Abstract
Background: Adolescents are long-standing tobacco prevention targets, given that smoking patterns typically originate before adulthood. Pediatric overweight/obesity remains at epidemic levels. Links between these two biobehavioral risks are not well understood, yet of keen public health and pediatric care relevance. The aims of the present study were to examine smoking behaviors and attitudes of overweight (OV), obese (OB), and severely obese (SO) adolescents, compared to healthy weight (HW), utilizing the nationally representative sample, Monitoring the Future.
Methods: Smoking behavior prevalence (ever, current, or age of initiation), perceived risk of harm, disapproval of others smoking, and peer smoking were determined for a pooled 2008–2009 sample of 19,678 10th graders (Mage=16.09±0.47 years) by CDC-defined BMI percentile-based categories within race/ethnic group (69.5% white, 14.5% African American, and 16.0% Hispanic). Logistic regression examined the impact of excess weight status on smoking behaviors and attitudes relative to HW.
Results: Relative to HW of same race/ethnicity, white or African American OV, OB, and SO had higher odds of recent smoking, with the highest prevalence among SO. For white youth, excess weight increased odds of ever smoking, early daily smoking (before grade 9), perceiving low risk of harm, and not disapproving of others smoking. Findings varied for African American or Hispanic youth.
Conclusions: As we move toward fostering a tobacco-free generation, youth whose weight exceeds healthy guidelines are high-risk targets for tobacco prevention messaging and close monitoring of cigarette use, particularly those who are severely obese as well as white youth of excess weight, starting before adolescence.
Introduction
Obesity and tobacco use are 2 of 10 “Winnable Battles” targeted by the CDC, given their profound morbidity and mortality risks, as well as the known prevention and intervention solutions for each. Concern is intensified when these two biobehavioral risks co-occur, with the all-cause mortality risk compounded 2.7- to 3.8-fold for the smoker who is also obese.1 Tobacco use typically onsets during adolescence, with prevalence rates increasing across the high school years.2 In fact, 9 of 10 adult smokers had their first cigarette before the age of 18.3 When smoking trajectories are tracked prospectively from adolescence into young adulthood (ages 12–28), clear patterns (e.g., abstainers, low users, and stable users) start to diverge as early as age 15.4,5 Links between adolescent-onset tobacco use and nicotine dependence6,7 further heightens the concern. As such, youth ages 12–17 are long-standing tobacco prevention targets that, in most recent years, have also emerged as a critical focus in obesity prevention efforts.
Encouragingly, tobacco prevention efforts having successfully reduced teen current (past 30 days) smoking rates since their peak in 1997 (i.e., reduction of 70% in 10th-grade students).2 However, during this same time period, rates of excess weight status in youth have reached epidemic levels, with rates of severe pediatric obesity continuing to rise.8 Further, as these “mirror image” trends have emerged, a small yet under-recognized body of literature suggests that youth of excess weight status may be a subgroup at greater risk for smoking behaviors (e.g., having ever smoked, smoking before the age of 13).9,10 Arguably, this makes sense given that adolescent health risk behaviors are known to cluster together. For example, contemporary data from Project EAT11 demonstrated that adolescents who smoked were also less likely to engage in other healthy lifestyle behaviors, such as participating in team sports, eating regular meals, and were more likely to consume fast food or soft drinks. Further, adolescents who want to lose weight may initiate smoking as a method of weight control.12 Examination of whether there are links between these two biobehavioral risks in adolescence is thus timely, of keen public health relevance, with potential clinical implications for clinical monitoring of pediatric patients whose weight exceeds healthy guidelines.
Considerable gaps in this developing literature exist, with several “next steps” needed to inform the testing of more explanatory models of these potential inter-relationships. For example, no studies to date have aimed to replicate previous findings while characterizing smoking across all pediatric excess weight status groups (overweight, obese, and severely obese) within one contemporary and nationally representative sample. This approach proves clinically relevant given that BMI cutpoints are often used as one criterion for referral or access to care (i.e., lifestyle modification programs and bariatric surgery programs) and from which unique risks for a specific weight status group can be identified. In addition, it is known that adolescents tend to associate with peers who engage in similar health risk behaviors and are influenced by what they perceive are the health risk beliefs and attitudes of their peer group.13 However, we lack an understanding of whether adolescent attitudes and beliefs about smoking (i.e., acceptability, health risks, and peer usage), often highlighted in prevention messaging, differ by weight status. Finally, previous literature has not considered known race/ethnic disparities in prevalence of obesity14 and substance use2 nor the differential impact of parental education and gender on both biobehavioral risks15 in their analytic strategy.
The aims of the present study were to examine cigarette smoking behaviors, attitudes about smoking, and perceptions of peer group cigarette smoking for adolescents of excess weight status (e.g., overweight, obese, and severely obese) relative to youth of healthy weight. To achieve this aim, a large (N=19,678) nationally representative sample of 10th-grade students (ages 14–17) was accessed from an ongoing epidemiological study of behaviors, attitudes, and values of adolescents in the United States, Monitoring the Future (MTF). Analyses were executed separately by race (white, African American, and Hispanic) and controlled for parental education and gender.
Methods
Study Design and Study Population
MTF is a national survey of behaviors and attitudes administered to adolescents (i.e., 8th, 10th, or 12th grade) in public and private schools and funded by the National Institute on Drug Abuse of the NIH. Study design, procedures, and the multistage random sampling process are described in detail elsewhere.16 MTF assigned each student a sampling weight to adjust for variations in selection probabilities occurring at each sampling stage (geographical, school, and students). The present study utilized pooled data from 10th graders in the 2008 and 2009 MTF annual surveys.17,18 The overall response rate for 10th-grade students (school response rate×participant response rate) was 84% in 200817 and 87% in 2009.18
Adolescent self-reported height and weight were obtained for a subsample of the pooled total sample (83.3%; n=26,517 of 31,838). Of this sample, participants with missing data for BMI percentile (9.2%) or with BMI values that were flagged by MTF as “biologically implausible” (i.e., too low or too high; 0.7%) based on the CDC criteria19 were excluded from analyses, leaving 23,882 participants. Given that the aims of the study were focused on the impact of excess weight, MTF participants who were underweight (<5th percentile, n=673 of 23,882; 2.8%) were excluded from the present analyses. Participants who did not identify themselves as either non-Hispanic white, non-Hispanic African American, or Hispanic (Mexican American, Chicano, Cuban American, Puerto Rican, or other Hispanic or Latino) were excluded from analyses (n=3,531 of 23,209;15.2%) owing to missing data or insufficient sample size for other racial/ethnic groups. This resulted in a final study N of 19,678 adolescents. The institutional review board at Cincinnati Children's Hospital (Cincinnati, OH) approved secondary data analysis of these MTF data.
Weight Status
Self-reported heights and weights were used to calculate BMI percentiles for age and gender. Healthy weight (5th–84th percentile), overweight (85th–94th percentile), and obese (95th–98th percentile) weight status groups were based on 2000 CDC criteria.19 The cutpoint for the severely obese weight status group was set at ≥99th percentile.20
Demographics
Adolescent self-reported demographic data included gender, age in years, and race (i.e., limited to white, African American, or Hispanic for the present study). Adolescents also reported their mother and/or fathers' highest level of education with the average value computed and scaled by MTF as follows: 1=grade school completion or less; 2=some high school; 3=high school completion; 4=some college; 5=college completion; and 6=graduate or professional school.
Dependent Variables
Cigarette smoking was assessed with two questions dichotomized to describe whether participants had ever smoked a cigarette or if they had smoked a cigarette in the past 30 days (hereafter referred to as “current”). Questions regarding grade of first cigarette and grade of first smoking daily were recoded as: 0=never; 1=before grade 9 (“early”); and −1=grades 9–10. For variables regarding attitudes about cigarette smoking and peer usage of cigarettes, questions were dichotomized such that greater risk was defined as participants endorsing low risk of harm (i.e., no risk, slight risk, or moderate risk) from smoking one or more packs of cigarettes per day; not disapproving of smoking one or more packs of cigarettes per day; endorsing that some, most, or all of one's friends smoke cigarettes; and endorsing that close friends do not disapprove of the participant smoking occasionally. These MTF variables have been shown to have adequate internal consistency, reliability, and predictive and discriminant validity across adolescence.21
Statistical Analysis
Mplus (version 7.11) was used to conduct all analyses and included survey sampling weights to adjust for the complicated survey design.22 Analyses were performed separately for white, African American, and Hispanic adolescents, with gender and parental education entered as covariates. Missing data for all analyses ranged between 2.7% and 13.3% across white, African American, and Hispanic adolescent groups and was handled by weighted least squares estimation in Mplus (WLSMV22). To evaluate the effect of weight status (overweight, obese, and severely obese vs. healthy weight) on each outcome variable, logistic regression analyses were used to obtain odds ratios (ORs) and bootstrapping procedures were used to obtain 95% confidence intervals (CIs). The false discovery rate procedure23 was used to control family-wise type I error across two distinct outcome domains (self-reported use; attitudes and peer use) for white, African American, or Hispanic adolescents.
Results
Sample Characteristics
Adolescent demographic data, weight status group, and cigarette smoking prevalence by race/ethnicity are presented in Table 1. The sample was 53% female and approximately 16 years of age. Hispanic youth had the highest rates of having tried a cigarette by their 10th-grade year, although whites had the highest rates of having smoked in the past 30 days. African American adolescents had the lowest rates of both smoking behaviors.
Table 1.
Demographic Characteristics and Smoking Behaviors of Study Sample (n=19,678) of 10th-Grade Students after Excluding Underweight Adolescents (Monitoring the Future 2008, 2009)
| Characteristic | White (n=13,679) | African American (n=2859) | Hispanic (n=3140) | Total (N=19,678) |
|---|---|---|---|---|
| % BMI categories | ||||
| Healthy (5th–84th percentile) | 75.3 | 63.9 | 67.8 | 72.5 |
| Overweight (85th–94th percentile) | 14.0 | 19.4 | 17.5 | 15.3 |
| Obese (95th–98th percentile) | 8.8 | 13.3 | 12.1 | 10.0 |
| Severely obese (≥99th percentile) | 1.9 | 3.5 | 2.6 | 2.2 |
| % female | 52.5 | 54.9 | 53.5 | 53.0 |
| Mean age (SD) in years | 16.09 (0.43) | 16.15 (0.57) | 16.06 (0.52) | 16.09 (0.47) |
| Modal parental educationa | 4 | 3 | 1 | 4 |
| Ever smoked cigarettesb, % | 32.2 | 25.3 | 37.2 | 32.0 |
| Smoked in the past 30 daysc, % | 14.4 | 6.2 | 11.8 | 12.8 |
Missing data for 4.9% of the sample. 1=grade school completion or less; 2=some high school; 3=high school completion; 4=some college; 5=college completion; and 6=graduate or professional school.
Missing data for 2.0%.
Missing data for 2.1%.
SD, standard deviation.
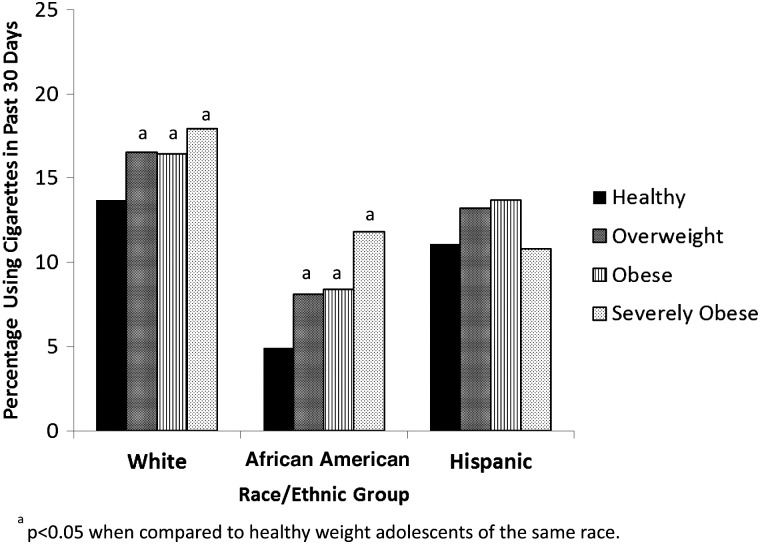
Weight Status and Cigarette Smoking
The associations between weight status group and cigarette smoking were examined after adjusting for demographic covariates (i.e., gender and parental education). Prevalence data and ORs by weight status for each race/ethnicity group are presented in Table 2. Compared to healthy weight adolescents of the same race/ethnicity, white adolescents in all excess weight groups, overweight African American, and obese Hispanic adolescents had higher odds of reporting ever smoking in their lifetime. In addition, white and African American adolescents in all excess weight groups were more likely to report current smoking. As seen in Figure 1, white adolescents, regardless of weight status, reported the highest rates of current cigarette smoking. Within each racial/ethnic group, current smoking was highest among severely obese white and African American adolescents, but lowest for severely obese Hispanic adolescents.
Table 2.
Prevalence and ORs of Cigarette Smoking Behaviors and Attitudes for White, African American, or Hispanic 10th-Grade Students (Monitoring the Future, 2008, 2009) by Weight Status Group
| Healthy | Overweight | Obese | Severely obese | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| White | % | % | OR | 95% CI | % | OR | 95% CI | % | OR | 95% CI |
| Cigarettes | ||||||||||
| Ever smoked cigarettes | 30.8 | 35.6 | 1.16* | 1.10–1.23 | 36.6 | 1.17* | 1.10–1.25 | 41.6 | 1.36* | 1.22–1.53 |
| Cigarette use in past 30 days | 13.7 | 16.5 | 1.15* | 1.09–1.21 | 16.4 | 1.12* | 1.02–1.22 | 17.9 | 1.27* | 1.08–1.48 |
| Early grade (<grade 9) of first use | ||||||||||
| Smoke first cigarette | 17.7 | 22.1 | 1.14* | 1.01–1.29 | 26.5 | 1.47* | 1.29–1.67 | 28.0 | 1.23 | 0.96–1.57 |
| Smoke daily | 4.2 | 6.1 | 1.27* | 1.04–1.51 | 7.5 | 1.41* | 1.18–1.73 | 9.4 | 1.59* | 1.02–2.21 |
| Attitudes and peer use | ||||||||||
| Low risk of harm from smoking ≥1 packs per day | 25.1 | 30.9 | 1.15* | 1.07–1.24 | 31.4 | 1.19* | 1.10–1.29 | 32.4 | 1.35* | 1.14–1.59 |
| Don't disapprove of smoking ≥1 packs per day | 12.0 | 14.4 | 1.10* | 1.01–1.19 | 17.5 | 1.28* | 1.15–1.43 | 20.2 | 1.54* | 1.23–1.92 |
| Some, most, or all of friends smoke cigarettes | 34.4 | 37.4 | 1.09 | 0.99–1.20 | 38.7 | 1.14* | 1.03–1.25 | 41.6 | 1.19 | 0.95–1.49 |
| Friends don't disapprove of smoking occasionally | 24.0 | 28.0 | 1.15 | 0.97–1.37 | 25.8 | 1.03 | 0.86–1.24 | 39.3 | 1.77* | 1.21–2.59 |
| African American | % | % | OR | 95% CI | % | OR | 95% CI | % | OR | 95% CI |
|---|---|---|---|---|---|---|---|---|---|---|
| Cigarettes | ||||||||||
| Ever smoked cigarettes | 23.7 | 29.9 | 1.20* | 1.06–1.35 | 24.7 | 0.98 | 0.83–1.15 | 31.2 | 1.18 | 0.89–1.58 |
| Cigarette use in past 30 days | 4.9 | 8.1 | 1.28* | 1.07–1.53 | 8.4 | 1.33* | 1.07–1.66 | 11.8 | 1.55* | 1.10–2.18 |
| Early grade (<grade 9) of first use | ||||||||||
| Smoke first cigarette | 15.5 | 21.3 | 1.09 | 0.83–1.41 | 16.0 | 1.06 | 0.79–1.81 | 18.4 | 0.67 | 0.44–1.27 |
| Smoke daily | 1.7 | 2.9 | 1.29 | 0.71–1.94 | 2.3 | 0.73 | 0.40–1.17 | 4.4 | 0.76 | 0.01–1.51 |
| Attitudes and peer use | ||||||||||
| Low risk of harm from smoking ≥1 packs per day | 27.6 | 25.7 | 0.90 | 0.80–1.02 | 26.5 | 0.88 | 0.74–1.04 | 17.4 | 0.72* | 0.58–0.88 |
| Don't disapprove of smoking ≥1 packs per day | 8.7 | 10.4 | 1.09 | 0.93–1.26 | 12.1 | 1.21 | 0.99–1.51 | 17.6 | 1.67* | 1.30–2.21 |
| Some, most, or all of friends smoke cigarettes | 24.9 | 23.5 | 0.97 | 0.81–1.16 | 27.2 | 1.02 | 0.83–1.27 | 39.1 | 1.44* | 1.09–1.90 |
| Friends don't disapprove of smoking occasionally | 13.8 | 20.4 | 1.31 | 0.96–1.79 | 25.4 | 1.32 | 0.78–2.22 | 12.5 | 0.66 | 0.06–7.73 |
| Hispanic | % | % | OR | 95% CI | % | OR | 95% CI | % | OR | 95% CI |
|---|---|---|---|---|---|---|---|---|---|---|
| Cigarettes | ||||||||||
| Ever smoked cigarettes | 35.5 | 41.3 | 1.13 | 1.01–1.26 | 41.8 | 1.20* | 1.05–1.38 | 35.4 | 1.02 | 0.76–1.37 |
| Cigarette use in past 30 days | 11.1 | 13.2 | 1.09 | 0.97–1.23 | 13.7 | 1.12 | 0.96–1.30 | 10.8 | 0.96 | 0.66–1.41 |
| Early grade (<grade 9) of first use | ||||||||||
| Smoke first cigarette | 23.4 | 26.4 | 0.92 | 0.78–1.15 | 28.9 | 1.07 | 0.89–1.40 | 20.3 | 0.86 | 0.41–1.51 |
| Smoke daily | 4.4 | 4.4 | 0.92 | 0.65–1.33 | 6.6 | 1.03 | 0.65–1.60 | 5.2 | 0.93 | 0.01–2.60 |
| Attitudes and peer use | ||||||||||
| Low risk of harm from smoking ≥1 packs per day | 31.2 | 33.0 | 1.11 | 1.00–1.24 | 32.5 | 1.05 | 0.86–1.28 | 43.9 | 1.35 | 0.93–1.96 |
| Don't disapprove of smoking ≥1 packs per day | 11.7 | 11.3 | 0.94 | 0.74–1.20 | 12.7 | 1.14 | 0.92–1.45 | 22.2 | 1.77* | 1.33–2.62 |
| Some, most, or all of friends smoke cigarettes | 36.7 | 30.0 | 0.98 | 0.73–0.97 | 39.4 | 1.10 | 0.93–1.31 | 43.8 | 1.27 | 0.88–1.84 |
| Friends don't disapprove of smoking occasionally | 20.4 | 20.2 | 0.88 | 0.67–1.17 | 25.0 | 1.20 | 0.89–1.61 | 33.3 | 1.33 | 0.66–2.66 |
Weight status groups are defined using % BMI categories as follows: healthy (5th–84th percentile); overweight (85th–94th percentile); obese (95th–98th percentile); and severely obese (≥99th percentile).
p<0.05.
OR, odds ratio; CI, confidence interval.
Figure 1.
Cigarette use in the past 30 days for 10th-grade students (Monitoring the Future 2008, 2009) by race and weight status group.
Grade of First Smoking Behavior
The ORs for early initiation (i.e., before grade 9) of cigarette smoking by weight status for each racial/ethnic group are presented in Table 2. Adolescents who responded “never” to these questions were excluded from the following analyses. Relative to healthy weight white adolescents, overweight and obese white adolescents had significantly higher odds of early initiation of ever smoking (Table 2). In addition, overweight, obese, and severely obese white adolescents had significantly higher odds of reporting daily smoking before grade 9. No significant associations were identified for African American or Hispanic adolescents.
Attitudes Regarding Cigarette Smoking and Perceived Peer Smoking
The associations of weight status group with attitudes regarding cigarette smoking and perceptions of peer cigarette smoking for each racial/ethnic group were examined after adjusting for covariates (Table 2). Across excess weight status groups, white adolescents had significantly higher odds of endorsing attitudes such as a low risk of harm and a lack of disapproval of others smoking one or more packs per day, compared to healthy weight white adolescents. Obese white adolescents also were significantly more likely to report having some, most, or all of their friends smoke. Finally, severely obese whites had significantly higher odds of believing that their friends would not disapprove of their smoking. Relative to healthy weight youth of the same racial/ethnic group, severely obese African American adolescents were less likely to perceive low risk in smoking one or more packs per day (i.e., they recognized health risk). In contrast, they had significantly higher odds of not disapproving of smoking in others as well as reporting that a majority of their friends smoke. Relative to healthy weight Hispanic adolescents, severely obese Hispanic adolescents had significantly higher odds of not disapproving of others smoking one or more packs per day.
Discussion
Current cigarette smoking for 10th-grade students in the United States was more prevalent among those whose weight exceeded healthy guidelines (BMI ≥85th percentile), with unique patterns emerging based on race/ethnicity and degree of excess weight. Specifically, current cigarette smoking was significantly more prevalent among white and African American adolescents across the entire excess weight spectrum (e.g., overweight, obese, and severely obese) than among same race adolescents of healthy weight.
Several additional distinctive risks emerged for white adolescents with excess weight. Relative to those of healthy weight, excess weight increased the odds of an adolescent ever having smoked and greater odds of their first smoke being in the eighth grade or younger. Further, excess weight increased the odds for white teens to endorse risky attitudes about smoking (e.g., perception of low risk of harm of smoking or lack of disapproval of others smoking more than a pack a day) and for some excess weight groups, the likelihood they associated with peers who also smoked or whom they believed would not disapprove of their smoking. Findings were more variable among African American or Hispanic adolescents, and at times, quite different. For example, for African American youth, only overweight adolescents (i.e., not obese or severely obese) were significantly more likely to have ever smoked.
It may be argued that the present effect sizes (i.e., ORs) were not large. Further, the majority of adolescent smokers in the present MTF sample were of healthy weight, given that healthy weight individuals represent the largest portion of the sample (73%). However, these data demonstrate that the percentage of early adolescents who carry two potentially damaging health risk factors (i.e., excess weight and smoking) is cause for concern and cannot be ignored. Current trends indicate that the majority of obese teens, particularly those who are severely obese, will remain obese as adults.24 Thus, while we move toward making the next generation one that is tobacco free, we have an emerging adult generation with compounding morbidity and mortality risks if their excess weight status persists and they also smoke.
Early smoking initiation alone is known to increase risks for concurrent use or progression to use/abuse other substances as well as nicotine dependence.5–7 Longitudinal studies are thus imperative to elucidate these and other (i.e., alcohol, marijuana, and illicit substances) health risk behavior pathways and their inter-relations with excess weight status in today's youth as they mature into adulthood. This is not to suggest that longitudinal studies are nonexistent. Rather, important work based on youth of previous generations underscores the importance of the current findings and call for future work. For example, Huang and colleagues accessed data from children (offspring) of females in the 1979 National Longitudinal Survey of Youth, finding that youth who were chronically obese, while less likely to smoke, showed a greater increase in smoking than youth who maintained a healthy weight.25 Further, in all youth (independent of weight), smoking and marijuana use increased obesity risk in the transition from adolescence to young adulthood.26
The present study also lends further support to the importance of the consideration of health disparities in obesity and tobacco use, as well as their potential downstream consequences. For example, epidemiological surveillance indicates that African American youth may have the lowest smoking rates, yet in adulthood, African American smoking rates surpass that of whites. Noting largely nonsignificant findings for Hispanic teens does not suggest that excess weight and smoking are not significant public health problems for Hispanic adolescents. Rather, weight status does not appear to compound smoking risks for Hispanic youth, which is in contrast to white and African American adolescents, and may suggest that the etiology of these risk factors differs for Hispanic youth. Moreover, the MTF Hispanic classification is broad and includes adolescents of different historical or cultural backgrounds. Conceivably, some of the inconsistent or lack of significant findings for Hispanic adolescents may reflect greater variation within that race/ethnic group27 or lower statistical power (e.g., weight group subsample size).
The results of the current study suggest that youth who carry excess weight, particularly white youth before adolescence, are high-risk targets for discussions regarding tobacco use and the associated health risks. It is widely accepted that pediatric care providers are uniquely positioned to monitor and assess patient's smoking risk and history in the context of routine care. However, as demonstrated by recent data published from the 2011 National Youth Tobacco Survey, the majority of adolescents (67.8%), including those who self-identified as being current smokers, reported no discussion or advice about tobacco use with any healthcare provider within the past year (i.e., doctor, nurse, or dentist).28 Providers within pediatric weight management programs, including bariatric surgery programs, should screen for tobacco use, be primed with prevention messaging, and be prepared with referral sources for those who have initiated smoking to help them quit. The CDC's “Talking to teens about tobacco use” aimed at pediatric providers, provides helpful tips, topics, and how to dispel myths with facts regarding tobacco use3 (see www.cdc.gov/tobacco/data_statistics/sgr/2012/pdfs/physician_card508.pdf).
Future Directions and Limitations
Understanding why smoking behaviors and excess weight status are linked in today's adolescents is a critically important area for future research, although the relationships are likely complex and multifactorial given the existing literature. For example, adolescent smoking behavior is known to be a peer group phenomenon, whether owing to conformity or through friendship choices.29,30 Further, adolescents who are socially isolated are more likely to smoke relative to others more embedded in the social network structure.31 It is widely accepted that adolescents who are overweight/obese, while not friendless, are more socially marginalized. It may be that as excess weight status increases, teens may have fewer friendship options and choose similarly marginalized peers, compounding peer-based influences for greater smoking behavior risks. These social contexts that promote cigarette smoking have been shown to have more impact on white adolescent smoking than for African American or Hispanic youth.32 In addition to social contexts, family context factors, be it heritability,33,34 or shared environment, such as parental/sibling smoking and parental/sibling obesity,35–37 are also known independent contributors to adolescent smoking or obesity risk.
Adolescent smoking behaviors have also long been associated with adolescent weight concerns and dieting.12,38 As such, adolescents of excess weight status may be smoking because they believe it will help them better manage their weight. Alternately, if they do smoke, they may believe quitting may lead to further weight gain, despite that links between smoking cessation and weight gain remaining a “conundrum.”39 For example, nicotine can suppress appetite, but there is also evidence that it enhances food reinforcement.40 Further, smoking also has a marked effect on the diversity of microbes in the gut microbiota,41 which, in turn, is associated with a gut metagenomic profile characteristic of obesity.42 Another avenue for further investigation may involve their level of physical activity and/or sedentary behavior, known correlates of both smoking and obesity.11,43,44 These aforementioned factors in addition to others (e.g., pubertal timing,45 psychological disinhibition/reward-seeking behavior,46,47 and depression48–50) illustrate the complexity of the shared behavioral and or physiological processes that may bind smoking and obesity together and are in need further exploration. Finally, longitudinal research that examines how these factors are linked temporally is critical.
The present findings must be interpreted within the context of several limitations. First, these data are cross-sectional, with temporal sequencing of the development of excess weight and smoking behaviors unknown. Longitudinal research is critical to elucidate developmental trajectories of weight and smoking behaviors (e.g., initiation, abstainers, infrequent smokers, daily smokers, and stable users) and paths to nicotine dependence, which, based on the present findings (e.g., age of first smoke), should begin before the eighth grade. Whereas this study focused on the most prevalent racial/ethnic groups in the United States (white, African American, and Hispanic), other groups were excluded owing to insufficient sample sizes when grouped by weight status. Future research should explore the associations of excess weight status and smoking behaviors by sex within racial/ethnic groups given that trends and potential prevention targets may be unique for males and females. Finally, MTF surveillance is limited to those adolescents attending high school and is therefore not fully representative of this age group.
Although this article is the first in the literature to characterize smoking behaviors and attitudes across all pediatric excess weight status groups (overweight, obese, and severely obese) within one large, contemporary sample, comparison and/or replication of the present findings with other data sources should consider the following. MTF methodology includes self-reported heights and weights from which BMI percentile-based categorization of weight status groups were determined. Whereas other large epidemiological studies have shown a high correlation between self-reports and actual measured values,51 it is also known that adolescent self-report may underestimate weight and overestimate height. As such, the present findings may actually underestimate the extent of excess weight in the MTF sample. MTF also flagged BMI values considered “biologically implausible” based on CDC guidelines. Though it is understandably necessary to set parameters to exclude implausible data in epidemiological surveillance, what was deemed implausible in 2000 might indeed be possible in this more contemporary cohort surveyed in 2008–2009. Therefore, the present study was limited in being able to fully characterize what may have been the most upper extremes of severe obesity in this MTF sample. However, the present data considerably expand the BMI window from our previous work with the 2007 Youth Risk Behavior Surveillance System (YRBSS) surveillance,10 where publically released data parameters for implausible BMI values were set at 55 kg/m2. Finally, to be consistent with our 2007 YRBSS report, a BMI value ≥99th percentile for age and gender was utilized as the cutpoint to define the severely obese group. We recognize that new nomenclature and severe obesity metrics (i.e., “percentage of the 95th percentile”) are growing in acceptance to refine the classification of the 99th percentile to more accurately track BMI percentile changes over time in youth who are severely obese and allow further delineation of severely obese subgroups.8,52,53 Post-hoc examination of the present sample indicates that the 99th percentile represents approximately the 130% of the 95th percentile, suggesting that the present severe obesity cutpoint is indeed conservative.
Conclusions
The noted declines in smoking rates in the United States are highly encouraging. However, the present data suggest evidence of two potentially inter-related pediatric biobehavioral risks and an emerging public health issue as the current generation of youth matures into adulthood. Tobacco and obesity prevention efforts should comprehensively endorse the range of health-promoting behaviors (e.g., not smoking, healthy eating, and being physically active) as being the peer group norm. Depicting youth of excess weight status in print and television prevention ad campaigns will aid in dispelling the myth that teens who smoke are thinner than those who do not smoke. Finally, this is a fertile area for research, with BMI or weight status an important consideration in future epidemiological monitoring. Comprehensive prospective studies aimed at understanding tobacco and obesity risk pathways are of vital importance to ensure the best health outcomes for the next generation of youth.
Acknowledgments
This article uses data from the Monitoring the Future Study, which is supported by grants from the National Institute on Drug Abuse (R01DA001411 and R01DA016575). Dr. Zeller's effort was supported by grants from the NIH (R01DK080020 and R01DA033415). Dr. Wu was supported by an NIH training grant (T32HD068223). Dr. Becnel also was supported by an NIH training grant (T32DK063929).
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Freedman DM, Sigurdson AJ, Rajaraman P, et al. . The mortality risk of smoking and obesity combined. Am J Prev Med 2006;31:355–362 [DOI] [PubMed] [Google Scholar]
- 2.Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future national results of drug use: 2012 overview, key findings on adolescent drug use. Institute for Social Research, The University of Michigan: Ann Arbor, MI, 2013. [Google Scholar]
- 3.Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General. US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office of Smoking and Health: Atlanta, GA, 2012 [PubMed] [Google Scholar]
- 4.Riggs NR, Chou CP, Li C, et al. . Adolescent to emerging adulthood smoking trajectories: when do smoking trajectories diverge, and do they predict early adulthood nicotine dependence? Nicotine Tob Res 2007;9:1147–1154 [DOI] [PubMed] [Google Scholar]
- 5.Nelson SE, Van Ryzin MJ, Dishion TJ. Alcohol, marijuana, and tobacco use trajectories from age 12 to 24 years: Demographic correlates and young adult substance use problems. Dev Psychopathol 2015:27:253–257 [DOI] [PubMed] [Google Scholar]
- 6.Dierker L, Swendsen J, Rose J, et al. ,; Tobacco Etiology Research Network (TERN). Transitions to regular smoking and nicotine dependence in the Adolescent National Comorbidity Survey (NCS-A). Ann Behav Med 2012;43:394–401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Apelberg BJ, Corey CG, Hoffman AC, et al. . Symptoms of tobacco dependence among middle and high school tobacco users: Results from the 2012 national youth tobacco survey. Am J Prev Med 2014;47(2 Suppl 1):S4–S14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Skinner AC, Skelton JA. Prevalence and trends in obesity and severe obesity among children in the United States, 1999–2012. JAMA Pediatr 2014;168:561–566 [DOI] [PubMed] [Google Scholar]
- 9.Farhat T, Iannotti RJ, Simons-Morton BG. Overweight, obesity, youth, and health-risk behaviors. Am J Prev Med 2010;38:258–267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Benoit Ratcliff M, Jenkins TM, Reiter-Purtill J, et al. . Risk-taking behaviors of adolescents with extreme obesity: Normative or not? Pediatrics 2011;127:827–834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Larson NI, Story M, Perry CL, et al. . Are diet and physical activity patterns related to cigarette smoking in adolescents? Findings from Project EAT. Prev Chronic Dis 2007;4:A51. [PMC free article] [PubMed] [Google Scholar]
- 12.Cawley J, Markowitz S, Tauras J. Lighting up and slimming down: The effects of body weight and cigarette prices on adolescent smoking initiation. J Health Econ 2004;23:293–311 [DOI] [PubMed] [Google Scholar]
- 13.La Greca AM, Bearman KJ, Moore H. Peer relations of youth with pediatric conditions and health risks: Promoting social support and healthy lifestyles. J Dev Behav Pediatr 2002;23:271–280 [DOI] [PubMed] [Google Scholar]
- 14.Wang CY, Gortmaker S, Taveras EM. Trends and racial/ethnic disparities in severe obesity among US children and adolescents, 1976–2006. Inter J Pediatr Obes 2011;6:12–20 [DOI] [PubMed] [Google Scholar]
- 15.Bachman JG, O'Malley PM, Johnston LD, et al. . Racial/ethnic differences in the relationship between parental education and substance use among U.S. 8th-, 10th-, and 12th-grade students: Findings from the Monitoring the Future project. J Alcohol Drugs 2011;72:279–285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bachman JG, Johnston LD, O'Malley PM, et al. . The Monitoring the Future project after thirty-seven years: Design and procedures. Institute for Social Research, The University of Michigan: Ann Arbor, MI, 2011. [Google Scholar]
- 17.Johnston LD, O'Malley PM, Bachman JG, et al. . Monitoring the Future National Survey Results on Drug Use, 1975–2008: Volume I, Secondary School Students (NIH publication no. 09-7402). National Institute on Drug Abuse: Bethesda, MD, 2009. [Google Scholar]
- 18.Johnston LD, O'Malley PM, Bachman JG, et al. . Monitoring the Future National Survey Results on Drug Use, 1975–2009: Volume I, Secondary School Students (NIH publication no. 10-7584). National Institute on Drug Abuse: Bethesda, MD, 2010. [Google Scholar]
- 19.National Center for Health Statistics. 2000 CDC growth charts: United States. 2015. Available at www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm Last accessed July1, 2014
- 20.Skelton JA, Cook SR, Auinger P, et al. . Prevalence and trends of severe obesity among US children and adolescents. Acad Pediatr 2009;9:322–329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Johnston L, O'Malley P, Bachman J, et al. . Monitoring the Future national results on adolescent drug use: Overview of key findings, 2010. Institute for Social Research, The University of Michigan: Ann Arbor, MI, 2011. [Google Scholar]
- 22.Mplus User's Guide, seventh edition [computer program]. Muthen & Muthen: Los Angeles, CA, 1998–2012 [Google Scholar]
- 23.Benjamini Y. Discovering the false discovery rate. J R Stat Soc B 2010;72:405–416 [Google Scholar]
- 24.Merten MJ. Weight status continuity and change from adolescence to young adulthood: Examining disease and health risk conditions. Obesity (Silver Spring) 2010;18:1423–1428 [DOI] [PubMed] [Google Scholar]
- 25.Huang DY, Lanza HI, Wright-Volel K, et al. . Developmental trajectories of childhood obesity and risk behaviors in adolescence. J Adolesc 2013;36:139–148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Huang DY, Lanza HI, Anglin MD. Association between adolescent substance use and obesity in young adulthood: A group-based dual trajectory analysis. Addict Behav 2013;38:2653–2660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wallace JM, Jr., Bachman JG, O'Malley PM, et al. . Tobacco, alcohol, and illicit drug use: Racial and ethnic differences among U.S. high school seniors, 1976–2000. Public Health Rep 2002;117(Suppl 1):S67–S75 [PMC free article] [PubMed] [Google Scholar]
- 28.Schauer GL, Agaku IT, King BA, et al. . Health care provider advice for adolescent tobacco use: Results from the 2011 National Youth Tobacco Survey. Pediatrics 2014;134:446–455 [DOI] [PubMed] [Google Scholar]
- 29.Kelly AB, O'Flaherty M, Connor JP, et al. . The influence of parents, siblings and peers on pre and early teen smoking: A multilevel model. Drug and Alcohol Rev 2011;30:381–387 [DOI] [PubMed] [Google Scholar]
- 30.Schaefer DR, Haas SA, Bishop NJ. A dynamic model of US adolescents' smoking and friendship networks. Am J Public Health 2012;102:e12–e18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Seo DC, Huang Y. Systematic review of social network analysis in adolescent cigarette smoking behavior. J Sch Health 2012;82:21–27 [DOI] [PubMed] [Google Scholar]
- 32.Griesler PC, Kandel DB. Ethnic differences in correlates of adolescent cigarette smoking. J Adolesc Health 1998;23:167–180 [DOI] [PubMed] [Google Scholar]
- 33.Lessov-Schlaggar CN, Kristjansson SD, Bucholz KK, et al. . Genetic influences on developmental smoking trajectories. Addiction 2012;107:1696–1704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McCarthy MI. Genomics, type 2 diabetes, and obesity. N Engl J Med 2010;363:2339–2350 [DOI] [PubMed] [Google Scholar]
- 35.Vuolo M, Staff J. Parent and child cigarette use: A longitudinal, multigenerational study. Pediatrics 2013;132:e568–e577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mahabee-Gittens EM, Xiao Y, Gordon JS, et al. . The role of family influences on adolescent smoking in different racial/ethnic groups. Nicotine Tob Res 2012;14:264–273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Martinson BC, VazquezBenitez G, Patnode CD, et al. . Obesogenic family types identified through latent profile analysis. Ann Behav Med 2011;42:210–220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Potter BK, Pederson LL, Chan SS, et al. . Does a relationship exist between body weight, concerns about weight, and smoking among adolescents? An integration of the literature with an emphasis on gender. Nicotine Tob Res 2004;6:397–425 [DOI] [PubMed] [Google Scholar]
- 39.Flegal KM. The conundrum of smoking cessation and weight gain. 2012;54:193–194 [DOI] [PubMed] [Google Scholar]
- 40.Donny EC, Caggiula AR, Weaver MT, et al. . The reinforcement-enhancing effects of nicotine: Implications for the relationship between smoking, eating and weight. Physiol Behav 2011;104:143–148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Biedermann L, Brulisauer K, Zeitz J, et al. . Smoking cessation alters intestinal microbiota: Insights from quantitative investigations on human fecal samples using FISH. Inflamm Bowel Dis 2014;20:1496–1501 [DOI] [PubMed] [Google Scholar]
- 42.Ridaura VK, Faith JJ, Rey FE, et al. . Gut microbiota from twins discordant for obesity modulate metabolism in mice. Science 2013;341:1241214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kaufman A, Augustson EM, Patrick H. Unraveling the relationship between smoking and weight: The role of sedentary behavior. J Obes 2012:735465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Boutelle K, Neumark-Sztainer D, Story M, et al. . Weight control behaviors among obese, overweight, and nonoverweight adolescents. J Pediatr Psychol 2002;27:531–540 [DOI] [PubMed] [Google Scholar]
- 45.Tanner-Smith EE. Negotiating the early developing body: Pubertal timing, body weight, and adolescent girls substance use. J Youth Adolesc 2010;39:1402–1416 [DOI] [PubMed] [Google Scholar]
- 46.Tarter RE, Kirisci L, Reynolds M, et al. . Neurobehavior disinhibition in childhood predicts suicide potential and substance use disorder by young adulthood. Drug Alcohol Depend 2004;76(Suppl 1):S45–S52 [DOI] [PubMed] [Google Scholar]
- 47.Reynolds B, Fields S. Delay discounting by adolescents experimenting with cigarette smoking. Addiction 2012;107:417–424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Prinstein MJ, La Greca AM. Childhood depressive symptoms and adolescent cigarette use: A six-year longitudinal study controlling for peer relations correlates. Health Psychol 2009;28:283–291 [DOI] [PubMed] [Google Scholar]
- 49.Windle M, Windle RC. Depressive symptoms and cigarette smoking among middle adolescents: Prospective associations and intrapersonal and interpersonal influences. J Consult Clin Psych 2001;69:215–226 [PubMed] [Google Scholar]
- 50.Anderson SE, Murray DM, Johnson CC, et al. . Obesity and depressed mood associations differ by race/ethnicity in adolescent girls. Inter J Pediatr Obes 2011;6:69–78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Brener ND, McManus T, Galuska DA, et al. . Reliability and validity of self-reported height and weight among high school students. J Adolesc Health 2003;32:281–287 [DOI] [PubMed] [Google Scholar]
- 52.Flegal KM, Wei R, Ogden CL, et al. . Characterizing extreme values of body mass index-for-age by using the 2000 Centers for Disease Control and Prevention growth charts. Am J Clin Nutr 2009;90:1314–1320 [DOI] [PubMed] [Google Scholar]
- 53.Kelly AS, Barlow SE, Rao G, et al. . Severe obesity in children and adolescents: Identification, associated health risks, and treatment approaches: A scientific statement from the American Heart Association. Circulation 2013;128:1689–1712 [DOI] [PubMed] [Google Scholar]