Abstract
Importance
Among women and men with severe obesity, evidence for improvement in urinary incontinence beyond the first year after bariatric surgery–induced weight loss is lacking.
Objectives
To examine change in urinary incontinence before and after bariatric surgery and to identify factors associated with improvement and remission among women and men in the first 3 years after bariatric surgery.
Design, Setting, and Participants
The Longitudinal Assessment of Bariatric Surgery 2 is an observational cohort study at 10 US hospitals in 6 geographically diverse clinical centers. Participants were recruited between February 21, 2005, and February 17, 2009. Adults undergoing first-time bariatric surgical procedures as part of clinical care by participating surgeons between March 14, 2006, and April 24, 2009, were followed up for 3 years (through October 24, 2012).
Intervention
Participants undergoing bariatric surgery completed research assessments before the procedure and annually thereafter.
Main outcomes and measures
The frequency and type of urinary incontinence episodes in the past 3 months were assessed using a validated questionnaire. Prevalent urinary incontinence was defined as at least weekly urinary incontinence episodes, and remission was defined as change from prevalent urinary incontinence at baseline to less than weekly urinary incontinence episodes at follow-up.
Results
Of 2458 participants, 1987 (80.8%) completed baseline and follow-up assessments. At baseline, the median age was 47 years (age range, 18-78 years), the median body mass index was 46 kg/m2 (range, 34-94 kg/m2), and 1565 of 1987 (78.8%) were women. Urinary incontinence was more prevalent among women (49.3%; 95% CI, 46.9%-51.9%) than men (21.8%; 95% CI, 18.2%-26.1%) (P < .001). After a mean 1-year weight loss of 29.5% (95% CI, 29.0%-30.1%) in women and 27.0% (95% CI, 25.9%-28.6%) in men, year 1 urinary incontinence prevalence was significantly lower among women (18.3%; 95% CI, 16.4%-20.4%) and men (9.8%; 95% CI, 7.2%-13.4%) (P < .001 for all). The 3-year prevalence was higher than the 1-year prevalence for both sexes (24.8%; 95% CI, 21.8%-26.5% among women and 12.2%; 95% CI, 9.0%-16.4% among men) but was substantially lower than baseline (P < .001 for all). Weight loss was independently related to urinary incontinence remission (relative risk, 1.08; 95% CI, 1.06-1.10 in women and 1.07; 95% CI, 1.02-1.13 in men) per 5% weight loss, as were younger age and the absence of a severe walking limitation.
Conclusions and Relevance
Among women and men with severe obesity, bariatric surgery was associated with substantially reduced urinary incontinence over 3 years. Improvement in urinary incontinence may be an important benefit of bariatric surgery.
Urinary incontinence (here after incontinence) affects approximately 30 million US adults1-3; can cause substantial distress, diminished quality of life, and limitations in daily functioning4,5; and may account for more than $60 billion in annual direct costs in the United States.6,7 Epidemiological studies8-10 have shown that obesity is an independent risk factor for prevalent and incident incontinence. Each 5-unit increase in body mass index above normal weight is associated with a 40% to 70% increased odds of prevalent incontinence and a 30% to 60% increased risk of incident incontinence over 5 to 10 years.11 The prevalence of incontinence has been reported to be as high as 60% to 70% among severely obese women12-15 and 24% among severely obese men.16
Because obesity is a potentially modifiable risk factor for incontinence, weight reduction has been investigated as a treatment option. Clinical trials of a low-calorie diet (resulting in 10%-15% weight loss) and behavioral weight reduction (resulting in 7%-9% weight loss) have reported reductions in the prevalence or severity of incontinence among obese women and men.17-20 Among severely obese populations, substantial improvement in incontinence has been reported during the first year after bariatric surgery,12-14,16,21-24 but evidence on the durability of this effect is lacking. In addition, previous studies have included minimal data on the type or frequency of incontinence, had small samples from single centers, were often limited to women, and did not report factors associated with incontinence improvement.
This study investigated incontinence outcomes in a large multisite observational cohort study designed to assess the risks and benefits of bariatric surgery. The objectives of this research were to characterize postoperative changes in the frequency and prevalence of incontinence by type, to examine postoperative remission and incidence of incontinence, and to identify factors associated with improvement and remission among women and men in the first 3 years after bariatric surgery.
Methods
Participants and Setting
Information on the protocol for this observational study is available at the clinical trials registration website (eAppendix in the Supplement). The Longitudinal Assessment of Bariatric Surgery 2 includes data collected from 10 hospitals at 6 clinical centers in the United States. Between February 21, 2005, and February 17, 2009, patients 18 years or older seeking a first-time bariatric surgical procedure with a participating surgeon were recruited.25 The Longitudinal Assessment of Bariatric Surgery 2 included 2458 participants undergoing a bariatric procedure between March 14, 2006, and April 24, 2009. To be included in this study, participants had to have completed the Urinary Incontinence Questionnaire (UIQ) at baseline and 1 or more follow-up assessments within the first 3 postoperative years (3-year follow-up spanned September 14, 2008, to October 24, 2012) (Figure 1). All centers obtained institutional review board approval, and individuals provided written informed consent to participate.
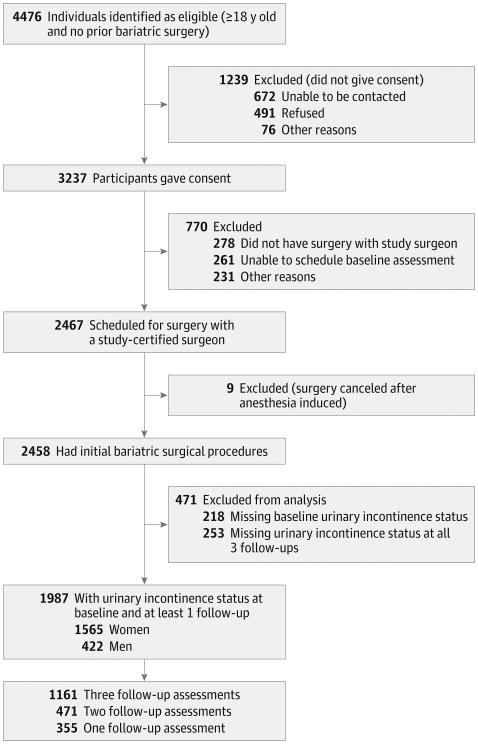
Figure 1. Study Participant Flow Diagram.
Assessments and Outcomes
A research assessment was performed within 30 days before surgery and annually after surgery by Longitudinal Assessment of Bariatric Surgery 2–trained and certified personnel.25 Assessments included a validated participant-reported UIQ.26 Participants were asked the following question: “In the past 3 months, how often have you typically leaked urine, even a small amount?” Responses included never, less than once per month, monthly (once or more each month), weekly (once or more each week), or daily (once or more each day). Those answering weekly or more frequently reported the number of times per week that urine loss occurred “with a physical activity like coughing, sneezing, lifting, or exercise” (stress incontinence episode), “an urge or the feeling that you needed to empty your bladder but you could not get to the toilet fast enough” (urgency incontinence episode), or for other reasons (other incontinence episode). The survey also assessed treatment for urinary incontinence over the past 3 months. The complete incontinence survey is available online (http://www.edc.gsph.pitt.edu/labs/public/labs-1descriptionpaper/Self_Assessment_Forms/UrinaryIncontinenceBaseline.pdf).
Because at least weekly incontinence is associated with reduced quality of life and increased treatment seeking,27,28 participants with at least weekly incontinence of any type were considered to have prevalent incontinence. Participants were defined as having prevalent stress-type or urgency-type incontinence if they reported stress-type or urgency-type incontinence, respectively, at least weekly. Prevalent incontinence was categorized as stress only, urge only, or both. Participants with prevalent incontinence at baseline had remission if they reported less than weekly incontinence at follow-up, or had complete remission if they reported no incontinence at follow-up. Incident incontinence was defined as less than weekly incontinence at baseline but prevalent incontinence at follow-up. Change from a more frequent to a less frequent category was considered improved frequency of incontinence.
Surgeons recorded the type of bariatric surgical procedure.25,29 Procedures other than Roux-en-Y gastric bypass and laparoscopic adjustable gastric band were grouped as other type.
Additional data were collected at baseline and annual follow-up assessments using physical examination, laboratory testing, and questionnaires.29 Standardized protocols were used to measure height at baseline and weight at each assessment. Body mass index was calculated as weight in kilograms divided by height in meters squared. Weight change over 3 years was calculated as the percentage change from baseline, whereas weight change between assessments was assessed in kilograms.
Sociodemographic characteristics were assessed by self-report. There were few self-reports of race other than white or black, so Asian, American Indian, Alaskan native, and native Hawaiian or other Pacific Islander were categorized as other race. White and other races were combined when testing the association between race and incontinence because baseline incontinence prevalence among those with other race was more similar to that of white participants than black participants. Women self-reported the number of prior live births and stillbirths, pregnancies in the past year, hormone therapy use, prior hysterectomy, and both women and men self-reported smoking status.30 Diabetes mellitus, hypertension, asthma, history of heart disease (ischemic heart disease or congestive heart failure), and stroke were identified with a combination of laboratory values (eg, glycated hemoglobin), physical examination measures (eg, blood pressure), participant report of medication use and comorbidity diagnoses from health care professionals, and medical records review using standard definitions.25 Severe walking limitation was defined as self-reported inability to walk 200 ft (61 m) without assistance, and the presence of depressive symptoms was defined as a score of at least 10 on version 1 of the Beck Depression Inventory.
Statistical Analysis
Descriptive statistics used to summarize baseline characteristics included frequencies and percentages for categorical data and medians and 25th and 75th percentiles for continuous data. Pearson χ2 tests were used to examine differences in percentages of incontinence between women and men. Other analyses were stratified by sex.
Data were assumed to be missing at random. Sensitivity analyses were performed to investigate the robustness of the results with respect to this assumption. The t test from a linear mixed model was used to determine whether weight change varied over time. Mixed-effects ordinal logistic regression models were utilized to assess the odds of change in incontinence frequency over time. Poisson mixed models with robust error variance were used to estimate and test changes over time in incontinence prevalence among the full sample, as well as remission and incidence among those with and without incontinence at baseline.
Pairwise comparisons were made between baseline and each follow-up assessment for the frequency and prevalence models. For all models, pairwise comparisons were made between years 1 and 2 and between years 2 and 3. P values and 95% CIs were adjusted for multiple comparisons.31 Based on the results of these analyses, Poisson models with robust error variance were used to evaluate whether weight from years 1 to 2 was associated with incontinence at year 2 among women with incontinence remission at year 1. Modeled percentages or means and 95% CIs are reported.
Among those with preoperative incontinence, mixed-effects ordinal logistic regression models and Poisson mixed models were used to identify factors independently related to change in the frequency and change in incontinence remission, respectively. Change in the frequency was quantified by the degree of change among 5 categories. All models controlled for baseline incontinence episodes frequency. Variables forced into models based on prior work relating them to incontinence3,8,34,35 were age, race, current smoking status, pregnancy in the past year, and percentage weight change. Additional baseline and follow-up variables were entered and retained in final models if they reached statistical significance (P < .05) through backward elimination. Interactions with time were retained in final models if they reached statistical significance. The ratio of the generalized χ2 statistic and its df are reported to indicate the goodness of fit of each model. Adjusted odds ratios (ORs) for improvement in the frequency and relative risks for remission of incontinence and 95% CIs are reported.
Analyses were conducted using statistical software (SAS, versions 9.3 and 9.4; SAS Institute Inc). Reported P values are 2-sided, and P < .05 was considered statistically significant.
Assessment Missing at Random Assumption
The UIQ was completed for 74.9% (7362 of 9832) of the potential assessments across time. More than 64.8% (1600 of 2470) of the missing UIQs were because no self-assessment forms were completed for an assessment. Another 29.2% (722 of 2471) were because participants stopped completing the self-assessment packet before reaching the UIQ. These missing data could not be attributed to incontinence status. However, for those missing incontinence status at 2 or 3 years, the prevalence of incontinence at other time points was greater and remained significant after controlling for factors (ie, site, age, and smoking status) that were independently related to the completeness of incontinence follow-up data (eTable 1 in the Supplement). Therefore, a sensitivity analysis was performed using imputed data.
When missing incontinence status was followed by known incontinence status, the missing status was imputed from a logistic regression model containing variables related to the completeness of follow-up data or to the prevalence of incontinence.32 To impute missing incontinence status that was not followed by known incontinence status, a pattern mixture model that did not assume missing at random was used.33 Finally, multiple imputation was used to combine the results from 30 imputed data sets. The modeled values from the sensitivity analysis are reported in eTable 2 and eTable 3 in the Supplement.
Results
This report includes 1987 of 2458 study participants (80.8%) (Figure 1). Participants were excluded from this analysis due to missing incontinence status at baseline (n = 218) or failure to complete all follow-up visits (n = 253). Among 1987 participants in the study, 1161 (58.4%) had 3 follow-up assessments, 471 (23.7%) had 2 follow-up assessments, and 355 (17.9%) had 1 follow-up assessment. At baseline, the median age was 47 years (age range, 18-78 years), the median body mass index was 46 (range, 34-94), and 78.8% (1565 of 1987) of participants were women (Table 1). Prevalent incontinence was reported by 49.3% (95% CI, 46.9%-51.9%) of women and by 21.8%(95%CI, 18.2%-26.1%) of men, with another 436 (27.9%) women and 106 (25.1%) men reporting some (but less than weekly) incontinence episodes (Table 2). Compared with men, women had more frequent incontinence episodes and were more likely to have any-type, stress-type, and urgency-type prevalent incontinence (P < .001 for all).
Table 1. Baseline Demographic and Clinical Characteristics of Adults Undergoing Bariatric Surgery, by Sexa.
| Variable | Women (n = 1565)b | Men (n = 422)b |
|---|---|---|
| Age, y | ||
| Median (IQR) | 46 (37-54) | 50 (40-58) |
| Range | 18-78 | 19-76 |
| Race, No. (%) | (n = 1554) | (n = 418) |
| White | 1330 (85.6) | 390 (93.3) |
| Black | 168 (10.8) | 21 (5.0) |
| Otherc | 56 (3.6) | 7 (1.7) |
| Hispanic or Latino ethnicity | 78 (5.0) | 14 (3.3) |
| College degree or higher | 573/1558 (36.8) | 169/420 (40.2) |
| Current or recent smoker | 200/1563 (12.8) | 37/421 (8.8) |
| BMI | ||
| Median (IQR) | 45.5 (41.6-50.9) | 47.1 (42.6-52.8) |
| Range | 33.8-87.3 | 33.7-94.3 |
| Severe walking limitation | 102/1453 (7.0) | 27/397 (6.8) |
| Diabetes mellitus | 442/1506 (29.3) | 185/403 (45.9) |
| History of stroke | 15/1563 (1.0) | 3 (0.7) |
| History of heart disease | 79/1554 (5.1) | 78 (18.5) |
| Hypertension | 981/1525 (64.3) | 333/415 (80.2) |
| Asthma | 428/1553 (27.6) | 75/419 (17.9) |
| Depressive symptomsd | 485/1526 (31.8) | 109/410 (26.6) |
| History of live birth or stillbirth | 1068/1450 (73.7) | NA |
| Pregnancy in past year | 7 (0.4) | NA |
| Hormone therapy use | 104/1543 (6.7) | NA |
| History of hysterectomy | 382/1522 (25.1) | NA |
| History of surgery for urinary incontinence | 101/1549 (6.5) | 4/419 (1.0) |
| Bariatric surgical procedure | ||
| Roux-en-Y gastric bypass | 1111 (71.0) | 280 (66.4) |
| Laparoscopic adjustable gastric band | 387 (24.7) | 115 (27.3) |
| Sleeve gastrectomy | 33 (2.1) | 16 (3.8) |
| Biliopancreatic diversion with duodenal switch | 12 (0.8) | 3 (0.7) |
| Banded gastric bypass | 22 (1.4) | 8 (1.9) |
| Among those with prevalence of urinary incontinence at least weekly, No. | 772 | 92 |
| Urinary incontinence type, No. (%) | (n = 744) | (n = 90) |
| Stress type only | 223 (30.0) | 4 (4.4) |
| Urgency type only | 82 (11.0) | 53 (58.9) |
| Both stress type and urgency type | 423 (56.9) | 14 (15.6) |
| Other | 16 (2.2) | 19 (21.1) |
| Treatment for urinary incontinence | 122/751 (16.2) | 9/89 (10.1) |
| Medication | 60/744 (8.1) | 8/89 (9.0) |
| Other | 81/744 (10.9) | 2/89 (2.2) |
Abbreviations: IQR, interquartile range; NA, not applicable.
Some totals differ from heading totals because of missing data.
Data presented as No. (%) unless otherwise noted.
Other race includes Asian, American Indian, Alaskan native, or native Hawaiian or other Pacific Islander.
Depressive symptoms defined as a Beck Depression Inventory score of at least 10.
Table 2. Observed Frequency of Urinary Incontinence Episodes and Prevalence of Any-Type, Stress-Type, and Urgency-Type Urinary Incontinence Before and After Bariatric Surgery.
| Variable | No/Total No. (%) | |||
|---|---|---|---|---|
| Baseline | Year 1 | Year 2 | Year 3 | |
| Women (n = 1565) | ||||
| Frequency of urinary incontinence episodes | (n = 1565) | (n = 1373) | (n = 1241) | (n = 1188) |
| Never | 357 (22.8) | 680 (49.5) | 576 (46.4) | 528 (44.4) |
| <Monthly | 247 (15.8) | 304 (22.1) | 257 (20.7) | 235 (19.8) |
| Monthly | 189 (12.1) | 139 (10.1) | 119 (9.6) | 135 (11.4) |
| Weekly | 352 (22.5) | 135 (9.8) | 160 (12.9) | 157 (13.2) |
| Daily | 420 (26.8) | 115 (8.4) | 129 (10.4) | 133 (11.2) |
| Prevalence of urinary incontinence at least weekly | ||||
| Any type | 772/1565 (49.3) | 250/1373 (18.2) | 289/1241 (23.3) | 290/1188 (24.4) |
| Stress type | 646/1530 (42.2) | 188/1357 (13.9) | 211/1226 (17.2) | 220/1169 (18.8) |
| Urgency type | 505/1528 (33.0) | 165/1359 (12.1) | 204/1229 (16.6) | 202/1174 (17.2) |
| Men (n = 422) | ||||
| Frequency of urinary incontinence episodes | (n = 422) | (n = 365) | (n = 317) | (n = 296) |
| Never | 224 (53.1) | 261 (71.5) | 223 (70.3) | 197 (66.6) |
| <Monthly | 73 (17.3) | 51 (14.0) | 38 (12.0) | 39 (13.2) |
| Monthly | 33 (7.8) | 15 (4.1) | 23 (7.3) | 22 (7.4) |
| Weekly | 46 (10.9) | 22 (6.0) | 19 (6.0) | 23 (7.8) |
| Daily | 46 (10.9) | 16 (4.4) | 14 (4.4) | 15 (5.1) |
| Prevalence of urinary incontinence at least weekly | ||||
| Any type | 92/422 (21.8) | 38/365 (10.4) | 33/317 (10.4) | 38/296 (12.8) |
| Stress type | 18/418 (4.3) | 10/360 (2.8) | 9/313 (2.9) | 6/294 (2.0) |
| Urgency type | 67/420 (16.0) | 23/362 (6.4) | 21/314 (6.7) | 24/293 (8.2) |
Among women, the mean weight loss after bariatric surgery was 29.5% (95% CI, 29.0%-30.1%), 30.4% (95% CI, 29.7%-31.0%), and 28.5% (95% CI, 27.9%-29.2%) at 1, 2, and 3 years, respectively. Among men, the mean weight loss after bariatric surgery was 27.0% (95% CI, 25.9%-28.1%), 26.8% (95% CI, 25.6%-28.0%), and 25.5% (95% CI, 24.4%-26.7%) at 1, 2, and 3 years, respectively.
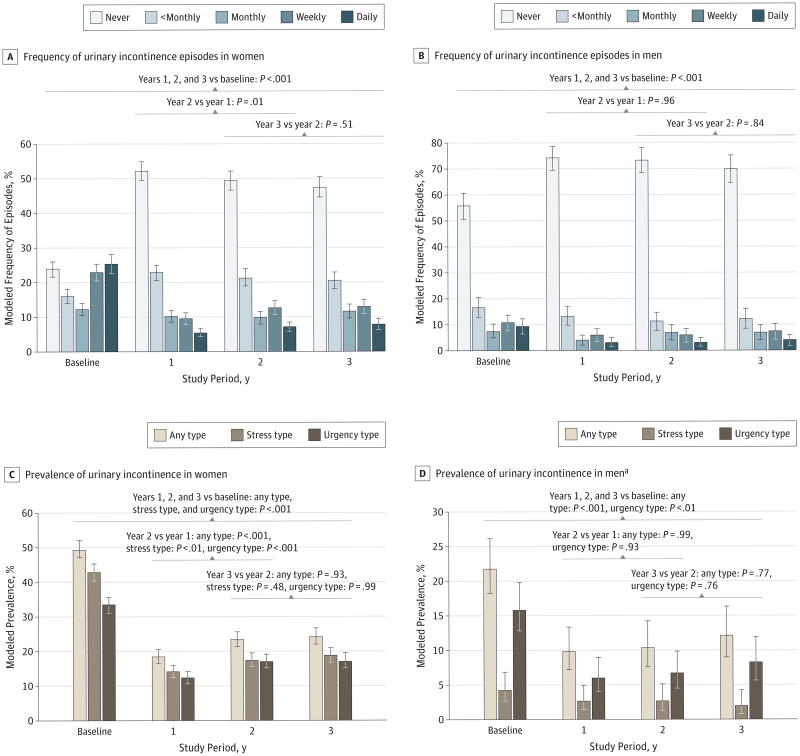
The frequency of incontinence episodes significanly decreased from baseline to each follow-up (observed data in Table 2; modeled data in Figure 2A and B and eTable 2A in the Supplement. Among women, the odds of improvement were highest at 1 year (OR, 7.67; 95% CI, 6.31-9.33) and remained high through 3 years (OR, 6.00; 95% CI, 4.92-7.31 at 2 years and OR, 5.36; 95% CI, 4.39-6.54 at 3 years) compared with baseline. Incontinence frequency increased in women from 1 to 2 years (odds of improvement, 0.78; 95% CI, 0.64-0.92) but was not different from that at 2 to 3 years (P = .51). Among men, the ORs for improvement from baseline were 2.99 (95% CI, 1.99-4.50), 2.73 (95% CI, 1.79-4.17), and 2.34 (95% CI, 1.53-3.58) at 1, 2, and 3 years, respectively. No changes in incontinence frequency after year 1 were observed.
Figure 2. Modeled Frequency of Urinary Incontinence Episodes and Prevalence of Any-Type, Stress-Type, and Urgency-Type Urinary Incontinence Before and After Bariatric Surgery.
Each follow-up time point was compared with baseline. Bars indicate 95% CIs.
a The overall P value for a time effect of change in prevalence of stress urinary incontinence among men was 0.31 so pairwise comparisons were not made.
Among women, the proportion reporting at least weekly prevalence of any-type, stress-type, or urgency-type incontinence was significantly lower at all follow-up time points compared with baseline (Figure 2C and eTable 2A in the Supplement). The prevalence of all types of incontinence was significantly higher at 2 years vs 1 year and then remained stable from 2 to 3 years. Trends among men were similar to those among women (Figure 2D and eTable 2A in the Supplement); however, with smaller sample size and lower incontinence prevalence, there was low power to detect small changes over time.
The percentage of women in remission was significantly lower at 2 years than at 1 year (P < .001) (Table 3 and eTable 3A in the Supplement). Although the mean weight change from baseline was similar at 1 and 2 years, there was variability in weight change.29 Therefore, we evaluated whether weight change from 1 to 2 years was associated with incontinence relapse at 2 years and found that each 5-kg increase in weight from years 1 to 2 increased the risk of incontinence relapse in women at 2 years by 29.4% (74 of 426) (relative risk, 1.29; 95% CI, 1.13-1.49).
Table 3. Modeled Urinary Incontinence Remission and Incidence After Bariatric Surgery.
| Urinary Incontinence Remission Since Baseline | No. | Model-Based Estimate, % (95% CI) | Adjusted P Value | |||
|---|---|---|---|---|---|---|
| Year 1 | Year 2 | Year 3 | Year 2 vs Year 1 | Year 3 vs Year 2 | ||
| Womena | ||||||
| Any type | 772 | 67.0 (63.7-70.6) | 59.9 (56.3-63.7) | 59.3 (55.6-63.2) | <.001 | .93 |
| Complete remissionb | 772 | 28.9 (25.7-32.4) | 26.8 (23.6-30.4) | 27.4 (24.2-31.2) | .44 | .92 |
| Stress type | 645 | 71.5 (67.9-75.3) | 68.3 (64.6-72.3) | 65.7 (61.8-69.9) | .20 | .34 |
| Urgency type | 505 | 72.5 (68.5-76.7) | 60.3 (55.8-65.1) | 59.9 (55.4-64.8) | <.001 | .98 |
| Incidence since baselinec | 793 | 3.3 (2.0-5.3) | 5.9 (4.0-8.7) | 6.6 (4.5-9.6) | <.01 | .79 |
| Men | ||||||
| Any type | 92 | 67.9 (58.8-78.5) | 68.7 (59.3-79.6) | 69.9 (60.2-81.2) | .98 | .96 |
| Complete remission | 92 | 49.8 (40.1-61.8) | 46.4 (36.5-59.0) | 47.3 (37.2-60.1) | .79 | .98 |
| Stress type | 18 | NAd | NAd | NAd | NAd | NAd |
| Urgency type | 67 | 72.5 (62.1-84.5) | 70.4 (59.7-82.9) | 73.5 (62.4-86.6) | .84 | .86 |
| Incidence since baseline | 330 | 3.3 (1.6-6.9) | 4.1 (2.0-8.4) | 6.6 (3.6-12.0) | .81 | .21 |
Abbreviation: NA, not applicable.
Remission refers to change from weekly prevalent incontinence at baseline (ie, weekly or more frequent incontinence) to less than weekly incontinence at follow-up.
Complete remission refers to change from weekly prevalent incontinence at baseline (ie, weekly or more frequent incontinence) to no incontinence at follow-up.
Incidence refers to change from less than weekly or no incontinence at baseline to prevalent incontinence (ie, weekly or more frequent incontinence) at follow-up.
Too rare to model: 10 of 13 were in remission at 1 year, 13 of 15 were in remission at 2 years, and 14 of 14 were in remission at 3 years.
The observed and modeled urinary frequency, prevalence, remission, and incidence from the sensitivity analysis (eTables 2B and 3B in the Supplement) were similar to the primary analyses, which assumed that data were missing at random. Furthermore, there were no differences in change over time (eTables 2B and 3B in the Supplement). Thus, we concluded that the modeled results reported can be used to draw conclusions about the entire analysis sample.
Greater weight loss was independently associated with improvement and remission of incontinence among women and men (Table 4). Each 5% additional weight loss was associated with a 27.7% (95% CI, 18.7%-37.4%) greater odds of improvement and an 8.2% (95% CI, 6.0%-10.4%) greater chance of remission in women, and with a 36.5% (95% CI, 9.1%-70.7%) greater odds of improvement and a 7.2% (95% CI, 1.7%-13.0%) greater chance of remission in men. Older age and severe walking limitation reduced the odds of incontinence improvement in women and men, as well as the chances of remission among women. For women, other factors independently associated with incontinence improvement were the presence of stress or urgency incontinence (vs both) at baseline, receipt of Roux-en-Y gastric bypass (vs laparoscopic adjustable gastric band), and absence of pregnancy in the past year (vs pregnancy).
Table 4. Factors Independently Related to Improvement in Frequency of Urinary Incontinence Episodes and to Urinary Incontinence Remission After Bariatric Surgery Among 772 Women and 92 Men With Prevalence of Urinary Incontinence at Least Weekly at Baselinea.
| Variable | Women | Men | ||||||
|---|---|---|---|---|---|---|---|---|
| Improvement in Frequency | Remission | Improvement in Frequency | Remission | |||||
| OR (95% CI) | P Value | RR (95% CI) | P Value | OR (95% CI) | P Value | RR (95% CI) | P Value | |
| Age, per 10 y older | 0.76 (0.65-0.89) | <.001 | 0.93 (0.89-0.97) | <.01 | 0.52 (0.31-0.90) | .02 | 0.87 (0.78-0.98) | .02 |
| Black race, reference is nonblack | 1.86 (0.98-3.52) | .06 | 1.14 (0.96-1.35) | .13 | 1.11 (0.08-14.81) | .94 | 1.17 (0.66-2.08) | .58 |
| Baseline urinary incontinence type, reference is both types | <.001 | b | b | b | ||||
| Stress type only | 2.24 (1.58-3.19) | NA | NA | NA | NA | NA | NA | |
| Urgency type only | 1.81 (1.11-2.95) | NA | NA | NA | NA | NA | NA | |
| Neither type | 1.81 (0.63-5.16) | NA | NA | NA | NA | NA | NA | |
| Bariatric surgical procedure, reference is laparoscopic adjustable gastric band | .02 | b | b | b | ||||
| Roux-en-Y gastric bypass | 1.63 (1.07-2.49) | NA | NA | NA | NA | NA | NA | |
| Other | 0.88 (0.41-1.92) | NA | NA | NA | NA | NA | NA | |
| Weight loss from baseline, per 5% weight loss | 1.28 (1.19-1.37) | <.001 | 1.08 (1.06-1.10) | <.001 | 1.37 (1.09-1.71) | <.01 | 1.07 (1.02-1.13) | .01 |
| Presurgery/postsurgery severe walking limitation | .01 | .01 | .04 | b | ||||
| Yes/yes vs no/no | 0.33 (0.16-0.66) | 0.62 (0.44-0.88) | 0.14 (0.01-1.59) | NA | NA | |||
| No/yes vs no/no | 0.55 (0.21-1.42) | 0.72 (0.49-1.05) | c | NA | NA | |||
| Yes/no vs no/no | 0.94 (0.48-1.84) | 0.90 (0.69-1.19) | 0.34 (0.02-7.52) | NA | NA | |||
| Yes/no vs yes/yes | 2.84 (1.21-6.63) | 1.46 (1.07-1.98) | c | NA | NA | |||
| After bariatric surgery | ||||||||
| Current smoker | 0.92 (0.57-1.49) | .74 | 0.97 (0.84-1.11) | .64 | 0.17 (0.03-0.98) | .05 | 0.97 (0.81-1.16) | .72 |
| Pregnancy in past year | 0.24 (0.07-0.79) | .02 | 0.88 (0.55-1.41) | .59 | NA | NA | NA | NA |
Abbreviations: NA, not applicable; OR, odds ratio; RR, relative risk.
Analyses controlled for study period and presurgery frequency of urinary incontinence, age, race, current smoking status, pregnancy in past year, percentage weight change, and any of the following variables that reached statistical significance (P < .05): preoperative history of live birth or stillbirth, ethnicity, bariatric surgical procedure, history of stroke, history of heart disease, history of hysterectomy, hormone therapy use, and preoperative and postoperative status (ie, no preoperative/no postoperative, no preoperative/yes postoperative, yes preoperative/no postoperative and yes preoperative/yes postoperative) of diabetes mellitus, hypertension, asthma, severe walking limitation, and depressive symptoms. Due to missing covariates, frequency models include 641 women and 77 men, and remission models include 646 women and 81 men of the 772 women and 92 men with prevalence of urinary incontinence at least weekly at baseline. The ratio of the generalized χ2 statistic and its df for improvement models was 0.25 for women and 0.75 for men. For remission models, it was 0.85 for women and 0.86 for men.
The RR (95% CI) or OR (95% CI) is not reported for variables that were not significant (P ≥ .05 overall) unless they were forced into the model (ie, age, race, current smoking status, pregnancy in past year, and percentage weight change).
Too few in no/yes group (≤3 per follow-up assessment) or yes/no group (≤2 per follow-up assessment) for valid comparison.
Discussion
Among women and men with severe obesity who underwent a bariatric surgical procedure, almost half of the women and more than one-fifth of the men reported prevalent (ie, at least weekly episodes) incontinence in the past 3 months. These percentages are similar to those in previous studies12-16 of patients with severe obesity planning weight reduction surgery.
During up to 3 years after bariatric surgery, substantial improvements in incontinence were observed, with most women and men achieving remission. Improvements after surgery were seen for any-type and urgency-type incontinence (in women and men) and for stress-type incontinence (in women only).
While impressive percentages of women had partial or complete improvements in incontinence, these percentages are lower than those observed in other bariatric surgery studies reporting incontinence remission in more than 90%14,23,24 and resolution in more than 50%12-14,21-24 of women at 1 year after surgery. Differences in these estimates may reflect differences in definitions of prevalent incontinence or in participant characteristics among prior smaller studies. Our finding that weight gain over the second postoperative year increased the risk of incontinence relapse highlights the importance of continued follow-up.
In contrast, we observed higher percentages of men with partial or complete remission compared with 2 small studies16,36 (n = 8 and n = 7, respectively) that found no improvement in incontinence after surgical weight loss. A behavioral weight loss program for overweight or obese adults with diabetes mellitus resulting in 9% weight loss at 1 year was associated with incontinence remission in 61 of 109 men (56.0%),20 similar to what is reported herein.
The magnitude of weight loss was an independent predictor of incontinence improvement for women and men. This is similar to the results of other studies12-14,16,21-24 of surgical and behavioral weight loss. The receipt of Roux-en-Y gastric bypass was associated with improvement in incontinence among women independent of weight loss, suggesting that this procedure may have independent effects on incontinence.29 The odds of improvement in incontinence after surgery were also lower among patients with known risk factors for incontinence such as older age, severe walking limitation, and pregnancy in the past year.3,8,34,35
Improvement in incontinence after weight reduction may be explained by multiple mechanisms.17,37,38 Obesity may contribute to incontinence because of greater intra-abdominal pressure due to central adiposity, which increases bladder pressure and urethral mobility, leading to stress incontinence, and may exacerbate detrusor instability and urgency incontinence. Obesity is also associated with diabetes mellitus and inflammation, which are risk factors for incontinence. Weight reduction may decrease pressure on the bladder and pelvic floor and alter systemic inflammation and hormonal milieu, reducing incontinence. Improvements in incontinence after bariatric surgery may also have resulted from positive changes in lifestyle (increased physical activity)39,40 or dietary composition (decreased bladder irritants such as caffeine).41
The desire to improve medical comorbidities is the primary reason why patients seek weight loss surgery,42 and urinary incontinence has been identified as a comorbidity associated with particularly great dissatisfaction among patients before bariatric surgery.43 Therefore, obese patients' perceptions of the effect of incontinence before weight loss and expectations of incontinence improvement after weight loss may help them commit to continuing practices that optimize weight loss after bariatric surgery.
Our study is a large multicenter trial, with data collected over 3 years of follow-up on a geographically diverse cohort using standardized and validated measures.25 These factors should make the results of our study generalizable to clinical practice. While the sample did not have complete follow-up data, we conclude based on the sensitivity analysis that the results reported can be used to draw conclusions about the entire analysis sample. However, our trial is an observational study without a control group, and baseline differences (measured and unmeasured) may contribute to differences in weight and incontinence outcomes. Data on incontinence were ascertained by self-report, and to the extent that self-report is not reliable, rates of incontinence prevalence and change may be underestimated or overestimated. Nevertheless, self-report may best represent incontinence from the patient's perspective, and the incontinence measures used in this study were previously validated against voiding diaries,26 the current gold standard for assessment of incontinence frequency and type.
Conclusions
In conclusion, bariatric surgery for women and men with severe obesity was associated with substantial improvement in urinary incontinence through 3 years after surgery. Improvement in urinary incontinence may help motivate severely obese patients with incontinence to undergo bariatric surgery and offer another important longer-term benefit of bariatric procedures.
Supplementary Material
Acknowledgments
Dr Subak reported receiving funding from Astellas Scientific and Medical Affairs, Inc via contracts with the University of California, San Francisco. Dr Courcoulas reported receiving research grants from Allergan, Pfizer, Covidien, EndoGastric Solutions, and Nutrisystem and reported serving on the scientific advisory boards of Ethicon and Johnson & Johnson Health Care Systems. Dr Flum reported receiving research grants from Covidien and Sanofi-Aventis. Dr Pender reported receiving research grants from GlaxoSmithKline and Covidien. Dr Pories reported receiving a research grant from Johnson & Johnson Health Care Systems. Dr Wolfe reported serving as a consultant and advisor for Covidien, Ethicon, Crospon, Viudico, and Medtronics and reported receiving a research grant from Enteromedics. Dr Huang reported receiving funding from Pfizer via contracts with the University of California, San Francisco to conduct research unrelated to bariatric surgery or urinary incontinence.
Funding/Support: The Longitudinal Assessment of Bariatric Surgery 2 represents a cooperative agreement funded by the National Institute of Diabetes and Digestive and Kidney Diseases, including the following grant numbers: grant U01 DK066557 (Data Coordinating Center), grant U01-DK66667 (Columbia University Medical Center) in collaboration with grant UL1-RR024996 (Cornell University Medical Center), grant U01-DK66568 (University of Washington) in collaboration with grant M01RR-00037 (Cornell University Medical Center), grant U01-DK66471 (Neuropsychiatric Research Institute), grant U01-DK66526 (East Carolina University), grant U01-DK66585 (University of Pittsburgh Medical Center) in collaboration with grant UL1-RR024153 (Cornell University Medical Center), and grant U01-DK66555 (Oregon Health & Science University). Dr Subak is the recipient of grant K24 DK080775 from the National Institute of Diabetes and Digestive and Kidney Diseases.
Role of the Funder/Sponsor: The National Institute of Diabetes and Digestive and Kidney Diseases scientists contributed to the design and conduct of the study, which included collection and management of data. The project scientist from the National Institute of Diabetes and Digestive and Kidney Diseases served as a member of the steering committee, along with the principal investigator from each clinical site and the Data Coordinating Center. The Data Coordinating Center housed all data during the study and performed data analyses according to a prespecified plan developed by the Data Coordinating Center biostatistician and approved by the steering committee and independent data and safety monitoring board. The decision to publish was made by the Longitudinal Assessment of Bariatric Surgery 2 steering committee, with no restrictions imposed by the sponsor. A National Institute of Diabetes and Digestive and Kidney Diseases scientist contributed to the interpretation of the data and preparation, review, or approval of the manuscript.
Footnotes
Author Contributions: Dr King and Ms Chen had, full access to all the data in the study and take, responsibility for the integrity of the data and the, accuracy of the data analysis.
Study concept and design: Subak, King.
Acquisition, analysis, or interpretation of data: Subak, King, Belle, Chen, Courcoulas, Flum, Pories, Wolfe, Huang.
Drafting of the manuscript: Subak, King.
Critical revision of the manuscript for important, intellectual content: All authors.
Statistical analysis: King, Chen.
Obtained funding: Belle, Courcoulas, Flum, Pories, Wolfe.
Study supervision: Belle, Courcoulas, Flum, Pories, Wolfe.
Conflict of Interest Disclosures: No other disclosures were reported.
Previous Presentations: This study was presented at the 2014 Annual Meeting of the American Urological Association; May 18, 2014; Orlando, Florida; and at the American Urogynecologic Society and International Urogynecological Association Joint Annual Scientific Meeting; July 25, 2014; Washington, DC.
References
- 1.Markland AD, Richter HE, Fwu CW, Eggers P, Kusek JW. Prevalence and trends of urinary incontinence in adults in the United States, 2001 to 2008. J Urol. 2011;186(2):589–593. doi: 10.1016/j.juro.2011.03.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thom DH, Van Den Eeden SK, Ragins AI, et al. Differences in prevalence of urinary incontinence by race/ethnicity. J Urol. 2006;175(1):259–264. doi: 10.1016/S0022-5347(05)00039-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buckley BS, Lapitan MC. Epidemiology Committee of the Fourth International Consultation on Incontinence, Paris 2008. Prevalence of urinary incontinence in men, women, and children: current evidence: findings of the Fourth International Consultation on Incontinence. Urology. 2010;76(2):265–270. doi: 10.1016/j.urology.2009.11.078. [DOI] [PubMed] [Google Scholar]
- 4.Grimby A, Milsom I, Molander U, Wiklund I, Ekelund P. The influence of urinary incontinence on the quality of life of elderly women. Age Ageing. 1993;22(2):82–89. doi: 10.1093/ageing/22.2.82. [DOI] [PubMed] [Google Scholar]
- 5.Huang AJ, Brown JS, Kanaya AM, et al. Quality-of-life impact and treatment of urinary incontinence in ethnically diverse older women. Arch Intern Med. 2006;166(18):2000–2006. doi: 10.1001/archinte.166.18.2000. [DOI] [PubMed] [Google Scholar]
- 6.Ganz ML, Smalarz AM, Krupski TL, et al. Economic costs of overactive bladder in the United States. Urology. 2010;75(3):526–532. 532.e1–532.e18. doi: 10.1016/j.urology.2009.06.096. [DOI] [PubMed] [Google Scholar]
- 7.Coyne KS, Wein A, Nicholson S, Kvasz M, Chen CI, Milsom I. Economic burden of urgency urinary incontinence in the United States: a systematic review. J Manag Care Pharm. 2014;20(2):130–140. doi: 10.18553/jmcp.2014.20.2.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Danforth KN, Townsend MK, Lifford K, Curhan GC, Resnick NM, Grodstein F. Risk factors for urinary incontinence among middle-aged women. Am J Obstet Gynecol. 2006;194(2):339–345. doi: 10.1016/j.ajog.2005.07.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khullar V, Sexton CC, Thompson CL, Milsom I, Bitoun CE, Coyne KS. The relationship between BMI and urinary incontinence subgroups: results from EpiLUTS. Neurourol Urodyn. 2014;33(4):392–399. doi: 10.1002/nau.22428. [DOI] [PubMed] [Google Scholar]
- 10.Townsend MK, Curhan GC, Resnick NM, Grodstein F. BMI, waist circumference, and incident urinary incontinence in older women. Obesity (Silver Spring) 2008;16(4):881–886. doi: 10.1038/oby.2008.14. [DOI] [PubMed] [Google Scholar]
- 11.Brown JS, Seeley DG, Fong J, Black DM, Ensrud KE, Grady D Study of Osteoporotic Fractures Research Group. Urinary incontinence in older women: who is at risk? Obstet Gynecol. 1996;87(5, pt 1):715–721. doi: 10.1016/0029-7844(96)00013-0. [DOI] [PubMed] [Google Scholar]
- 12.Burgio KL, Richter HE, Clements RH, Redden DT, Goode PS. Changes in urinary and fecal incontinence symptoms with weight loss surgery in morbidly obese women. Obstet Gynecol. 2007;110(5):1034–1040. doi: 10.1097/01.AOG.0000285483.22898.9c. [DOI] [PubMed] [Google Scholar]
- 13.Deitel M, Stone E, Kassam HA, Wilk EJ, Sutherland DJ. Gynecologic-obstetric changes after loss of massive excess weight following bariatric surgery. J Am Coll Nutr. 1988;7(2):147–153. doi: 10.1080/07315724.1988.10720232. [DOI] [PubMed] [Google Scholar]
- 14.Laungani RG, Seleno N, Carlin AM. Effect of laparoscopic gastric bypass surgery on urinary incontinence in morbidly obese women. Surg Obes Relat Dis. 2009;5(3):334–338. doi: 10.1016/j.soard.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 15.Richter HE, Burgio KL, Clements RH, Goode PS, Redden DT, Varner RE. Urinary and anal incontinence in morbidly obese women considering weight loss surgery. Obstet Gynecol. 2005;106(6):1272–1277. doi: 10.1097/01.AOG.0000187299.75024.c4. [DOI] [PubMed] [Google Scholar]
- 16.Ranasinghe WK, Wright T, Attia J, et al. Effects of bariatric surgery on urinary and sexual function. BJU Int. 2011;107(1):88–94. doi: 10.1111/j.1464-410X.2010.09509.x. [DOI] [PubMed] [Google Scholar]
- 17.Subak LL, Whitcomb E, Shen H, Saxton J, Vittinghoff E, Brown JS. Weight loss: a novel and effective treatment for urinary incontinence. J Urol. 2005;174(1):190–195. doi: 10.1097/01.ju.0000162056.30326.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Subak LL, Wing R, West DS, et al. PRIDE Investigators. Weight loss to treat urinary incontinence in overweight and obese women. N Engl J Med. 2009;360(5):481–490. doi: 10.1056/NEJMoa0806375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wing RR, Creasman JM, West DS, et al. Program to Reduce Incontinence by Diet and Exercise. Improving urinary incontinence in overweight and obese women through modest weight loss. Obstet Gynecol. 2010;116(2, pt 1):284–292. doi: 10.1097/AOG.0b013e3181e8fb60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Breyer BN, Phelan S, Hogan PE, et al. Look AHEAD Research Group. Intensive lifestyle intervention reduces urinary incontinence in overweight/obese men with type 2 diabetes: results from the Look AHEAD trial. J Urol. 2014;192(1):144–149. doi: 10.1016/j.juro.2014.02.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Whitcomb EL, Horgan S, Donohue MC, Lukacz ES. Impact of surgically induced weight loss on pelvic floor disorders. Int Urogynecol J. 2012;23(8):1111–1116. doi: 10.1007/s00192-012-1756-5. [DOI] [PubMed] [Google Scholar]
- 22.Cuicchi D, Lombardi R, Cariani S, Leuratti L, Lecce F, Cola B. Clinical and instrumental evaluation of pelvic floor disorders before and after bariatric surgery in obese women. Surg Obes Relat Dis. 2013;9(1):69–75. doi: 10.1016/j.soard.2011.08.013. [DOI] [PubMed] [Google Scholar]
- 23.Srinivasa S, Hill LS, Sammour T, Hill AG, Babor R, Rahman H. Early and mid-term outcomes of single-stage laparoscopic sleeve gastrectomy. Obes Surg. 2010;20(11):1484–1490. doi: 10.1007/s11695-010-0267-z. [DOI] [PubMed] [Google Scholar]
- 24.Kuruba R, Almahmeed T, Martinez F, et al. Bariatric surgery improves urinary incontinence in morbidly obese individuals. Surg Obes Relat Dis. 2007;3(6):586–590. doi: 10.1016/j.soard.2007.08.007. [DOI] [PubMed] [Google Scholar]
- 25.Belle SH, Berk PD, Chapman WH, et al. LABS Consortium. Baseline characteristics of participants in the Longitudinal Assessment of Bariatric Surgery-2 (LABS-2) study. Surg Obes Relat Dis. 2013;9(6):926–935. doi: 10.1016/j.soard.2013.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bradley CS, Brown JS, Van Den Eeden SK, Schembri M, Ragins A, Thom DH. Urinary incontinence self-report questions: reproducibility and agreement with bladder diary. Int Urogynecol J. 2011;22(12):1565–1571. doi: 10.1007/s00192-011-1503-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Burgio KL, Ives DG, Locher JL, Arena VC, Kuller LH. Treatment seeking for urinary incontinence in older adults. J Am Geriatr Soc. 1994;42(2):208–212. doi: 10.1111/j.1532-5415.1994.tb04954.x. [DOI] [PubMed] [Google Scholar]
- 28.Tennstedt SL, Chiu GR, Link CL, Litman HJ, Kusek JW, McKinlay JB. The effects of severity of urine leakage on quality of life in Hispanic, white, and black men and women: the Boston Community Health Survey. Urology. 2010;75(1):27–33. doi: 10.1016/j.urology.2009.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Courcoulas AP, Christian NJ, Belle SH, et al. Longitudinal Assessment of Bariatric Surgery (LABS) Consortium. Weight change and health outcomes at 3 years after bariatric surgery among individuals with severe obesity. JAMA. 2013;310(22):2416–2425. doi: 10.1001/jama.2013.280928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gosman GG, King WC, Schrope B, et al. Reproductive health of women electing bariatric surgery. Fertil Steril. 2010;94(4):1426–1431. doi: 10.1016/j.fertnstert.2009.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Edwards D, Berry JJ. The efficiency of simulation-based multiple comparisons. Biometrics. 1987;43(4):913–928. [PubMed] [Google Scholar]
- 32.Li KH. Imputation using Markov chains. J Stat Comput Simul. 1988;30(1):57–79. [Google Scholar]
- 33.Molenberghs G, Kenward MG, editors. Missing Data in Clinical Studies. chap 16 Hoboken, NJ: John Wiley & Sons Inc; 2007. Pattern-mixture models. [Google Scholar]
- 34.Wu JM, Vaughan CP, Goode PS, et al. Prevalence and trends of symptomatic pelvic floor disorders in U.S. women. Obstet Gynecol. 2014;123(1):141–148. doi: 10.1097/AOG.0000000000000057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tennstedt SL, Link CL, Steers WD, McKinlay JB. Prevalence of and risk factors for urine leakage in a racially and ethnically diverse population of adults: the Boston Area Community Health (BACH) Survey. Am J Epidemiol. 2008;167(4):390–399. doi: 10.1093/aje/kwm356. [DOI] [PubMed] [Google Scholar]
- 36.Roberson EN, Gould JC, Wald A. Urinary and fecal incontinence after bariatric surgery. Dig Dis Sci. 2010;55(9):2606–2613. doi: 10.1007/s10620-010-1190-9. [DOI] [PubMed] [Google Scholar]
- 37.Townsend MK, Danforth KN, Lifford KL, et al. Incidence and remission of urinary incontinence in middle-aged women. Am J Obstet Gynecol. 2007;197(2):167.e1–167.e5. doi: 10.1016/j.ajog.2007.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Subak LL, Richter HE, Hunskaar S. Obesity and urinary incontinence: epidemiology and clinical research update. J Urol. 2009;182(6 suppl):S2–S7. doi: 10.1016/j.juro.2009.08.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Townsend MK, Danforth KN, Rosner B, Curhan GC, Resnick NM, Grodstein F. Physical activity and incident urinary incontinence in middle-aged women. J Urol. 2008;179(3):1012–1016. doi: 10.1016/j.juro.2007.10.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Danforth KN, Shah AD, Townsend MK, et al. Physical activity and urinary incontinence among healthy, older women. Obstet Gynecol. 2007;109(3):721–727. doi: 10.1097/01.AOG.0000255973.92450.24. [DOI] [PubMed] [Google Scholar]
- 41.Jura YH, Townsend MK, Curhan GC, Resnick NM, Grodstein F. Caffeine intake, and the risk of stress, urgency and mixed urinary incontinence. J Urol. 2011;185(5):1775–1780. doi: 10.1016/j.juro.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Munoz DJ, Lal M, Chen EY, et al. Why patients seek bariatric surgery: a qualitative and quantitative analysis of patient motivation. Obes Surg. 2007;17(11):1487–1491. doi: 10.1007/s11695-008-9427-9. [DOI] [PubMed] [Google Scholar]
- 43.Karmali S, Kadikoy H, Brandt ML, Sherman V. What is my goal? expected weight loss and comorbidity outcomes among bariatric surgery patients. Obes Surg. 2011;21(5):595–603. doi: 10.1007/s11695-009-0060-z. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.