Abstract
Background
Postoperative delirium (POD), defined as an acute state of confusion with fluctuating consciousness and inattention following surgery, is frequently seen in the elderly population. While the etiology of postoperative delirium has not been completely elucidated, one major trigger for POD appears to be the inflammatory response associated with surgery. We therefore hypothesized that intraoperative blood transfusion, a known trigger and amplifier of inflammation, is an independent risk factor for early POD in older patients undergoing surgery.
Design
Secondary analysis using a database created for a prospective cognitive outcomes study.
Setting
University hospital.
Participants
472 patients older than 65 years undergoing major non-cardiac surgery.
Measurements
Perioperative data was examined for association with POD on the first postoperative day. Multivariable logistic regression analysis was conducted to determine whether intraoperative blood transfusion independently predicts postoperative delirium after adjusting for covariates known to be associated with onset of both delirium and blood transfusions.
Results
137 patients (29%) developed delirium on the first postoperative day. The multivariable logistic regression model identified age, gender, history of CNS disorder, preoperative cognitive dysfunction and pain as well as blood transfusions as independent risk factors for postoperative delirium. Intraoperative administration of more than 1000ml erythrocyte concentrates (RBC) was the strongest predictor for POD on the first postoperative day (odds ratio, 3.68; 95% confidence interval, 1.32–10.94; p<0.001).
Conclusion
Intraoperative blood transfusion of more than 1000ml RBC increases the risk for delirium on the first postoperative day in elderly patients undergoing non-cardiac surgery.
Keywords: delirium, surgery, transfusion
INTRODUCTION
Postoperative delirium (POD), defined as “the acute onset and fluctuating course of mental status impairment, including inattention and either disorganized thinking or altered level of consciousness” 1 is frequently seen following surgery in elderly patients. Its incidence is reported to range from 9 to 87%, depending on patient age and type of surgery.2 Postoperative delirium results in prolonged hospital stays and worse postoperative outcome and increases the risk for early and long-term mortality.3 Postoperative delirium leads to increased physical dependence and a higher rate of discharge to a nursing home.4 Therefore, understanding the etiology and identifying risk factors for postoperative delirium could inform interventions to improve the outcomes of elderly patients undergoing surgery.
Although several risk factors for the development of postoperative delirium have been identified 5, its etiology is still not fully understood and probably multifactorial. One hypothesized cause of postoperative delirium is that it is the result of an acute inflammatory response, as increased serum and CSF concentrations of IL-1, IL-6 and IL-8 were found in patients with postoperative delirium. 6
Trauma such as surgery is known to trigger an inflammatory response. Another known trigger of an inflammatory response is blood transfusion. Transfusion has shown to directly increase plasma concentrations of inflammatory mediators 7 and to amplify the inflammatory response evoked by surgery.8 Such proinflammatory effects may explain why blood transfusion has been associated with decreased survival in trauma, following coronary artery bypass grafting 9, and in intensive care unit patients. 10
We hypothesized that blood transfusion, due to its proinflammatory effect, is an independent risk factor for the development of early postoperative delirium in elderly patients. Applying multivariable logistic regression, we included not only established preoperative risk factors of postoperative delirium into the model, but also controlled for covariates commonly associated with blood transfusion, such as blood loss, length of surgery, surgical risk group and preoperative hemoglobin concentrations to demonstrate the independent effect of blood transfusion on the development of postoperative delirium.
METHODS
The present study involved secondary analysis using a database created for a prospective cognitive outcomes study investigating the pathophysiology of postoperative delirium in older surgical patients. This prospective cohort study was approved by the University of California, San Francisco Committee on Human Research, and informed consent was obtained preoperatively from each study patient. The database contained complete datasets for all pre-, intra-, and postoperative variables used in the present analysis.
Study population
The original outcome study took place at the University of California, San Francisco Medical Center, from 2003–2011. The study inclusion criteria included English-speaking patients ≥65 years of age undergoing non-cardiac surgery requiring anesthesia and who were anticipated to stay in the hospital for longer than 48 hours. Exclusion criteria were inability to provide informed consent and preoperative delirium.
Patient Assessment
Research assistants conducted pre- and post-operative patient interviews in person. The preoperative interview occurred less than 48 hours before surgery in the preoperative clinic. During this preoperative interview, the patients were evaluated for depressive symptoms, pain, functional status, and cognitive status. Baseline cognitive status was obtained preoperatively using the Telephone Interview for Cognitive Status (TICS).11 TICS is an 11-item test (with a maximum score of 41 points), which correlates well with the Mini-Mental State Examination and widely used for screening of dementia. Scores below 30 on the TICS are considered to indicate cognitive impairment. During the same preoperative interview, the following neuropsychological tests were administered: the Word List Learning Test, the Digit Symbol Test, and the Controlled Verbal Fluency Test. These neuropsychological tests were repeated on the first two postoperative days. The tests were chosen as they target domains that were considered likely to change from pre- to post-operatively.
Delirium Assessment
A research assistant conducted structured interviews preoperatively and on the first two postoperative days between the hours of 9 a.m. to 12 pm. to determine the presence of delirium, defined using the Confusion Assessment Method (CAM).12 This method was developed as a screening instrument based on operationalization of the Diagnostic and Statistical Manual of Mental Disorders-III-R criteria. Based on a structured interview, the CAM algorithm consists of four clinical criteria: acute onset and fluctuating course, inattention, disorganized thinking, and altered level of consciousness. In order for delirium to be defined, both the first and second criteria have to be present, plus either criterion three or four. CAM has a sensitivity of 94–100% and a specificity of 90–95% and has a high interobserver reliability, and has convergent agreement with four other mental status tests. The research assistants were trained in the use of the CAM based on a detailed manual developed by Inouye et al. for administration of the CAM. The occurrence of delirium was defined as the patient meeting CAM criteria for delirium on any of the postoperative day assessments. Assessments were validated by one of the co-authors (LPS).
Statistical Methods
A logistic regression model was used to examine the association between blood transfusion and delirium. Bivariate and multivariable analyses were conducted to assess unadjusted and adjusted risks of delirium. Besides blood transfusion, the candidate predictors for the multivariable model included age, gender, TICS score, history of CNS disorder, alcohol use and chronic narcotic use, preoperative hemoglobin and creatinine concentrations, as well as ASA class, blood loss, length of surgery, and surgical risk group. This list of predictors of postoperative delirium was created in order to identify blood transfusion as an independent predictor of POD while controlling for factors previously shown to be related to delirium. An attempt was made to control for as many predictors of postoperative delirium as possible.
Hosmer and Lemeshow’s goodness-of-fit test was used to assess the fit of the model. Both Pearson and deviance residuals were assessed for normality and non-linearity across predictors. DFBETA’s were used to look for influential points. 13
All statistical analysis was performed with SAS, version 9.2 (Cary, NC) and R 2.15.1.
RESULTS
The present study analyzed the data of 472 patients older than 65 years old that underwent major non-cardiac surgery. Performed procedures included knee surgery (n=66, 15.2%), hip surgery (n=77, 17.8%), spinal surgery (n=90, 20.8%), abdominal surgery (n=117, 27.0%), thoracic surgery (n=25, 5.8%) and miscellaneous other procedures (n=58, 13.3%).
One hundred and thirty seven (29.0%) patients developed delirium on the first postoperative day (Table 1). Patients with postoperative delirium were more likely to receive blood transfusions (40.3% vs 25.8%) and received more blood (839±1207 vs. 572±841ml) compared to those without postoperative delirium. Patients who developed postoperative delirium were on average older, more often female, were more likely to have a history of previous CNS disorder and alcohol abuse, had lower TICS scores and higher pain scores during the preoperative assessment, a higher surgical risk score, and a higher incidence of preoperative anemia. These bivariate analyses are shown in Table 2.
Table 1.
Incidence of Delirium on the first postoperative day
| N (%) | |
|---|---|
| Delirium on Day 1 | |
| Yes | 137 (29.0) |
| No | 335 (71.0) |
Table 2.
Descriptive statistics and bivariate analyses. A logistic model was used to assess effects against onset of delirium on the first postoperative day.
| Delirium | No Delirium | P-Value | Odds Ratio (95% CI) | |
|---|---|---|---|---|
| Age | ||||
| <75 | 64 (46.7) | 228 (68.1) | - | - |
| >=75 | 73 (53.3) | 107 (31.9) | <.01 | 1.78 (1.25, 2.54) |
|
| ||||
| Gender | ||||
| Female | 86 (62.8) | 140 (41.8) | - | - |
| Male | 51 (37.2) | 195 (58.2) | <.01 | .54 (.38, .76) |
|
| ||||
| History of CNS Disorder | ||||
| Yes | 81 (59.1) | 140 (41.8) | - | - |
| No | 56 (40.9) | 195 (58.2) | <.01 | 1.89 (1.33, 2.69) |
|
| ||||
| History of Chronic Narcotic Use | ||||
| Yes | 89 (65.0) | 244 (72.8) | - | - |
| No | 48 (35.0) | 91 (27.2) | .06 | 1.41 (.98, 2.03) |
|
| ||||
| History of Alcohol Use | ||||
| Yes | 72 (52.6) | 138 (41,2) | - | - |
| No | 65 (47.4) | 197 (58.8) | .04 | .69 (.49, .98) |
|
| ||||
| Preoperative TICS Score | ||||
| <35 | 113 (82.5) | 219 (65.4) | - | - |
| >=35 | 24 (17.5) | 116 (34.6) | <.01 | .47 (.30, .71) |
|
| ||||
| Preoperative Pain Score | ||||
| 0 – 4 | 97 (70.8) | 276 (82.3) | - | - |
| 4+ | 40 (29.2) | 59 (17.6) | <.01 | 1.74 (1,16, 2.58) |
|
| ||||
| Preoperative Hemoglobin | ||||
| >=13 | 59 (43.1) | 193 (57.8) | - | - |
| <13 | 78 (56.9) | 142 (42.3) | <.01 | 1.88 (1.31, 2.70) |
|
| ||||
| Preoperative Creatinine | ||||
| <=1.3 | 115 (83.9) | 293 (87.4) | - | - |
| >1.3 | 22 (16.1) | 42 (12.5) | .51 | 1.19 (.69, 2.01) |
|
| ||||
| Surgery Risk | ||||
| 1–2 | 98 (71.5) | 283 (84.5) | - | - |
| 3 | 39 (28.5) | 52 (15.5) | <.01 | 1.87 (1.23, 2.82) |
|
| ||||
| ASA Class | ||||
| 1 or 2 | 57 (41.6) | 158 (47.2) | - | - |
| 3 or 4 | 80 (58.4) | 177 (52.8) | .08 | 1.37 (.97, 1.94) |
|
| ||||
| Anesthesia Duration | ||||
| <=3 hours | 25 (18.2) | 68 (20.3) | - | - |
| >3 hours | 112 (81.8) | 267 (79.7) | .40 | 1.22 (.78, 1.96) |
|
| ||||
| Blood Loss (per 500) | 850.8 (1191) | 617.5 (1224) | .05 | 1.07 (1.00, 1.15) |
|
| ||||
| Blood Transfusion | ||||
| 0 ml | 78 (56.9) | 246 (73.4) | - | - |
| <1000 ml | 35 (25.5) | 69 (20.6) | .03 | 1.60 (1.05, 2.41) |
| >=1000 ml | 23 (17.5) | 20 (6.0) | <.01 | 3.18 (1.82, 5.60) |
Columns 1 and 2 report the count (%) except for blood loss which reports the mean (SD).
Abbreviations: TICS: Telephone Interview for Cognitive Status, ASA: American Society of Anesthesiologists
Multivariable logistic regression was used to assess the adjusted effect of blood transfusion. Table 3 reports the results from the multivariable model. This model identified age, female gender, history of central nervous system (CNS) disorder, preoperative TICS score of less than 35, higher pain scores (≥4 out of 10 on the numerical rating scale) and received blood transfusions of more than 1000ml of erythrocyte concentrates (RBC) to be significant risk factors for postoperative delirium. Of note, intraoperative transfusion of more than 1000ml of RBC was the strongest predictor for delirium on the first postoperative day (odds ratio, 3.68; 95% confidence interval, 1.32–10.94; p<0.001). Figure 1 provides a visual description of the results from the full model.
Table 3.
Results of the multivariable logistic model. The Hosmer-Lemeshow test resulted in a p-value of .94 indicating the model fits the data well.
| p-Value | Odds Ratio (95% CI) | |||
|---|---|---|---|---|
| Age | ||||
| <75 | - | - | ||
| >=75 | .02 | 1.72 (1.09, 2.73) | ||
|
| ||||
| Gender | ||||
| Male | - | - | ||
| Female | <.01 | 1.88 (1.18, 3.03) | ||
|
| ||||
| History of CNS Disorder | ||||
| No | - | - | ||
| Yes | <.01 | 1.94 (1.24, 3.06) | ||
|
| ||||
| History of Chronic Narcotic Use | ||||
| Yes | - | - | ||
| No | .94 | 1.02 (.61, 1.70) | ||
|
| ||||
| History of Alcohol Abuse | ||||
| Yes | - | - | ||
| No | .65 | 1.11 (.71, 1.73) | ||
|
| ||||
| Preoperative TICS score | ||||
| >=35 | - | - | ||
| <35 | <.01 | 2.07 (1.22, 3.61) | ||
|
| ||||
| Preoperative Pain Score | ||||
| 0 – 4 | - | - | ||
| 4+ | <.01 | 1.52 (.88, 2.61) | ||
|
| ||||
| Preoperative Hemoglobin | ||||
| >=13 mg/DL | - | - | ||
| <13 mg/DL | .33 | 1.26 (.79, 2.01) | ||
|
| ||||
| Surgery Risk | ||||
| 1–2 | - | - | ||
| 3 | .13 | 1.66 (.85, 3.21) | ||
|
| ||||
| ASA Class | ||||
| 1 or 2 | - | - | ||
| 3 or 4 | .75 | 1.11 (.68, 1.70) | ||
|
| ||||
| Anesthesia Duration | ||||
| <=3 hrs | - | - | ||
| >3 hrs | .72 | 1.11 (.63, 1.99) | ||
|
| ||||
| Blood Loss (per 500) | .18 | .92 (.79, 1.03) | ||
|
| ||||
| Blood Transfusion | ||||
| 0 | - | - | ||
| <1000 ml | .70 | 1.12 (.63, 2.00) | ||
| >=1000 ml | .01 | 3.68 (1.32, 10.94) | ||
Figure 1.
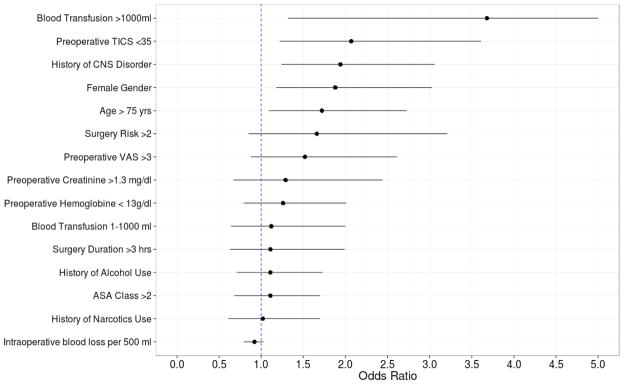
Results from the multivariable logistic model. Odds ratio estimates along with 95% confidence intervals are plotted for each covariate. We see blood transfusion of more than 1000 ml leads to the greatest risk of developing delirium on the first postoperative day.
Abbreviations: TICS: Telephone Interview for Cognitive Status, VAS: Visual Analog Scale for Pain, ASA: American Society of Anesthesiologists
DISCUSSION
The present study demonstrates that administration of intraoperative blood transfusions in older patients increases their risk of developing delirium on the first postoperative day. This is not the first study to report an association between intraoperative blood transfusions and postoperative delirium, but the first that identifies blood transfusion as the strongest predictor for early postoperative delirium in spite of controlling for risk factors associated with intraoperative blood transfusions, such as blood loss, duration of surgery, surgical risk, and preoperative hemoglobin concentrations.
Intraoperative transfusion of larger volumes of blood has repeatedly been linked to postoperative delirium. Gao et al. 14 associated transfusions of more than 800ml blood with postoperative delirium in spine patients. And a larger study in cardiac surgery patients identified blood transfusions of more than 2000ml as a precipitating factor for postoperative delirium. 15 Marcantonio et al. identified in a study with 1341 patients intraoperative blood loss, number of blood units transfused and lowest postoperative hematocrit to be associated with postoperative delirium.16 However, using logistic regression adjusting for risk factors for delirium, they subsequently identified a low postoperative hematocrit, but not transfusions or blood loss to be an independent risk factor for postoperative delirium. Similarly, Lee and Park 17, as well as Kawaguchi et al. 18 reported an association between postoperative hemoglobin concentrations, but not blood transfusions and delirium in older patients undergoing spine surgery. However, both studies were very small with only 11 and 13 patients diagnosed with postoperative delirium.
Marcantonio et al. suggested that postoperative levels of hematocrit should be kept at 30% to prevent postoperative delirium. The authors suggested that delirium may be the consequence of a central nervous system insult caused by the low hematocrit (i.e. decreased oxygen delivery). Such a suggestion however is not supported by our current results which demonstrate that patients with a postoperative hemoglobin concentration of 8–10 mg/dl have the same risk in developing postoperative delirium as patients with a hemoglobin concentration above 10mg/dl. Therefore, the findings of the present study provide evidence that avoiding perioperative blood transfusions in procedures with only moderate blood loss and accepting lower postoperative levels of hemoglobin may result in decreased risk for postoperative delirium. However, we cannot exclude that hemoglobin concentrations lower than 8 g/dl may precipitate postoperative delirium, as none of the patients in our study population had such a low hemoglobin concentration postoperatively.
Comparison with earlier studies might be complicated by different study designs. The prevalence of postoperative delirium was higher in our study than in the studies cited above. We believe that this is due to the prospective design of our study, our targeting older patients, and a higher sensitivity to detect postoperative delirium because patients were interviewed serially by the same research assistants. The majority of postoperative delirium patients presents with hypoactive delirium. 19 The large percentage of patients who did not present with agitated delirium may have been missed, thus resulting in an underestimation of the incidence of postoperative delirium in retrospective studies or studies that did not perform a postoperative assessment in all enrolled study patients using appropriate tests.
The most likely explanation for the deleterious effects of blood transfusion is its ability to trigger an inflammatory response. Stored red blood cell units contain activated inflammatory cells and mediators such as the cytokines tumor necrosis factor α (TNFα) and interleukin (IL)-6, IL-8 and IL 18. 20 The association between postoperative delirium and an inflammatory state is well established 21, 22, but by which mechanism inflammation triggers delirium is still incompletely understood.
Proinflammatory cytokines may increase the risk of delirium through multiple mechanisms. Systemic cytokine release is transmitted to the brain via direct neural pathways, transport across the blood-brain barrier or via the circumventricular region. The result is microglial activation and further cytokine release in cerebral tissue 23, resulting in direct impairment of neuronal function. 24 In addition, cytokines may lead to a central cholinergic deficit, a well established cause of delirium.25 Cytokines reduce choline acetyltransferase (ChAT) immunoreactive neurons thus inhibiting the biosynthesis of acetylcholine.26 In addition cytokines modify cerebral neurotransmission by reducing acetylcholine release. 27 However, this retrospective analysis is limited by the lack of perioperative serum cytokine concentration measurements. Therefore, the discussed link between an inflammatory response evoked by intraoperative transfusions and postoperative delirium remains merely speculative.
The present analysis focuses on delirium development on the first postoperative day as the effects of intraoperative blood transfusions are expected to be short lasting, based on the assumption that the development of POD was the consequence of an inflammatory response evoked by intraoperative transfusions. Such an inflammatory response is known to be transient. Administration of one unit of RBC in combination with 1 fresh frozen plasma (FFP) was reported to increase cytokine concentrations in healthy volunteers for only three hours. 28 When combined with the proinflammatory effects of the surgical trauma, such effects would be expected to be longer lasting. A recently published study in patients receiving transfusions during cardiac surgery demonstrated that concentrations of IL-6, IL-10, and IL-12 increased immediately after surgery, but then decreased within 24 hrs. 29
Whether leucocyte reduction of blood products ameliorates the inflammatory response following transfusion has so far not been adequately investigated. During the time of this investigation, leukocyte reduction of erythrocyte concentrates was already routinely performed in our institution. At this point we can only speculate that a lack of leukocyte reduction in blood products would result in an even higher incidence of early postoperative delirium in transfused patients.
The fact that both intraoperative transfusions and postoperative anemia are potentially risk factors for postoperative delirium appears to be a clinical dilemma because both transfusing or withholding a transfusion may harm the patient. A possible solution to avoid this situation could be advance targeted transfusion in anemic patients scheduled for procedures associated with larger blood loss. A recently published pilot study hypothesized that anemic patients scheduled for cardiac surgery who received blood transfusions 24 to 48 hours before surgery might be at lower risk for developing acute kidney injury than those patients who receive intraoperative blood transfusions. 30 Similarly, if anemic patients receive blood transfusion 24 to 48 hours before surgery rather than intraoperatively, the perioperative inflammatory response may be ameliorated, thus potentially reducing their risk for postoperative delirium. However, to investigate such hypothesis, an adequately powered prospective randomized study would be required.
In summary, our study identifies intraoperative blood transfusion as an independent risk factor for the development of postoperative delirium on the first postoperative day in elderly patients undergoing major non-cardiac surgery. Subsequent studies should determine whether a more restrictive approach to transfusion, which may result in lower postoperative hematocrits, lowers the incidence of postoperative delirium. Also, future studies should assess whether anti-inflammatory interventions lower the incidence of postoperative delirium. Until the mechanism by which blood transfusion increases risk for delirium is determined, clinicians should be aware that patients who received an intraoperative blood transfusion are at increased risk for development of early postoperative delirium and should be monitored accordingly.
Acknowledgments
This project was supported in part by the National Institute of Aging, National Institutes of Health, Bethesda, MD, Grant # NIH 1RO1AG031795-03 (Leung).
Sponsor’s Role: None
Footnotes
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
Author Contributions:
Matthias Behrends: study concept and design, data collection, data analysis, manuscript preparation
Glen DePalma: data analysis, statistical analysis, manuscript review
Laura Sands: study design, statistical analysis, manuscript review
Jacqueline Leung: study design, patient recruitment, manuscript review
References
- 1.Inouye SK. Prevention of delirium in hospitalized older patients: Risk factors and targeted intervention strategies. Ann Med. 2000;32:257–263. doi: 10.3109/07853890009011770. [DOI] [PubMed] [Google Scholar]
- 2.Whitlock EL, Vannucci A, Avidan MS. Postoperative delirium. Minerva Anestesiologica. 2011;77:448–456. [PMC free article] [PubMed] [Google Scholar]
- 3.Inouye SK. Delirium in older persons. N Engl J Med. 2006;354:1157–1165. doi: 10.1056/NEJMra052321. [DOI] [PubMed] [Google Scholar]
- 4.Marcantonio ER, Goldman L, Mangione CM, et al. A clinical prediction rule for delirium after elective noncardiac surgery. JAMA. 1994;271:134–139. [PubMed] [Google Scholar]
- 5.Steiner LA. Postoperative delirium. Part 1: Pathophysiology and risk factors. Eur J Anaesthesiol. 2011;28:628–636. doi: 10.1097/EJA.0b013e328349b7f5. [DOI] [PubMed] [Google Scholar]
- 6.Plaschke K, Fichtenkamm P, Schramm C, et al. Early postoperative delirium after open-heart cardiac surgery is associated with decreased bispectral EEG and increased cortisol and interleukin-6. Intensive Care Med. 2010;36:2081–2089. doi: 10.1007/s00134-010-2004-4. [DOI] [PubMed] [Google Scholar]
- 7.Avall A, Hyllner M, Bengtson JP, et al. Postoperative inflammatory response after autologous and allogeneic blood transfusion. Anesthesiology. 1997;87:511–516. doi: 10.1097/00000542-199709000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Fransen E, Maessen J, Dentener M, et al. Impact of blood transfusions on inflammatory mediator release in patients undergoing cardiac surgery. Chest. 1999;116:1233–1239. doi: 10.1378/chest.116.5.1233. [DOI] [PubMed] [Google Scholar]
- 9.Spiess BD. Transfusion of blood products affects outcome in cardiac surgery. Semin Cardiothorac Vasc Anesth. 2004;8:267–281. doi: 10.1177/108925320400800402. [DOI] [PubMed] [Google Scholar]
- 10.Hebert PC, Wells G, Blajchman MA, et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group. N Engl J Med. 1999;340:409–417. doi: 10.1056/NEJM199902113400601. [DOI] [PubMed] [Google Scholar]
- 11.Brandt JSM, Folstein MF. The telephone interview for cognitive status. Neuropsychiatry Neuropsychol Behav Neurol. 1988;1:111–117. [Google Scholar]
- 12.Inouye SK, van Dyck CH, Alessi CA, et al. Clarifying confusion: The confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113:941–948. doi: 10.7326/0003-4819-113-12-941. [DOI] [PubMed] [Google Scholar]
- 13.Kutner M. Applied Linear Statistics Models. Boston: McGraw-Hill Irwin; 2005. [Google Scholar]
- 14.Gao R, Yang ZZ, Li M, et al. Probable risk factors for postoperative delirium in patients undergoing spinal surgery. Eur Spine J. 2008;17:1531–1537. doi: 10.1007/s00586-008-0771-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bucerius J, Gummert JF, Borger MA, et al. Predictors of delirium after cardiac surgery delirium: Effect of beating-heart (off-pump) surgery. J Thorac Cardiovasc Surg. 2004;127:57–64. doi: 10.1016/s0022-5223(03)01281-9. [DOI] [PubMed] [Google Scholar]
- 16.Marcantonio ER, Goldman L, Orav EJ, et al. The association of intraoperative factors with the development of postoperative delirium. Am J Med. 1998;105:380–384. doi: 10.1016/s0002-9343(98)00292-7. [DOI] [PubMed] [Google Scholar]
- 17.Lee JK, Park YS. Delirium after spinal surgery in Korean population. Spine. 2010;35:1729–1732. doi: 10.1097/BRS.0b013e3181c423fc. [DOI] [PubMed] [Google Scholar]
- 18.Kawaguchi Y, Kanamori M, Ishihara H, et al. Postoperative delirium in spine surgery. Spine J. 2006;6:164–169. doi: 10.1016/j.spinee.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 19.Robinson TN, Raeburn CD, Tran ZV, et al. Motor subtypes of postoperative delirium in older adults. Arch Surg. 2011;146:295–300. doi: 10.1001/archsurg.2011.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hensler T, Heinemann B, Sauerland S, et al. Immunologic alterations associated with high blood transfusion volume after multiple injury: Effects on plasmatic cytokine and cytokine receptor concentrations. Shock. 2003;20:497–502. doi: 10.1097/01.shk.0000095058.62263.1f. [DOI] [PubMed] [Google Scholar]
- 21.Lemstra AW, Kalisvaart KJ, Vreeswijk R, et al. Pre-operative inflammatory markers and the risk of postoperative delirium in elderly patients. Int J Geriatr Psychiatry. 2008;23:943–948. doi: 10.1002/gps.2015. [DOI] [PubMed] [Google Scholar]
- 22.Rudolph JL, Ramlawi B, Kuchel GA, et al. Chemokines are associated with delirium after cardiac surgery. J Gerontol A Biol Sci Med Sci. 2008;63:184–189. doi: 10.1093/gerona/63.2.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.van Gool WA, van de Beek D, Eikelenboom P. Systemic infection and delirium: When cytokines and acetylcholine collide. Lancet. 2010;375:773–775. doi: 10.1016/S0140-6736(09)61158-2. [DOI] [PubMed] [Google Scholar]
- 24.Garden GA, Moller T. Microglia biology in health and disease. J Neuroimmune Pharmacol. 2006;1:127–137. doi: 10.1007/s11481-006-9015-5. [DOI] [PubMed] [Google Scholar]
- 25.Hshieh TT, Fong TG, Marcantonio ER, et al. Cholinergic deficiency hypothesis in delirium: A synthesis of current evidence. J Gerontol A Biol Sci Med Sci. 2008;63:764–772. doi: 10.1093/gerona/63.7.764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Willard LB, Hauss-Wegrzyniak B, Wenk GL. Pathological and biochemical consequences of acute and chronic neuroinflammation within the basal forebrain cholinergic system of rats. Neuroscience. 1999;88:193–200. doi: 10.1016/s0306-4522(98)00216-4. [DOI] [PubMed] [Google Scholar]
- 27.Taepavarapruk P, Song C. Reductions of acetylcholine release and nerve growth factor expression are correlated with memory impairment induced by interleukin-1beta administrations: Effects of omega-3 fatty acid EPA treatment. J Neurochem. 2010;112:1054–1064. doi: 10.1111/j.1471-4159.2009.06524.x. [DOI] [PubMed] [Google Scholar]
- 28.Frietsch T, Fessler H, Kirschfink M, et al. Immune response to autologous transfusion in healthy volunteers: WB versus packed RBCs and FFP. Transfusion. 2001;41:470–476. doi: 10.1046/j.1537-2995.2001.41040470.x. [DOI] [PubMed] [Google Scholar]
- 29.Bilgin YM, van de Watering LM, Versteegh MI, et al. Effects of allogeneic leukocytes in blood transfusions during cardiac surgery on inflammatory mediators and postoperative complications. Critical Care Med. 2010;38:546–552. doi: 10.1097/CCM.0b013e3181c0de7b. [DOI] [PubMed] [Google Scholar]
- 30.Karkouti K, Wijeysundera DN, Yau TM, et al. Advance targeted transfusion in anemic cardiac surgical patients for kidney protection: An unblinded randomized pilot clinical trial. Anesthesiology. 2012;116:613–621. doi: 10.1097/ALN.0b013e3182475e39. [DOI] [PubMed] [Google Scholar]


