Abstract
In China, approximately 30,000 babies are born with hearing impairment each year. However, the molecular factors causing congenital hearing impairment in the Xiamen area of Fujian province have not been evaluated. To provide accurate genetic testing and counseling in the Xiamen area, we investigated the molecular etiology of non-syndromic deafness in a deaf population from Xiamen. Unrelated students with hearing impairment (n = 155) who attended Xiamen Special Education School in Fujian Province were recruited for this study. Three common deafness-related genes, GJB2, SLC26A4, and mtDNA12SrRNA, were analyzed using all-exon sequencing. GJB2 mutations were detected in 27.1% (42/155) of the entire cohort. The non-syndromic hearing loss (NSHL) hotspot mutations c.109G>A (p.V37I) and c.235delC were found in this population, whereas the Caucasian hotspot mutation c.35delG was not. The allelic frequency of the c.109G>A mutation was 9.03% (28/310), slightly higher than that of c.235delC (8.39%, 26/310), which is the most common GJB2 mutation in most areas of China. The allelic frequency of the c.109G>A mutation was significantly higher in this Xiamen’s deaf population than that in previously reported cohorts (P = 0.00). The SLC26A4 mutations were found in 16.77% (26/155) of this cohort. The most common pathogenic allele was c.IVS7-2A>G (6.13%, 19/310), and the second most common was the c.1079C>T (p.A360V) mutation (1.94%, 6/310) which has rarely been reported as a hotspot mutation in other studies. The mutation rate of mtDNA12SrRNA in this group was 3.87% (6/155), all being the m.A1555G mutation. These findings show the specificity of the common deaf gene-mutation spectrum in this area. According to this study, there were specific hotspot mutations in Xiamen deaf patients. Comprehensive sequencing analysis of the three common deaf genes can help portray the mutation spectrum and develop optimal testing strategies for deaf patients in this area.
Introduction
Hearing impairment is among the most common congenital disorders; approximately half of the cases are caused by genetic factors. In China, many previous genetic screening studies have shown that GJB2, SLC26A4, and mtDNA12SrRNA are the three most common causes of non-syndromic deafness, and the mutations in these three genes can explain 26.65–35.7% of the pathogenesis of Chinese non-syndromic hearing impairment [1–3]. Mutations in GJB2 have been reported to be the most common molecular defect in the Chinese deaf population, with an almost 21% mutation detection rate; of these mutations, c.235delC is the most common in the Chinese deaf population [4,5]. The most common mutation of SLC26A4 seen in the Chinese deaf population is c.IVS7-2A>G; its detection rate can be as high as 12.5% [6–8]. The most common mutation of mtDNA12SrRNA is m.A1555G, the frequency of which was reported to be 3.43% in a Chinese deaf population [9].
China is a large country with the highest population in the world. Chinese people from different areas may have different genetic backgrounds due to geographical and language separation [10]. Xiamen is a city in the South Fujian region in southern China, neighboring the Golden Gate Island of Taiwan. Because it is an island, Xiamen communicated with the mainland by boat and it was relatively isolated before the construction of Xiamen Gaoji Seawall in 1955. The most ancient Xiamen resident migrated from the Chinese Central Plains region due to the wars during the Chinese Shang, Tang, and Song Dynasties, and maintained their language (now called Hokkien or Southern Min) and traditional culture. The close-relative marriage rule can be traced back to ancient China, where intermarriages among individuals with the same surname or among clansmen were forbidden or not encouraged. However, the phenomenon of marriage among individuals who have the same language and culture prevailed [11]. Until now, no systematic genetic analysis of deaf patients in Xiamen has been reported previously. To provide accurate genetic testing and counseling in the Xiamen area, we evaluated the molecular etiology of non-syndromic deafness in a deaf population from Xiamen Special Education School. In total, 155 patients with severe-to-profound hearing loss were recruited for this investigation. All exons in the open reading frames (ORF) of the GJB2, SLC26A4, and mtDNA12SrRNA genes were sequenced and analyzed.
Materials and Methods
Patients and DNA samples
In total, 155 unrelated patients with hearing impairment (152 students, three teachers) from Xiamen Special Education School in Fujian province were recruited for this study. The patient cohort consisted of 93 males and 62 females, 5–36 years old (13.40 years, on average): in terms of ethnicity, the cohort comprised 153 Han and two She. Hearing tests demonstrated that the level of hearing loss was severe to profound in all cases. There were 25 patients whose families had more than one other family member with a hearing impairment. No family had a consanguineous marriage except that one patient’s parents were cousin.
The protocol for this investigation was performed with the approval of the ethics committees of the Chinese PLA General Hospital and Fujian Provincial Hospital. The notification of deafness gene detection was performed a half month prior. We provided the consent form and individual information questionnaire to patients and guardians who volunteered to participate in this detection study. We obtained informed consent from all participants; in the case of minors, consent was obtained from their parents/guardians on their behalf. All of the subjects or their guardians signed the informed consent forms prior to blood sampling. Questionnaires included basic information, including name, age, address, family history, health records of the mother during pregnancy, and a clinical history of the patient, such as infections, possible head or brain injury, and the use of aminoglycoside antibiotics. All subjects underwent hearing tests and medical examinations. DNA was extracted from peripheral blood leukocytes using a commercially available DNA extraction kit (Watson Biotechnologies Inc., Shanghai, China).
Variant analysis
The coding exons plus approximately 50–100 bp of the flanking intron regions of GJB2, SLC26A4, and mtDNA12SrRNA were amplified by polymerase chain reaction (PCR), and Sanger sequencing was used to determine the sequences in all patients. According to the manufacturer’s manual, the results were analyzed using an ABI 3100 DNA sequencing machine (ABI, Foster City, CA, USA) and the ABI 3100 Analysis Software (ver. 3.7 NT). Patients with monoallelic GJB2 coding region mutations were further tested for the GJB2 c.IVS1+1G>A mutation or defects in GJB2 exon 1 and its basal promoter [5,6]. Data analysis was performed using SPSS20.0 software.
Results
GJB2
Fourteen variants were identified in this cohort. Seven of them were pathogenic including three frameshift deletions (c.235delC, c.176del16, c.299delAT), one frameshift insertion (c.512insAACG), and three missense mutations [c.109G>A(p.V37I), c.257C>G(p.T86R), c.187G>T(p.V63L)]. The mutant alleles of GJB2 accounted for 20.0% (62/310) of the total alleles in the 155 NSHL patients(Table 1). Unlike most areas of China, the most common mutation allele of GJB2 in Xiamen was not c.235delC but c.109G>A. The allele frequency of c.109G>A was 9.03% (28/310), followed by 8.39% (26/310) for c.235delC, 0.65% (2/310) for c.257C>G, 0.65% (2/310) for c.299delAT, 0.65% (2/310) for c.512insAAGG, 0.32% (1/310) for c.176del16, and 0.32% (1/310) for c.187G>A (Table 2). There were seven types of GJB2 polymorphisms: c.11G>A, c.34G>T, c.79G>A, c.341A>G, c.368C>A, c.571T>C, and c.608T>C. All of the variants were reported and discussed in previous studies.
Table 1. GJB2 genotypes of deaf patients from Xiamen special education school.
| Allele 1 | Allele 2 | Number of patients | ||||
|---|---|---|---|---|---|---|
| Nucleotide change | Consequence or amino acid change | Category | Nucleotide change | Consequence or amino acid change | Category | |
| c.109G>A[12] | p.V37I | Pathogenic | c.109G>A | p.V37I | Pathogenic | 4 |
| c.176del16[5] | Frameshift | Pathogenic | c.257C>G[5] | p.T86R | Pathogenic | 1 |
| c.235delC[5] | Frameshift | Pathogenic | c.235delC | Frameshift | Pathogenic | 9 |
| c.235delC | Frameshift | Pathogenic | c.299delAT[13] | Frameshift | Pathogenic | 2 |
| c.235delC | Frameshift | Pathogenic | c.257C>G | p.T86R | Pathogenic | 1 |
| c.235delC | Frameshift | Pathogenic | c.512insAACG | Frameshift | Pathogenic | 1 |
| c.235delC | Frameshift | Pathogenic | c.109G>A | p.V37I | Pathogenic | 1 |
| c.512insAACG[5] | Frameshift | Pathogenic | c.109G>A | p.V37I | Pathogenic | 1 |
| c.109G>A | p.V37I | Pathogenic | 12 | |||
| c.109G>A | p.V37I | Pathogenic | c.34G>T[5] | p.G12D | Polymorphism | 1 |
| c.109G>A | p.V37I | Pathogenic | c.79G>A,c.341A>G[14] | p.V27I,p.E114G | Polymorphism | 4 |
| c.109G>A | p.V37I | Pathogenic | c.571T>C[15] | p.F191L | Polymorphism | 1 |
| c.187G>T[13] | p.V63L | pathogenic | 1 | |||
| c.235delC | Frameshift | Pathogenic | c.79G>A,c.341A>G | p.V27I,p.E114G | Polymorphism | 1 |
| c.235delC | Frameshift | Pathogenic | c.79G>A | p.V27I | Polymorphism | 1 |
| c.235delC | Frameshift | Pathogenic | c.608T>C[14] | p.I203T | Polymorphism | 1 |
| c.11G>A[16] | p.G4D | Polymorphism | 1 | |||
| c.79G>A,c.341A>G | p.V27I,p.E114G | Polymorphism | 26 | |||
| c.79G>A,c.341A>G | p.V27I,p.E114G | Polymorphism | c.79G>A,c.341A>G | p.V27I,p.E114G | Polymorphism | 10 |
| c.79G>A,c.341A>G | p.V27I,p.E114G | Polymorphism | c.608T>C | p.I203T | Polymorphism | 5 |
| c.79G>A | p.V27I | Polymorphism | c.608T>C | p.I203T | Polymorphism | 3 |
| c.79G>A | p.V27I | Polymorphism | c.368C>A | p.T123N | Polymorphism | 1 |
| c.79G>A | p.V27I | Polymorphism | 8 | |||
| c.341A>G | p.E114G | Polymorphism | 1 | |||
| c.571T>C | p.F191L | Polymorphism | 1 | |||
| c.608T>C | p.I203T | Polymorphism | 9 | |||
Table 2. Allele Frequencies of GJB2 mutation in 155 deaf patients from Xiamen special education school.
| Mutations in the genes | Consequence or amino acid change | Number of alleles | Alleles Frequency (%) | Reference | |
|---|---|---|---|---|---|
| GJB2 | c.109G>A | p.V37I | 28 | 9.03 | 16 |
| c.235delC | Frameshift | 26 | 8.39 | 5 | |
| c.257C>G | p.T86R | 2 | 0.65 | 5 | |
| c.299delAT | Frameshift | 2 | 0.64 | 35 | |
| c.512insAAGG | Frameshift | 2 | 0.65 | 5 | |
| c.176del116 | Frameshift | 1 | 0.32 | 5 | |
| c.187G>A | p.V63L | 1 | 0.32 | 35 |
There were 20 patients (12.9%) confirmed to have GJB2 deafness-causing mutations: 13 homozygotes (nine with the c.235delC allele and four with the c.109G>A allele) and seven compound heterozygotes. Twenty-two patients (14.2%) carried only one heterozygous pathogenic mutation: one with c.187G>T, three with c.235delC and eighteen with c.109G>A. Thus, the detection rate of GJB2 mutations in the patients was 27.1% (42/155) (Table 1).
Among the 24 patients carrying at least one c.109G>A allele, there were four homozygotes, one compound heterozygote with c.235delC, one compound heterozygote with 512insAACG, and 18 single heterozygotes. The second most common mutation of GJB2 in this group was c.235delC, with a mutation allele frequency of 8.39% (26/310): nine homozygotes, five compound heterozygotes, and three heterozygotes.
SLC26A4
Twenty-two variants were identified in this cohort, including three novel variants (c.1167G>A, c.1738_1739delAA, and c.1764_1765insAGGAAAATA). Among the four splice site variants in this cohort, c.IVS7-2A>G and c.IVS16-6G>A are pathogenic because they affect canonical splice donor and acceptor nucleotide positions that had been previously identified; c.IVS11+47T>C was previously identified as a polymorphism, and c.IVS7-18T>C was considered a polymorphism in our laboratory, which will be analyzed further in the Discussion section. The three frameshift insertions [c.916_917insG (FS306, P329*), c.1692_1693insA (FS565, P573*), and c.1764_1765insAGGAAAATA (FS558)], two truncated mutations [c.2086C>T (p.Q696*) and c.1336C>T (p.Q446*)], and one frameshift deletion [c.1738_1739delAA (FS580, P606*)] were considered pathogenic due to a dramatic prematurely altered or truncated protein. Combining the prediction of SIFT and Polyphen-2 with the results of previous studies, the following 12 missense variants were analyzed in our cohort: c.1079C>T (p.A360V), c.2168A>G (p.H723R), c.754T>C (p.S252P), c.1229C>T (p.T410M), c.1472T>C (p.I491T), c.1595G>T (p.S532I), and c.2007C>G (p.D669E) were considered pathogenic mutations, and c.1790T>C (p.L597S) and c.147C>G (p.S49R) were deemed polymorphisms. c.2283A>G (p.T761T) and c.1167G>A (p.G389G, this study) were considered polymorphisms without amino acid sequence alteration after the nucleotide changed. c.2009T>C (p.V670A) still had unknown significance according to our data and prediction, which will be discussed later (Table 3).
Table 3. SLC26A4 genotypes of deaf patients from Xiamen special education school.
| Allele 1 | Allele 2 | Number of patients | ||||
|---|---|---|---|---|---|---|
| Nucleotide change | Consequence or amino acid change | Category | Nucleotide change | Consequence or amino acid change | Category | |
| c.754T>C[17] | p.S252P | Pathogenic | c.1738_1739delAA | FS580,P606* | Pathogenic | 1 |
| c.916_917insG[18] | FS306,P329* | Pathogenic | c.2168A>G[19] | p.H723R | Pathogenic | 1 |
| c.IVS7-2A>G[7] | aberrant splicing | Pathogenic | c.IVS7-2A>G | aberrant splicing | Pathogenic | 5 |
| c.IVS7-2A>G | aberrant splicing | Pathogenic | c.1079C>T[20] | p.A360V | Pathogenic | 3 |
| c.IVS7-2A>G | aberrant splicing | Pathogenic | c.2086C>T[21] | p.Q696* | Pathogenic | 2 |
| c.IVS7-2A>G | aberrant splicing | Pathogenic | c.1336C>T[7] | p.Q446* | Pathogenic | 1 |
| c.IVS7-2A>G | aberrant splicing | Pathogenic | c.2007C>G[22] | p.D669E | Pathogenic | 1 |
| c.IVS7-2A>G | aberrant splicing | Pathogenic | c.2168A>G | p.H723R | Pathogenic | 1 |
| c.1079C>T | p.A360V | Pathogenic | c.1079C>T | p.A360V | Pathogenic | 1 |
| c.1229C>T[17] | p.T410M | Pathogenic | c.2168A>G | p.H723R | Pathogenic | 1 |
| c.1692_1693insA[6] | FS565,P573* | Pathogenic | c.2168A>G | p.H723R | Pathogenic | 1 |
| c.147C>G[23] | p.S49R | pathogenic | 1 | |||
| c.IVS7-2A>G | aberrant splicing | Pathogenic | 1 | |||
| c.1472T>C[7] | p.I491T | Pathogenic | 1 | |||
| c.1595G>T[6] | p.S532I | Pathogenic | 1 | |||
| c.IVS16-6G>A [24] | aberrant splicing | Pathogenic | 2 | |||
| c.IVS16-6G>A | aberrant splicing | Pathogenic | c.IVS11+47T>C[25] | splice site variant | Polymorphism | 1 |
| c.1764_1765insAGGAAAATA | Frameshift | Pathogenic | 1 | |||
| c.2009T>C[23] | p.V670A | Unknown | 2 | |||
| c.IVS7-18T>G[26] | splice site variant | Polymorphism | 3 | |||
| c.IVS7-18T>G | splice site variant | Polymorphism | c.IVS11+47T>C | splice site variant | Polymorphism | 1 |
| c.1167G>A | p.G389G | Silent variants | 1 | |||
| c.IVS11+47T>C | splice site variant | Polymorphism | c.IVS11+47T>C | splice site variant | Polymorphism | 4 |
| c.IVS11+47T>C | splice site variant | Polymorphism | 23 | |||
| c.1790T>C[27] | p.L597S | Polymorphism | 1 | |||
| c.2283A>G[6] | p.T761T | Silent variants | 4 | |||
Note:
*: stop codon
There were 18 (11.61%) patients confirmed to be carrying two SLC26A4 pathogenic mutations: six homozygotes (5 c. IVS 7-2A>G and 1 c.1079C>T), twelve compound heterozygotes, and eight (5.16%) patients with one SLC26A4 pathogenic mutation. Thus, the detection rate of SLC26A4 mutations was 16.77% (26/155) in this patient cohort.
The most common mutation of SLC26A4 was c.IVS7-2A>G, with a 6.13% (19/310) allele frequency. Except for five homozygotes and one heterozygote of it, there were eight patients carrying c.IVS7-2A>G heterozygous mutations combined with the other mutations included three c.1079C>T, two c.2086C>T, one c.2168A>G, one c.1336C>T, and one c.2007C>G.
The mutation allele frequency was 1.61% (5/310) for c.1079C>T, 1.29% (4/310) for c.2168A>G, 0.97% (3/310) for c. ivs16-6G>A, 0.65% (2/310) for c.2086C>T and 0.32% (1/310) for each of the others (Table 4).
Table 4. Allele Frequencies of SLC26A4 mutation in 155 deaf patients from Xiamen special education school.
| Mutations in the genes | Consequence or amino acid change | Number of alleles | Alleles Frequency (%) | Reference | |
|---|---|---|---|---|---|
| SLC26A4 | c.IVS7-2A>G | aberrant splicing | 19 | 6.13 | 7 |
| c.1079C>T | p.A360V | 5 | 1.61 | 23 | |
| c.2168A>G | p.H723R | 4 | 1.29 | 21 | |
| c.IVS16-6G>A | aberrant splicing | 3 | 0.97 | 43 | |
| c.2086C>T | p.Q696* | 2 | 0.65 | 41 | |
| c.754T>C | p.S252P | 1 | 0.32 | 39 | |
| c.916_917insG | FS306,P329* | 1 | 0.32 | 40 | |
| c.1229C>T | p.T410M | 1 | 0.32 | 39 | |
| c.1336C>T | p.Q446* | 1 | 0.32 | 7 | |
| c.1472T>C | p.I491T | 1 | 0.32 | 7 | |
| c.1595G>T | p.S532I | 1 | 0.32 | 6 | |
| c.1692_1693insA | FS565,P573* | 1 | 0.32 | 6 | |
| c.2007C>G | p.D669E | 1 | 0.32 | 42 | |
| c.1738_1739delAA | FS580,606* | 1 | 0.32 | This study | |
| c.1764_1765insAGGAAAATA | Frameshift | 1 | 0.32 | This study |
Note:
*: stop codon
Mutation analysis
c.IVS7-18T>C
This variant has been proposed to exert a likely pathogenic effect according to the reported data (http://deafnessvariationdatabase.org/). According to the Fruitfly analysis tool (http://www.fruitfly.org/seq_tools/splice.html), a change in the splice donor sequence from T to C in intron 7 (c. IVS7-18T>C) of SLC26A4 is predicted to make no difference in splice site recognition by the splicing factor from 0.93 to 0.92 (when the score is reduced to less than 0.4, the mutation may affect the function of the original). We checked the previous records of our laboratory and found that four of 261 control subjects (1.53%) carried the single heterozygous c.IVS7-18T>C allele. Based on prediction analysis and our laboratory data, we concluded that this variation was a polymorphism.
c.2009T>C (p.V670A)
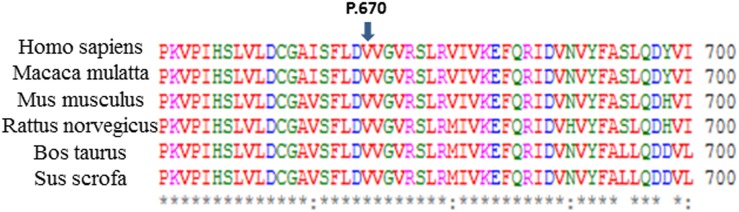
This variant was not found in 1,668 EVAS patients from our laboratory before this study, and the mutation frequency of c.2009T>C in this Xiamen’s cohort was 1.29% (2/155). We predicted the pathogenicity of this mutation by SIFT and Polyphen-2, and the results suggested “tolerant,” with a SIFT score of 0.05 and “possibly damaging” with a Polyphen-2 score of 0.873 by each. We made an alignment of the SLC26A4 amino acid sequence of six species, namely Homo sapiens (043511), Macaca mulatta (XP_001094049.1), Mus musculus (NP_035997.1), Rattus norvegicus (NP_062087.1), Bos taurus (XP_608706.3), and Sus scrofa (XP_003357559.1) (Fig 1), and the results suggested the evolutionary conservation of c.2009T>C. However, only two of 155 patients (1.29%) were found to carry the heterozygote of this variant in the present study; thus, a conclusion still cannot be reached.
Fig 1. Protein alignment showing conservation of residues GJB2 V670 across six species.
An alignment of the SLC26A4 amino acid sequence of six species suggested the evolutionary conservation of c.2009T>C (p.V670A).
mtDNA12SrRNA
Six patients (3.87%) carried a mtDNA12SrRNA mutation, all of which were the m.1555A>G homoplasmic mutation. Four patients had a clear history of aminoglycoside antibiotic use. Among them, one used gentamicin alone, one used streptomycin alone, one combined gentamicin and streptomycin, and one combined streptomycin and neomycin.
Discussion
GJB2
In this study, GJB2 mutations were detected in 27.1% (42/155) of all patients, with 12.9% (20/155) having two pathogenic mutations and 14.2% (22/155) having only one mutant allele. c.109G>A (p.V37I) and c.235delC were the hotspot mutations in the non-syndromic hearing loss (NSHL) patients in the Xiamen area, whereas the Caucasian hotspot mutation c.35delG [28,29] was not detected. Unlike other areas of China, c.235delC (8.39%) was not the most common GJB2 mutation, but rather c.109G>A, the allelic mutation frequency of which was 9.03% (28/310), indicating some features of GJB2 mutations in this area.
In East Asians, the c.109G>A (p.V37I) mutation is common: the frequency of this allele in the deaf population had been reported to be 4.3% in Thailand [30], 0.6% in Korea [31], 1.0% in Japan [32] and 4.2%(175/4162) in China [5]. Li reported that the frequency of c.109G>A mutation in newborns was 6.2% in Shanghai, China [12]. Given that some individuals with normal hearing also carry the homozygous c.109G>A mutation, there has been much controversy concerning its significance [33,34]. Recent research has shown that the hearing phenotypes of homozygous c.109G>A patients could be diverse in Chinese Han, and such patients may even show severe to profound hearing loss [35]. In our group, the four patients with the homozygous c.109G>A mutation had severe-to-profound hearing loss, the severity of which was similar to that of others in this cohort. In our study, the allele frequency of the c.109G>A mutation was 9.03% (28/310). Compared with the former data (4.2%, 175/4126) from the large Chinese deaf population evaluated by Dai [5], the frequency of the c.109G>A mutation in Xiamen was remarkably higher than that obtained in Dai’s results (P = 0.00). Because the c.109G>A mutation has been found in many countries in Southeast Asia, Oceania, East Asia, North Africa, Eastern Europe, and the Middle East, the complexity of its origin and migration should be considered. Furthermore, it will be worthwhile to study the founder effect and migration route in China based upon the large-sized samples from representative areas of China that could explain the significant differences in the frequency of c.109G>A among the studies of different Chinese deaf populations [36].
In East and Southeast Asia, c.235delC has been reported as the most common mutation acting as a frameshift mutation causing premature protein termination in hearing impaired patients, while lower frequencies were reported in Europe and Oceania [19–31]. In an earlier nationwide study by our group, Dai analyzed the GJB2 mutation of 2063 unrelated NSHL students from 23 different regions of China, the c.235delC mutation allele frequency was 12.34% (509/4,126)[5]. Compared with the 8.39% (26/310) c.235delC mutation allele frequency in the Xiamen area, the difference in the c.235delC mutation allele frequency was not significant (P = 0.064), reflecting a certain consistency of the c.235delC frequency between the Xiamen and entire nation. The shift in the c.235delC mutation from the most common to the second most common was a feature of the Xiamen deaf population that might indicate that, among the Xiamen aboriginals, the carrying rate of c.235delC was likely lower than the carrying rate of c.109G>A in Xiamen.
The c.512insAACG mutation was first reported by Dai; it is a frameshift mutation with a mutation allele frequency of 0.58% (12/2,063) in a Chinese population [5]. In our group, two patients were c.512insAACG compound heterozygotes with c.235delC and c.109G>A, respectively, resulting in a 0.65% (2/310) mutation allele frequency.
SLC26A4
Pendrin, a 780-amino acid protein, functions as a transmembrane anion exchanger and is encoded by SLC26A4. Over 100 mutations in the SLC26A4 (PDS) gene are involved in both Pendred syndrome (PS) and NSHL (DFNB4), showing specific differences among racial backgrounds. The mutation hot spots are p.T416P and c.IVS8+1G>A in Northern Europe [37], versus p.H723R and c. IVS7-2A>G in South Korea [19] and p.H723R in Japan [38]. It was reported by Dai that the most common Chinese SLC26A4 mutation is c.IVS7-2A>G, the mutation allele frequency reported in that study was 8.65% (566/6542)[8]. In our study, whole exons of SLC26A4 were sequenced, and the most common mutation in our Xiamen patient cohort was also c.IVS7-2A>G, the mutation allele frequency was 6.13% (19/310). The frequencies of c.IVS7-2A>G found in Xiamen’s deaf population and in the large Chinese deaf population evaluated by Dai [8] are not significantly different (P = 0.12).
c.1079C>T (p.A360V), the second most common mutation of SLC26A4 in the Xiamen patient cohort, was first reported in Taiwan by Lai et al. in 2007, with two compound heterozygous missense mutations involving a residue in a highly conserved domain of the eighth transmembrane region [20]. One of the patients in Taiwan with a compound heterozygous mutation of c.1079C>T and c.IVS7-2A>G was positive for both the perchlorate discharge test (PDT) and anti-thyroid peroxidase antibodies (anti-TPO Abs), suggestive of Pendred’s syndrome. This mutation has rarely been reported in other studies. In our group, there was one homozygous mutation and three compound heterozygous mutations of c.1079C>T and c.IVS7-2A>G, but none of the patients had thyroid dysfunction. The four patients were aged 17, 11, 15, and 18 years, respectively, and the onset ages of deafness were 2, 3, 2, and 3.4 years, respectively. Compared with the previous studies by Dai [7]and Guo [1] in China, c.1079C>T was not found in 647(135+514) patients and 167(50+117) normal control subjects. However, one study by Yuan [6] in China found only one heterozygote in their large cohort of 2,352 patients and none in the normal control group. The phenomenon of c.1079C>T mostly being found in Xiamen and Taiwan, but very rarely occurring in other areas, suggested the nature of the distribution of this mutation. Previous investigations of multiple regions of China did not include the Southern Fujian people, whose dialect is Hokkien (Southern Min). Hokkien is one of the eight main Chinese dialects that are popularly spoken in Taiwan and Xiamen. Historically, a proportion of Taiwan's population migrated from southern China (mostly from Xiamen and Quanzhou). This may partly explain why c.1079C>T has mostly been found in Xiamen and Taiwan; however, more samples from such areas will be needed to analyze the origin and migration of c.1079C>T.
c.2168A>G (p.H723R) is a common mutation in Japanese and Korean populations, with mutation allele frequencies of 4.1% and 10.34%[39–41], respectively. The c.2168A>G allele frequency was reported to be 1.51%(71/4704)in China [6]. In our report, the mutation allele frequency was 1.29% in the Xiamen area. The allele frequency of c.2168A>G in this study is consistent with the allele frequency of this mutation in Yuan’s study [6]. Our study suggested differences in the c.2168A>G frequency among countries and areas. Haplotype analyses in previous studies confirmed that c.2168A>G was a founder mutation in Japan, Korea and China, but the geographical environment and migration route may suggest explanations for the significant gradient distribution of c.2168A>G in these three East Asian countries [36].
mtDNA12SrRNA
Associated with aminoglycoside antibiotic-induced deafness [42], the mtDNA12SrRNA mutation shows variation by racial and geographic origins in populations with non-syndromic hearing loss, with a frequency of 0.6-2.5% in Caucasians [43–47], 2.4% in Danes [44], 1.8% in Turks [45], 0.7% in Germans, 1.8% in Hungarians, and 2.4% in Poles [43]. It also showed frequencies of 3% and 5.3% in Japanese and Indonesian deaf populations, respectively [44,45]. The m.1555A>G mutation is a common mutation of the mitochondrial 12SrRNA gene, shown to be the third most common mutation in China with a frequency of 3.43%[9]. In this study, the 3.87% (6/155) frequency of m.A1555G was close to that observed by Dai (3.43%).
Conclusions
In this study, the three most common deafness-associated genes were investigated by exon sequencing in a cohort of deaf patients recruited from Xiamen Special Education School. According to exon sequencing of GJB2, SLC26A4, and mtDNA12SrRNA, almost half of the deaf cases appeared to have a genetic etiology. Our data revealed special hotspots and spectra of mutations in the Xiamen deaf population, and this information will be helpful in designing the protocol for genetic testing for deafness and achieving an accurate molecular diagnosis in the Xiamen area.
Supporting Information
(DOCX)
Acknowledgments
We sincerely thank all of the subjects for their participation and cooperation in this study.
Data Availability
All relevant data are within the paper.
Funding Statement
This work was supported by a grant from the Minister of Science and Technology of China (2012BAI09B00), Chinese National Nature Science Foundation Research Grants (81230020, 81200751), State 863 High Technology R&D Key Project of China (2012AA020101), Postdoctoral Science Foundation Grant of China (2013M542450).
References
- 1. Guo YF, Liu XW, Guan J, Han MK, Wang DY, Zhao YL, et al. GJB2, SLC26A4 and mitochondrial DNA A1555G mutations in prelingual deafness in Northern Chinese subjects. Acta Otolaryngol. 2008;128(3):297–303. 10.1080/00016480701767382 [DOI] [PubMed] [Google Scholar]
- 2. Yuan Y, You Y, Huang D, Cui J, Wang Y, Wang Q, et al. Comprehensive molecular etiology analysis of nonsyndromic hearing impairment from typical areas in China. J Transl Med. 2009;7:79 10.1186/1479-5876-7-79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Xin F, Yuan Y, Deng X, Han M, Wang G, Zhao J, et al. Genetic mutations in nonsyndromic deafness patients of Chinese minority and Han ethnicities in Yunnan, China. J Transl Med. 2013;11:312 10.1186/1479-5876-11-312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dai P, Yu F, Han B, Yuan Y, Li Q, Wang G, et al. The prevalence of the 235delC GJB2 mutation in a Chinese deaf population. Genet Med. 2007;9(5):283–9. [DOI] [PubMed] [Google Scholar]
- 5. Dai P, Yu F, Han B, Liu X, Wang G, Li Q, et al. GJB2 mutation spectrum in 2,063 Chinese patients with nonsyndromic hearing impairment. J Transl Med. 2009;7:26 10.1186/1479-5876-7-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Yuan Y, Guo W, Tang J, Zhang G, Wang G, Han M, et al. Molecular epidemiology and functional assessment of novel allelic variants of SLC26A4 in non-syndromic hearing loss patients with enlarged vestibular aqueduct in China. PloS one. 2012;7(11):e49984 10.1371/journal.pone.0049984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dai P, Yuan Y, Huang D, Zhu X, Yu F, Kang D, et al. Molecular etiology of hearing impairment in Inner Mongolia: mutations in SLC26A4 gene and relevant phenotype analysis. J Transl Med. 2008;6:74 10.1186/1479-5876-6-74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dai P, Li Q, Huang D, Yuan Y, Kang D, Miller DT, et al. SLC26A4 c.919-2A>G varies among Chinese ethnic groups as a cause of hearing loss. Genet Med. 2008;10(8):586–92. [DOI] [PubMed] [Google Scholar]
- 9. Liu X, Dai P, Huang DL, Yuan HJ, Li WM, Cao JY, et al. Large-scale screening of mtDNA A1555G mutation in China and its significance in prevention of aminoglycoside antibiotic induced deafness. Zhonghua yi xue za zhi. 2006;86(19):1318–22. Chinese. [PubMed] [Google Scholar]
- 10. Chen J, Zheng H, Bei JX, Sun L, Jia WH, Li T, et al. Genetic structure of the Han Chinese population revealed by genome-wide SNP variation. Am J Hum Genet. 2009;85(6):775–85. 10.1016/j.ajhg.2009.10.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Xu S, Yin X, Li S, Jin W, Lou H, Yang L, et al. Genomic dissection of population substructure of Han Chinese and its implication in association studies. Am J Hum Genet. 2009;85(6):762–74. 10.1016/j.ajhg.2009.10.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Li L, Lu J, Tao Z, Huang Q, Chai Y, Li X, et al. The p.V37I exclusive genotype of GJB2: a genetic risk-indicator of postnatal permanent childhood hearing impairment. PloS one. 2012;7(5):e36621 10.1371/journal.pone.0036621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hwa HL, Ko TM, Hsu CJ, Huang CH, Chiang YL, Oong JL, et al. Mutation spectrum of the connexin 26 (GJB2) gene in Taiwanese patients with prelingual deafness. Genet Med. 2003;5(3):161–5. [DOI] [PubMed] [Google Scholar]
- 14. Yan D, Park HJ, Ouyang XM, Pandya A, Doi K, Erdenetungalag R, et al. Evidence of a founder effect for the 235delC mutation of GJB2 (connexin 26) in east Asians. Hum Genet. 2003;114(1):44–50. [DOI] [PubMed] [Google Scholar]
- 15. Ohtsuka A, Yuge I, Kimura S, Namba A, Abe S, Van Laer L, et al. GJB2 deafness gene shows a specific spectrum of mutations in Japan, including a frequent founder mutation. Hum Genet. 2003;112(4):329–33. [DOI] [PubMed] [Google Scholar]
- 16. Zainal SA, Md Daud MK, Abd Rahman N, Zainuddin Z, Alwi Z. Mutation detection in GJB2 gene among Malays with non-syndromic hearing loss. Int J Pediatr Otorhinolaryngol. 2012;76(8):1175–9. 10.1016/j.ijporl.2012.04.027 [DOI] [PubMed] [Google Scholar]
- 17. Park HJ, Shaukat S, Liu XZ, Hahn SH, Naz S, Ghosh M, et al. Origins and frequencies of SLC26A4 (PDS) mutations in east and south Asians: global implications for the epidemiology of deafness. J Med Genet. 2003;40(4):242–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wang QJ, Zhao YL, Rao SQ, Guo YF, Yuan H, Zong L, et al. A distinct spectrum of SLC26A4 mutations in patients with enlarged vestibular aqueduct in China. Clin Genet. 2007;72(3):245–54. [DOI] [PubMed] [Google Scholar]
- 19. Tsukamoto K, Suzuki H, Harada D, Namba A, Abe S, Usami S. Distribution and frequencies of PDS (SLC26A4) mutations in Pendred syndrome and nonsyndromic hearing loss associated with enlarged vestibular aqueduct: a unique spectrum of mutations in Japanese. Eur J Hum Genet. 2003;11(12):916–22. [DOI] [PubMed] [Google Scholar]
- 20. Lai CC, Chiu CY, Shiao AS, Tso YC, Wu YC, Tu TY, et al. Analysis of the SLC26A4 gene in patients with Pendred syndrome in Taiwan. Metabolism. 2007;56(9):1279–84. [DOI] [PubMed] [Google Scholar]
- 21. Huang S, Han D, Yuan Y, Wang G, Kang D, Zhang X, et al. Extremely discrepant mutation spectrum of SLC26A4 between Chinese patients with isolated Mondini deformity and enlarged vestibular aqueduct. J Transl Med. 2011;9:167 10.1186/1479-5876-9-167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Okamoto Y, Mutai H, Nakano A, Arimoto Y, Sugiuchi T, Masuda S, et al. Subgroups of enlarged vestibular aqueduct in relation to SLC26A4 mutations and hearing loss. Laryngoscope. 2014;124(4):E134–40. 10.1002/lary.24368 [DOI] [PubMed] [Google Scholar]
- 23. Hu H, Wu L, Feng Y, Pan Q, Long Z, Li J, et al. Molecular analysis of hearing loss associated with enlarged vestibular aqueduct in the mainland Chinese: a unique SLC26A4 mutation spectrum. J Hum Genet. 2007;52(6):492–7. [DOI] [PubMed] [Google Scholar]
- 24. Yang JJ, Tsai CC, Hsu HM, Shiao JY, Su CC, Li SY. Hearing loss associated with enlarged vestibular aqueduct and Mondini dysplasia is caused by splice-site mutation in the PDS gene. Hear Res. 2005;199(1–2):22–30. [DOI] [PubMed] [Google Scholar]
- 25. Choi BY, Stewart AK, Nishimura KK, Cha WJ, Seong MW, Park SS, et al. Efficient molecular genetic diagnosis of enlarged vestibular aqueducts in East Asians. Genet Test Mol Biomarkers. 2009;13(5):679–87. 10.1089/gtmb.2009.0054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nishio SY, Usami S. Deafness gene variations in a 1120 nonsyndromic hearing loss cohort: molecular epidemiology and deafness mutation spectrum of patients in Japan. Ann Otol Rhinol Laryngol. 2015;124 Suppl 1:49S–60S. 10.1177/0003489415575059 [DOI] [PubMed] [Google Scholar]
- 27. Choi BY, Stewart AK, Madeo AC, Pryor SP, Lenhard S, Kittles R, et al. Hypo-functional SLC26A4 variants associated with nonsyndromic hearing loss and enlargement of the vestibular aqueduct: genotype-phenotype correlation or coincidental polymorphisms? Hum Mutat. 2009;30(4):599–608. 10.1002/humu.20884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Van Laer L, Coucke P, Mueller RF, Caethoven G, Flothmann K, Prasad SD, et al. A common founder for the 35delG GJB2 gene mutation in connexin 26 hearing impairment. J Med Genet. 2001;38(8):515–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Gasparini P, Rabionet R, Barbujani G, Melchionda S, Petersen M, Brondum-Nielsen K, et al. High carrier frequency of the 35delG deafness mutation in European populations. Genetic Analysis Consortium of GJB2 35delG. Eur J Hum Genet. 2000;8(1):19–23. [DOI] [PubMed] [Google Scholar]
- 30. Wattanasirichaigoon D, Limwongse C, Jariengprasert C, Yenchitsomanus PT, Tocharoenthanaphol C, Thongnoppakhun W, et al. High prevalence of V37I genetic variant in the connexin-26 (GJB2) gene among non-syndromic hearing-impaired and control Thai individuals. Clin Genet. 2004;66(5):452–60. [DOI] [PubMed] [Google Scholar]
- 31. Han SH, Park HJ, Kang EJ, Ryu JS, Lee A, Yang YH, et al. Carrier frequency of GJB2 (connexin-26) mutations causing inherited deafness in the Korean population. J Hum Genet. 2008;53(11–12):1022–8. 10.1007/s10038-008-0342-7 [DOI] [PubMed] [Google Scholar]
- 32. Abe S, Usami S, Shinkawa H, Kelley PM, Kimberling WJ. Prevalent connexin 26 gene (GJB2) mutations in Japanese. J Med Genet. 2000;37(1):41–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Pollak A, Skorka A, Mueller-Malesinska M, Kostrzewa G, Kisiel B, Waligora J, et al. M34T and V37I mutations in GJB2 associated hearing impairment: evidence for pathogenicity and reduced penetrance. Am J Med Genet A. 2007;143A(21):2534–43. [DOI] [PubMed] [Google Scholar]
- 34. Gallant E, Francey L, Tsai EA, Berman M, Zhao Y, Fetting H, et al. Homozygosity for the V37I GJB2 mutation in fifteen probands with mild to moderate sensorineural hearing impairment: further confirmation of pathogenicity and haplotype analysis in Asian populations. Am J Med Genet A. 2013;161A(9):2148–57. 10.1002/ajmg.a.36042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Chai Y, Chen D, Sun L, Li L, Chen Y, Pang X, et al. The homozygous p.V37I variant of GJB2 is associated with diverse hearing phenotypes. Clin Genet. 2015;87(4):350–5. 10.1111/cge.12387 [DOI] [PubMed] [Google Scholar]
- 36. Tsukada K, Nishio SY, Hattori M, Usami S. Ethnic-Specific Spectrum of GJB2 and SLC26A4 Mutations: Their Origin and a Literature Review. Ann Otol Rhinol Laryngol. 2015;124 Suppl 1:61S–76S. 10.1177/0003489415575060 [DOI] [PubMed] [Google Scholar]
- 37. Campbell C, Cucci RA, Prasad S, Green GE, Edeal JB, Galer CE, et al. Pendred syndrome, DFNB4, and PDS/SLC26A4 identification of eight novel mutations and possible genotype-phenotype correlations. Hum Mutat. 2001;17(5):403–11. [DOI] [PubMed] [Google Scholar]
- 38. Park HJ, Lee SJ, Jin HS, Lee JO, Go SH, Jang HS, et al. Genetic basis of hearing loss associated with enlarged vestibular aqueducts in Koreans. Clin Genet. 2005;67(2):160–5. [DOI] [PubMed] [Google Scholar]
- 39. Usami S, Nishio SY, Nagano M, Abe S, Yamaguchi T, Deafness Gene Study C. Simultaneous screening of multiple mutations by invader assay improves molecular diagnosis of hereditary hearing loss: a multicenter study. PloS one. 2012;7(2):e31276 10.1371/journal.pone.0031276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Du W, Guo Y, Wang C, Wang Y, Liu X. A systematic review and meta-analysis of common mutations of SLC26A4 gene in Asian populations. Int J Pediatr Otorhinolaryngol. 2013;77(10):1670–6. 10.1016/j.ijporl.2013.07.023 [DOI] [PubMed] [Google Scholar]
- 41. Lee KY, Choi SY, Bae JW, Kim S, Chung KW, Drayna D, et al. Molecular analysis of the GJB2, GJB6 and SLC26A4 genes in Korean deafness patients. Int J Pediatr Otorhinolaryngol. 2008;72(9):1301–9. 10.1016/j.ijporl.2008.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Prezant TR, Agapian JV, Bohlman MC, Bu X, Oztas S, Qiu WQ, et al. Mitochondrial ribosomal RNA mutation associated with both antibiotic-induced and non-syndromic deafness. Nat Genet. 1993;4(3):289–94. [DOI] [PubMed] [Google Scholar]
- 43. Kupka S, Toth T, Wrobel M, Zeissler U, Szyfter W, Szyfter K, et al. Mutation A1555G in the 12S rRNA gene and its epidemiological importance in German, Hungarian, and Polish patients. Hum Mutat. 2002;19(3):308–9. [DOI] [PubMed] [Google Scholar]
- 44. OS E, Montserrat-Sentis B, Gronskov K, Brondum-Nielsen K. The A1555G mtDNA mutation in Danish hearing-impaired patients: frequency and clinical signs. Clin Genet. 2002;62(4):303–5. [DOI] [PubMed] [Google Scholar]
- 45. Tekin M, Duman T, Bogoclu G, Incesulu A, Comak E, Fitoz S, et al. Frequency of mtDNA A1555G and A7445G mutations among children with prelingual deafness in Turkey. Eur J Pediatr. 2003;162(3):154–8. [DOI] [PubMed] [Google Scholar]
- 46. Li R, Greinwald JH Jr., Yang L, Choo DI, Wenstrup RJ, Guan MX. Molecular analysis of the mitochondrial 12S rRNA and tRNASer(UCN) genes in paediatric subjects with non-syndromic hearing loss. J Med Genet. 2004;41(8):615–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Jacobs HT, Hutchin TP, Kappi T, Gillies G, Minkkinen K, Walker J, et al. Mitochondrial DNA mutations in patients with postlingual, nonsyndromic hearing impairment. Eur J Hum Genet. 2005;13(1):26–33. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
Data Availability Statement
All relevant data are within the paper.