | .01 |
|
| |||
| Aminopenicillin or cephalosporin,a plus macrolide | 1421 (20.0) | 3363 (26.6) | <.001 |
|
| |||
| Aminopenicillin or cephalosporin,a plus vancomycin or clindamycin | 209 (2.9) | 306 (2.4) | .03 |
|
| |||
| Other | 1183 (16.7) | 2130 (16.9) | .73 |
Abbreviations: CRP, C-reactive protein; ED, emergency department; ESR, erythrocyte sedimentation rate; IQR, interquartile range.
Third-generation cephalosporin (ceftriaxone or cefotaxime).
Recognizing the limitations of even highly detailed administrative data to control for unmeasured confounders, we subsequently developed grouped treatment models using the hospital direct admission rate in place of the individual assignment to ED or direct admission, an adaptation of the instrumental variable approach.28 Each patient was assigned a probability of being admitted directly that was equal to the direct admission rate at the hospital where they received their care. We then repeated hierarchical generalized linear models, substituting the hospital rate of direct admission for the actual admission type for each patient, adjusting for individual patient- and hospital-level covariates as already described. This analysis was limited to children cared for at hospitals with more than 11 admissions during the study period, the 25th percentile for number of admissions.
To evaluate variation in direct admission rates across hospitals, we calculated rates of direct admission at this group of hospitals. Adjusted rates were calculated using a hierarchical generalized linear model with hospital random effects, adjusting for covariates as already described. Recognizing that LOS and cost are closely tied to hospital practice, to evaluate variation in outcomes at the hospital level, we calculated the difference in mean LOS and hospital cost between ED and direct admissions within each hospital, using sign tests to assess differences between admission type. This analysis was limited to hospitals that had at least 5 ED admissions and 5 direct admissions during the study period. All analyses were performed using SAS version 9.3 (SAS Institute Inc).
Results
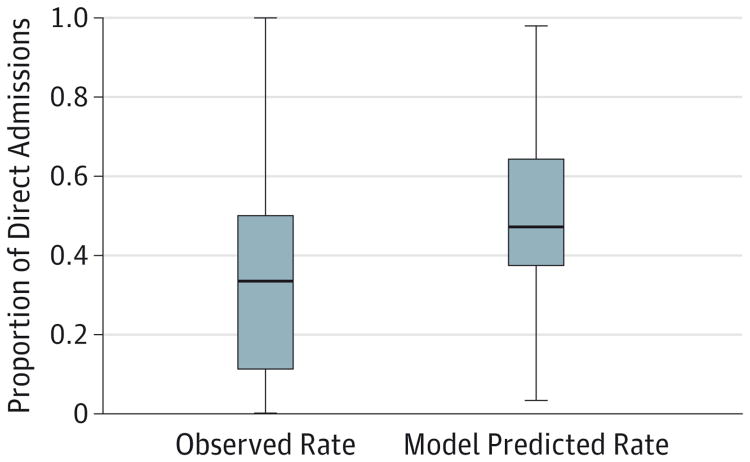
A total of 19 736 children from 278 hospitals met our eligibility criteria, including 7100 (36.0%) admitted directly and 12 636 (64.0%) who were first seen in the ED. Rates of direct admission varied significantly among hospitals (Figure 1), with a median direct admission rate of 33.3% (interquartile range, 11.1%-50.0%).
Figure 1. Adjusted and Unadjusted Rates of Direct Admission for Children With Pneumonia.
Adjusted rates were calculated using a hierarchical generalized linear model, adjusting for patient and hospital characteristics, year of admission, and a random effect for hospital.
There were small but statistically significant differences between the groups with respect to age and the proportion of children admitted during respiratory season, whereas larger differences were observed with respect to race and insurance status (Table 1). Children admitted directly were more likely to be white and to have private health insurance. They were also more likely to receive their initial hospital care from a general pediatrician and less likely to have asthma. Hospital characteristics also differed between the groups, with considerably more children admitted directly at smaller, rural hospitals in the south. Only 14.2% of children who had a direct admission received care at a children's hospital compared with 28.8% of those who were admitted through the ED.
There were significant differences between the groups with respect to initial investigations and management (Table 1). Children admitted directly were less likely to have had initial diagnostic testing and were less likely to have received steroids and short-acting β-agonists. The majority of children in both groups received aminopenicillins or cephalosporins alone or in combination with a macrolide as their initial antibiotic therapy. All of the aforementioned differences in diagnostic testing and initial management persisted in our analysis that was limited to children with hospitalizations of 1-day duration (eTable in the Supplement).
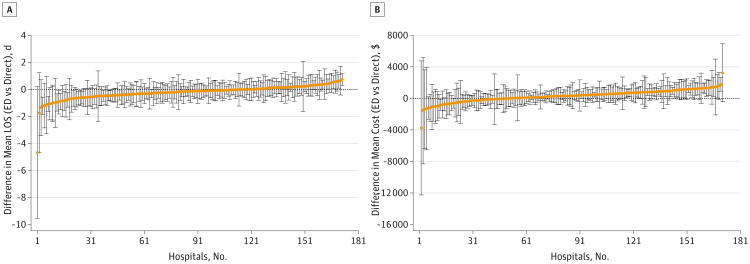
Unadjusted outcomes differed between the groups (Table 2), but there were no significant differences with respect to ICU transfer or readmission. The average LOS was somewhat longer among children admitted directly, although both groups had a median LOS of 2 days. Children admitted directly were considerably less likely to have a hospital stay of less than 2 days, with 18.2% of children admitted directly having high turnover hospitalizations compared with 27.3% of children admitted through the ED. Despite the longer LOSs, total hospital costs were 16% lower, on average, among children admitted directly. Figure 2 illustrates within-hospital mean differences in cost and LOS between ED admissions and direct admissions among 172 hospitals with at least 5 admissions of each type. At 70% of hospitals (n = 120), direct admissions were associated with a longer mean LOS (P < .001), and at 70% of hospitals (n = 120), direct admissions were associated with a lower mean hospital cost relative to admissions through the ED (P < .001).
Table 2. Unadjusted Outcomes Among Children With Pneumonia Admitted Directly to the Hospital and Children Admitted Through the ED.
| Children, No. (%) | |||
|---|---|---|---|
|
|
|||
| Outcome | Direct Admission (n = 7100) | ED Admission (n = 12 636) | P Value |
| Length of stay, d | |||
|
| |||
| Mean (SD) | 2.6 (1.6) | 2.5 (1.7) | <.001a |
|
| |||
| Median (IQR) | 2 (2-3) | 2 (1-3) | |
|
| |||
| High turnover hospitalization (<2 d) | 1291 (18.2) | 3452 (27.3) | <.001b |
|
| |||
| Total hospital cost, $ | |||
|
| |||
| Mean (SD) | 3685 (3487) | 4380 (3896) | <.001a |
|
| |||
| Median (IQR) | 2903 (1965-4354) | 3453 (2357-5166) | |
|
| |||
| Transfer to ICU (≥2 d) | 42 (0.6) | 99 (0.8) | .12b |
|
| |||
| Inpatient mortality | 1 (0.01) | 2 (0.02) | .92b |
|
| |||
| All-cause <30-d readmission | 62 (0.9) | 146 (1.2) | .06b |
Abbreviations: ED, emergency department; ICU, intensive care unit; IQR, interquartile range.
Determined by use of the Wilcoxon rank sum test.
Determined by use of the Pearson χ2 test.
Figure 2. Differences in Mean LOS (A) and Mean Total Hospital Cost (B) Between Children With Pneumonia Admitted From the ED and Those Admitted Directly to the Hospital.
Across 172 hospitals with at least 5 admissions via each admission source during the study period (July 1, 2007–June 30, 2010). Hospitals are ordered by rank. The error bars reflect the 95% CIs of the within-hospital differences in length of stay (LOS) and cost. ED indicates emergency department.
Adjusting for clustering within hospitals and controlling for patient and hospital characteristics, we found that there were no significant differences between the groups with respect to ICU transfer or readmission (Table 3). However, LOS was 9% longer among children admitted directly, while the total hospital cost was 12% less. In adjusted models, children admitted directly had 39% decreased odds of high turnover hospitalization relative to those first seen in the ED. Point estimates and P values were consistent in our grouped treatment sensitivity analyses. In addition, point estimates and 95% CIs were essentially unchanged using the presence or absence of ED billing codes as a surrogate for point of origin codes (data not shown). In our sub-analysis that was limited to children with high turnover hospitalizations, adjusted costs were 28% less for children admitted directly than for children admitted through the ED (cost ratio, 0.72 [95% CI, 0.71-0.74]), and there was no significant difference in rates of readmission (OR, 0.58 [95% CI, 0.27-1.28]).
Table 3. Adjusted Outcomes Among Children With Pneumonia Admitted Directly to the Hospital and Children Admitted Through the Emergency Department.
| Outcome | Risk Ratio (95% CI) | P Value |
|---|---|---|
| Length of staya | ||
| Adjusted for covariates and propensity scoreb | 1.09 (1.07-1.11) | <.001 |
| Grouped treatment plus covariate adjustmentb,c | 1.16 (1.05-1.26) | <.01 |
| Total hospital costa | ||
| Adjusted for covariates and propensity scoreb | 0.88 (0.87-0.90) | <.001 |
| Odds Ratio (95% CI) | ||
| High turnover hospitalization (<2 d) | ||
| Adjusted for covariates and propensity scoreb | 0.61 (0.56-0.66) | <.001 |
| Grouped treatment plus covariate adjustmentb,c | 0.42 (0.27-0.66) | <.001 |
| Transfer to intensive care unit | ||
| Adjusted for covariates and propensity scoreb | 1.29 (0.83-2.00) | .25 |
| Grouped treatment plus covariate adjustmentb,c | 0.38 (0.06-2.57) | .32 |
| Readmission (<30 d) | ||
| Adjusted for covariates and propensity scoreb | 0.80 (0.57-1.13) | .20 |
| Grouped treatment plus covariate adjustmentb,c | 0.77 (0.41-1.46) | .42 |
Log-transformed and trimmed at 3 SDs above the mean.
Hierarchical generalized linear modeling with hospital random effect, adjusted for clustering within hospitals, as well as propensity for direct admission, age, sex, race/ethnicity, payor, year of admission, admitting physician, admission during respiratory season, asthma, influenza, disorders of fluids and electrolytes, severity markers, geographic region, hospital bed size, rurality, hospital teaching status, and children's hospital status.
Limited to patients in hospitals admitting more than 11 patients (equivalent to 25th percentile in data set).
Discussion
To our knowledge, this large, multihospital study is the first to compare children admitted directly to the hospital with children initially cared for in the ED with regard to disease management, outcomes, and resource utilization. We observed considerable variation in rates of direct admission across hospitals, with smaller, rural, general community hospitals being more likely to admit patients directly. Adjusting for patient and hospital characteristics and clustering within hospitals, we found that the rates of ICU transfer and readmission did not differ significantly between children admitted directly to the hospital and those admitted through the ED. However, children admitted directly were considerably less likely to have high turnover hospitalizations (defined as hospital stays of less than 2 days in duration)25,26 and had modestly longer LOSs. In contrast, direct admission was associated with substantially lower total hospital costs, reflecting decreased resource utilization in this group. Children admitted directly were less likely to receive almost all diagnostic tests, both in our full cohort and when we repeated our analysis that was limited to children with high turnover hospitalizations.
A review of the literature reveals very few past studies characterizing outcomes, risks, or benefits of direct admission, despite the substantial proportion of patients admitted to the hospital directly.29 One study among adults admitted with sepsis found that direct admission was associated with increased mortality, which the authors speculated to be related to provision of less efficient care.8 Similarly, a study5 examining outcomes of unscheduled adult hospitalizations found that patients admitted directly had a higher mortality rate for time-sensitive conditions such as acute myocardial infarction and sepsis than those admitted from the ED, a difference not observed among adults admitted with pneumonia or asthma. Several disease-, patient-, and health system–level factors may limit the applicability of these adult studies to pediatrics; unlike the aforementioned adult studies, we did not find increased rates of adverse outcomes among children admitted directly.
Direct admissions involve the referral of patients by out-patient health care providers directly to hospital-based providers, requiring patients to have access to outpatient health care providers, as well as communication between these providers and hospital-based physicians to initiate direct admission processes. In contrast, communication between outpatient providers and ED physicians is not essential to ED referral and occurs with variable frequency.30 The communication inherent in direct admission processes may affect decision making about whether or not a patient requires admission and may have contributed to the decreased odds of high turnover hospitalization that we observed among children admitted directly. This communication may also reduce the need for in-patient diagnostic testing, particularly if testing has been initiated prior to admission. We observed that smaller, rural, general community hospitals were more likely to admit patients directly. Hospital-based providers in these hospitals may be more likely to have established relationships with primary care providers (or primary care providers may continue to manage their own patients), thereby facilitating communication and transitions of care.31
Our findings have important policy implications. Our results suggest that increasing rates of direct admission may, in some cases, be a safe strategy to reduce hospital costs and ED overcrowding, with the caveat that direct admission requires access to an outpatient provider. We observed that directly admitted children were significantly more likely to have private health insurance than those admitted through the ED. Publically insured and uninsured children are considerably less likely to have a medical home,32 the absence of which is a major barrier to direct admission.
Our results should be interpreted in light of several limitations. First, we used ICD-9-CM codes to identify patients with pneumonia, which may have resulted in potential misclassification. We attempted to minimize misclassification by using a previously validated ICD-9-CM algorithm18 and by limiting our analysis to children who received antibiotics on the first day of hospitalization. Second, because our analysis used administrative data, we had limited ability to assess pneumonia severity or social factors that may have influenced decisions regarding admission source, and there may be additional un-measured confounders that influenced our observed outcomes. In particular, we recognize that the decision to admit through the ED is likely to be influenced by severity of illness. However, grouped treatment modeling is a rigorous method intended to account for potential confounding by indication due to unmeasured factors, and our point estimates using this approach aligned well with our primary multivariable analyses. Third, the LOS measure in the PDW is limited to total hosdays, making this measure insensitive to smaller differences between the groups. Related to this, as in other administrative data sources, ED LOS is not included in the PDW LOS measure. Fourth, tests and treatments performed in the out-patient setting are not available in the PDW, so we are unable to determine if children admitted directly were more likely to have diagnostic testing or treatments initiated prior to admission. If children admitted directly received more diagnostic testing in the outpatient setting prior to admission, the differences in initial pneumonia management observed (Table 1) may not reflect all resource utilization. Future studies using data sets that include both inpatient and outpatient health care costs are needed to better understand the potential savings associated with direct admissions. Finally, because our study examined pneumonia only, future studies are needed to characterize management and outcomes of other conditions among children.
Conclusions
Although direct admission was associated with decreased costs overall, it is notable that these findings did not apply to all hospitals within our sample. At approximately one-third of hospitals, direct admissions were associated with higher mean hospital costs. Given the considerable variability in rates and outcomes of direct admission demonstrated in our study, there are undoubtedly cultural, system, and population factors that influence the ability of direct admissions to reduce testing, high turnover hospitalizations, and costs. Future studies characterizing these factors and the direct admission policies and practices that influence outcomes will help to define best practices. Further studies are also needed to define the conditions in which children are most likely to benefit from direct admission and to implement systems to enable direct admissions when safe and cost-effective.
Supplementary Material
Acknowledgments
Funding/Support: Dr Leyenaar was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health (grant UL1 RR025752). Dr Lagu was supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health (Award K01HL114745).
Role of the Sponsor: The funder had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Author Contributions: Dr Pekow had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Leyenaar, Lagu, Pekow, Lindenauer.
Acquisition, analysis, or interpretation of data: Leyenaar, Shieh, Lagu, Pekow, Lindenauer.
Drafting of the manuscript: Leyenaar.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Shieh, Pekow.
Obtained funding: Leyenaar, Lindenauer.
Administrative, technical, or material support: Lagu.
Study supervision: Lagu, Pekow, Lindenauer.
Conflict of Interest Disclosures: None reported.
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Previous Presentation: This study was presented at the Plenary Session, the Best of Research, Innovations and Vignettes, at the Society of Hospital Medicine's Annual Meeting; March 25, 2014; Las Vegas, Nevada.
Contributor Information
JoAnna K. Leyenaar, Division of Pediatric Hospital Medicine, Department of Pediatrics, Tufts University School of Medicine, Boston, Massachusetts.
Meng-Shiou Shieh, Center for Quality of Care Research, Baystate Medical Center, Springfield, Massachusetts.
Tara Lagu, Center for Quality of Care Research, Baystate Medical Center, Springfield, Massachusetts; Department of Medicine, Tufts University School of Medicine, Boston, Massachusetts; Division of General Medicine, Baystate Medical Center, Springfield, Massachusetts.
Penelope S. Pekow, Center for Quality of Care Research, Baystate Medical Center, Springfield, Massachusetts; School of Public Health and Health Sciences, University of Massachusetts, Amherst.
Peter K. Lindenauer, Center for Quality of Care Research, Baystate Medical Center, Springfield, Massachusetts; Department of Medicine, Tufts University School of Medicine, Boston, Massachusetts; Division of General Medicine, Baystate Medical Center, Springfield, Massachusetts.
References
- 1.Committee on the Future of Emergency Care in the United States Health System; Board on Health Care Services; Institute of Medicine. Hospital-Based Emergency Care: At the Breaking Point. Washington, DC: National Academies Press; 2006. [Google Scholar]
- 2.Merrill C, Owens PL. Reasons for being admitted to the hospital through the emergency department for children and adolescents, 2004. [Accessed February 10, 2014];Healthcare Cost and Utilization Project (HCUP) Statistical Brief 33. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb33.pdf. Published June 2007.
- 3.Merrill C, Owens PL. Hospital admissions that began in the emergency department for children and adolescents, 2004. [Accessed February 10, 2014];Healthcare Costs and Utilization Project (HCUP) Statistical Brief 32. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb32.jsp. Published June 2007. [PubMed]
- 4.Tang N, Stein J, Hsia RY, Maselli JH, Gonzales R. Trends and characteristics of US emergency department visits, 1997-2007. JAMA. 2010;304(6):664–670. doi: 10.1001/jama.2010.1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kocher KE, Dimick JB, Nallamothu BK. Changes in the source of unscheduled hospitalizations in the United States. Med Care. 2013;51(8):689–698. doi: 10.1097/MLR.0b013e3182992c7b. [DOI] [PubMed] [Google Scholar]
- 6.Schuur JD, Venkatesh AK. The growing role of emergency departments in hospital admissions. N Engl J Med. 2012;367(5):391–393. doi: 10.1056/NEJMp1204431. [DOI] [PubMed] [Google Scholar]
- 7.Bjertnaes OA. The association between survey timing and patient-reported experiences with hospitals: results of a national postal survey. BMC Med Res Methodol. 2012;12(1):13. doi: 10.1186/1471-2288-12-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Powell ES, Khare RK, Courtney DM, Feinglass J. Lower mortality in sepsis patients admitted through the ED vs direct admission. Am J Emerg Med. 2012;30(3):432–439. doi: 10.1016/j.ajem.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 9.Elixhauser A. Hospital stays for children, 2006. [Accessed February 1, 2012];Healthcare Costs and Utilization Project (HCUP) Statistical Brief 56. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb56.jsp. Published July 2008.
- 10.Lu S, Kuo DZ. Hospital charges of potentially preventable pediatric hospitalizations. Acad Pediatr. 2012;12(5):436–444. doi: 10.1016/j.acap.2012.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kronman MP, Hersh AL, Feng R, Huang YS, Lee GE, Shah SS. Ambulatory visit rates and antibiotic prescribing for children with pneumonia, 1994-2007. Pediatrics. 2011;127(3):411–418. doi: 10.1542/peds.2010-2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lindenauer PK, Pekow P, Wang K, Mamidi DK, Gutierrez B, Benjamin EM. Perioperative beta-blocker therapy and mortality after major noncardiac surgery. N Engl J Med. 2005;353(4):349–361. doi: 10.1056/NEJMoa041895. [DOI] [PubMed] [Google Scholar]
- 13.Rothberg MB, Pekow PS, Lahti M, Brody O, Skiest DJ, Lindenauer PK. Antibiotic therapy and treatment failure in patients hospitalized for acute exacerbations of chronic obstructive pulmonary disease. JAMA. 2010;303(20):2035–2042. doi: 10.1001/jama.2010.672. [DOI] [PubMed] [Google Scholar]
- 14.Lindenauer PK, Pekow P, Wang K, Gutierrez B, Benjamin EM. Lipid-lowering therapy and in-hospital mortality following major noncardiac surgery. JAMA. 2004;291(17):2092–2099. doi: 10.1001/jama.291.17.2092. [DOI] [PubMed] [Google Scholar]
- 15.Feudtner C, Dai D, Hexem KR, Luan X, Metjian TA. Prevalence of polypharmacy exposure among hospitalized children in the United States. Arch Pediatr Adolesc Med. 2012;166(1):9–16. doi: 10.1001/archpediatrics.2011.161. [DOI] [PubMed] [Google Scholar]
- 16.McLeod L, French B, Dai D, Localio R, Keren R. Patient volume and quality of care for young children hospitalized with acute gastroenteritis. Arch Pediatr Adolesc Med. 2011;165(9):857–863. doi: 10.1001/archpediatrics.2011.132. [DOI] [PubMed] [Google Scholar]
- 17.Lasky T, Greenspan J, Ernst FR, Gonzalez L. Pediatric vancomycin use in 421 hospitals in the United States, 2008. PLoS One. 2012;7(8):e43258. doi: 10.1371/journal.pone.0043258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Williams DJ, Shah SS, Myers A, et al. Identifying pediatric community-acquired pneumonia hospitalizations: accuracy of administrative billing codes. JAMA Pediatr. 2013;167(9):851–858. doi: 10.1001/jamapediatrics.2013.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brogan TV, Hall M, Williams DJ, et al. Variability in processes of care and outcomes among children hospitalized with community-acquired pneumonia. Pediatr Infect Dis J. 2012;31(10):1036–1041. doi: 10.1097/INF.0b013e31825f2b10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Weiss AK, Hall M, Lee GE, Kronman MP, Sheffler-Collins S, Shah SS. Adjunct corticosteroids in children hospitalized with community-acquired pneumonia. Pediatrics. 2011;127(2):e255–e263. doi: 10.1542/peds.2010-0983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ambroggio L, Taylor JA, Tabb LP, Newschaffer CJ, Evans AA, Shah SS. Comparative effectiveness of empiric β-lactam monotherapy and β-lactam-macrolide combination therapy in children hospitalized with community-acquired pneumonia. J Pediatr. 2012;161(6):1097–1103. doi: 10.1016/j.jpeds.2012.06.067. [DOI] [PubMed] [Google Scholar]
- 22.Feudtner C, Hays RM, Haynes G, Geyer JR, Neff JM, Koepsell TD. Deaths attributed to pediatric complex chronic conditions: national trends and implications for supportive care services. Pediatrics. 2001;107(6):99. doi: 10.1542/peds.107.6.e99. [DOI] [PubMed] [Google Scholar]
- 23.Feudtner C, Christakis DA, Connell FA. Pediatric deaths attributable to complex chronic conditions: a population-based study of Washington State, 1980-1997. Pediatrics. 2000;106(1, pt 2):205–209. [PubMed] [Google Scholar]
- 24.Prabaker KK, Hayden MK, Weinstein RA, Lin MY CDC Prevention Epicenter Program. Use of the point of origin code from a universal billing form, UB-04, to efficiently identify hospitalized patients admitted from other health care facilities. Am J Infect Control. 2012;40(7):659–662. doi: 10.1016/j.ajic.2011.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Macy ML, Stanley RM, Sasson C, Gebremariam A, Davis MM. High turnover stays for pediatric asthma in the United States: analysis of the 2006 Kids' Inpatient Database. Med Care. 2010;48(9):827–833. doi: 10.1097/MLR.0b013e3181f2595e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Macy ML, Stanley RM, Lozon MM, Sasson C, Gebremariam A, Davis MM. Trends in high-turnover stays among children hospitalized in the United States, 1993-2003. Pediatrics. 2009;123(3):996–1002. doi: 10.1542/peds.2008-1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gelman A, Hill J. Data Analysis Using Regression and Multilevel/Hierarchical Models. New York, NY: Cambridge University Press; 2007. [Google Scholar]
- 28.Johnston SC, Henneman T, McCulloch CE, van der Laan M. Modeling treatment effects on binary outcomes with grouped-treatment variables and individual covariates. Am J Epidemiol. 2002;156(8):753–760. doi: 10.1093/aje/kwf095. [DOI] [PubMed] [Google Scholar]
- 29.Owens PM, Thompson J, Elixhauser A, Ryan K. Healthcare Cost and Utilization Project (HCUP) Care of Children and Adolescents in US Hospitals: HCUP Fact Book No.4. [Accessed February 10, 2014];Agency for Healthcare Research and Quality website. http://archive.ahrq.gov/data/hcup/factbk4/
- 30.Carrier E, Yee T, Holzwart RA. Coordination between emergency and primary care physicians. [Accessed January 27, 2014];NIHCR Research Brief No 3. http://www.nihcr.org/ED-Coordination.html. Published February 2011.
- 31.Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831–841. doi: 10.1001/jama.297.8.831. [DOI] [PubMed] [Google Scholar]
- 32.Mannix R, Chiang V, Stack AM. Insurance status and the care of children in the emergency department. J Pediatr. 2012;161(3):536–541.e3. doi: 10.1016/j.jpeds.2012.03.013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.